NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Moxifloxacin is a fourth generation fluoroquinolone with expanded activity against gram-positive bacteria as well as atypical pathogens. Moxifloxacin has been linked to mild ALT elevations during therapy and to rare instances of idiosyncratic acute liver injury with symptoms and jaundice.
Background
Moxifloxacin (mox" i flox' a sin) is a fourth generation fluoroquinolone with expanded activity against gram-positive bacteria including multidrug resistant strains of Streptococcus pneumoniae. Like other fluoroquinolones, moxifloxacin is active against a wide range of aerobic gram-positive and gram-negative organisms. The quinolones are believed to act by inhibition of bacterial DNA gyrase and topoisomerase IV that are required for synthesis of bacterial mRNAs (transcription) and DNA replication. In contrast, DNA gyrases are not present in human [and other eukarotic] cells and the equivalent topoisomerases are not sensitive to fluoroquinolone inhibition. Moxifloxacin was approved for use in the United States in 1999 and is available generically and under the commercial names of Avelox, Moxeza and Vigamox. Current indications include mild-to-moderate bacterial infections such as sinusitis, bronchitis, community acquired pneumonia, skin infections, cellulitis, abscesses and complicated intraabdominal infections due to sensitive organisms. Moxifloxacin is also commonly used as a second line agent for therapy of tuberculosis and atypical mycobacterial infections. Moxifloxacin is available in formulations of 400 mg tablets, the usual dose being 400 mg daily for 5 to 14 days. Intravenous formulations are available for moderate to severe infections, the usual IV dosages being 400 mg daily. Common side effects include gastrointestinal upset, headaches, skin rash and allergic reactions. Less common but more severe side effects of the fluoroquinolones include prolongation of the QT interval, seizures, hallucinations, tendon rupture, severe hypersensitivity syndromes, angioedema, photosensitivity and Stevens Johnson syndrome.
Hepatotoxicity
Moxifloxacin, like other fluoroquinolones, is associated with a low rate (1% to 3%) of serum enzyme elevations during therapy. These abnormalities are generally mild, asymptomatic and transient, resolving even with continuation of therapy. Moxifloxacin has been linked to rare but occasionally severe and even fatal cases of acute liver injury. The time to onset is typically short (1 day to 3 weeks) and the presentation is often abrupt with nausea, fatigue, abdominal pain and jaundice. The pattern of serum enzyme elevations can be either hepatocellular or cholestatic, cases with the shorter times to onset usually being more hepatocellular. In addition, the onset of illness may occur a few days after the medication is stopped. Many (but not all) cases have prominent allergic manifestations with fever and rash, and the liver injury may occur in the context of a generalized hypersensitivity reaction (Case 1). Autoantibodies are usually not present. Cases with a cholestatic pattern of enzymes may run a prolonged course but are usually self-limiting, although at least one case of chronic cholestasis and vanishing bile duct syndrome leading to liver failure has been published. Most reported cases have been mild with recovery within 4 to 8 weeks of onset.
Likelihood score: B (rare but likely cause of clinically apparent liver injury).
Mechanism of Injury
The cause of hepatic injury is unknown but is likely to be immune-mediated as many cases occur in the context of a system hypersensitivity reaction. Moxifloxacin is metabolized by sulfate or glucuronide conjugation and has no effect on cytochrome P450 enzymes.
Outcome and Management
Mild-to-moderate hepatic injury due to moxifloxacin should be followed by full recovery within 4 to 8 weeks. Fulminant cases and chronic cholestatic forms with vanishing bile duct syndrome have been described. Cross reactivity of the hepatic injury between different fluoroquinolones has not been demonstrated, but is suspected based upon the similarity of clinical patterns of injury and latency. Thus, patients who develop clinically apparent liver injury from moxifloxacin should be advised to avoid further exposure to other fluoroquinolones.
