NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Committee to Review WIC Food Packages. Review of WIC Food Packages: Improving Balance and Choice: Final Report. Washington (DC): National Academies Press (US); 2017 May 1.
The first major changes to the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food packages in 35 years were recommended by the Institute of Medicine (IOM) in 2006 and implemented by state agencies in 2009 as a result of the U. S. Department of Agriculture's Food and Nutrition Service (USDA-FNS) 2007 interim regulation. Since then, there have also been numerous changes in the WIC environment. This chapter presents a review of changes in the food packages themselves as well as the numerous other changes that have occurred since 2006 and that could potentially affect any updates to the WIC food packages. These include changes in the number and types of WIC participants, economic factors such as participants' food expenditures and the costs of the program, and dietary guidance. Also included here is a description of the experience of WIC participants today. The chapter concludes with a summary of key findings and conclusions reached by the committee upon examination of the evidence described throughout the chapter.
ADAPTATION TO THE WIC FOOD PACKAGE CHANGES PROPOSED IN 2006
A description of the WIC food package changes implemented in response to the 2006 IOM recommendations is provided in Chapter 1 and in Appendix C, Table C-1. Although the 2006 recommendations were based on the best science available, a number of research activities have been undertaken since then to continue to evaluate the impact of WIC generally and the food package changes specifically. As described in Appendix E, Table E-1, USDA-sponsored investigators have studied changes in the behavior of vendors, the availability of vegetables and fruits for purchase with the cash value voucher (CVV), the availability of foods in new sizes, and the pattern of household-level food purchases. The information presented below and throughout this chapter is based on key findings from these and other studies.
Challenges to Implementation of the 2009 Food Package Changes
Implementation of the 2009 food packages involved challenges at the federal, state, and local agency levels, as well as for vendors and manufacturers. A summary of the key challenges and actions taken to resolve these challenges is presented in Table 2-1 and described in detail in the phase I report (NASEM, 2016). For the most part, these challenges have since been overcome, but they remain relevant to consider in future rounds of food package revisions.
At the state agency level, notable challenges included production and distribution of the 1-pound loaf of bread, dealing with the “dangling quart” of milk, changes to container sizes available in the marketplace (e.g., juice and peanut butter), and implementation of the CVV (a description of the CVV is provided in Chapter 1). But along with these challenges, as noted in Chapter 1, a key benefit of the 2009 food package changes, finalized in 2014, was the ability for states to tailor packages (USDA/FNS, 2007a). Although the additional options led to some inconsistencies in specific foods available from state to state, it enabled state administrators to make decisions that maximize the suitability of the foods for their own population and that also contain costs. For example, the Final Rule allows children ages 12 to 24 months to receive fat-reduced milks if overweight or obesity is a concern (USDA/FNS, 2014a). As of 2015, 72 percent of WIC state agencies had adopted this option, covering 60 percent of WIC participants (USDA/FNS, 2015A).
At the vendor level, despite challenges to ensuring WIC foods were available, most evidence suggests that the food package revisions were beneficial for vendors, increasing both sales and profitability for the items offered in the revised food package (Andreyeva et al., 2011) and increasing sales of newly eligible food items to non-WIC customers (Gittelsohn et al., 2012). However, the revised food packages were designed to be cost-neutral to WIC. Thus, while sales apparently increased from WIC foods for some items (reduced-fat milk, whole grains, fruits, and vegetables), sales likely decreased for others (whole milk, juice) (Andreyeva et al., 2013a; Andreyeva and Luedicke, 2013b, 2014). Although some vendors reported difficulty finding and maintaining suppliers for some foods, available evidence finds that prices for these items did not increase, suggesting that vendors adjusted their supply quantities without incurring increased costs (Zenk et al., 2014).
At the local level, results from multiple studies have documented the effect of WIC nutrition education on participant knowledge, attitudes, and behavior change (USDA/ERS, 2007; Kavanagh et al., 2008; Ritchie et al., 2010; USDA/FNS, 2010; Sullivan et al., 2011; Whaley et al., 2012a,b; Hildebrand et al., 2014; Isbell et al., 2014; USDA/FNS, 2016c). A few of these studies have examined the effects of nutrition education on participant adaptation to the 2009 food package changes in particular. In California, Ritchie et al. (2010) demonstrated that nutrition education alone led to increased consumption of low-fat milk and whole grains even before the 2009 changes to the WIC food packages. Following the change, consumption of these foods increased further (Whaley et al., 2012b). A study of the effect of the 2009 breastfeeding food package change on rates of breastfeeding demonstrated significant increases in exclusive breastfeeding in the 6 months prior to the policy change when staff training and participant education focused on the upcoming policy changes (Whaley et al., 2012a). Similar changes were not evident in other states where staff training and participant education specific to the breastfeeding food package changes were not a focus prior to the food package change. Together, these studies suggest that achieving the intended health impact of the WIC food packages and 2009 revisions is facilitated by staff training and participant education.
Finally, the electronic benefit transfer (EBT) system is designed to enhance efficiency across the program by limiting purchases to only those foods authorized by the program. However, the linked databases that code “WIC-approved” foods must be updated continually in response to changes in the marketplace, which poses an administrative burden. USDA-FNS is in the process of developing a nationally representative Universal Product Code (UPC) database in collaboration with states, which should help to alleviate some of this burden. Because WIC benefits are grouped by EBT systems at the household rather than individual level, an additional benefit of the EBT system is the flexibility it allows in food acquisition when more than one family member is a WIC participant. Another vendor-level benefit of the EBT system was demonstrated by Phillips et al. (2014), who reported that EBT implementation both improved the ability of vendors to track inventory and stabilized inventory because participants were able to make purchases throughout the month instead of during a single visit. In addition, vendor reimbursement occurred more quickly.
CHANGES IN THE WIC-PARTICIPATING POPULATION
This section provides an overview of key characteristics of the WIC-participating population and changes since 2006. Specifically, the committee examined participation rates, demographics (including income and employment status), expenditures of the WIC-participating population on food, and breastfeeding trends of the WIC-participating population compared to the U.S. population generally.
WIC Participation Rates
Although the national WIC caseload increased between 2006 and 2010 (see Figure 2-1), reaching a peak of approximately 9 million in 2010, participation declined thereafter to approximately 8 million by 2014 and continued to decline into 2015 (USDA/ERS, 2015a). The year 2014 marked the fourth consecutive year—and only the fourth year in the program's history—that participation for women, infants, and children all fell (see Figure 2-2). In parallel, between fiscal years (FYs) 2013 and 2014, overall expenditures across USDA nutrition assistance programs decreased 5 percent and participation in the Supplemental Nutrition Assistance Program (SNAP) and the National School Lunch Program decreased by 2 and 1 percent, respectively. However, during the same period, participation in the School Breakfast Program and the number of meals served in the Child and Adult Care Food Program both increased by 2 percent (USDA/ERS, 2015b).
The reasons for the overall decline in WIC participation since 2010 are unclear, but the decline may be at least partially attributable to decreasing U.S. birthrates, as well as to the nation's improving economic health. From 2007 to 2009, the United States experienced an economic downturn that may have caused more individuals to have incomes low enough to ensure eligibility for WIC. During the recession, Medicaid, SNAP, and Temporary Assistance for Needy Families (TANF), experienced increases in participation and received increased funding through the American Recovery and Reinvestment Act of 2009 (KFF, 2009, 2015; CBO, 2012; EOPUS, 2014). Participants in these programs who meet WIC age and physiological state criteria are automatically eligible for WIC. Not only has the country been experiencing a still-incomplete recovery from the recession that began in 2008, but other recent changes in Medicaid, SNAP, and TANF may have affected WIC eligibility and participation as well. Additionally, between October 1 and 16, 2013, the federal government experienced a shutdown, which resulted in a gap in funding for the WIC program at the beginning of the fiscal year. Although most states maintained WIC services, some offered modified services; program recovery was slow in some states, lasting up to a year.
In addition to these demographic and economic changes that may have influenced WIC participation between 2010 and 2015, the committee considered whether the food package changes initially implemented in 2009 may have contributed as well. To do this, the committee used state-level data on participation and the number eligible for WIC from 2006–2012 (USDA/FNS, 2011a, 2013, 2014b, 2015b; Bitler and Hoynes, 2013). The analysis considered the effects of national trends, time invariant state factors, the date of implementation of the new food package, unemployment rate, births per capita, and participation in TANF/SNAP/Unemployment Insurance (UI). Details of the estimation method are discussed in Appendix F. The results suggest no significant difference between participation before versus after implementation of the new food packages. The estimated effect was not statistically significant, and it was small in magnitude.
Demographics of the WIC-Participating Population
WIC Participation by Age and Physiological State
The proportion of WIC participants varies among women by physiologic state and among children by age, but this proportion has remained relatively stable since 2006 (see Table 2-2). Data from 2012 indicate that 63 percent of individuals eligible for WIC nationwide participated in the program (USDA/FNS, 2015b). This includes 85 percent of eligible infants, 53 percent of eligible children, 71 percent of eligible pregnant women, and 77 percent of eligible postpartum women (USDA/FNS, 2015b). The majority of women who participate in WIC are pregnant. Of the remaining women, approximately half are breastfeeding and half are postpartum but not breastfeeding. More than half of infants are fully formula-fed. Of the remaining infants, approximately half are fully and half are partially breastfed. The majority of WIC participants are children (53 percent in 2014) (USDA/FNS, 2015c). Many eligible children discontinue participation after 1 year of age (USDA/FNS, 2011a), although the specific reasons for this behavior are unknown.
Racial and Ethnic Composition of the WIC-Participating Population
WIC serves a population with a diverse racial and ethnic composition, and this composition, based on major race and ethnicity categories, has not changed more than 3 percent between 2006 and 2014 (USDA/FNS, 2007a, 2015c) (see Figures 2-3a and 2-3b). Of note in the figures below, the percentage of WIC participants who reported being white increased between 2006 and 2014 by a few percentage points (see Figure 2-3a), yet the percentage of Hispanic/Latino participants remained the same despite an increase in proportions of Hispanic people in the U.S. population (see Figure 2-3b) (USCB, 2011). There was also a decrease in the percentage of WIC participants who reported being American Indian and Alaskan Native between 2006 and 2014. The U.S. population has increased 9 percent since 2005, with the greatest contributions to population growth from immigration, temporary and permanent residency, and other population shifts (DHS, 2014). According to the U.S. Census Bureau, the majority of growth in the U.S. population from 2000 to 2010 resulted from an increase in Hispanic and Asian populations (USCB, 2011). The 2010 American Community Survey found that 92 percent of the U.S. Hispanic population comprises 10 subgroups, with the top three being Mexican, Puerto Rican, and Cuban (Motel and Patten, 2012). Although there are no available national data on racial and ethnic subgroups in the WIC-participating population, these subgroup proportions likely reflect a national trend.
Income Distribution
The WIC-participating population is exceptionally poor compared to the general U.S. population. WIC household income is generally much lower than the qualifying income requirement of not more than 185 percent of the federal poverty-to-income ratio. In 2014, 74 percent of all WIC participants reported incomes at or below federal poverty guideline, with 38 percent reporting incomes equal to or less than 50 percent of the Federal poverty guideline (USDA/FNS, 2015c). This 74 percent figure represents an increase from 2006, when 67 percent of WIC participants had household incomes that fell at or below the federal poverty guideline (USDA/FNS, 2007b).
Employment Status of WIC Participants
Although data on the employment status of WIC participants were not available to the committee, U.S. Census Bureau data for 2014 indicate that 20 percent of working women (15.2 million women) were below 185 percent of poverty. Forty-one percent of these women were working full-time (6.2 million), and 59 percent were working part-time (9.0 million) (USCB, 2015). The number of low-income working families in the United States rose from 10.2 million in 2010 to 10.4 million in 2011 (Roberts et al., 2013). In 2012, 39 percent of these families were headed by working mothers (Povich et al., 2014). Among all families, the share of low-income, female-headed working families increased from 54 percent in 2007 to 58 percent in 2012 (Povich et al., 2014).
Data from the American Time Use Survey (2003–2011) indicate that full-time employment appears to be associated with significantly reduced time spent preparing food (Sliwa et al., 2015). Data from the same survey (2006–2008) show that lower income and the presence of young children are both associated with significantly more time spent in food preparation (Senia et al., 2014). A smaller study of more than 2,000 mothers in Minnesota supports this finding, and indicates that those with full-time employment spent less time on food preparation and consumed fewer vegetables and fruits compared to mothers with part-time or no employment (Bauer et al., 2012). Working mothers may also experience additional time stress that can affect preparation of healthy meals at home (Jabs and Devine, 2006; Beshara et al., 2010).
Food Expenditures of WIC Participants
The committee was tasked with planning and implementing an analysis of food expenditures for the WIC-participating population using national data. Data from the Food Acquisition and Purchase Survey (FoodAPS) (USDA/ERS, 2015c) were used in phase I to compare household expenditures on total food, food at home, and food away from home among three groups: (1) WIC-participating households, (2) WIC-eligible, nonparticipating households (i.e., households with incomes less than or equal to 185 percent of the poverty-to-income ratio and with a pregnant woman or child less than 5 years old), and (3) WIC-ineligible, nonparticipating households (i.e., households with incomes greater than 185 percent of the poverty-to-income ratio) with a pregnant woman or children less than 5 years of age (NASEM, 2016).1
These data also allow for examination of detailed expenditures by WIC-participating households for specific WIC food categories. As described in further detail in Chapter 10 of the phase I report (NASEM, 2016), FoodAPS is a nationally representative, stratified sampling of 4,826 households from April 2012 through January 2013. Data on food expenditures were collected over a 7-day period, with all household members asked to track and report their food purchases or acquisitions during the survey week. Information on each “event” (i.e., purchase or acquisition) included whether the food was purchased or acquired at home or away from home, total expenditure, and source of payment (i.e., specifically whether the event included use of payment with a WIC voucher and, if so, the amount of payment allotted to WIC items). Although in most cases it was not possible to know exactly which foods were obtained with the WIC food voucher (because more than one type of tender may have been reported), by examining individual food codes, purchased items could be categorized as WIC food items. Data were weighted using the household weights provided in the FoodAPS documentation.2 Mean food expenditures were compared between WIC-participating households and both types of non-WIC-participating households using t-tests and the Pearson chi-square statistic (Rao and Scott, 1984).3
The analysis of the FoodAPS data provides evidence on the total food expenditures and expenditures on food groups for WIC-participating households to assess the relative contribution of the WIC food packages to their food expenditures. Overall, as shown in Table 2-3 (i.e., updated from Table 10-2 in the phase I report [NASEM, 2016]), the average weekly expenditures for food at home (FAH) for WIC-participating households was $124.20/week, similar to weekly expenditures of WIC-eligible, nonparticipating households ($113.20/week). WIC-participating households had marginally greater (p = 0.10) expenditures on food away from home (FAFH) expenditures ($60.59/week) than those of WIC-eligible, nonparticipating households ($47.06/week). The average value of WIC expenditures for these WIC-participating households was $10.75/week. Among all WIC-participating households (i.e., both those that made WIC purchases during the week and those that did not), this represents 8.8 percent of total FAH expenditures. Among the nearly one-third of WIC-participating households (32.3 percent) that made a purchase with a WIC benefit during the week, WIC expenditures represented 24.3 percent of reported FAH expenditures for that week.
