NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Abacavir sulfate is a nucleoside analogue and reverse transcriptase inhibitor which is used in combination with other agents in the therapy of the human immunodeficiency virus (HIV) infection and the acquired immunodeficiency syndrome (AIDS). Abacavir is a rare cause of clinically apparent drug induced liver injury.
Background
Abacavir (a bak' a vir) (cyclopropylaminopurinylcyclopentene: ABC) is a structural analogue of guanosine and acts by competing with naturally occurring nucleosides for incorporation into the HIV DNA strand during viral replication, causing inhibition of the viral polymerase and chain termination. Abacavir is indicated for the treatment of HIV infection in combination with other HIV medications such as lamivudine and zidovudine. Abacavir is available generically and under the trade name Ziagen in a 20 mg/mL oral solution and a 300 mg oral tablet. Abacavir is also available in fixed combination with lamivudine as Epzicom and Kivexa, with zidovudine and lamivudine as Trizivir and with dolutegravir and lamivudine as Triumeq. The recommended dose of abacavir is 300 mg orally twice daily or 600 mg orally once daily in adults and 8 mg/kg orally twice daily in children larger than 15 kg, with a maximum daily dose of 300 mg. Abacavir was approved for use in the United States in 1998 and is currently used in many antiretroviral regimens. Common side effects include diarrhea, loss of appetite, nausea, headache, and fatigue.
Hepatotoxicity
Elevations in serum aminotransferase levels above 5 times the upper limit of normal occur in up to 6% of patients on abacavir. These elevations are usually mild, transient and do not require dose adjustment. Clinically apparent hepatotoxicity is rare, but isolated cases [usually anicteric] have been published. The liver injury usually arises in the context of abacavir hypersensitivity syndrome and may be overshadowed by the allergic syndromes of fever, rash and fatigue. The onset is usually within 1 to 3 months of starting abacavir. The serum enzyme pattern can be hepatocellular or cholestatic. Patients typically recover rapidly within 4 weeks of stopping therapy.
Likelihood score: C (probable cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the clinically apparent hepatotoxicity from abacavir is hypersensitivity in some cases and is typically associated with the HLA-B*57:01 haplotype. Abacavir binds to the antigen-binding cleft of the HLA-B*57:01 molecule and alters its peptide binding repertoire. Testing for this allele is available in the United States and is recommended before starting abacavir. There are few cases of nonhypersensitivity abacavir induced hepatitis (Case 1) in which the mechanism is unknown.
Outcome and Management
Most cases of liver injury associated with abacavir have been mild and anicteric and resolved rapidly within 4 weeks of discontinuation. There have been no convincing published cases of acute liver failure or vanishing bile duct syndrome due to abacavir. Patients with hepatotoxicity due to abacavir can generally tolerate other antiretroviral agents, rechallenge should be avoided, particularly in cases with features of hypersensitivity.
Drug Class: Antiviral Agents, Antiretroviral Agents
Other Drugs in the Subclass, Nucleoside Analogues: Adefovir, Didanosine, Emtricitabine, Entecavir, Lamivudine, Stavudine, Telbivudine, Tenofovir, Zidovudine
CASE REPORT
Case 1. Abnormal liver function tests occurring in a young HLA B*5701-negative woman shortly after switching to abacavir.
[Modified from: Soni S, Churchill DR, Gilleece Y. Abacavir-induced hepatotoxicity: a report of two cases. AIDS 2008; 22: 2557-8. PubMed Citation]
A 26 year old woman switched from a regimen of zidovudine, lamivudine and nevirapine to abavir/lamivudine/nevirapine and developed nausea six weeks later, but continued on therapy for another month when liver tests were found to be abnormal. Before starting abacavir, she had tested negative for the HLA B*57:01 allele and had normal serum aminotransferase levels. She did not drink alcohol to excess and had no history of liver disease. Serological testing showed no evidence of acute or chronic hepatitis B or C and she tested positive for anti-HAV and anti-HBs, indicative of previous vaccinations. On presentation, serum ALT was 433 U/L. Nevirapine was stopped, but she did not improve and a liver biopsy was done showing severe acute hepatitis with lobular collapse, changes suggestive of drug induced liver injury. Abacavir was discontinued and her symptoms quickly improved. Serum aminotransferases returned to normal 4 weeks later.