Drug Class: Antiinfective Agents
Other Drugs in the Subclass, Fluoroquinolones: Ciprofloxacin, Delafloxacin, Gemifloxacin, Levofloxacin, Norfloxacin, Ofloxacin
CASE REPORT
Case 1. Severe hypersensitivity reaction and hepatitis due to moxifloxacin therapy.(1)
A previously healthy 45 year old man was treated with moxifloxacin for suspected sinusitis and developed severe rash, facial edema and fever one week later. He was admitted with the diagnosis of Stevens Johnson syndrome and was treated with systemic and topical corticosteroids. He had a past medical history of allergic reactions of amoxicillin and erythromycin, but had not received fluoroquinolone antibiotics in the past. He had no history of liver disease, alcohol abuse or risk factors for viral hepatitis. He was taking ranitidine and an antihistamine but denied taking over-the-counter or herbal preparations. On admission, serum aminotransferase values were markedly elevated (~18 fold) and the day after he became jaundiced (Table). There was no eosinophilia or lymphocytosis. Tests for hepatitis A, B and C were negative as were autoantibodies. An abdominal ultrasound was normal except for somewhat echogenic texture of the liver suggesting fatty infiltration. He was treated with methylprednisolone and his skin rash and jaundice improved over three weeks. Ultimately, liver tests returned to normal values.
Key Points
| Medication: | Moxifloxacin, 400 mg daily |
|---|---|
| Pattern: | Hepatocellular (R=11.4) |
| Severity: | 3+ (jaundice and hospitalization) |
| Latency: | 10 days |
| Recovery: | Approximately 3 weeks |
| Other medications: | Antihistamines, ranitidine |
Laboratory Values
Comment
This patient developed symptoms of generalized hypersensitivity approximately 9 days after starting moxifloxacin. He had an accompanying hepatitis and jaundice that was not severe. Some degree of hepatic involvement is common with severe hypersensitivity reactions to antibiotics, but usually the allergic manifestations dominate the clinical picture. Notice that the liver injury worsened for a week after stopping the implicated medication before beginning to resolve. The patient should be advised strongly to avoid further exposure to fluoroquinolone antibiotics.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Moxifloxacin – Generic, Avelox®
DRUG CLASS
Antiinfective Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Moxifloxacin HCl | 186826-86-8 | C21-H24-F-N3-O4.Cl-H |
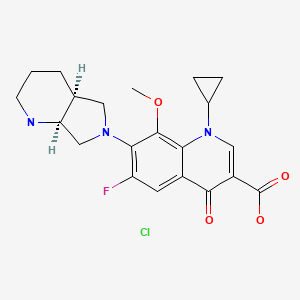
|
CITED REFERENCE
- 1.
- Orman ES, Conjeevaram HS, Vuppalanchi R, Freston JW, Rochon J, Kleiner DE, Hayashi PH., DILIN Research Group. Clinical and histopathologic features of fluoroquinolone-induced liver injury. Clin Gastroenterol Hepatol. 2011;9:517–23.e3. [PMC free article: PMC3718017] [PubMed: 21356330]
ANNOTATED BIBLIOGRAPHY
References updated: 10 March 2020
- Zimmerman HJ. Quinolones. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999. p 603.(Expert review of hepatotoxicity published in 1999 mentions that cinoxacin, nalidixic acid, ciprofloxacin, norfloxacin, enoxacin, and ofloxacin are associated with minor serum enzyme elevations during therapy and with rare instances of clinically apparent liver injury; moxifloxacin is not discussed).
- Moseley RH. Hepatotoxicity of antimicrobials and antifungal agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 463-82.(Review of hepatotoxicity of antibiotics mentions that hepatocellular and cholestatic forms of injury have been reported due to the quinolones including cases of ductopenia, acute liver failure and death).
- MacDougall C. The quinolones. Sulfonamides, trimethoprim-sulfamethoxazole, quinolones, and agents for urinary tract infections. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1015-8.(Textbook of pharmacology and therapeutics).
- Soto S, López-Rosés L, Avila S, et al. Moxifloxacin-induced acute liver injury. Am J Gastroenterol. 2002;97:1853–4. [PubMed: 12135060](69 year old man developed jaundice 3 weeks after completing a 5 day course of moxifloxacin for bronchitis [bilirubin 28.5 mg/dL, ALT 58 U/L, Alk P 249 U/L], resolving within 2 months of onset).
- Moxifloxacin--a new fluoroquinolone antibacterial. Drug Ther Bull. 2004;42:61–2. [PubMed: 15310155](Concise review of moxifloxacin shortly after its approval in the US states that it has no advantage over other, safer and less expensive antibiotics; ALT elevations mentioned as a potential side effect).