The data also allowed comparison of expenditures for specific WIC food items among the three groups of households. As shown in Table 2-4, the overall average level of expenditures on identified WIC food items ($21.55/week) was significantly larger for WIC-participating households than for eligible non-WIC-participating households ($14.82/week, p = 0.01), and was similar to the average expenditures of the non-WIC-participating households with income greater than 185 percent of the poverty income ratio ($21.31/week). The share of WIC food items in FAH expenditures was higher for WIC-participating households than for the other households (18 percent overall for WIC-participating households, and 13 percent and 13.5 percent of total FAH expenditures for the low-income and higher-income non-WIC-participating households, respectively; p = 0.01). Among households with WIC expenditures during the week (WIC paid >0), expenditures on WIC food items averaged 29 percent of total FAH expenditures. Because WIC-participating households also used other resources to acquire WIC food items, the average value of WIC food items acquired was greater than the value of reported WIC expenditures in the week.4
Also shown in Table 2-4, for most of the identified food items, WIC-participating households spent more than other households. For example, WIC-participating households spent a weekly average of $1.42 on eggs, compared to $0.72 for WIC-eligible, nonparticipating households and $1.00 for non-WIC-participating higher-income households; and WIC-participating households spent $3.98 per week on milk, compared to $3.05 per week for eligible, non-WIC-participating households and $3.88 per week for non-WIC-participating higher- income households. Weekly expenditures on breakfast cereals were close in value across the three groups. WIC-participating households spent less on vegetables and fruits ($1.79/week) than did the other higher-income households ($2.60/week).5
The FoodAPS data show how expenditures on WIC food items were made in the “shopping trip” (event) among the household groups. At the level of purchase and acquisition events, as shown in Table 2-5, the average value of WIC expenditures as a purchase event was $21.74. Expenditures for most WIC food items were larger when WIC vouchers were used at the shopping event (WIC Paid >0) than otherwise (WIC Paid = 0). Compared to when WIC vouchers were used during an event (WIC paid >0) ($15.68/event),6 average spending on identified WIC food items was less when WIC vouchers were not used (WIC paid = 0) ($3.58/event). The same pattern holds for most individual food items. For example, when WIC vouchers were used (WIC paid >0), WIC-participating households spent an average $3.43 on milk during a single shopping trip, compared to, on average, $0.59 when vouchers were not used (WIC paid = 0).7 Among the low income households, WIC-participating households had higher expenditures for infant formula, eggs, and juice in shopping trips (shopping events) compared with other low income households.
The analysis of expenditure patterns among the three groups of households shows that the expenditures of WIC-participating households differ from other households in several ways. In comparison to other eligible households with income less than 185 percent of the poverty-to-income threshold, WIC-participating households spent more on total food expenditures and more on FAFH. Comparable households with higher-income spent more than WIC-participating households both in total and for FAH and FAFH. WIC-participating households spent more on identified WIC food items in a week than did comparable households with income less than 185 percent of the poverty-to-income ratio. The amount spent on identified WIC food items was comparable to the spending level of the higher-income, non-WIC-participating households.
Breastfeeding Trends in the WIC-Participating Population Compared to the U.S. Population
Healthy People 2020's goals for breastfeeding are presented in Table 2-6 (HHS, 2015). In 2011, the U.S. Surgeon General called for action to support these goals, recommending that families, communities, health care centers, and employment sites provide the support necessary for women to initiate and continue breastfeeding (HHS, 2011). To assess progress toward reaching these goals, the U.S. Centers for Disease Control and Prevention (CDC) estimates breastfeeding prevalence across the United States every 2 years, using data from the U.S. National Immunization Survey. The most recent estimates reflect statistics for children born in 2013 and represent survey data from 2014 and 2015 (see Table 2-6). As shown in the table, although the national goal for initiation of breastfeeding has nearly been achieved, goals for duration of breastfeeding have been more challenging to meet (CDC, 2016a). This may result, in part, from differences in breastfeeding behavior related to racial and ethnic groups, maternal education and age, and WIC participation (CDC, 2010).
In addition to varying by income, the proportion of women that breastfeed varies among racial and ethnic groups. In 2009 and 2013, for example, the prevalence of breastfeeding at 6 months was consistently lowest for non-Hispanic African Americans (33 and 39 percent of infants, respectively) and non-Hispanic American Indian/Alaska Native (39 and 41 percent, respectively) and highest for non-Hispanic Asian (86 and 84 percent, respectively) (see Table 2-7). Studies of breastfeeding prevalence in the WIC-participating population show similar variation, with fewer African-American women initiating and sustaining breastfeeding compared to other racial and ethnic groups (Hurley et al., 2008; Marshall et al., 2013; McKinney et al., 2016). The underlying reasons for racial and ethnic differences in breastfeeding prevalence are not well understood at this time, but differences among racial/ethnic groups in ever breastfeeding are now relatively small (from 79 to 99 percent of the proportion of non-Hispanic whites who ever breastfed) (see Figure 2-4). There are much larger differences among racial/ethnic groups in continued breastfeeding at 6 months (from 36 to 111 percent of the proportion of non-Hispanic whites who continued to breastfeed at 6 months) (see Figure 2-4).
In the WIC-participating population, the most recent WIC Participant and Program Characteristics (PC2014) report indicated that, in 2014, 70 percent of infants (served by agencies that provided data) were ever breastfed (USDA/FNS, 2015c). Although other measures of breastfeeding prevalence were available to the committee, the longest time-series for which all-infant and WIC-infant prevalence of breastfeeding could be compared was at 6 months of age (see Figure 2-5) (1971 through 2013 for U.S. infants; 1978–2013 for WIC infants) (Ryan et al., 2002; CDC, 2015). In 2013, all-infant 6-month breastfeeding prevalence was 49 percent, while the WIC-infant estimate was 39 percent. Although a lower proportion of WIC infants were breastfed than those in the general population, the prevalence of breastfeeding in both groups has been increasing since the late 1970s.
Six-month breastfeeding prevalence in the U.S. population has consistently tracked with income. As shown in Table 2-8, from 2008 to 2013, 6-month breastfeeding prevalence ranged from as low as 33 to 38 percent for women under 100 percent of the poverty level to as high as 60 to 70 percent in women at 600 percent or more of the poverty level (CDC, 2016b). Although breastfeeding increased during this time period for women in all income levels, increases between 2008 and 2013 were highest among women with income above 200 percent of the poverty level. Other available data indicate that between 2004 and 2008, breastfeeding prevalence was lower for WIC-participating women compared to WIC-eligible, nonparticipating women, with substantial differences across racial/ethnic groups (CDC, 2010).
Promotion of Breastfeeding in the WIC Program
A number of breastfeeding promotion and support strategies have been in place as part of Healthy People 2020 that may have helped to increase the prevalence of breastfeeding in both WIC-participating and non-WIC-participating populations. These include strategies to increase the proportion of employers that have worksite lactation support programs, reduce the proportion of breastfed newborns that receive formula supplementation within the first 2 days of life, and increase the proportion of live births that occur in facilities that provide recommended care for lactating mothers and their infants (HHS, 2015). The Baby-Friendly Hospital Initiative has been assisting hospitals with meeting these goals (IOM, 2011b; WHO, 2012).
Additionally, since the food package revisions implemented in 2009, there has been a concerted effort within WIC to increase the proportion of women who breastfeed. The committee's phase I review of breastfeeding (see Chapter 7 in NASEM, 2016) found that the 2009 changes to the food package were associated with small improvements in breastfeeding initiation (USDA/FNS, 2011a; Whaley et al., 2012a; Chiasson et al., 2013; Langellier et al., 2014; Joyce and Reeder, 2015). However, it was not possible to determine whether these improvements resulted from the food package changes themselves, the enhanced breastfeeding promotion and support activities begun at about the same time, or both.
As of 1996, states were no longer required to conduct an annual evaluation of breastfeeding promotion and support activities (P.L. 104-193, Personal Responsibility and Work Opportunity Reconciliation Act of 1996). As a result, other than in Whaley et al. (2012a), little information exists as to which specific breastfeeding promotion and support activities within WIC have been the most successful. Implementation of the USDA's Loving Support© program is one way that WIC breastfeeding activities are supported, but implementation varies depending upon available state-level resources.
USDA-FNS Guidance Related to Provision of Infant Formula
Provision of Infant Formula in the First Month
The choice to breastfeed is complex; protection, promotion, and support activities must be in place to ensure success (Pérez-Escamilla and Chapman, 2012; Pérez-Escamilla et al., 2012).8 The introduction of formula during the first weeks after birth is a risk factor for both shorter duration of exclusive and also any breastfeeding (Walker, 2015). In accordance, the most recent WIC breastfeeding guidance issued by USDA-FNS states that the WIC program's intent is that all women be supported to breastfeed exclusively. For women who want to breastfeed, it states: “Infant formula in the first month may only be issued after careful assessment of the mother and infant by staff with breastfeeding training. If it is determined some formula is appropriate for the infant in the first month, the mother should be advised on the appropriate amount of formula to feed the infant” (USDA/FNS, 2016a). The current WIC food packages reflect this guidance. The food packages for breastfed infants from 0–1 month of age have no formula, or (at the state's option) up to one can of powder infant formula in the container size that provides closest to 104 reconstituted fluid ounces on a case-by-case basis. Infants who need more than 104 ounces of formula in the first month (or need any formula in states that do not allow one can) must be issued the fully formula-fed package.
Tailoring the Amounts of Formula Issued
The USDA-FNS guidance document referenced above also advises tailoring of infant formula issuance: “The goal is to provide as minimal an amount of supplemental formula as is needed, while offering counseling and support, in order to help the mother establish and maintain successful milk production” (USDA/FNS, 2016a). The full nutrition benefit is designed to provide close to 100 percent of the nutritional needs of the nonbreastfed infant from birth to 6 months. There are currently limited data available that describe the feeding patterns of women who receive the full nutrition benefit. One study conducted in California (Whaley et al., 2012a) documented that food packages are generally well aligned with actual feeding practices, but there is still some misalignment: 12 percent of mothers who receive the full formula package from 0–6 months reported doing some breastfeeding. This suggests the potential for overfeeding and supports the need for careful assessment of the mother and infant by staff with breastfeeding training to adequately assess the formula needs of all dyads. A larger study of food package alignment with feeding behavior was recently included in the USDA FNS 2016 Research and Evaluation Plan (USDA/FNS, 2016c).
Evidence for the Benefits of Breastfeeding Promotion and Support in WIC
At present, the availability and implementation of breastfeeding support and promotion activities at the state level are highly variable. Some variation is linked to available resources, and some may reflect differing needs of state-specific WIC-participating populations. The best example of these activities in the WIC program is in California, where Whaley et al. (2012a) found that when breastfeeding support and promotion efforts were paired with the new food packages, the proportion of WIC participants who chose to fully breastfeed increased by 86 percent. The specific activities implemented included two statewide campaigns. First, the Healthy Habits for Life campaign was the staff wellness component of the campaign that started 9 months prior to the food package changes and included training materials to help WIC staff make healthy lifestyle changes in preparation for helping WIC participants to make those same changes.9 Second, the Healthy Habits Begin at Birth campaign, started 6 months before the food package changes, focused on pregnant women, postpartum and breastfeeding women, and infants. This helped prepare WIC families for the upcoming food package changes that related to infant feeding, especially breastfeeding and introducing baby foods. The finding that the proportion of women choosing the fully breastfeeding packages started to increase before the actual food package changes, and then increased even more substantially after the changes and have been maintained, suggests that pairing support and educational activities with policy changes has maximal effect on participant behavior change. However, as a result of budget constraints, breastfeeding support resources are not universally available to all women participating in WIC who choose to breastfeed.
Effects of the 2009 Food Package Changes on the Choice to Breastfeed
The food packages implemented in 2009 were designed to encourage exclusive breastfeeding by allowing very limited issuance of infant formula to breastfeeding women in the first 30 days postpartum. States may allow the issuance of one can of formula in the infant's first month of life, but they are not permitted to create food packages that routinely issue formula to breastfeeding women during this period (USDA/FNS, 2014a). Although the intention of this policy was to support breastfeeding in the immediate postpartum period, evidence indicates the policy had an unintended consequence because women had to choose between two options: (1) receive no formula from WIC, or (2) receive the maximum formula allowance provided to nonbreastfeeding mothers. In some states, a third option to receive 1 can of formula is available in the first month. The results of the largest study of the impact of the food package changes on breastfeeding rates showed that there were no changes in breastfeeding initiation that could be attributed to the revised food packages (USDA/FNS, 2011b). Although issuance of the full breastfeeding package (the first option noted above) increased in the first month, there was also an increase in issuance of the full-formula package (the second option noted above) (USDA/FNS, 2011b). The results of this study also indicated that although issuance of the full breastfeeding package was higher in the first month after implementation of the 2009 food packages, the transition of infants out of this package and into a partially breastfeeding or fully formula-feeding package occurred at a significantly faster rate compared to before implementation of the 2009 food packages. Although there is some evidence that the allowance of one can of formula in the first month helps support breastfeeding, data are not available on either the impact of a one-can policy or its breadth of implementation.