Key Points
| Medication: | Abacavir |
|---|---|
| Pattern: | Hepatocellular |
| Severity: | 1+ (no jaundice) |
| Latency: | 4 weeks |
| Recovery: | 4 weeks |
| Other medications: | Nevirapine, lamivudine, lopinavir |
Comment
While liver injury as a part of the hypersensitivity reaction to abacavir is most common in persons with the HLA B*57:01 allele, hepatotoxicity can occur without frank hypersensitivity in other individuals. The injury in this case arose after 6 weeks of therapy, although the presence of liver disease was not suspected until several weeks later. The patient did not become jaundiced (bilirubin levels were not mentioned), but the severity of the illness was shown by liver biopsy findings and manifested by the presence of persistent symptoms. Elevations in serum aminotransferase levels are common during antiretroviral therapy and do not always warrant dose adjustment of drug-continuation. However, the co-occurrence of clinical symptoms and serum aminotransferase elevations is usually indicative of moderate or severe injury and should trigger investigation and alteration in drug regimen.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Abacavir – Ziagen®
DRUG CLASS
Antiviral Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Abacavir | 136470-78-5 | C14-H18-N6-O |
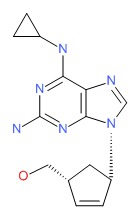 |
ANNOTATED BIBLIOGRAPHY
References updated: 04 January 2016
- Núñez M. Hepatic toxicity of antiviral agents. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 505-18.(Review of hepatotoxicity of antiviral agents including the nucleoside reverse transcriptase inhibitors).
- Flexner C. Antiretroviral agents and treatment of HIV infection. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1623-64.(Textbook of pharmacology and therapeutics).
- http://aidsinfo.nih.gov/guidelines.(Clinical guidelines on the use of antiretroviral agents in HIV-1 infected adults, adolescents and children).
- Lewis W, Dalakas MC. Mitochondrial toxicity of antiviral drugs. Nature Med 1995; 1: 417-23. [PubMed: 7585087](Review of mechanisms for mitochondrial injury by nucleoside analogues, including inhibition of mitochondrial DNA polymerase gamma).
- Brinkman K, ter Hofstede HJ, Burger DM, Smeitink JAM, Koopmans PP. Adverse effects of reverse transcriptase inhibitors: mitochondrial toxicity as a common pathway. AIDS 1998; 12: 1735-44. [PubMed: 9792373](Review of mitochondrial function and role of mitochondrial toxicity or depletion in the adverse side effects of nucleoside analogues).
- Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Hepatotoxicity associated with antiretroviral therapy in adults infected with human immunodeficiency virus and the role of hepatitis C or B virus infection. JAMA 2000; 283: 74-80. [PubMed: 10632283](Among 298 patients with HIV infection, ALT elevations above 5 times ULN occurred in 10.4% per year during antiretroviral treatment; factors associated with ALT elevations included ritonavir [27.3%] and coinfection with either HCV or HBV; ALT with bilirubin elevations occurred in 3 patients; 2 on indinavir and all 3 with coinfection).
- Velasco M, Guijarro C. Elevated liver enzymes following initiation of antiretroviral therapy. JAMA 2000; 283: 2526-7. [PubMed: 10815112](Letter in response to Sulkowski et al. [JAMA 2000] pointing out that antiretroviral therapy can cause immune reconstitution and flares of hepatitis B or C which may be misdiagnosed as hepatotoxicity).
- Sulkowski MS, Thomas DL, Chaisson RE, Moore RD. Elevated liver enzymes following initiation of antiretroviral therapy JAMA 2000; 283: 2526-7. [PubMed: 10815113](Reply to Velasco and Guijarro pointing out that the majority of the ALT elevations described could not be attributed to immune reconstitution).