- Nori S, Bebesio C, Brashear R, Travers JB. Moxifloxacin-associated drug hypersensitivity syndrome with toxic epidermal necrolysis and fulminant hepatitis failure. Arch Dermatol. 2004;140:1537–8. [PubMed: 15611441](23 year old woman developed fever, rash and abdominal pain 3 days after starting moxifloxacin [bilirubin 2.7 mg/dL, ALT 3453 U/L, lymphocytosis], with progression to toxic epidermal necrolysis and acute liver failure and death despite liver transplantation within 2 weeks).
- Iannini PB. The safety profile of moxifloxacin and other fluoroquinolones in special patient populations. Curr Med Res Opin. 2007;23:1403–13. Erratum in: Curr Med Res Opin 2007; 23(9): 2303; dosage error in article text. [PubMed: 17559736](Systematic review of the literature on the safety of moxifloxacin; serum enzyme elevations were reported in occur 2-3% of patients, but were usually mild and self-limited even with continuing therapy; clinically apparent liver injury has been reported with trovafloxacin, gatifloxacin, and levofloxacin, but not with moxifloxacin).
- Van Bambeke F, Tulkens PM. Safety profile of the respiratory fluoroquinolone Moxifloxacin. Comparison with other fluoroquinolones and other antibacterial classes. Drug Safety. 2009;32:359–78. [PubMed: 19419232](Review of safety of moxifloxacin in comparison to other antibiotics and other fluoroquinolones; rare instances of acute liver failure have been attributed to moxifloxacin [0.7 per million prescriptions based upon FDA reporting rate]).
- Franco Hidalgo S, Prieto de Paula JM, García Lorenzo R, Salado Valdivieso I. Gastroenterol Hepatol. 2009;32:719–20. [Moxifloxacin and hepatic toxicity] Spanish. [PubMed: 19664854](44 year old man developed jaundice following a 4 day course of moxifloxacin for sinusitis [bilirubin 5.8 mg/dL, ALT 862 U/L, Alk P 421 U/L], resolving within one month of stopping).
- Puerto Alonso JL, Díaz Souza P, Chamorro Mohedano J, Rojas Martín E. Med Clin (Barc). 2010;134:375–6. [Fatal acute hepatitis and cholestasis associated with liver disease] Spanish. [PubMed: 19447449](58 year old man developed jaundice 1 week after completing a 5 day course of moxifloxacin [bilirubin 27 mg/dL, ALT 2589 U/L, Alk P 94 U/L, prothrombin index 36%], with progressive liver failure and death one month later).
- Orman ES, Conjeevaram HS, Vuppalanchi R, Freston JW, Rochon J, Kleiner DE, Hayashi PH., DILIN Research Group. Clinical and histopathologic features of fluoroquinolone-induced liver injury. Clin Gastroenterol Hepatol. 2011;9:517–23.e3. [PMC free article: PMC3718017] [PubMed: 21356330](Among 679 cases of drug induced liver injury presenting between 2004 and 2010 at 8 US medical centers, 12 [1.8%] were attributed to fluoroquinolones including 6 cipro-, 4 moxi-, 1 levo-, and 1 gatifloxacin; the average time to onset was 4 days [range 1-39], with both hepatocellular and cholestatic enzyme patterns, seven with rash or fever, mortality was limited to those with hepatocellular injury and jaundice; hepatic injury was class specific; moxifloxacin cases included 3 men, 1 woman, ages 45-71 years, onset after 1-7 days, 1 with fever and 2 with rash [bilirubin 0.9-5.3 mg/dL, ALT 220-1311 U/L, Alk P 253-837 U/L], one patient developed vanishing bile duct syndrome and underwent liver transplantation: Case 1).
- Roberts CH, Smith C, Breen R, Gadhok R, Murphy M, Aryee A, Cropley I, et al. Hepatotoxicity in the treatment of tuberculosis using moxifloxacin-containing regimens. Int J Tuberc Lung Dis. 2011;15:1275–6. [PubMed: 21943863](Retrospective analysis of liver test abnormalities in 194 patients on tuberculosis therapies, found no increase in liver abnormalities with moxifloxacin based therapies).