Barriers and Incentives to Breastfeeding in the WIC-Participating Population
The committee's phase I report (NASEM, 2016, Chapter 7) covered barriers, motivators and incentives for breastfeeding as well as the effect of the WIC breastfeeding food package on breastfeeding promotion, initiation, and duration among both WIC and low-income populations. Identified barriers to breastfeeding were numerous and included social norms, cultural factors, social structures, employment,10 and biomedical factors (see Table 7-4 in NASEM, 2016), although the influence of each specific barrier on breastfeeding in the WIC-participating population could not be determined.
There is some evidence that breastfeeding promotion and support provided through the WIC program improves breastfeeding initiation (Olson et al., 2010; Whaley et al, 2012a; Haider et al., 2014; Hildebrand et al., 2014) and duration (Bonuck et al., 2005; Olson et al., 2010; Pugh et al., 2010; Chapman et al., 2013; Haider et al., 2014; Reeder et al., 2014). Data are less convincing for the effects of promotion and support on exclusivity of breastfeeding (Anderson et al., 2005, 2007; Bonuck et al., 2005; Hayes et al., 2008; Meehan et al., 2008; Hopkinson and Konefal Gallagher, 2009; Petrova et al., 2009; Sandy et al., 2009; Bunik et al., 2010; Olson et al., 2010; Pugh et al., 2010; Kandiah, 2011; Chapman et al., 2013; Haider et al., 2014; Hildebrand et al., 2014; Howell et al., 2014; Reeder et al., 2014). WIC participants may perceive that the program delivers conflicting messages by supporting breastfeeding while also distributing infant formula at no cost to participants (Holmes et al., 2009).
WIC participation has been associated with a lower proportion of women who initiate breastfeeding and shorter durations of exclusive and any breastfeeding compared to women not participating in WIC (Li et al., 2005; Hendricks et al., 2006; Ryan and Zhou, 2006; Jacknowitz and Tiehen, 2007; Flower et al., 2008; Bunik et al., 2009; Ziol-Guest and Hernandez, 2010; Jensen, 2012; Mao et al., 2012; Marshall et al., 2013; Ma et al., 2014; Bullinger and Gurley-Calvez, 2016; Gregory et al., 2016). However, these findings are dependent upon methodology applied and treatment of selection bias.11 Using variation in food prices as an instrumental variable (as a means of controlling for selection bias), it was reported that WIC participation decreases the proportion of women that exclusively breastfeed by nearly 50 percent (Bullinger and Gurley-Calvez, 2016). Yet, Gregory et al. (2016), using a propensity-matching method, reported that WIC participation was not associated with a lower likelihood of breastfeeding at 3 months and that WIC participants and nonparticipants differed with respect to baseline factors that predict breastfeeding. Both studies used the Infant Feeding Practices II dataset to develop their samples. Evidence on the effect of timing of entry into WIC on these outcomes is not conclusive (Joyce et al., 2008; Ziol-Guest and Hernandez, 2010; Tenfelde et al., 2011; Langellier et al., 2012; Ma and Magnus, 2012; Jacobson et al., 2015; Metallinos-Katsaras et al., 2015).
WIC PROGRAM COSTS OVER TIME
Any changes to the food packages to be recommended by the committee are required to be cost-neutral so the current average food package cost (with adjustments for inflation) can be maintained. Total WIC costs, including Food and Nutrition Services administration, were $6.2 billion in 2015, representing a decrease of almost $1 billion from 2011, when total costs were $7.2 billion. Average per participant monthly food costs have also declined, to $43.37 in 2015, from $46.69 in 2011 (USDA/FNS, 2016b) (see Table 2-9).
Major cost savings are made available to the WIC program through the infant formula rebate system. The total dollar value of rebates received from infant formula manufacturers by WIC state agencies in FY2015 was $1.8 billion, an increase of about $124 million since 2012, when $1.69 billion in rebates were received (USDA/FNS, 2016b) (see Table 2-10).
RELEVANT CHANGES IN THE ENVIRONMENT SINCE 2006: DIETARY PATTERNS, THE FOOD SUPPLY, AND DIETARY GUIDANCE
In this section, changes in the environment since the previous food package review that have implications for the revised food packages are summarized. These include changes in dietary patterns in the U.S. population, an expansion of the variety of foods available in the marketplace, and changes in dietary guidance.
Dietary Patterns of Americans Have Changed
There have been several changes in consumption of food groups by the U.S. population since the 2006 report. Most notably, after decades of increases, mean energy intake decreased significantly between 2003–2004 and 2009–2010 for the U.S. population overall (Ford and Dietz, 2013). Additionally, between 2007–2008 and 2011–2012 (periods immediately before and after the 2009 food package changes), in women 20 years and older, consumption of whole grains increased 34 percent, consumption of seafood low in omega-3 fatty acids increased by 26 percent, and consumption of nuts and seeds increased by 28 percent (see Table 2-11). In contrast, consumption of soy products decreased by 30 percent. Between 2007–2008 and 2011–2012, in children ages 2–5 years, consumption of seafood high in omega-3 doubled, yogurt consumption increased by 83 percent, and consumption of whole grains increased by 46 percent (see Table 2-12). The committee's analysis (see Chapter 4) indicated that, despite these increases, intakes of whole grains and seafood are nonetheless below recommended amounts for both WIC-eligible women and children. Economic Research Service (ERS) data indicate that per capita wheat product consumption (whole grain and refined) has declined since 2000 (USDA/ERS, 2016a), a trend which could be related to consumer interests in lowering carbohydrate intake or in gluten-free products. Although comparison of 2007–2008 and 2011–2012 is provided for discussion, the direction and magnitude of change varies depending upon the survey years compared.
Expansion of the Variety of Foods Available in the Marketplace Since 2006
According to an ERS report on trends in new food products in the United States (USDA/ERS, 2014a), from 2006 to 2010, the share of new products in the categories of fruit and vegetables, dairy products, pasta and rice, and infant food increased while the share of new snack product and beverage introductions decreased. The variety of available fresh fruit has been robust over the past decade, possibly spurred by a greater ethnic diversity of consumers (Bentley and Pérez, 2015). On the other hand, the availability of 100% fruit juice has fallen steadily since its peak in 1977. Availability per capita of 100% orange juice, which accounts for half of the availability all fruit juice in the United States, decreased 54 percent between 1977 and 2012 (Bentley and Pérez, 2015).
The introduction of new-product claims gives some indication of changes in the food supply that result from changes in consumer preferences. In 2010, “no gluten” ranked among the top 10 claims for the first time, with nearly triple the number of products making this claim compared to 2006 (USDA/ERS, 2014a). “Low or no fat” product claims also moved to the top 10 claims for the first time since 2006. From 2006 to 2010, launches of new products with “whole grain” claims doubled worldwide (Oldways Whole Grains Council, 2016).
The Food Supply and the WIC Program
Several recent changes in the U.S. food supply with implications for the revised food packages can be attributed to the influence of WIC itself. For example, since the Child Nutrition and WIC Reauthorization Act of 2004, which included provisions for infant formula manufacturers to bid for state WIC contracts, manufacturers have been bidding for formulas supplemented with the fatty acids docosahexaenoic acid (DHA) and arachidonic acid (ARA).12 When bidding began, these products were relatively new additions to formula options in the marketplace (USDA/ERS, 2011a). At present, nearly all infant formulas sold in the United States are supplemented with DHA and ARA, an indication of WIC's significant influence on the infant formula market (USDA/ERS, 2011a). Another example of WIC's influence on the U.S. food supply is anecdotal evidence suggesting that increased availability of 1-pound loaves of whole wheat bread can be attributed to the addition of this item to the WIC food packages in 2009 (Oliveira and Frazao, 2015).
Changes in Dietary Guidance
The 2006 IOM review of WIC food packages drew on the 2005 Dietary Guidelines for Americans (DGA) (USDA/HHS, 2005). The DGA are updated every 5 years, and since the 2006 review, the 2010 and the 2015–2020 DGA have been issued. As described in the statement of task, the committee was charged with aligning WIC food packages for individuals ages 2 years and older with the most current DGA. Recommendations for infants and children less than 2 years of age draw on the recommendations of the American Academy of Pediatrics (AAP) and other authoritative groups. Changes in dietary guidance since 2005 relevant to the WIC food packages are summarized below.
In addition to these changes, the Dietary Guidelines Advisory Committee reported strong evidence that the seafood industry has rapidly expanded to meet demand and that fisheries are increasingly employing sustainable management strategies to avoid long-term collapse (USDA/HHS, 2015). This is important given WIC's broad reach and recommendations included herein related to fish in the food packages.
Changes to Recommended Food Group Intakes
This review presents an opportunity to improve the alignment of the food packages after two changes in the DGA and after introduction of the 2009 food package changes. Compared to the 2005 DGA (see Table 2-13), the 2010 DGA reorganized the vegetable food group into five subgroups. The recommended food intakes increased for “red-orange vegetables,” “starchy vegetables,” and “beans and peas.” The recommended quantities of “dark-green vegetables” and “other vegetables” decreased. There were no changes in recommended intakes of total fruit, grains, protein foods, or oils. Recommended intakes of dairy foods were slightly increased for two levels of caloric intake. Compared to the 2010 DGA, the 2015–2020 DGA included no changes to the recommended amounts from each of the major food groups or food subgroups, except for small changes to the subgroups of protein foods. In summary, the major change in the DGA since the 2005 edition relevant to this review is the reformulation of the vegetable subgroups. This reformulation has already resulted in the committee's recommendation that WIC participants should be allowed to acquire white potatoes with their CVV (IOM, 2015).
Changes to Food Patterns
The food patterns in the 2010 DGA included templates for several variations in the USDA Food Patterns, including the Dietary Approaches to Stop Hypertension (DASH) Eating Plan, and Mediterranean, vegetarian, and vegan patterns. The 2015–2020 DGA included a healthy U.S.-style, healthy Mediterranean, and healthy vegetarian patterns (USDA/HHS, 2016).
Shortfall Nutrients and Nutrients of Public Health Concern
The 2015–2020 DGA identified nine nutrients (vitamin A, vitamin D, vitamin E, vitamin C, folate, calcium, magnesium, fiber, and potassium) as “shortfall” nutrients, that is, nutrients that are underconsumed relative to Dietary Reference Intake recommendations (see Table 2-14 for a comparison across the 2005, 2010, and 2015–2020 DGA). Calcium, vitamin D, fiber, and potassium were further classified as nutrients of public health concern because their underconsumption has been linked to adverse health outcomes. For adolescent and premenopausal females, iron was also identified as a shortfall nutrient because of risk of iron-deficiency. Compared to the 2010 DGA, the 2015–2020 DGA no longer identified choline and vitamin K in adults, phosphorus in children, and vitamin B12 in adults over 50 as shortfall nutrients. In the 2010 DGA, folate was not identified as a shortfall nutrient, rather a nutrient of concern for women capable of becoming pregnant; the newer guidelines continue to recommend that women of reproductive age supplement a diet rich in vegetables, fruits, and grains with foods enriched with folic acid or that include folic acid supplements. The 2015–2020 DGA still consider iron a nutrient of public health concern.
Limiting Added Sugars, Saturated Fats, and Other Food Components
Both the 2010 DGA (USDA/HHS, 2010) and 2015–2020 DGA (USDA/HHS, 2016) focused on limiting added sugars in the diet, with the 2015–2020 DGA specifically recommending limiting added sugars to no more than 10 percent of total calories. The 2015–2020 DGA also retained the 2010 DGA recommendation to limit saturated fat to no more than 10 percent of total calories. (In the 2010 DGA, a maximum percentage of total energy intake from both saturated fats and added sugars was also provided.) Depending on energy needs, the 2015-2020 DGA specify that recommended limits for energy intakes for added sugars and saturated fats (plus energy from other “calories for other uses” [COU]13) could actually be lower (or greater) than 10 percent. For example, most calories in a 1,200- to 1,800-kcal food pattern are needed to meet nutrient intake needs, leaving less than 10 percent of total calories for other uses (i.e., intake from all COU combined must be less than 10 percent of total calories).
The 2010 DGA recommended that adults up to 50 years of age limit their sodium intake to 2,300 mg per day and that adults 51 years and older, African Americans, and adults with hypertension, diabetes, or chronic kidney disease limit sodium intake to 1,500 mg daily. In contrast, the 2015–2020 DGA recommend a sodium limit of 2,300 mg per day for all adults.
The 2010 DGA recommendation to limit cholesterol was not retained, although the 2015–2020 DGA recommend limiting intake to as little dietary cholesterol as possible while maintaining a healthy eating pattern (USDA/HHS, 2016). This position is consistent with recommendations made by the American College of Cardiology/American Heart Association (ACC/AHA, 2013). Eggs, a primary source of cholesterol in the American diet, are currently included in the WIC food packages for children and women. Amounts were reduced in 2009 primarily to allow room for additional foods and, secondarily, to reduce the total amount of cholesterol in the package (IOM, 2006). Contributions of the WIC foods to COU are further reviewed in Chapter 3.
Changes in Dietary Guidance for Infants and Children Up to 2 Years of Age
Since the 2006 IOM report, minor updates have been made to dietary guidance for individuals less than 2 years of age. In 2008, the AAP issued guidance recommending reduced-fat milks for children over the age of 1 year for whom overweight or obesity are concerns (AAP, 2008). As denoted in the Final Rule, USDA-FNS permits the issuance of reduced-fat milks for children 1 year of age and over who fall into this category (USDA/FNS, 2014a). Also in 2008, the AAP published a statement reporting insufficient data to document a protective effect of any dietary intervention on allergy development beyond 4 to 6 months of age (Greer et al., 2008). Results of the committee's review of current dietary guidance for infants and children up to 2 years of age and alignment of the food packages are presented in Chapter 3.
Updates to Nutrient Intake Recommendations and Evidence for Importance in Growth and Development
The DGA apply the Dietary Reference Intakes (DRI) as the basis for identifying nutrient inadequacies. The DRI are also part of the process used to generate food patterns for specific kcal levels. Since the 2006 review of WIC food packages, the IOM has issued one report updating the DRI for calcium and vitamin D (IOM, 2011a). Also since 2006, the importance of choline, omega-3 fatty acids, and vitamin D in fetal growth and development has become clearer. The evidence for the role of these nutrients was reviewed in more detail in the phase I report (NASEM, 2016, Chapter 6).