- Hetherington S, McGuirk S, Powell G, Cutrell A, Naderer O, Spreen B, Lafon S, et al. Hypersensitivity reactions during therapy with nucleoside reverse transcriptase inhibitor abacavir. Clin Ther 2001; 23: 1603-14. [PubMed: 11726000](Among ~200,000 patients treated with abacavir, 1803 had a suspected hypersensitivity reaction [4.3% of those in clinical trials] marked by fever, rash, fatigue and GI upset, mostly within 1-3 weeks of starting abacavir; 14% had accompanying liver test abnormalities).
- Mallal S, Nolan D, Witt C, Masel G, Martin AM, Moore C, Sayer D, et al. Association between presence of HLA-B*5701, HLA-DR7, and HLA-DQ3 and hypersensitivity to HIV-1 reverse transcriptase inhibitor abacavir. Lancet 2002; 359: 727-32. [PubMed: 11888582](Among 200 Australian patients started on abacavir, 18 developed hypersensitivity, 14 [78%] of whom had HLA-B*57:01 vs 2% [4/167] of controls).
- Hetherington S, Hughes ARR, Mosteller M, Shortino D, Baker KL, Spreen W, Lai E, et al. Genetic variations in HLA-B region and hypersensitivity reactions to abacavir. Lancet 2002; 1121-2. [PubMed: 11943262](Case controlled study found HLA-B57 in 46% of 84 patients with abacavir hypersensitivity vs 4% of 113 controls; more significant in whites than blacks).
- Spengler U, Lichterfeld M, Rockstroh JK. Antiretroviral drug toxicity.a challenge for the hepatologist? J Hepatol 2002; 36: 283-94. [PubMed: 11830343](Review of the diagnosis of drug induced liver disease in patients with HIV on antiretroviral agents with discussion of mechanisms including mitochondrial toxicity and hypersensitivity reactions).
- Dumouchel-Champagne H, Bouhour D, Ferry T, Durupt F, Granier P. Rétion d'hypersensibilité l'abacavir ou hétite syphilitique? Presse Med 2003; 32: 1577-8. [PubMed: 14576594](24 year old man developed rash and fever 15 days after starting abacavir with ALT 129 U/L and Alk P 299 U/L; there was no response to stopping abacavir and he was later found to have syphilis).
- Kontorinis N, Dieterich D. Hepatotoxicity of antiretroviral therapy. AIDS Rev 2003; 5: 36-43. [PubMed: 12875106](Review of hepatotoxicity of antiretroviral drugs; definition of hepatotoxicity in antiretroviral studies; grade 1=1.25-2.5 times, grade 2=2.6-5 times, grade 3=5.1-10 times and grade 4=>10 times normal or baseline ALT values; abacavir and lamivudine are least likely to cause hepatotoxicity).
- Ogedegbe AO, Sulkowski MS. Antiretroviral-associated liver injury. Clin Liver Dis 2003; 7: 475-99. [PubMed: 12879995](Review of hepatotoxicity of antiretrovirals; ALT elevations above 5 times ULN reported in 7% with zidovudine, 16% didanosine, 9-13% stavudine, <1% lamivudine, tenofovir and abacavir, 3-10% protease inhibitors, 10% nevirapine and 8% efavirenz; recommends monitoring at 4 weeks and then every 12 weeks, stopping if ALT levels are >10 times ULN or if symptoms of liver injury are present, monitoring more closely if ALT levels are elevated).
- Ofotokun I, Pomeroy C. Sex differences in adverse reactions to antiretroviral drugs. Top HIV Med 2003; 11: 55-9. [PubMed: 12717043](Review of sex differences in adverse events; mentions a higher frequency of mitochondrial toxicity and hypersensitivity in women than men).
- Lonergan JT, McComsey GA, Fisher RL, Shalit P, File TM Jr, Ward DJ, Williams VC, et al. for the ESS40010(TARHEEL) Study Team. Lack of recurrence of hyperlactatemia in HIV-infected patients switched from stavudine to abacavir or zidovudine. J Acquir Immune Defic Syndr 2004; 36: 935-42. [PubMed: 15220700](Prospective study of 118 patients with HIV infection on stavudine who switched to abacavir or zidovudine; lactate levels fell upon stopping stavudine and despite starting other agents; few were markedly hyperlactatemic).