- Paterson JM, Mamdani MM, Manno M, Juurlink DN., Canadian Drug Safety and Effectiveness Research Network. Fluoroquinolone therapy and idiosyncratic acute liver injury: a population-based study. CMAJ. 2012;184:1565–70. [PMC free article: PMC3470619] [PubMed: 22891208](Population based, case control study of antibiotic exposure and subsequent hospitalization for liver injury within 30 days in elderly Canadian outpatients found weak associations with ciprofloxacin [adjusted odds ratio 1.56]), levofloxacin [2.06] and moxifloxacin [2.44], but not clarithromycin or cefuroxime).
- Hayashi PH, Chalasani NP. Liver injury in the elderly due to fluoroquinolones: should these drugs be avoided? CMAJ. 2012;184:1555–6. [PMC free article: PMC3470615] [PubMed: 22891207](Editorial in response to Paterson [2013] stressing the low absolute risk of liver injury from the fluoroquinolones [4-9 per 100,000 exposures]).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, including 26 due to antibiotics, but none were attributed to moxifloxacin or other fluoroquinolones).
- Kwon H, Lee SH, Kim SE, Lee JH, Jee YK, Kang HR, Park BJ, et al. Spontaneously reported hepatic adverse drug events in Korea: multicenter study. J Korean Med Sci. 2012;27:268–73. [PMC free article: PMC3286773] [PubMed: 22379337](Summary of 2 years of adverse event reporting in Korea; of 9360 reports, 567 were liver related, including 29 [5.1%] attributed to quinolones).
- Harr T, French LE. Stevens-Johnson syndrome and toxic epidermal necrolysis. Chem Immunol Allergy. 2012;97:149–66. [PubMed: 22613860](Review of the clinical features, epidemiology, genetics and pathogenesis of SJS and TEN).
- Patel TK, Barvaliya MJ, Sharma D, Tripathi C. A systematic review of the drug-induced Stevens-Johnson syndrome and toxic epidermal necrolysis in Indian population. Indian J Dermatol Venereol Leprol. 2013;79:389–98. [PubMed: 23619444](Systematic review of 10 case series of SJS/TEN from India identified 352 cases, among which 342 implicated a medication with most common being antimicrobials [37%], anticonvulsants [16%] and NSAIDs [16%]; fluoroquinolones accounted for 33 cases [10%], 4 of which were due to ciprofloxacin).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, one due to trovafloxacin [acute liver failure], but none attributed to ciprofloxacin or other fluoroquinolones).
- Kuzman I, Bezlepko A, Kondova Topuzovska I, Rókusz L, Iudina L, Marschall HP, Petri T. Efficacy and safety of moxifloxacin in community acquired pneumonia: a prospective, multicenter, observational study (CAPRIVI). BMC Pulm Med. 2014;14:105. [PMC free article: PMC4105837] [PubMed: 24975809](Among 2733 patients with community acquired pneumonia treated with moxifloxacin [400 mg daily], cure rates were 94% while adverse events arose in 5% and “no hepatic side effects …were reported”).
- Alshammari TM, Larrat EP, Morrill HJ, Caffrey AR, Quilliam BJ, LaPlante KL. Risk of hepatotoxicity associated with fluoroquinolones: a national case-control safety study. Am J Health Syst Pharm. 2014;71:37–43. [PubMed: 24352180](Retrospective analysis of Veterans Affairs patients receiving a fluoroquinolone [n=7862] found a higher relative risk of developing acute liver injury after receipt of ciprofloxacin compared to matched controls [adjusted odds ratio: OR=1.29], but not after receipt of levofloxacin [OR=1.16) or moxifloxacin [OR=0.98]).
- Kaye JA, Castellsague J, Bui CL, Calingaert B, McQuay LJ, Riera-Guardia N, Saltus CW, et al. Risk of acute liver injury associated with the use of moxifloxacin and other oral antimicrobials: a retrospective, population-based cohort study. Pharmacotherapy. 2014;34:336–49. [PMC free article: PMC4260122] [PubMed: 24865821](In a nested case control analysis of a health care network database of persons between 2001 and 2009, 8 selected antibiotics were assessed for association with risk of hospitalization for liver injury, adjusted relative risks being significantly elevated for levofloxacin [3.2], moxifloxacin [2.3], doxycycline [2.5], amoxicillin/clavulanate [2.5] and amoxicillin [2.3], but not for clarithromycin [1.8], telithromycin [1.7] or cefuroxime [0.9]).