THE WIC PARTICIPANT EXPERIENCE TODAY
The WIC participant experience today, illustrated in Figure 2-6, is influenced by a number of factors related both to the food packages themselves and to the WIC environment. These factors include racial and ethnic subgroup differences in food preferences and infant and child feeding practices; behavioral barriers and motivators; environmental and economic factors affecting the availability and access to food; and administrative and vendor challenges associated with the WIC food packages. The committee considered the interplay of these factors to ensure that WIC food packages are culturally suitable, efficient for nationwide distribution, and not burdensome to administer. Details of the committee's review of these components are available in Chapter 2 of the phase I report (NASEM, 2016). Key points from that review are summarized here.
Cultural Variation in Satisfaction with the 2009 Food Package Changes
Multiple studies have documented moderate to high satisfaction with the 2009 changes in the WIC food packages (Gleason and Pooler, 2011; Whaley et al., 2012b; Ishdorj and Capps, 2013; Bertmann et al., 2014; Ritchie et al., 2014). However, evidence also indicates cultural variation in participants' satisfaction with certain types or amounts of food items. Black et al. (2009) conducted interviews and focus groups with WIC participants and caregivers throughout Maryland to assess perceptions of the proposed food package changes and examine differences in food preferences by race and ethnicity. Although food preferences appeared to be similar between non-Hispanic black and non-Hispanic white participants, Hispanic respondents were more likely than non-Hispanic respondents to prefer beans compared to peanut butter and to express dislike for frozen and canned vegetables. In a statewide survey of nearly 3,000 mostly (79 percent) Hispanic WIC participants and caregivers in California, Ritchie et al. (2014) reported that nearly all (91 percent) respondents were satisfied with the new food items introduced (vegetables and fruits, whole grains, and lower-fat milk). Additionally, a higher proportion of primarily Spanish speakers (compared to primarily English speakers) were satisfied with vouchers for whole grains, vouchers for lower-fat milk, and the amount of juice; and a higher proportion of primarily English speakers (compared to primarily Spanish speakers) were satisfied only with the amount of milk and not with the amounts of other foods. Actual consumption of foods was difficult to ascertain. In a quasi-experimental study in northern Illinois, Zenk et al. (2012) found that the availability of fresh fruit and vegetables at authorized WIC retailers increased significantly after the 2009 package changes for African-American culturally specific vegetables and fruits, but not for Latino culturally specific vegetables and fruits.14
Redemption of WIC Foods
In addition to published studies of the acceptability of the 2009 food packages, the committee also examined state data on foods actually purchased (i.e., from states that have implemented the EBT system). A summary of redemption data gathered from a sample of states at various time points between 2012 and 2016 is presented in Table 2-15 (see the table footnotes for time ranges). Available data indicate that redemption was variable for most food categories, but consistently high for infant formula and consistently low for jarred infant meats. For foods provided in more than one food package, it was not possible to determine if redemption was different among food packages. There were not enough data to determine whether states with high concentrations of particular racial and ethnic groups have higher redemption for specific items (e.g., tortillas or beans are common Hispanic staples). Nonetheless, the committee considered possible regional differences in food and substitution preferences in its deliberations.
Barriers to WIC Participation and Redemption
Key barriers to WIC participation and redemption of WIC foods are summarized in Box 2-1, and details of the committee's review are available in Appendix G, Table G-1. Although the quantitative evidence identified by the committee was sufficient to support only an association, not a causal relationship, between these barriers and either participation or redemption, possibilities for maximizing both participation and redemption include: streamlining the registration process (Gilbert et al., 2014), enhancing customer service and reducing wait times for participants (Christie et al., 2006), informing participants of local vendors (Gleason et al., 2014), ensuring culturally-appropriate nutrition messaging (Phillips et al., 2014), enhancing the perceived value of packages (Gleason and Pooler, 2011), and examining the impact of minimum stocking requirements on food availability (Gleason et al., 2011). As the EBT system is implemented nationwide (by 2020), it may remove several of the identified barriers (Phillips et al., 2014).
The WIC Participant Shopping Experience
Although studies are limited, qualitative work among WIC programs nationwide suggests that the participant shopping experience can be another key barrier to participation and redemption of WIC foods. Prior to the food package revisions, a survey administered to parents and caretakers of WIC participants in New York State found that issues with food procurement (store policies, food availability) and the WIC food packages (adequacy, satisfaction with the items) were barriers to participation (Woelfel et al., 2004).15 Several small studies were carried out after implementation of the 2009 food package changes to evaluate the perception and use of the CVV by WIC participants (Christie et al., 2006; Gleason and Pooler, 2011; Najjar, 2013; Bertmann et al., 2014; Gleason et al., 2014). Bertmann et al. (2014) reported that CVVs were inconsistently redeemed in Arizona. They identified the following barriers to redemption: participants' perception of annoyance or anger expressed by cashier or other shoppers; cashiers' lack of training; fluctuation in enforcement of WIC redemption rules from store to store and week to week; and feelings of embarrassment or judgment when using the CVV. The authors cautioned, however, that their findings might not be generalizable to other WIC-participating populations. In a Wisconsin study of WIC participant CVV redemption patterns, Gleason and Pooler (2011) reported positive responses overall to the package changes, but with differences in non-use and maximum use of the CVV among some WIC subpopulations. Some participants described a level of discomfort with having to do math in the store, which the researchers hypothesized may be enough to deter use of the benefits. Additionally, the authors identified several vendor-level challenges, including difficulties in maintaining fresh foods (particularly in smaller stores), anticipating client demand, and having the correct sizes available. Najjar (2013) reported that helpful vendors and both vendor and participant understanding about the use of the CVV can positively affect the WIC shopping experience.
The effect of allowing split tender for CVV purchases (using a different payment method for the amount over the CVV benefit) on redemption has yet to be comprehensively evaluated. Inasmuch as WIC provides vouchers for all other foods based on quantity, not value, WIC participants may pay less attention to food prices when redeeming their vouchers (Hoynes and Schanzenbach, 2015). The CVV, however, is a cash benefit, and purchasing power may vary regionally. In a study of 26 metropolitan market areas, Leibtag and Kumcu (USDA/ERS, 2011b) found that the 20 most commonly purchased vegetables and fruits cost 30 to 70 percent more in the highest-priced compared to the lowest-priced market areas.
WIC Participant Shopping Venues
The types of stores from which WIC benefits are typically redeemed is relevant when considering the availability of WIC foods in specific store types and food package changes that may affect small and large vendors differently. Based on the most recent ERS evaluation (USDA/ERS, 2016c), WIC participants redeem their benefits mostly (77 percent) at large stores (super stores, supermarkets, and large grocery stores). Approximately 63 percent of WIC vendors can be classified as large stores. However, data indicate that the proportion of WIC redemptions at large stores varies by state, ranging from 50 to 99 percent. In some states, smaller stores play a significant role, accounting for as many as 70 percent of WIC retail vendors (Rhode Island) and capturing as much as 50 percent of WIC retail redemptions (California) (USDA/ERS, 2016c). An earlier study (conducted in 2009) which showed a similar focus on large stores indicated that most WIC participants used their vouchers and did most other food shopping at the same store (84 percent); reasons provided for shopping at a different store for WIC foods included convenience (44 percent) and cost (32 percent) (USDA/FNS, 2012).
Although Ford and Dzewaltowski (2010) found that WIC mothers had access to many food stores within a 3-mile radius of their home, whether residing in a micropolitan or metropolitan area, and a recent study of SNAP and WIC-participating households using nationally representative data from USDA's National Household Food Acquisition and Purchase Survey (FoodAPS) indicated that the nearest store was an average of 2.0 miles from the household, the same FoodAPS data also indicated that the store primarily used for grocery shopping was, on average, 3.4 miles from the household (USDA/ERS, 2015). FoodAPS also indicated that the vast majority (88 percent) of WIC-participating households accessed grocery stores using their own vehicle, and 7 percent of WIC-participating households reported walking, biking, using public transport, shuttle, delivery, or some other form of transportation (USDA/ERS, 2015d).
Availability of WIC Foods
Several research groups have examined the effects of the 2009 changes to the WIC food packages on food availability and, therefore, access to WIC foods. Studies comparing vendor inventory before versus after the 2009 changes in Illinois (Zenk et al., 2012), Connecticut (Andreyeva et al., 2011), Baltimore, Maryland (Cobb et al., 2015), Hartford, Connecticut (Havens et al., 2012), and New Orleans, Louisiana (O'Malley et al., 2014; Rose et al., 2014) have indicated improved availability of fruits, vegetables, lower-fat milks, juices, jarred infant vegetables and fruits, and/or whole grains among WIC vendors. Cobb et al. (2015) found that both becoming WIC-authorized and the WIC policy change itself were associated with significant increases in WIC-relevant “healthy food availability”16 scores. Havens et al. (2012) likewise reported improvements in “healthy food supply”17 scores among WIC convenience and grocery stores, although the improvements varied from 16 percent in higher-income neighborhoods to 39 percent in lower-income areas. A systematic review of four studies confirmed overall improved availability of WIC foods at WIC-authorized vendors (Schultz et al., 2015). Andreyeva et al. (2011) and Zenk et al. (2014) noted some carryover in improved availability to stores that did not participate in WIC, possibly attributable to changes in the food supply chain.
Nationwide Distribution and Costs of Food
As part of its consideration of changes to the food packages, the committee evaluated information on the cost and national distribution of foods (including to low-income neighborhoods). The purpose of this evaluation was to ensure that foods in the revised packages are accessible to WIC participants living in different geographic areas of the United States, including both rural and urban areas. The committee factored into its considerations seasonal variability in food availability, pricing (including regional price differences and price variability of product substitutions), the impact of shelf stability on nationwide distribution, vendor requirements for inventory turnover limits of perishable food products, and types of vendors in different locales (e.g., supermarket versus trading post). Although most WIC redemptions occur at large stores, some participants may have access primarily to smaller vendors, so all store sizes were important to consider (USDA/ERS, 2016c).
KEY FINDINGS AND CONCLUSIONS
This chapter includes a review of the many WIC programmatic and other environmental changes of relevance to the review of food packages. Table 2-16 summarizes the key findings and conclusions reached by the committee upon examination of the evidence described in this chapter.
REFERENCES
- AAP (American Academy of Pediatrics) Committee on Nutrition. Lipid screening and cardiovascular health in childhood. Pediatrics. 2008;122(1):198–208. [PubMed: 18596007]
- ACC/AHA (American College of Cardiology/American Heart Association). Guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. 2013. [November 6, 2016]. http://circ
.ahajournals .org/content/circulationaha /early/2013/11/11/01 .cir.0000437738 .63853.7a.full.pdf. [PubMed: 24222016] - Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Changes in access to healthy foods after implementation of the WIC food package revisions. Washington, DC: USDA/ERS; 2011.
- Andreyeva T, Luedicke J, Middleton AE, Long MW, Schwartz MB. Positive influence of the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages on access to healthy foods. Journal of the Academy of Nutrition Dietetics. 2012;112(6):850–858. [PubMed: 22709812]
- Andreyeva T, Luedicke J, Tripp AS, Henderson KE. Effects of reduced juice allowances in food packages for the Women, Infants, and Children program. Pediatrics. 2013a;131(5):919–927. [PMC free article: PMC4074658] [PubMed: 23629613]
- Andreyeva T, Luedicke J. Federal food package revisions: Effects on purchases of whole-grain products. American Journal of Preventive Medicine. 2013b;45(4):422–429. [PubMed: 24050418]
- Andreyeva T, Luedicke J, Henderson KE, Schwartz MB. The positive effects of the revised milk and cheese allowances in the Special Supplemental Nutrition Program for Women, Infants, and Children. Journal of the Academy of Nutrition and Dietetics. 2014;114(4):622–630. [PubMed: 24210878]
- Bauer KW, Hearst MO, Escoto K, Berge JM, Neumark-Sztainer D. Parental employment and work-family stress: Associations with family food environments. Social Science and Medicine. 2012;75(3):496–504. [PMC free article: PMC3586574] [PubMed: 22591825]
- Bentley J, Pérez A. Fresh fruit makes up a growing share of U.S. fruit availability. USDA/ERS; 2015. [December 21, 2016]. https://www
.ers.usda .gov/amber-waves/2015 /may/fresh-fruit-makes-up-a-growing-share-of-us-fruit-availability. - Bertmann FM, Barroso C, Ohri-Vachaspati P, Hampl JS, Sell K, Wharton CM. Women, infants, and children cash value voucher (CVV) use in Arizona: A qualitative exploration of barriers and strategies related to fruit and vegetable purchases. Journal of Nutrition Education and Behavior. 2014;46(3 Suppl):S53–S58. [PubMed: 24809997]
- Beshara M, Hutchinson A, Wilson C. Preparing meals under time stress. The experience of working mothers. Appetite. 2010;55(3):695–700. [PubMed: 20937335]
- Bitler M, Hoynes H. The more things change, the more they stay the same? The safety net and poverty in the great recession. Journal of Labor Economics (working paper). 2013 [CrossRef]
- Black MM, Hurley KM, Oberlander SE, Hager ER, McGill AE, White NT, Quigg AM. Participants' comments on changes in the revised Special Supplemental Nutrition Program for Women, Infants, and Children food packages: The Maryland Food Preference Study. Journal of the American Dietetic Association. 2009;109(1):116–123. [PubMed: 19103331]
- Bonuck KA, Freeman K, Trombley M. Country of origin and race/ethnicity: Impact on breastfeeding intentions. Journal of Human Lactation. 2005;21(3):320–326. [PubMed: 16113020]
- Bullinger LR, Gurley-Calvez T. WIC participation and maternal behavior: Breastfeeding and work leave. Contemporary Economic Policy. 2016;34(1):158–172.