- Giola M, Basilico C, Grossi P. Fatal lactic acidosis associated with tenofovir and abacavir. Int J Infect Dis 2005; 9: 228-9. [PubMed: 15916912](60 year old man developed fatal lactic acidosis and liver injury 5 months after being switched from stavudine to abacavir while continuing tenofovir and nevirapine [ALT 70 U/L, lactate 9.7 micromol], and progressive acidosis).
- Abrescia N, D.Abbraccio M, Figoni M, Busto A, Maddaloni A, De Marco M. Hepatotoxicity of antiretroviral drugs. Curr Pharm Des 2005; 11: 3697-710. [PubMed: 16305505](Review of hepatotoxicity of antiretrovirals; major syndrome with nucleoside analogues is mitochondrial injury with lactic acidosis and severe hepatomegaly and steatosis).
- Stekler J, Maenza J, Stevens C, Holte S, Malhotra U, McElrath MJ, Corey L, et al. Abacavir hypersensitivity reaction in primary HIV infection. AIDS 2006; 20: 1269-74. [PubMed: 16816555](Among 50 men with acute HIV infection treated with a regimen including abacavir, 9 [18%] developed symptoms of hypersensitivity [rash, fever, fatigue] 1-60 days after starting, but all resolved and no mention of hepatotoxicity; only two had HLA B* 57:01).
- Bourlière M, Duclos-Vallé JC, Pol S. [Liver and antiretrovirals: hepatotoxicity, steatosis and monitoring of patients with liver disease] Gastroenterol Clin Biol 2007; 31: 895-905. French. [PubMed: 18166875](Review of hepatotoxicity of antiretrovirals in French discussing patterns of idiosyncrasy, hypersensitivity [nevirapine and abacavir], mitochondrial toxicity [zalcitabine, didanosine, stavudine, zidovudine], steatohepatitis [protease inhibitors with lipodystrophy], immune restoration [in patients with HBV or HCV coinfection], recommendations for management focusing on prevention and monitoring).
- Jain MK. Drug-induced liver injury associated with HIV medications. Clin Liver Dis 2007; 11: 615-39, vii-viii. [PubMed: 17723923](Review of hepatotoxicity of antiretroviral drugs; ALT elevations occur in 2-18% of patients, but often resolve spontaneously even without dose modification; classes of injury include hypersensitivity [nevirapine, efavirenz, abacavir], mitochondrial injury [stavudine, didanosine, zidovudine], flares of hepatitis B [lamivudine, emtricitabine, tenofovir], flares of hepatitis C [any potent regimen], idiosyncratic injury [ritonavir, nevirapine, efavirenz], cholestatic hepatitis [many agents]).
- Esser S, Helbig D, Hillen U, Dissemond J, Grabbe S. Side effects of HIV therapy. J Dtsch Dermatol Ges 2007; 5: 745-54. [PubMed: 17760894](Review of side effects of antiretroviral agents focusing on immune reconstitution syndrome, lipodystrophy, cutaneous skin reactions, hypersensitivity reactions [abacavir, nevirapine], hyperbilirubinemia [indinavir, atazanavir], local reactions [enfuvirtide] and hyperpigmentation [zidovudine, emtricitabine]).
- Waters LJ, Mandalia S, Gazzard B, Nelson M. Prospective HLA-B*5701 screening and abacavir hypersensitivity: a single centre experience. AIDS 2007; 21: 2533-4. [PubMed: 18025891](Hypersensitivity reactions to abacavir occurred in only 2% of HLA-B*57:01-negative patients; symptoms included fever, rash and gastrointestinal upset).
- FDA notifications. Abacavir package insert changes approved. Hypersensitivity, other issues addressed. AIDS Alert 2008; 23: 102-4. [PubMed: 18939305](FDA update regarding adverse effects of abacavir).
- Mallal S, Phillips E, Carosi G, Molina JM, Workman C, Tomazic J, Jäl-Guedes E, et al.; PREDICT-1 Study Team. HLA-B*5701 screening for hypersensitivity to abacavir. N Engl J Med 2008; 358: 568-79. PubMed Citation. [PubMed: 18256392](Prospective trial of screening for HLA-B*57:01 in 1956 patients given abacavir; hypersensitivity reactions occurred in 7.8% of unscreened controls vs 3.4% of screened; but immunologically confirmed cases occurred only in unscreened group [2.7% vs 0%]).