- Dawson R, Diacon AH, Everitt D, van Niekerk C, Donald PR, Burger DA, Schall R, et al. Efficiency and safety of the combination of moxifloxacin, pretomanid (PA-824), and pyrazinamide during the first 8 weeks of antituberculosis treatment: a phase 2b, open-label, partly randomised trial in patients with drug-susceptible or drug-resistant pulmonary tuberculosis. Lancet. 2015;385(9979):1738–47. [PubMed: 25795076](Among 207 patients with pulmonary tuberculosis treated with 8 weeks of moxifloxacin [100 or 200 mg], pretomanid and pyrazinamide, response rates were similar as were adverse events although ALT or AST elevations were more frequent with moxifloxacin-pretomanid regimens [17% vs 12%]).
- Goldberg DS, Forde KA, Carbonari DM, Lewis JD, Leidl KB, Reddy KR, Haynes K, et al. Population-representative incidence of drug-induced acute liver failure based on an analysis of an integrated health care system. Gastroenterology 2015; 148: 1353-61. e3. [PMC free article: PMC4446162] [PubMed: 25733099](Analysis of Kaiser Permanente health care database from 2004 to 2011 identified 62 patients with suspected acute liver failure, 32 [52%] of whom had a presumed drug etiology, the most common being acetaminophen [18: 56%] and various herbal products [5: 16%], with single instances attributed to imatinib, simvastatin, leflunomide, isoniazid and valproate, but none to fluoroquinolones).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 38 cases [4%] were attributed to fluoroquinolones, including 16 due to ciprofloxacin [the 8th most common prescription drug cause], 13 due to levofloxacin and 8 to moxifloxacin).
- Barrera CM, Mykietiuk A, Metev H, Nitu MF, Karimjee N, Doreski PA, Mitha I, et al. SOLITAIRE-ORAL Pneumonia Team. Efficacy and safety of oral solithromycin versus oral moxifloxacin for treatment of community-acquired bacterial pneumonia: a global, double-blind, multicentre, randomised, active-controlled, non-inferiority trial (SOLITAIRE-ORAL). Lancet Infect Dis. 2016;16:421–30. [PubMed: 26852726](Among 860 patients with bacterial pneumonia treated with solithromycin [5 days] or moxifloxacin [7 days] response rates were similar as were adverse events and there were no serious hepatic adverse events).
- Naidoo A, Naidoo K, McIlleron H, Essack S, Padayatchi N. A review of moxifloxacin for the treatment of drug-susceptible tuberculosis. J Clin Pharmacol. 2017;57:1369–86. [PMC free article: PMC5663285] [PubMed: 28741299](Review of the role of moxifloxacin in treatment of tuberculosis mentions that rates of hepatotoxicity are reported to be less with moxifloxacin-based regimens and it is believed to be “liver-sparing”, although published differences in rates were not statistically significant).
- Xu P, Chen H, Xu J, Wu M, Zhu X, Wang F, Chen S, Xu J. Moxifloxacin is an effective and safe candidate agent for tuberculosis treatment: a meta-analysis. Int J Infect Dis. 2017;60:35–41. [PubMed: 28495364](Metaanalysis of nine controlled studies of the addition of moxifloxacin to antituberculosis drug regimens concludes that addition of moxifloxacin may increase the rate of culture conversion and decrease the rate of relapse but does not increase the rate of adverse events; no specific mention or discussion of rates of ALT elevations or hepatotoxicity).
- Marin AC, Nyssen OP, McNicholl AG, Gisbert JP. Efficacy and safety of quinolone-containing rescue therapies after the failure of non-bismuth quadruple treatments for Helicobacter pylori eradication: systematic review and meta-analysis. Drugs. 2017;77:765–76. [PubMed: 28361211](Systematic review of efficacy of fluoroquinolone-containing therapies of H. pylori infection after failure of standard treatments found eradication in 80% with triple and 90% with quadruple therapy; rates of specific adverse events were not discussed).