- Bunik M, Krebs NF, Beaty B, McClatchey M, Olds DL. Breastfeeding and WIC enrollment in the Nurse Family Partnership program. Breastfeeding Medicine. 2009;4(3):145–149. [PMC free article: PMC6463997] [PubMed: 19243262]
- Bunik M, Shobe P, O'Connor ME, Beaty B, Langendoerfer S, Crane L, Kempe A. Are 2 weeks of daily breastfeeding support insufficient to overcome the influences of formula? Academic Pediatrics. 2010;10(1):21–28. [PubMed: 20129478]
- CBO (Congressional Budget Office). The Supplemental Nutrition Assistance Program. Washington, DC: Congressional Budget Office; 2012. [December 21, 2016]. https://www
.cbo.gov/sites /default/files/cbofiles /attachments/04-19-SNAP.pdf. - CDC (Centers for Disease Control and Prevention). Racial and ethnic differences in breastfeeding initiation and duration, by state—National Immunization Survey, United States, 2004-2008. Morbidity and Mortality Weekly Report. 2010;59(11):327–334. [PubMed: 20339344]
- CDC. Nutrition, physical activity and obesity data, trends and maps web site. 2015. [December 21, 2016]. https://nccd
.cdc.gov/NPAO_DTM. - CDC. Breastfeeding report card. 2016a. [December 21, 2016]. https://www
.cdc.gov/breastfeeding /pdf/2016breastfeedingreportcard.pdf. - CDC. National Immunization Survey (NIS). 2016b. [October 14, 2016]. https://www
.cdc.gov/breastfeeding /data/nis_data/index.htm. - Chapman DJ, Morel K, Bermudez-Millan A, Young S, Damio G, Pérez-Escamilla R. Breastfeeding education and support trial for overweight and obese women: A randomized trial. Pediatrics. 2013;131(1):e162–e170. [PMC free article: PMC3529944] [PubMed: 23209111]
- Chiasson MA, Findley SE, Sekhobo JP, Scheinmann R, Edmunds LS, Faly AS, McLeod NJ. Changing WIC changes what children eat. Obesity (Silver Spring). 2013;21(7):1423–1429. [PubMed: 23703806]
- Christie C, Watkins JA, Martin A, Jackson H, Perkin JE, Fraser J. Assessment of client satisfaction in six urban WIC clinics. Florida Public Health Review. 2006;3:35–42.
- Cobb LK, Anderson CAM, Appel L, Jones-Smith J, Bilal U, Gittelsohn J, Franco M. Baltimore city stores increased the availability of healthy food after WIC policy change. Health Affairs. 2015;34(11):1849–1857. [PubMed: 26526242]
- DHS (U.S. Department of Homeland Security). 2013 yearbook of immigration statistics. Washington, DC: U.S. Department of Homeland Security, Office of Immigration Statistics; 2014.
- Dunn RL, Kalich KA, Fedrizzi R, Phillips S. Barriers and contributors to breastfeeding in WIC mothers: A social ecological perspective. Breastfeeding Medicine. 2015;10(10):493–501. [PubMed: 26565749]
- EOPUS (Executive Office of the President of the United States). The economic impact of the American Recovery and Reinvestment Act five years later: Final report to Congress. 2014. [December 21, 2016]. https://www
.whitehouse .gov/sites/default /files/docs/cea_arra_report.pdf. - Flower KB, Willoughby M, Cadigan RJ, Perrin EM, Randolph G. Understanding breastfeeding initiation and continuation in rural communities: A combined qualitative/quantitative approach. Maternal and Child Health Journal. 2008;12(3):402–414. [PMC free article: PMC2692345] [PubMed: 17636458]
- Ford PB, Dzewaltowski DA. Limited supermarket availability is not associated with obesity risk among participants in the Kansas WIC program. Obesity (Silver Spring). 2010;18(10):1944–1951. [PubMed: 20057363]
- Ford ES, Dietz WH. Trends in energy intake among adults in the United States: Findings from NHANES. American Journal of Clinical Nutrition. 2013;97(4):848–853. [PMC free article: PMC4598942] [PubMed: 23426032]
- Gilbert D, Nanda J, Paige D. Securing the safety net: Concurrent participation in income eligible assistance programs. Maternal and Child Health Journal. 2014;18(3):604–612. [PubMed: 23771236]
- Gittelsohn J, Laska MN, Andreyeva T, Foster G, Rose D, Tester J, Lee SH, Zenk SN, Odoms-Young A, McCoy T, Ayala GX. Small retailer perspectives of the 2009 women, infants and children program food package changes. American Journal of Health Behavior. 2012;36(5):655–665. [PMC free article: PMC4703098] [PubMed: 22584093]
- Gleason S, Pooler J. The effects of changes in WIC food packages on redemptions: Final report. Altarum Institute; 2011. [December 21, 2016]. http://naldc
.nal.usda .gov/download/50613/PDF. - Gleason S, Morgan R, Bell L, Pooler J. Impact of the revised WIC food package on small WIC vendors: Insight from a four-state evaluation. Altarum Institute; 2011. [December 21, 2016]. http://www
.calwic.org /storage/FourStateWICFoodPackageEvaluation-Full _Report-20May11.pdf. - Gleason S, McGuire D, Morgan R. Opportunities to enhance American Indian access to the WIC food package: Evidence from three case studies. Altarum Institute; 2014. [December 21, 2016]. http://altarum
.org/sites /default/files/uploaded-publication-files /Opportunities%20to %20Enhance%20Am%20Indian %20Access%20to %20the%20WIC%20FP_fmt_04.pdf. - Greer FR, Sicherer SH, Burks AW., American Academy of Pediatrics Committee on Nutrition. Effects of early nutritional interventions on the development of atopic disease in infants and children: The role of maternal dietary restriction, breastfeeding, timing of introduction of complementary foods, and hydrolyzed formulas. Pediatrics. 2008;121(1):183–191. [PubMed: 18166574]
- Gregory EF, Gross SM, Nguyen TQ, Butz AM, Johnson SB. WIC participation and breastfeeding at 3 months postpartum. Maternal and Child Health Journal. 2016;20(8):1735–1744. [PMC free article: PMC4936931] [PubMed: 26994607]
- Haider SJ, Chang LV, Bolton TA, Gold JG, Olson BH. An evaluation of the effects of a breastfeeding support program on health outcomes. Health Services Research. 2014;49(6):2017–2034. [PMC free article: PMC4254137] [PubMed: 25039793]
- Havens EK, Martin KS, Yan J, Dauser-Forrest D, Ferris AM. Federal nutrition program changes and healthy food availability. American Journal of Preventive Medicine. 2012;43(4):419–422. [PubMed: 22992360]
- Hayes DK, Prince CB, Espinueva V, Fuddy LJ, Li R, Grummer-Strawn LM. Comparison of manual and electric breast pumps among WIC women returning to work or school in Hawaii. Breastfeeding Medicine. 2008;3(1):3–10. [PubMed: 18333763]
- Hendricks K, Briefel R, Novak T, Ziegler P. Maternal and child characteristics associated with infant and toddler feeding practices. Journal of the American Dietetic Association. 2006;106(1 Suppl 1):S135–S148. [PubMed: 16376637]
- HHS (U.S. Department of Health and Human Services). The Surgeon General's call to action to support breastfeeding. 2011. [December 21, 2016]. http://www
.surgeongeneral .gov/library/calls /breastfeeding/calltoactiontosupportbreastfeeding.pdf. - HHS. Healthy People 2020: Maternal, infant, and child health objectives. 2015. [December 21, 2016]. https://www
.healthypeople .gov/2020/topics-objectives /topic/maternal-infant-and-child-health /objectives. - Hildebrand DA, McCarthy P, Tipton D, Merriman C, Schrank M, Newport M. Innovative use of influential prenatal counseling may improve breastfeeding initiation rates among WIC participants. Journal of Nutrition Education and Behavior. 2014;46(6):458–466. [PubMed: 24998174]
- Holmes AV, Chin NP, Kaczorowski J, Howard CR. A barrier to exclusive breastfeeding for WIC enrollees: Limited use of exclusive breastfeeding food package for mothers. Breastfeeding Medicine. 2009;4(1):25–30. [PubMed: 19196037]
- Hopkinson J, Konefal Gallagher M. Assignment to a hospital-based breastfeeding clinic and exclusive breastfeeding among immigrant Hispanic mothers: A randomized, controlled trial. Journal of Human Lactation. 2009;25(3):287–296. [PubMed: 19436060]
- Howell EA, Bodnar-Deren S, Balbierz A, Parides M, Bickell N. An intervention to extend breastfeeding among black and Latina mothers after delivery. American Journal of Obstetrics and Gynecology. 2014;210(3):239.e1–239.e5. [PMC free article: PMC3938878] [PubMed: 24262719]
- Hoynes H, Schanzenbach DW. U.S. food and nutrition programs. 2015. [October 26, 2016]. http://www
.nber.org/chapters/c13488.pdf. - Hurley KM, Black MM, Papas MA, Quigg AM. Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low-income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Maternal and Child Nutrition. 2008;4(2):95–105. [PMC free article: PMC6860842] [PubMed: 18336643]
- IOM (Institute of Medicine). WIC food packages: Time for a change. Washington, DC: The National Academies Press; 2006.
- IOM. Dietary Reference Intakes for calcium and vitamin D. Washington, DC: The National Academies Press; 2011a. [PubMed: 21796828]
- IOM. Early childhood obesity prevention policies. Washington, DC: The National Academies Press; 2011b. [PMC free article: PMC3262615] [PubMed: 22332102]
- IOM. Review of WIC food packages: An evaluation of white potatoes in the cash value voucher: Letter report. Washington, DC: The National Academies Press; 2015. [PMC free article: PMC4642435] [PubMed: 26567207]
- Isbell MG, Seth JG, Atwood RD, Ray TC. A client-centered nutrition education model: Lessons learned from Texas WIC. Journal of Nutrition Education and Behavior. 2014;46(1):54–61. [PubMed: 24188801]
- Ishdorj A, Capps O. The effect of revised WIC food packages on native American children. American Journal of Agricultural Economics. 2013;95(5):1266–1272.
- Jabs J, Devine CM. Time scarcity and food choices: An overview. Appetite. 2006;47(2):196–204. [PubMed: 16698116]
- Jacknowitz A, Tiehen L. Transitions into and out of the WIC program: A cause for concern? Social Service Review. 2007;83(2):151–183.
- Jacobson LT, Twumasi-Ankrah P, Redmond ML, Ablah E, Hines RB, Johnston J, Collins TC. Characteristics associated with breastfeeding behaviors among urban versus rural women enrolled in the Kansas WIC program. Maternal and Child Health Journal. 2015;19(4):828–839. [PubMed: 25047788]
- Jensen E. Participation in the Supplemental Nutrition Program for Women, Infants and Children (WIC) and breastfeeding: National, regional, and state level analyses. Maternal and Child Health Journal. 2012;16(3):624–631. [PubMed: 21505775]
- Joyce T, Reeder J. Changes in breastfeeding among WIC participants following implementation of the new food package. Maternal and Child Health Journal. 2015;19(4):868–876. [PubMed: 25095768]
- Joyce T, Racine A, Yunzal-Butler C. Reassessing the WIC effect: Evidence from the Pregnancy Nutrition Surveillance System. Journal of Policy Analysis and Management. 2008;27(2):277–303. [PubMed: 18401924]
- Kandiah J. Teaching new mothers about infant feeding cues may increase breastfeeding duration. Food and Nutrition Sciences. 2011;2(4):259–264.
- Kavanagh KF, Cohen RJ, Heinig MJ, Dewey KG. Educational intervention to modify bottle-feeding behaviors among formula-feeding mothers in the WIC program: Impact on infant formula intake and weight gain. Journal of Nutrition Education and Behavior. 2008;40(4):244–250. [PubMed: 18565465]
- KFF (Henry J. Kaiser Family Foundation). A foundation for health reform: Findings of a 50 state survey of eligibility rules, enrollment and renewal procedures, and cost-sharing practices in Medicaid and CHIP for children and parents during 2009. Washington, DC: Henry J. Kaiser Family Foundation; 2009. [December 21, 2016]. https:
//kaiserfamilyfoundation .files.wordpress .com/2013/01/8028.pdf. - KFF. Medicaid financing: How does it work and what are the implications? Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2015. [December 21, 2016]. http://files
.kff.org /attachment/issue-brief-medicaid-financing-how-does-it-work-and-what-are-the-implications. - Langellier BA, Pia Chaparro M, Whaley SE. Social and institutional factors that affect breastfeeding duration among WIC participants in Los Angeles County, California. Maternal and Child Health Journal. 2012;16(9):1887–1895. [PubMed: 22205423]
- Langellier BA, Chaparro MP, Wang MC, Koleilat M, Whaley SE. The new food package and breastfeeding outcomes among women, infants, and children participants in Los Angeles County. American Journal of Public Health. 2014;104(Suppl 1):S112–S118. [PMC free article: PMC4011093] [PubMed: 24354843]
- Li R, Darling N, Maurice E, Barker L, Grummer-Strawn LM. Breastfeeding rates in the United States by characteristics of the child, mother, or family: The 2002 National Immunization Survey. Pediatrics. 2005;115(1):e31–e37. [PubMed: 15579667]
- Ma P, Magnus JH. Exploring the concept of positive deviance related to breastfeeding initiation in black and white WIC enrolled first time mothers. Maternal and Child Health Journal. 2012;16(8):1583–1593. [PubMed: 21822964]
- Ma X, Liu J, Smith M. WIC participation and breastfeeding in South Carolina: Updates from prams 2009-2010. Maternal and Child Health Journal. 2014;18(5):1271–1279. [PubMed: 24057992]
- Mao CY, Narang S, Lopreiato J. Breastfeeding practices in military families: A 12-month prospective population-based study in the national capital region. Military Medicine. 2012;177(2):229–234. [PubMed: 22360072]
- Marshall C, Gavin L, Bish C, Winter A, Williams L, Wesley M, Zhang L. WIC participation and breastfeeding among white and black mothers: Data from Mississippi. Maternal and Child Health Journal. 2013;17(10):1784–1792. [PubMed: 23203317]
- McKinney CO, Hahn-Holbrook J, Chase-Lansdale PL, Ramey SL, Krohn J, Reed-Vance M, Raju TN, Shalowitz MU., Community Child Health Research Network. Racial and ethnic differences in breastfeeding. Pediatrics. 2016;138(2) [PMC free article: PMC4960721] [PubMed: 27405771]
- Meehan K, Harrison GG, Afifi AA, Nickel N, Jenks E, Ramirez A. The association between an electric pump loan program and the timing of requests for formula by working mothers in WIC. Journal of Human Lactation. 2008;24(2):150–158. [PubMed: 18436966]
- Metallinos-Katsaras E, Brown L, Colchamiro R. Maternal WIC participation improves breastfeeding rates: A statewide analysis of WIC participants. Maternal and Child Health Journal. 2015;19(1):136–143. [PubMed: 24777674]
- Motel S, Patten E. The 10 largest Hispanic origin groups: Characteristics, rankings, top counties. Washington, DC: Pew Research Center; 2012.