- Soni S, Churchill DR, Gilleece Y. Abacavir-induced hepatotoxicity: a report of two cases. AIDS 2008; 22: 2557-8. [PubMed: 19005287](Two cases of anicteric liver injury [peak ALT 433 and 580 U/L] after 2-3 months of abavir therapy, both patients did not have HLA-B*57:01 and both resolved within 4 weeks of stopping: Case 1).
- Hughes CA, Foisy MM, Dewhurst N, Higgins N, Robinson L, Kelly DV, Lechelt KE. Abacavir hypersensitivity reaction: an update. Ann Pharmacother 2008; 42: 387-96. [PubMed: 18303141](Review of abacavir hypersensitivity; occurs in ~5% of patients exposed, usually in first 6 weeks [mean=11 days], worsening if continued and improving in 2-3 days of stopping, fever in 80%, rash in 70%, fatigue, myalgias, headache, diarrhea, itching, respiratory symptoms, dyspnea, or pharyngitis and liver test abnormalities occasionally; linked to HLA-B*57:01, which is found in 8% of European whites, <1% of Africans; confirmed cases rare in HLA-B57-negative subjects).
- Hammer SM, Eron JJ Jr, Reiss P, Schooley RT, Thompson MA, Walmsley S, Cahn P, et al.; International AIDS Society-USA. Antiretroviral treatment of adult HIV infection: 2008 recommendations of the International AIDS Society-USA panel. JAMA 2008; 300: 555-70. [PubMed: 18677028](Updated recommendations on use of antiviral therapy in adults with HIV infection including use of recently approved agents raltegravir, maraviroc and etravirine).
- Inductivo-Yu I, Bonacini M. Highly active antiretroviral therapy-induced liver injury. Current Drug Safety 2008; 3: 4-13. [PubMed: 18690975](Review of drug induced liver injury due to antiretroviral agents).
- Soriano V, Puoti M, Garcia-Gascó Rockstroh JK, Benhamou Y, Barreiro P, McGovern B. Antiretroviral drugs and liver injury. AIDS 2008; 22: 1-13. [PubMed: 18090386](Review of hepatotoxicity of antiretrovirals with recommendations on management, stopping therapy if symptoms arise, with overt jaundice [direct bilirubin], evidence of mitochondrial toxicity, ALT >10 times ULN, ALT at lower levels if newly marketed agent; important to rule out other causes: problematic agents include didanosine, stavudine and zidovudine; nevirapine and efavirenz, full dose ritonavir and tipranavir).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected between 2004 and 2008, 7 were attributed to antiretroviral agents, 2 nevirapine, 1 efavirez and 4 miscellaneous combinations).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, 3 antiretroviral agents were among the top 40 causes, including zidovudine [8th, 106 cases], lamivudine [26th, 45 cases] and nevirapine [36th, 37 cases]).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol 2010; 105: 2396-404. [PubMed: 20648003](313 cases of drug induced liver injury were seen between 1997 and 2008 at a large hospital in Bangalore, India; none were attributed to antiretroviral agents).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury and 4 to antiretroviral agents, including 3 to combinations with stavudine and 1 to abacavir).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N: Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr 2011; 53: 182-9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, none were attributed to an antiretroviral agent).
- Sanchez-Giron F, Villegas-Torres B, Jaramillo-Villafuerte K, Silva-Zolezzi I, Fernandez-Lopez JC, Jimenez-Sanchez G, Carnevale A. Association of the genetic marker for abacavir hypersensitivity HLA-B*5701 with HCP5 rs2395029 in Mexican Mestizos. Pharmacogenomics 2011; 12: 809-14. [PubMed: 21510768](HLA-B*57:01 was identified in 2% of Mexican Mestizos and was in complete linkage disequilibrium with HCP5 rs2395029).