- Bonkovsky HL, Kleiner DE, Gu J, Odin JA, Russo MW, Navarro VM, Fontana RJ, Ghabril MS, et al. U.S. Drug Induced Liver Injury Network Investigators. Clinical presentations and outcomes of bile duct loss caused by drugs and herbal and dietary supplements. Hepatology. 2017;65:1267–77. [PMC free article: PMC5360519] [PubMed: 27981596](Among 363 patients with drug induced liver injury who underwent liver biopsy, 26 [7%] had bile duct loss of whom 94% developed evidence of chronic liver injury suggestive of vanishing bile duct syndrome, 2 of which were due to fluoroquinolones, 1 to moxifloxacin and 1 levofloxacin).
- Dixit A, Karandikar MV, Jones S, Nakamura MM. Safety and Tolerability of Moxifloxacin in Children. J Pediatric Infect Dis Soc. 2018;7:e92–e101. [PubMed: 29939314](Among 221 children who received 300 course of moxifloxacin, drug related aminotransferase elevations occurred in 8 [2.7%] with ALT ranging from 114 to 805 U/L and AST from 96 to 807 U/L]; no mention of jaundice or need for discontinuation).
- Tweed CD, Wills GH, Crook AM, Dawson R, Diacon AH, Louw CE, McHugh TD, et al. Liver toxicity associated with tuberculosis chemotherapy in the REMoxTB study. BMC Med. 2018;16:46. [PMC free article: PMC5875008] [PubMed: 29592805](Analysis of liver test abnormalities occurring in a trial of 1928 patients comparing standard 6 month isoniazid based regimens with shorter 4 month regimens using moxifloxacin and ethambutol found ALT elevations above 3 times ULN in 5.2% overall, 9.4% with standard therapy, 8% with 4 month course and 6% with 4 month course using ethambutol instead of isoniazid; two patients died of liver failure, one with rash, hemodynamic instability and rising bilirubin that was considered “hepatitis of unknown cause”).
- Comparison table: some systemic fluoroquinolones. Med Lett Drugs Ther. 2018;60:e57–e58. [PubMed: 29635268](Table comparing 4 fluoroquinolones [cipro-, levo-, dela- and moxifloxacin] mentions that ALT and AST elevations are a class adverse event).
- File TM, Goldberg L, Das A, Sweeney C, Saviski J, Gelone SP, Seltzer E, et al. Efficacy and Safety of Intravenous-to-oral Lefamulin, a Pleuromutilin Antibiotic, for the Treatment of Community-acquired Bacterial Pneumonia: The Phase III Lefamulin Evaluation Against Pneumonia (LEAP 1) Trial. Clin Infect Dis. 2019;69:1856–67. [PMC free article: PMC6853694] [PubMed: 30722059](Among 551 adults with community acquired pneumonia treated with intravenous lefamulin [150 mg every 12 hrs] or moxifloxacin [400 mg every 24 hrs] with option to switch to oral forms for 5-11 days, response rates were similar [87% vs 90%] as were adverse events overall [both 38%] and ALT elevations [1.8% vs 2.2%], and there were no hepatic related discontinuations or severe adverse events).
- Alexander E, Goldberg L, Das AF, Moran GJ, Sandrock C, Gasink LB, Spera P, et al. Oral lefamulin vs moxifloxacin for early clinical response among adults with community-acquired bacterial pneumonia: the LEAP 2 randomized clinical trial. JAMA. 2019;322:1661–71. [PMC free article: PMC6865224] [PubMed: 31560372](Among 738 adults with community acquired pneumonia treated with oral lefamulin [600 mg twice daily] or moxifloxacin [400 mg once daily] for 5 days, early clinical response rates were identical [91%], while gastrointestinal adverse events were more frequent with lefamulin including diarrhea [12% vs 1%] and nausea [5% vs 2%], but not ALT or AST elevations [0.5-0.8% vs 1.1%]).
- Mavros MN, Theochari NA, Kyriakidou M, Economopoulos KP, Sava JA, Falagas ME. Fluoroquinolone based versus β-lactam-based regimens for complicated intra-abdominal infections: a meta-analysis of randomised controlled trials. Int J Antimicrob Agents. 2019;53:746–54. [PubMed: 30639629](Systematic review of controlled trials of fluoroquinolones versus β-lactam-based antibiotic regimens found similar rates of efficacy and adverse events, no discussion of ALT elevations or liver related toxicities).