- Najjar S. Master's thesis. Seattle: University of Washington, School of Public Health; 2013. Barriers to WIC benefits redemption among participants in Washington State.
- NASEM (National Academies of Sciences, Engineering, and Medicine). Review of WIC food packages: Proposed framework for revisions: Interim report. Washington, DC: The National Academies Press; 2016. [PubMed: 27512745] [CrossRef]
- Oldways Whole Grain Council. Whole grain statistics. 2016. [December 21, 2016]. http:
//wholegrainscouncil .org/newsroom/whole-grain-statistics. - Oliveira V, Frazao E. Painting a more complete picture of WIC: How WIC impacts nonparticipants. USDA/ERS; 2015. [December 21, 2016]. https://www
.ers.usda .gov/amber-waves/2015 /april/painting-a-more-complete-picture-of-wic-how-wic-impacts-nonparticipants. - Olson BH, Haider SJ, Vangjel L, Bolton TA, Gold JG. A quasi-experimental evaluation of a breastfeeding support program for low income women in Michigan. Maternal and Child Health Journal. 2010;14(1):86–93. [PubMed: 19082697]
- O'Malley K, Luckett BG, Dunaway LF, Bodor JN, Rose D. Use of a new availability index to evaluate the effect of policy changes to the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) on the food environment in New Orleans. Public Health Nutrition. 2015;18(1):25–32. [PMC free article: PMC10270924] [PubMed: 24762525]
- Pérez-Escamilla R, Chapman DJ. Breastfeeding protection, promotion, and support in the United States: A time to nudge, a time to measure. Journal of Human Lactation. 2012;28(2):118–121. [PubMed: 22526338]
- Pérez-Escamilla R, Curry L, Minhas D, Taylor L, Bradley E. Scaling up of breastfeeding promotion programs in low- and middle-income countries: The “breastfeeding gear” model. Advances in Nutrition. 2012;3(6):790–800. [PMC free article: PMC3648703] [PubMed: 23153733]
- Petrova A, Ayers C, Stechna S, Gerling JA, Mehta R. Effectiveness of exclusive breastfeeding promotion in low-income mothers: A randomized controlled study. Breastfeeding Medicine. 2009;4(2):63–69. [PubMed: 19239405]
- Phillips D, Bell L, Morgan R, Pooler J. Transition to EBT in WIC: Review of impact and examination of participant redemption patterns: Final report. Altarum Institute; 2014. [December 21, 2016]. http://altarum
.org/sites /default/files/uploaded-publication-files /Altarum_Transition %20to%20WIC%20EBT_Final %20Report_071614.pdf. - Povich D, Roberts B, Mather M. Low-income working mothers and state policy: Investing for a better economic future. Chevy Chase, MD: The Working Poor Families Project; 2014.
- Pugh LC, Serwint JR, Frick KD, Nanda JP, Sharps PW, Spatz DL, Milligan RA. A randomized controlled community-based trial to improve breastfeeding rates among urban low-income mothers. Academic Pediatrics. 2010;10(1):14–20. [PMC free article: PMC2818063] [PubMed: 19854119]
- Rao JNK, Scott AJ. On Chi-squared tests for multiway contingency tables with cell proportions estimated from survey data. Annals of Statistics. 1984;12(1):46–60.
- Reeder JA, Joyce T, Sibley K, Arnold D, Altindag O. Telephone peer counseling of breastfeeding among WIC participants: A randomized controlled trial. Pediatrics. 2014;134(3):e700–e709. [PMC free article: PMC4143999] [PubMed: 25092936]
- Ritchie LD, Whaley SE, Spector P, Gomez J, Crawford PB. Favorable impact of nutrition education on California WIC families. Journal of Nutrition Education and Behavior. 2010;42(3 Suppl):S2–S10. [PubMed: 20399405]
- Ritchie LD, Whaley SE, Crocker NJ. Satisfaction of California WIC participants with food package changes. Journal of Nutrition Education and Behavior. 2014;46(3 Suppl):S71–S78. [PubMed: 24810000]
- Roberts B, Povich D, Mather M. Low-income working families: The growing economic gap. Chevy Chase, MD: The Working Poor Families Project; 2013.
- Rose D, O'Malley K, Dunaway LF, Bodor JN. The influence of the WIC food package changes on the retail food environment in New Orleans. Journal of Nutrition Education and Behavior. 2014;46(3 Suppl):S38–S44. [PubMed: 24809995]
- Ryan AS. More about the Ross Mothers Survey. Pediatrics. 2005;115(5):1450–1451. [PubMed: 15867081]
- Ryan AS, Zhou W. Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978-2003. Pediatrics. 2006;117(4):1136–1146. [PubMed: 16585308]
- Ryan A, Wenjun Z, Acosta A. Breastfeeding continues to increase into the new millennium. Pediatrics. 2002;11(6):1103–1109. [PubMed: 12456906]
- Sandy JM, Anisfeld E, Ramirez E. Effects of a prenatal intervention on breastfeeding initiation rates in a Latina immigrant sample. Journal of Human Lactation. 2009;25(4):404–411. quiz 458-459. [PubMed: 19487705]
- Schultz DJ, Byker Shanks C, Houghtaling B. The impact of the 2009 Special Supplemental Nutrition Program for Women, Infants, and Children food package revisions on participants: A systematic review. Journal of the Academy of Nutrition and Dietetics. 2015;115(11):1832–1846. [PubMed: 26276067]
- Senia MC, Jensen HH, Zhylyevskyy O. Time in eating and food preparation among single adults. Review of Economics of the Household. 2014:1–34. [CrossRef]
- Sliwa SA, Must A, Perea F, Economos CD. Maternal employment, acculturation, and time spent in food-related behaviors among Hispanic mothers in the United States. Evidence from the American Time Use Survey. Appetite. 2015;87:10–19. [PubMed: 25451579]
- Sullivan EM, Bignell WE, Andrianos A, Anderson AK. Impact of education and training on type of care provided by community-based breastfeeding counselors: A cross-sectional study. International Breastfeeding Journal. 2011;6:12. [PMC free article: PMC3177880] [PubMed: 21871062]
- Tenfelde S, Finnegan L, Hill PD. Predictors of breastfeeding exclusivity in a WIC sample. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2011;40(2):179–189. [PubMed: 21314715]
- Tisone CA, Guerra SA, Lu W, McKyer EL, Ory M, Dowdy D, Wang S, Miao J, Evans A, Hoelscher DM. Food-shopping environment disparities in Texas WIC vendors: A pilot study. American Journal of Health Behavior. 2014;38(5):726–736. [PubMed: 24933142]
- USCB (U.S. Census Bureau). Overview of race and Hispanic origin: 2010. 2011. [December 21, 2016]. http://www
.census.gov /content/dam/Census /library/publications /2011/dec/c2010br-02.pdf. - USCB. Population clock. 2015. [December 21, 2016]. http://www
.census.gov. - USDA (U.S. Department of Agriculture). Beans and peas are unique foods. 2015. [August 29, 2016]. https://www
.choosemyplate .gov/vegetables-beans-and-peas. - USDA/ARS (U.S. Department of Agriculture/Agricultural Research Service). What we eat in America, NHANES 2005-2012. Beltsville, MD: USDA/ARS; 2005-2012. [December 21, 2016]. http://www
.cdc.gov/nchs/nhanes/wweia.htm. - USDA/ARS. Food patterns equivalents database 2011-2012: Methodology and user guide. Beltsville, MD: USDA/ARS; 2014. [December 21, 2016]. http://www
.ars.usda.gov /SP2UserFiles/Place /80400530/pdf/fped/FPED_1112.pdf. - USDA/ERS (U.S. Department of Agriculture/Economic Research Service). Could behavioral economics help improve diet quality for nutrition assistance program participants? Washington, DC: USDA/ERS; 2007. [December 21, 2016]. http://ben
.cornell.edu/pdfs/USDA-BeEcon .pdf. - USDA/ERS. The infant formula market. Consequences of a change in contract brand. Washington, DC: USDA/ERS; 2011a. [January 30, 2017]. https://www
.ers.usda .gov/webdocs/publications /err124/6918_err124.pdf?v=41056. - USDA/ERS. The WIC fruit and vegetable cash voucher: Does regional price variation affect buying power? Washington, DC: USDA/ERS; 2011b. [March 2, 2015]. http://www
.ers.usda.gov /media/127579/eib75.pdf. - USDA/ERS. Cost containment in the WIC program: Vendor peer groups and reimbursement rates. Washington, DC: USDA/ERS; 2014a. [December 21, 2016]. https://www
.ers.usda .gov/webdocs/publications /err171/48701_err171_summary.pdf. - USDA/ERS. Transition to EBT in WIC: Review of impact and examination of participant redemption patterns: Final report. Altarum Institute; 2014b. [December 21, 2016]. http://altarum
.org/sites /default/files/uploaded-publication-files /Altarum_Transition %20to%20WIC%20EBT_Final %20Report_071614.pdf. - USDA/ERS. The WIC program: Background, trends, and economic issues. 2015th ed. Washington, DC: USDA/ERS; 2015a. [December 21, 2016]. https://www
.aap.org/en-us /advocacy-and-policy /federal-advocacy /Documents/USDAWIC2015Report.pdf. - USDA/ERS. The food assistance landscape FY 2014 annual report. Washington, DC: USDA/ERS; 2015b. [November 7, 2016]. http://www
.ers.usda.gov /webdocs/publications /eib137/52406_eib137_summary.pdf. - USDA/ERS. FoodAPS national household Food Acquisition and Purchase Survey. Washington, DC: USDA/ERS; 2015c. [December 21, 2016]. http://www
.ers.usda.gov /data-products/foodaps-nationalhousehold-food-acquisition-and-purchase-survey.aspx. - USDA/ERS. Where do Americans shop for food and how do they travel to get there? Washington, DC: USDA/ERS; 2015d. [January 30, 2017]. https://www
.ers.usda .gov/webdocs/publications /eib138/eib138_errata.pdf?v=42636. - USDA/ERS. Wheat's role in the U.S. diet has changed over the decades. Washington, DC: USDA/ERS; 2016a. [December 21, 2016]. http://www
.ers.usda.gov /topics/crops/wheat /wheats-role-in-the-us-diet.aspx. - USDA/ERS. National household food acquisition and purchase survey (FoodAPS). User's guide to survey design, data collection, and overview of datasets. 2016b. [December 21, 2016]. http://www
.ers.usda.gov /webdocs/DataFiles /FoodAPS_National_Household _Food_Acquisition _and_Purchase_Survey_17984 //53285_UserGuideFoodAPS.pdf. - USDA/ERS. Where do WIC participants redeem their food benefits? An analysis of WIC food dollar redemption patterns by store type. Washington, DC: USDA/ERS; 2016c. [November 7, 2016]. http://www
.ers.usda.gov /webdocs/publications /eib152/57246_eib152.pdf. - USDA/FNS (U.S. Department of Agriculture/Food and Nutrition Research Service). Interim Rule, 7 C.F.R. § 246. Alexandria, VA: USDA/FNS; 2007a. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC food packages;
- USDA/FNS. WIC participant and program characteristics 2006. Alexandria, VA: USDA/FNS; 2007b. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files/pc2006.pdf. - USDA/FNS. WIC participant and program characteristics 2008. Alexandria, VA: USDA/FNS; 2010. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files/pc2008_0.pdf. - USDA/FNS. National and state-level estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibles and program reach, 2000-2009. Alexandria, VA: USDA/FNS; 2011a.
- USDA/FNS. Evaluation of the birth month breastfeeding changes to the WIC food packages. Alexandria, VA: USDA/FNS; 2011b. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files/BirthMonth.pdf. - USDA/FNS. National survey of WIC participants II. Alexandria, VA: USDA/FNS; 2012. [December 21, 2016]. http://www
.fns.usda.gov /national-survey-wic-participants-ii. - USDA/FNS. National and state-level estimates of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibles and program reach, 2010. Alexandria, VA: USDA/FNS; 2013. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files /WICEligibles2010Vol1.pdf. - USDA/FNS. Final Rule, 7 C.F.R. § 246. 2014a. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Revisions in the WIC food packages;
- USDA/FNS. National and state-level estimates of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibles and program reach, 2011, Vol I. Alexandria, VA: USDA/FNS; 2014b. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files /WICEligibles2011Volume1.pdf. - USDA/FNS. WIC food packages policy options II, final report. Alexandria, VA: USDA/FNS; 2015a. [December 21, 2016]. http://www
.fns.usda.gov /wic-food-package-policy-options-ii. - USDA/FNS. National and state-level estimates of the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) eligibles and program reach, 2012, Vol I. Alexandria, VA: USDA/FNS; 2015b. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files /ops/WICEligibles2012-Volume1.pdf. - USDA/FNS. WIC participant and program characteristics 2014: Final report. Alexandria, VA: USDA/FNS; 2015c. [December 21, 2016]. http://www
.fns.usda.gov /sites/default/files/ops/WICPC2014 .pdf. - USDA/FNS. Special Supplemental Nutrition Program for Women, Infants and Children (WIC): Food package policy and guidance. Alexandria, VA: USDA/FNS; 2016a. [August 26, 2016]. http://www
.fns.usda.gov /sites/default/files /wic/WIC-Food-Package-Policy-Guidance.pdf. [PubMed: 27008717] - USDA/FNS. WIC program. Alexandria, VA: USDA/FNS; 2016b. [July 13, 2016]. http://www
.fns.usda.gov/pd/wic-program. - USDA/FNS. Food and Nutrition Service Research and Evaluation Plan—Fiscal Year 2016. Alexandria, VA: USDA/FNS; 2016c. [September 16, 2016]. http://www
.fns.usda.gov /sites/default/files /ops/studyand-evaluation-plan-2016 .pdf. - USDA/HHS (U.S. Department of Agriculture/U.S. Department of Health and Human Services). Dietary Guidelines for Americans 2005. U.S. Government Printing Office; 2005. [December 21, 2016]. http://www
.health.gov /dietaryguidelines/dga2005 /document/pdf/DGA2005.pdf. - USDA/HHS. Dietary Guidelines for Americans 2010. U.S. Government Printing Office; 2010. [December 21, 2016]. http://www
.health.gov /dietaryguidelines/dga2010 /dietaryguidelines2010.pdf. - USDA/HHS. The report of the Dietary Guidelines Advisory Committee on the Dietary Guidelines for Americans, 2015, to the Secretary of Agriculture and the Secretary of Health and Human Services. USDA/HHS; 2015. [December 21, 2016]. http://www
.health.gov /dietaryguidelines/2015scientific-report /PDFs/Scientific-Report-of-the-2015-Dietary-Guidelines-AdvisoryCommittee.pdf. - USDA/HHS. Dietary Guidelines for Americans 2015. U.S. Government Printing Office; 2016. [August 29, 2016]. https://health
.gov/dietaryguidelines /2015. - Walker M. Formula supplementation of breastfed infants: Helpful or hazardous? ICAN: Infant, Child, & Adolescent Nutrition. 2015;7(4):198–207.