- Kostenko L, Kjer-Nielsen L, Nicholson I, Hudson F, Lucas A, Foley B, Chen K, et al. Rapid screening for the detection of HLA-B57 and HLA-B58 in prevention of drug hypersensitivity. Tissue Antigens 2011; 78: 11-20. [PubMed: 21501118](Description of a monoclonal antibody reactive to HLA-B57 and B58 that was reliable in screening peripheral blood lymphocytes for these HLA alleles and might be used clinically).
- Trottier B, Machouf N, Thomas R, Gallant S, Longpré D, Vézina S, Boissonnault M, Lavoie S, Legault D, Dion H, Nguyen VK. Abacavir/lamivudine fixed-dose combination with ritonavir-boosted darunavir: a safe and efficacious regimen for HIV therapy. HIV Clin Trials 2012; 13: 335-42. [PubMed: 23195671](Among 65 patients with HIV infection [HLA-B*57:01 negative] treated with lamivudine, abacavir and darunavir with ritonavir for 48 weeks, none developed ALT elevations greater than 3 times ULN).
- Illing PT, Vivian JP, Dudek NL, Kostenko L, Chen Z, Bharadwaj M, Miles JJ, et al. Immune self-reactivity triggered by drug-modified HLA-peptide repertoire. Nature 2012; 486(7404): 554-8. [PubMed: 22722860](Abacavir binds specifically to HLA-B*57:01, lying across the bottom of the antigen binding clerft, changing its shape and chemistry and altering the repertoire of peptides that can bind and be presented by HLA-B*57:01).
- Kaniwa N, Saito Y. Pharmacogenomics of severe cutaneous adverse reactions and drug-induced liver injury. J Hum Genet 2013; 58: 317-26. [PubMed: 23635947](Review of genetics of severe cutaneous adverse reactions, including hypersensitivity reactions to abacavir which has been linked closely to HLA-B*57:01 in both Caucasian and African populations).
- Borghi V, Bisi L, Manzini L, Cossarizza A, Mussini C. Absence of liver steatosis in HIV-HCV co-infected patients receiving regimens containing tenofovir or abacavir. Infection 2013; 41: 425-9. [PubMed: 23225268](Analysis of liver biopsies from 205 patients with HIV/HCV coinfection found significant steatosis [>5%] in 48% and its presence was associated with HCV genotype 3 and exposure to stavudine, but not to abacavir, lamivudine, didanosine or tenofovir).
- Illing PT, Vivian JP, Purcell AW, Rossjohn J, McCluskey J. Human leukocyte antigen-associated drug hypersensitivity. Curr Opin Immunol 2013; 25: 81-9. [PubMed: 23141566](Review of the basis of T cell activation by the interaction of abacavir with the antigen presenting HLA motif of B*57:01, abacavir appearing to alter the nature of the peptides that were accomodated in the antigen binding cleft of the HLA allele).
- Di Filippo E, Ripamonti D, Rizzi M. Abacavir-induced liver toxicity in an HIV-infected patient. AIDS 2014; 28: 613. [PubMed: 24469001](37 year old man without HLA B*57:01 was found to have raised serum enzymes without symptoms or allergic manifestations 8 weeks after switching from zidovudine to abacavir [ALT 770 U/L, bilirubin and Alk P not given], improving rapidly on switching back to zidovudine).
- Daly AK. Human leukocyte antigen (HLA) pharmacogenomic tests: potential and pitfalls. Curr Drug Metab 2014; 15: 196-201. [PubMed: 24694233](Review of use of HLA typing to avoid adverse drug reactions, discusses the role of HLA-B*57:01 before prescribing abacavir and HLA-B*15:02 before prescribing carbamazepine in East Asians).
- Haas C, Ziccardi MR, Borgman J. Abacavir-induced fulminant hepatic failure in a HIV/HCV co-infected patient. BMJ Case Rep 2015; 2015. [PMC free article: PMC4680310] [PubMed: 26670894](50 year old man with HIV-HCV coinfection who had HLA-B*57:01 developed nausea and myalgias 2 weeks after switching to abacivr, dolutegravir and lamivudine [Triumeq] and subsequently developed acute liver and renal dysfunction [bilirubin not given, ALT 310 U/L, INR 2.3, creatinine 3.1 mg/dL, CPK 6896 U/L], responding rapidly to stopping abacavir and hydration; probably rhabdomyolysis more than hepatic failure).