- Kuula LSM, Viljemaa KM, Backman JT, Blom M. Fluoroquinolone-related adverse events resulting in health service use and costs: A systematic review. PLoS One. 2019;14:e0216029. [PMC free article: PMC6485715] [PubMed: 31026286](Systematic review of observational studies on safety of fluoroquinolones concluded that due to lack of published literature, health service and costs could not be evaluated).
- Nunn AJ, Phillips PPJ, Meredith SK, Chiang CY, Conradie F, Dalai D, van Deun A, et al. STREAM Study Collaborators. A Trial of a Shorter Regimen for Rifampin-Resistant Tuberculosis. N Engl J Med. 2019;380:1201–13. [PubMed: 30865791](Among 424 patients with rifampin-resistant tuberculosis treated with a short course regimen [9-11 months] including high dose moxifloxacin or a longer course regimen [20 months] of standard therapy, response rates were similar [79% vs 80%] as were adverse event rates, but hepatobiliary disorders were more frequent with the moxifloxacin-containing courses [8.9% vs 5.7] including ALT elevations of more than 5 times ULN [6.6% vs 1.7%]).
- Tweed CD, Dawson R, Burger DA, Conradie A, Crook AM, Mendel CM, Conradie F, et al. Bedaquiline, moxifloxacin, pretomanid, and pyrazinamide during the first 8 weeks of treatment of patients with drug-susceptible or drug-resistant pulmonary tuberculosis: a multicentre, open-label, partially randomised, phase 2b trial. Lancet Respir Med. 2019;7:1048–58. [PMC free article: PMC7641992] [PubMed: 31732485](Among 240 patients with pulmonary tuberculosis treated with 1 of 3 regimens for 56 days, liver enzyme elevations were the most frequent adverse event with ALT or AST elevations above 5 times ULN in 5-10% of patients in the 3 regimens and resulted in drug withdrawal in 10 patients, but there were no deaths attributable to therapy).
- Velayutham B, Jawahar MS, Nair D, Navaneethapandian P, Ponnuraja C, Chandrasekaran K, Narayan Sivaramakrishnan G, et al. 4-month moxifloxacin containing regimens in the treatment of patients with sputum-positive pulmonary tuberculosis in South India - a randomised clinical trial. Trop Med Int Health. 2020 Jan 14; [Epub ahead of print] [PubMed: 31944502](Among 1371 patients with pulmonary tuberculosis treated with 3 or 4 month moxifloxacin based regimens vs standard 6 month regimen, moderate-to-severe hepatic adverse events occurred in 2.2% receiving moxifloxacin and 1.2% on standard therapy).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Delafloxacin.[LiverTox: Clinical and Researc...]Review Delafloxacin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Fluoroquinolone therapy and idiosyncratic acute liver injury: a population-based study.[CMAJ. 2012]Fluoroquinolone therapy and idiosyncratic acute liver injury: a population-based study.Paterson JM, Mamdani MM, Manno M, Juurlink DN, Canadian Drug Safety and Effectiveness Research Network. CMAJ. 2012 Oct 2; 184(14):1565-70. Epub 2012 Aug 13.
- Antibacterial activity of the fourth-generation fluoroquinolones gatifloxacin and moxifloxacin against ocular pathogens.[Adv Ther. 2003]Antibacterial activity of the fourth-generation fluoroquinolones gatifloxacin and moxifloxacin against ocular pathogens.Callegan MC, Ramirez R, Kane ST, Cochran DC, Jensen H. Adv Ther. 2003 Sep-Oct; 20(5):246-52.
- Review Moxifloxacin: a respiratory fluoroquinolone.[Expert Opin Pharmacother. 2008]Review Moxifloxacin: a respiratory fluoroquinolone.Miravitlles M, Anzueto A. Expert Opin Pharmacother. 2008 Jul; 9(10):1755-72.
- Review Review of third-and fourth-generation fluoroquinolones in ophthalmology: in-vitro and in-vivo efficacy.[Adv Ther. 2008]Review Review of third-and fourth-generation fluoroquinolones in ophthalmology: in-vitro and in-vivo efficacy.Scoper SV. Adv Ther. 2008 Oct; 25(10):979-94.
- Moxifloxacin - LiverToxMoxifloxacin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...