- Whaley SE, Koleilat M, Whaley M, Gomez J, Meehan K, Saluja K. Impact of policy changes on infant feeding decisions among low-income women participating in the Special Supplemental Nutrition Program for Women, Infants, and Children. American Journal of Public Health. 2012a;102(12):2269–2273. [PMC free article: PMC3519334] [PubMed: 23078467]
- Whaley SE, Ritchie LD, Spector P, Gomez J. Revised WIC food package improves diets of WIC families. Journal of Nutrition Education and Behavior. 2012b;44(3):204–209. [PubMed: 22406013]
- WHO (World Health Organization). Baby-friendly hospital initiative. World Health Organization; 2012. [December 21, 2016]. http://www
.who.int/nutrition /topics/bfhi/en. - Woelfel ML, Abusabha R, Pruzek R, Stratton H, Chen SG, Edmunds LS. Barriers to the use of WIC services. Journal of the American Dietetic Association. 2004;104(5):736–743. [PubMed: 15127057]
- Zenk SN, Odoms-Young A, Powell LM, Campbell RT, Block D, Chavez N, Krauss RC, Strode S, Armbruster J. Fruit and vegetable availability and selection: Federal food package revisions, 2009. American Journal of Preventive Medicine. 2012;43(4):423–428. [PubMed: 22992361]
- Zenk SN, Powell LM, Odoms-Young AM, Krauss R, Fitzgibbon ML, Block D, Campbell RT. Impact of the revised Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) food package policy on fruit and vegetable prices. Journal of the Academy of Nutrition and Dietetics. 2014;114(2):288–296. [PMC free article: PMC4084875] [PubMed: 24183996]
- Ziol-Guest KM, Hernandez DC. First- and second-trimester WIC participation is associated with lower rates of breastfeeding and early introduction of cow's milk during infancy. Journal of the American Dietetic Association. 2010;110(5):702–709. [PubMed: 20430131]
Footnotes
- 1
Significant differences detected in these comparisons cannot necessarily be attributed to WIC participation.
- 2
All standard errors account for oversampling and the complex survey design of FoodAPS Sampling weights were constructed based on the FoodAPS survey stratification of households with the survey target groups determined by SNAP receipt and poverty status, and used to produce estimates that are nationally representative of U.S. households. To apply sampling weights, the committee used the svyset command in STATA (a data analysis and statistical software package) and followed guidance in FoodAPS Users Guide (USDA/ERS, 2016b).
- 3
These data were generated under contract with the Center for Agricultural and Rural Development at Iowa State University, then checked by committee members.
- 4
This could also be due to misclassification of some items as WIC-qualifying when in fact they are not. The misclassification errors would be similar across the household categories.
- 5
The amount reported here as “vegetables and fruits” includes processed vegetables and fruits (with “food codes”).
- 6
For purchase events when WIC was used (WIC Paid >0), the analysis captured only 81 percent of the reported total WIC value spent. Possible reasons to explain why the sum of item expenses differs from the reported total WIC expenditures include the fact that not all items have a reported expenditure or imputed expenditure. This would include some of the WIC items in our calculations, including vegetables and fruits purchased with a CVV.
- 7
Of note is the relatively low value of expenditures on vegetables and fruits during WIC shopping events ($0.10), compared to what participants redeemed when vouchers were not used ($0.45). The very small value recorded for expenditures on vegetables and fruits when WIC benefits were used in the event (WIC Paid >0) may reflect misreporting of the vegetables and fruits expenditures when using the CVV. Underreporting and misclassification of food expenditures acquired with WIC benefits would mean that the total amount of WIC expenditures is underestimated.
- 8
The committee recognizes that some women are unable to breastfeed fully.
- 9
A full description of the Healthy Habits campaigns can be found at https://www
.cdph.ca.gov /programs/wicworks /Pages/WICHealthyHabits2009.aspx (accessed December 19, 2016). - 10
Following the release of the phase I report, the literature search update identified additional references. In Dunn et al. (2015), employment status was significantly associated with breastfeeding duration. Over half of women breastfeeding for 6 months or longer were not employed full time or part time.
- 11
See Chapter 4 for a discussion of selection bias.
- 12
There were some state/alliance bids that specified DHA/ARA formula products as early as 2002 (see https://ideas
.repec.org /p/sda/workpa/12008.html, accessed December 19, 2016). - 13
In the 2015–2020 DGA, calories from added sugars and saturated fat, along with calories from added refined starch, as well as additional calories from the recommended food groups, and alcohol, are termed “calories for other uses” (COU). In the 2010 DGA, calories from added sugars, saturated fats, and alcohol were termed “discretionary calories.”
- 14
See Appendix G, Table G-2, for detail from Zenk et al. (2012).
- 15
Although this study fell outside the committee's search parameters for publication year, the committee considered its findings to be particularly applicable.
- 16
The “healthy food availability” scores, ranging from 0 to 27 points, that were allotted based on the presence and number of varieties available of the following items: fruit (4 points), vegetables (4 points), low-fat milk (1 point), lean beef and chicken (4 points), healthy frozen meals (1 point), whole-wheat bread (4 points), low-sodium alternatives (2 points), and low-sugar cereal (2 points) as well as the relative shelf space of healthy versus unhealthy alternatives of milk and frozen food (Cobb et al., 2015).
- 17
The “healthy food supply” score was a composite of data on availability, variety, quality, and prices of foods including cow's milk; soy milk; tofu; fresh, canned, and frozen fruit and vegetables; canned sardines and salmon; whole-grain bread and tortillas; brown rice; and whole-grain cereals (Andreyeva et al., 2012).
Figures
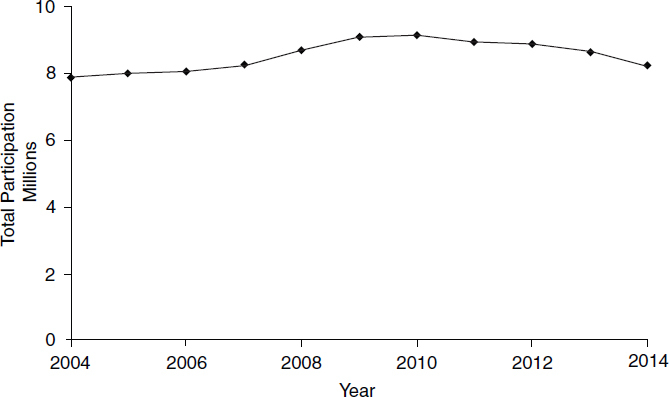
FIGURE 2-1Annual number of participants in the WIC program constructed from monthly averages of participants, FY2004–2015
NOTES: FY2014 is the latest complete data. Data for FY2015 may be incomplete.
SOURCE: USDA/FNS, 2016b.

FIGURE 2-2Average annual WIC participation by participant category, 2004–2014
NOTE: No participation data were available for 2005, 2007, or 2009.
SOURCES: USDA/FNS, 2007b, 2010, 2015b.

FIGURE 2-3bDistribution of ethnicity of WIC participants, 2006 and 2014
SOURCES: USDA/FNS, 2007b, 2015c.

FIGURE 2-4Breastfeeding prevalence by racial/ethnic group expressed as a percentage of values for non-Hispanic whites: United States, 2013
SOURCE: HHS, 2015.

FIGURE 2-5Six-month breastfeeding prevalence: 1971–2013
NOTES: Data exclusively for WIC eligible, nonparticipants were not available. Therefore, the comparison of all infants to WIC infants is an underestimate of the difference of interest, namely WIC nonparticipants vs. WIC-participating infants. Two data sources were used to construct this time series: the Ross Laboratories Mothers' Survey (Ryan et al., 2002) and the Centers for Disease Control and Prevention (CDC, 2015). The Ross Laboratories Mothers' Survey is a large national survey conducted by Ross Laboratories, a manufacturer of infant formula. Ross sent questionnaires each month to a sample of mothers. Nearly 1 million surveys were sent annually in the 1990s (Ryan, 2005). For example, in 1996, 744,000 questionnaires were mailed (Ryan et al., 2002). Data for 1971 to 1999 are from the Ross Mothers' Survey. Line breaks indicate missing data.
SOURCES: Ryan et al., 2002; CDC, 2015.
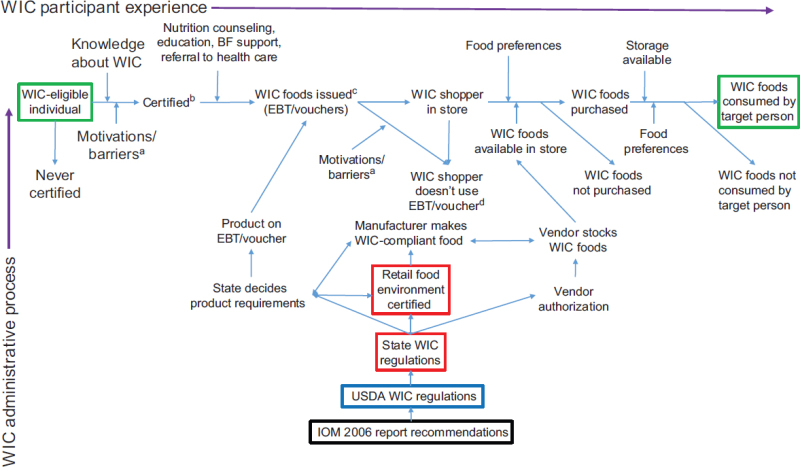
FIGURE 2-6Overview of the WIC program administrative and participant processes
Legislative mandates may also affect WIC regulations.
NOTES: This figure is a theoretical representation; it does not consider effects of other individual or household resources.
a Potential participant barriers may include lack of access to transportation to the WIC site and/or the vendor, time required to visit a WIC site, inconvenient WIC clinic hours, lack of knowledge about the program, or lack of preference for WIC foods, among other barriers.
b Certification for WIC requires the individual to be categorically eligible (pregnant, postpartum woman, infant, child up to age 5), meet income eligibility guidelines (<185 percent of the federal poverty level), provide proof of residence in the state where benefits are issued and have a nutritional risk. Women certified during pregnancy are certified for the duration of pregnancy plus up to 6 weeks postpartum. Postpartum recertification following the birth of the infant is for either 6 months (if not breastfeeding) or 12 months (if breastfeeding), after which time the mother is no longer eligible for WIC. In the case of a fetal or pregnancy loss, women remain eligible and can be recertified for the program for 6 months after the end of the pregnancy. Beginning in 2013, the Federal Rule gave states the discretion to certify infants and children for either a 6- or 12-month period (USDA/FNS, 2015b). As of this writing, certification periods for infants and children are 6 or 12 months depending on state-level decisions. The need for the participant to visit the program site for recertification is not illustrated in this diagram.
c EBT benefits/food vouchers are valid for a 1-month period. States have the discretion to decide whether the 1-month benefit period is a calendar month (e.g., June 1–30) or a rolling month based on the date of benefit issuance (e.g., June 20–July 19). For an individual who is certified, up-to-date on all required documentation, and has no high-risk conditions, benefits can be issued for up to a 3-month period. This means that, although WIC foods are issued for a 1-month period, a participant may be issued up to 3 months of benefits at one visit. Only the current month of benefits can be used immediately. The remaining benefits issued for use in future month(s) must be retained and used only in the future month(s). Valid dates for future month benefits are printed on the voucher or included on the EBT receipt. The need for the participant to visit the program site to obtain EBT benefits/food vouchers is not illustrated in this diagram.
d Significant lack of redemption or under-redemption of a WIC food is information used by WIC state agencies to make decisions about available products. This feedback loop is not represented in this diagram.