- Yip VL, Alfirevic A, Pirmohamed M. Genetics of immune-mediated adverse drug reactions: a comprehensive and clinical review. Clin Rev Allergy Immunol 2015; 48(2-3): 165-75. [PubMed: 24777842](Review and update of genetic associations with severe drug adverse events including abacavir hypersensitivity reactions and HLA-B*57:01).
- Lin KY, Liao SH, Liu WC, Cheng A, Lin SW, Chang SY, Tsai MS, et al. Cholelithiasis and nephrolithiasis in HIV-positive patients in the era of combination antiretroviral therapy. PLoS One 2015; 10 :e0137660. [PMC free article: PMC4567270] [PubMed: 26360703](Review of records of 910 patients with HIV infection who underwent abdominal ultrasonography over an 11 year period, 680 of whom had a second examination, found 4.3% had developed cholelithiasis which in multivariate analysis was associated with atazanavir/r therapy and older age while new onset nephrolithiasis occurred in 3.7% and was associated with chronic hepatitis B or C, hyperlipidemia and exposure to abacavir).
- Michels AW, Ostrov DA. New approaches for predicting T cell-mediated drug reactions: A role for inducible and potentially preventable autoimmunity. J Allergy Clin Immunol 2015; 136: 252-7. [PMC free article: PMC4529959] [PubMed: 26254052](Review of the pathogenesis and HLA associations of severe drug adverse events with features of hypersensitivity and their similarity to spontaneous autoimmune diseases).
- Pirmohamed M, Ostrov DA, Park BK. New genetic findings lead the way to a better understanding of fundamental mechanisms of drug hypersensitivity. J Allergy Clin Immunol 2015; 136: 236-44. PubMed 26254050. [PMC free article: PMC4534769] [PubMed: 26254050](Update and review of HLA associations with serious drug reactions including abacavir hypersensitivity which appears to the T-cell mediated and linked to HLA-B*57:01).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-1352. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to abacavir).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Resistance profile of the human immunodeficiency virus type 1 reverse transcriptase inhibitor abacavir (1592U89) after monotherapy and combination therapy. CNA2001 Investigative Group.[J Infect Dis. 2000]Resistance profile of the human immunodeficiency virus type 1 reverse transcriptase inhibitor abacavir (1592U89) after monotherapy and combination therapy. CNA2001 Investigative Group.Harrigan PR, Stone C, Griffin P, Nájera I, Bloor S, Kemp S, Tisdale M, Larder B. J Infect Dis. 2000 Mar; 181(3):912-20.
- Review Co-formulated abacavir-lamivudine-zidovudine for initial treatment of HIV infection and AIDS.[Cochrane Database Syst Rev. 2013]Review Co-formulated abacavir-lamivudine-zidovudine for initial treatment of HIV infection and AIDS.Shey MS, Kongnyuy EJ, Alobwede SM, Wiysonge CS. Cochrane Database Syst Rev. 2013 Mar 28; 2013(3):CD005481. Epub 2013 Mar 28.
- Substitution of nevirapine, efavirenz, or abacavir for protease inhibitors in patients with human immunodeficiency virus infection.[N Engl J Med. 2003]Substitution of nevirapine, efavirenz, or abacavir for protease inhibitors in patients with human immunodeficiency virus infection.Martínez E, Arnaiz JA, Podzamczer D, Dalmau D, Ribera E, Domingo P, Knobel H, Riera M, Pedrol E, Force L, et al. N Engl J Med. 2003 Sep 11; 349(11):1036-46.
- Review Abacavir: a review of its clinical potential in patients with HIV infection.[Drugs. 2000]Review Abacavir: a review of its clinical potential in patients with HIV infection.Hervey PS, Perry CM. Drugs. 2000 Aug; 60(2):447-79.
- Review Zidovudine.[LiverTox: Clinical and Researc...]Review Zidovudine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Abacavir - LiverToxAbacavir - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...