Tables
TABLE 2-1Challenges to Implementation of the 2009 Food Package Revisions
| Stakeholder | Challenge | Resolution |
|---|---|---|
| Federal | Dangling quart: after substitution options, a quart of milk remained, creating a stocking challenge for vendors | Yogurt substitution option in place of the “dangling quart”; states are permitted to authorize purchase of quart sizes of milk (USDA/FNS, 2014a) |
| Container size: change in sizes of peanut butter from 18 to 16 ounces, and in some juices from 64 to 59 ounces | Permission for state authorization of different sizes as approved by USDA-FNSa (USDA/FNS, 2016a) | |
| CVV: A new food instrument based on a fixed cash value | Permission for “split tender” so that participants can cover any overage with cash (USDA/FNS, 2014a) | |
| Federal/State | CVV: A new food instrument based on a cash value; difficult for participants to select an amount of produce that exactly matched the value | Education to staff, participants, and vendors |
| State agency | CVV in lieu of jarred infant food vegetables and fruits (currently fresh only) for infants 9 to 11 months of age; difficult if states offer canned, frozen, or dried vegetables and fruits for other participants | No resolution; some states have not implemented the option because of Management Information System limitations |
| EBT: requires development of a database for WIC-approved foods | Established strategies by early EBT adopters, a model for later adopters; development of a national UPC database is required for state use (P.L. 111-296, Healthy, Hunger-Free Kids Act of 2010) | |
| Cost containment: balancing with diversity and availability of foods | Not fully resolved: rebates contain costs, but limit program ability to support breastfeeding; cost-containment may limit vendors, brands, sizes, forms, or prices (e.g. “least expensive brand”b requirements) | |
| Container size: change in sizes of peanut butter from 18 to 16 ounces, and in some juices from 64 to 59 ounces and in some juices from 64 to 59 ounces | Permission for state authorization of different sizes as approved by USDA-FNS | |
| Local agency | Introduction of new foods or changes to foods | Staff and participant education |
| Vendor | Requirement in the Final Rule to stock at least two different fruits and two different vegetables | Vendors' choice of less perishable options or canned/frozen varieties if the state authorizes canned, frozen, or dried options (USDA/FNS, 2015a) |
| Stocking the specific size; maintaining freshness (Gleason et al., 2011) | Higher prices for WIC foods (Tisone et al., 2014; USDA/ERS, 2014a) | |
| Difficulty finding distributors and suppliers for specific food items (Andreyeva et al., 2011; Gittelsohn et al., 2012) | ND | |
| Manufacturer | Specific size or product with the WIC food specification not available | At higher cost, modified production streams to manufacture the required product; or prohibitive cost so the product is not manufacturedc |
NOTES: CVV = cash value voucher; EBT = electronic benefit transfer; ND = No data are available as to whether this continues to be a challenge; UPC = Universal Product Code; USDA-FNS = U.S. Department of Agriculture's Food and Nutrition Service.
- a
States are permitted to authorize different sizes only if there is limited availability of the prescribed specified size and nutritional integrity is not compromised (see USDA/FNS, 2016a).
- b
The “least expensive brand” requirement is a strategy selected by some states by which participants are directed to the products that are the least expensive among all products offered by that store that meet WIC specifications.
- c
Personal communication, National Pasta Association, July 16, 2015. Report is available in the public access file for this study (Email: paro@nas
.edu). SOURCES: As cited in the table.
TABLE 2-2Participation of Women and Children in WIC by Physiological State or Feeding Mode, FY2005–2006 and 2015–2016
| Group or Subgroup | April 2006 | 2015–2016 | ||||
|---|---|---|---|---|---|---|
| Number of Participants Nationwide | Proportion of the WIC-Participating Population (%) | Number of Participants Nationwide | Proportion of the WIC-Participating Population (%) | |||
| Of Women | Of All WIC Participants | Of Women | Of All WIC Participants | |||
| Nationwide | 8,772,217 | 8,023,742 | ||||
| Total women | 2,205,594 | — | 25 | 1,923,171 | — | 24 |
| Pregnant women | 986,433 | 45 | 11 | 772,151 | 40 | 10 |
| Postpartum women | 634,372 | 29 | 7 | 557,464 | 29 | 7 |
| Partially BF women | NR | — | — | 345,371 | 18 | 4 |
| Fully BF women | NR | — | — | 248,186 | 13 | 3 |
| BF women | 584,789 | 27 Of Infants | 7 Of All WIC Participants | 593,557 | 31 Of Infants | 7 Of All WIC Participants |
| Total infants | 2,272,626 | — | 26 | 1,939,740 | — | 24 |
| FF infants | NR | — | — | 1,340,943 | 69 | 17 |
| Partially BF infants | NR | — | — | 349,113 | 18 | 4 |
| Fully BF infants | NR | — | — | 249,684 | 13 | 3 |
| Total children | 4,293,997 | — | 49 | 4,160,832 | — | 52 |
NOTES: BF = breastfeeding/breastfed; FF = formula-fed; NR = not reported.
SOURCES: USDA/FNS, 2007b, 2016b.
TABLE 2-3Summary Statistics for Weekly Food Expenditures for WIC-Participating and Other Households
| Expenditure Variable | Mean Weekly Expenditures in Dollars (SE) | ||
|---|---|---|---|
| WIC-Participating Households (N = 461) | Non-WIC, Income ≤185% PIR (Pregnant, or Child <5 years) (N = 306) | Non-WIC, Income >185% PIR (Pregnant, or Child <5 years) (N = 241) | |
| Food Expenditures (1 week) | |||
| Total food expenditures ($) | 184.78 (10.33) | 160.21 (10.66)b | 242.46 (15.45)a |
| Food at home (FAH) ($) | 124.20 (6.12) | 113.20 (8.10) | 164.14 (13.09)a |
| Food away from home (FAFH) ($) | 60.59 (6.6) | 47.06 (4.92)b | 7 8.33 (6.35)b |
| WIC Expenditure Patterns (1 week) | |||
| % of households using WIC in week (% of total) | 32.3 (3.8) | ||
| Average value of WIC expenditures in week ($) | 10.75 (1.82) | ||
| WIC expenditures as share of total food expenditures (all WIC-participating households) (%) | 5.8 (0.9) | ||
| WIC expenditures as share of total FAH expenditures (for all WIC-participating households) (%) | 8.8 (1.3) | ||
| WIC expenditures as share of total FAH expenditures (for households with WIC event in week) (%) | 24.3 (2.5) | ||
NOTES: FAFH = food away from home; FAH = food at home; PIR = federal poverty-to-income ratio; SE = standard error; SNAP = Supplemental Nutrition Assistance Program. Population weights were applied. This table is reproduced from Table 10-2 from the WIC committee phase I report.
- a
Significantly different from the WIC-participating households at a 1 percent level of statistical significance.
- b
Significantly different from the WIC-participating households at a 10 percent level of statistical significance.
SOURCE: USDA/ERS, 2015c.
TABLE 2-4Weekly Household Expenditures: Total Expenditures, Expenditures When WIC Is Used (WIC Paid >0) and When WIC Is Not Used (WIC Paid = 0)
| WIC Participating Households | Non-WIC, Income ≤185% (Pregnant or Child <5) | Non-WIC, Income >185% (Pregnant or Child <5) | |||
|---|---|---|---|---|---|
| N = 461 | WIC Paid >0 N = 150 | WIC Paid = 0 N = 311 | N = 306 | N = 241 | |
| Total food at home expenditure (FAH) ($) | 124.18 (7.62) | 160.92 (9.30) | 106.77 (9.66) | 113.15 (8.07) | 164.14 (13.09) |
| Total WIC expenditure ($) | 10.75 (1.82) | 33.42 (4.09) | |||
| WIC food item expenditure ($) | 21.55 (2.03) | 41.44 (3.58) | 12.13 (1.60) | 14.82 (1.24)a | 21.31 (2.01) |
| WIC items/Total FAH Expenditure (%) | 17.90 (1.37) | 29.21 (2.51) | 11.55 (1.01) | 13.14 (1.10)a | 13.46 (0.82)a |
| ($) | ($) | ($) | ($) | ($) | |
| Breakfast cereal | 2.40 (0.38) | 5.08 (0.80) | 1.13 (0.30) | 2.49 (0.29) | 2.31 (0.35) |
| Infant cereal | 0.03 (0.03) | 0.01 (0.01) | 0.04 (0.04) | 0.02 (0.02) | 0.02 (0.02) |
| Infant vegetable and fruit | 0.56 (0.21) | 1.08 (0.55) | 0.31 (0.16) | 0.34 (0.15) | 0.45 (0.20) |
| Infant meat | 0.02 (0.01) | 0.02 (0.02) | 0.02 (0.02) | 0.09 (0.07) | 0.01 (0.01) |
| Infant formula | 3.21 (1.23) | 9.62 (3.72) | 0.17 (0.12) | 0.48 (0.21)b | 0.96 (0.59)c |
| Milk | 3.98 (0.40) | 7.19 (0.68) | 2.46 (0.40) | 3.05 (0.31)c | 3.88 (0.39) |
| Cheese | 3.20 (0.37) | 4.90 (0.55) | 2.44 (0.46) | 2.54 (0.32) | 5.07 (1.04)c |
| Soy milk | 0.27 (0.11) | 0.55 (0.32) | 0.15 (0.08) | 0.22 (0.09) | 0.23 (0.08) |
| Eggs | 1.42 (0.21) | 2.04 (0.30) | 1.13 (0.26) | 0.72 (0.09)a | 1.00 (0.17) |
| Legumes | 0.64 (0.14) | 0.77 (0.27) | 0.57 (0.16) | 0.61 (0.16) | 0.43 (0.11) |
| Peanut butter | 0.35 (0.10) | 0.78 (0.23) | 0.14 (0.09) | 0.26 (0.08) | 0.09 (0.03)b |
| Vegetable and fruit | 1.79 (0.31) | 2.53 (0.53) | 1.45 (0.37) | 1.44 (0.27) | 2.60 (0.37)c |
| Fish | 0.21 (0.07) | 0.21 (0.08) | 0.21 (0.10) | 0.25 (0.08) | 0.05 (0.02)b |
| Bread | 0.49 (0.14) | 1.33 (0.36) | 0.09 (0.04) | 0.19 (0.07)b | 0.34 (0.11)b |
| Juice | 1.76 (0.27) | 3.32 (0.63) | 1.03 (0.17) | 1.13 (0.18)c | 1.49 (0.29) |
| Yogurt | 1.21 (0.24) | 2.12 (0.48) | 0.78 (0.25) | 0.96 (0.20) | 2.18 (0.43)b |
| Tofu | – (–) | – (–) | – (–) | 0.02 (0.01) | 0.19 (0.13) |
NOTES: FAH = food at home. Population weights were applied.
- a
Significantly different from the WIC-participating households at a 1 percent level of statistical significance.
- b
Significantly different from the WIC-participating households at a 5 percent level of statistical significance.
- c
Significantly different from the WIC-participating households at a 10 percent level of statistical significance.
SOURCE: USDA/ERS, 2015c.
TABLE 2-5Food Expenditures Events During Week: Total for Event, Amount WIC Paid (WIC Paid >0) and Other Paid (WIC Paid = 0)
| WIC Participating Households | Non-WIC, Income ≤185% (Pregnant or Child <5) | Non-WIC, Income >185% (Pregnant or Child <5) | |||
|---|---|---|---|---|---|
| N = 1,967 | WIC Paid >0 N = 252 | WIC Paid = 0 N = 1,715 | N = 1,055 | N = 826 | |
| Total food at home (FAH) expenditure in event ($) | 29.54 (1.37) | 25.42 (3.03) | 30.09 (1.5) | 33.6 (2.03) | 47.82 (3.16)a |
| Total WIC expenditure in event ($) | 21.74 (2.26) | ||||
| WIC food item expenditure in event ($) | 4.96 (0.33) | 15.68 (1.54) | 3.58 (0.28) | 4.31 (0.32) | 6.15 (0.54) |
| WIC items/total FAH expenditure in events (%) | 21.73 (1.60) | 68.02 (4.42) | 15.13 (1.54) | 14.88 (1.90) | 13.73 (1.06)c |
| WIC items/WIC expenditure in events (%) | 81.47 (8.18) | ||||
| $ | $ | $ | $ | $ | |
| Breakfast cereal | 0.55 (0.08) | 1.39 (0.25) | 0.45 (0.09) | 0.72 (0.09) | 0.67 (0.10) |
| Infant cereal | 0.01 (0.01) | - | 0.01 (0.01) | 0.00 (0.00) | 0.01 (0.00) |
| Infant vegetable and fruit | 0.13 (0.05) | 0.55 (0.36) | 0.07 (0.03) | 0.1 (0.03) | 0.13 (0.05) |
| Infant meat | 0.01 (0.00) | – (–) | 0.01 (0.00) | 0.03 (0.02) | 0.00 (0.00) |
| Infant formula | 0.74 (0.20) | 5.61 (1.62) | 0.11 (0.05) | 0.14 (0.06)a | 0.28 (0.13)c |
| Milk | 0.91 (0.09) | 3.43 (0.38) | 0.59 (0.08) | 0.89 (0.08) | 1.12 (0.12) |
| Cheese | 0.74 (0.09) | 1.24 (0.27) | 0.67 (0.09) | 0.74 (0.09) | 1.46 (0.25) |
| Soy milk | 0.06 (0.03) | 0.15 (0.08) | 0.05 (0.03) | 0.06 (0.02) | 0.07 (0.02) |
| Eggs | 0.33 (0.05) | 0.64 (0.12) | 0.29 (0.05) | 0.21 (0.03)b | 0.29 (0.05) |
| Legumes | 0.15 (0.03) | 0.23 (0.05) | 0.14 (0.03) | 0.18 (0.05) | 0.13 (0.03) |
| Peanut butter | 0.08 (0.02) | 0.33 (0.09) | 0.05 (0.02) | 0.07 (0.02) | 0.03 (0.01)b |
| Vegetable and fruit | 0.41 (0.05) | 0.10 (0.03) | 0.45 (0.06) | 0.42 (0.08) | 0.75 (0.10)a |
| Fish | 0.05 (0.02) | 0.01 (0.01) | 0.05 (0.02) | 0.42 (0.08)a | 0.02 (0.01)c |
| Bread | 0.11 (0.03) | 0.63 (0.15) | 0.05 (0.02) | 0.07 (0.02) | 0.10 (0.03) |
| Juice | 0.41 (0.05) | 1.36 (0.27) | 0.28 (0.04) | 0.06 (0.02)a | 0.43 (0.08) |
| Yogurt | 0.28 (0.05) | 0.03 (0.02) | 0.31 (0.06) | 0.28 (0.06) | 0.63 (0.13)b |
| Tofu | – (–) | – (–) | – (–) | 0.01 (0.00) | 0.05 (0.04) |
NOTES: Population weights were applied.
- a
Significantly different from the WIC-participating households at a 1 percent level of statistical significance.
- b
Significantly different from the WIC-participating households at a 5 percent level of statistical significance.
- c
Significantly different from the WIC-participating households at a 10 percent level of statistical significance.
SOURCE: USDA/ERS, 2015c.
TABLE 2-6Healthy People 2020 Breastfeeding Objectives Compared to 2014–2015 Proportion (%) of Children Who Were Breastfed at Various Ages
| Breastfeeding Behavior and Infant Age | Healthy People 2020: Objectives | 2014–2015 U.S. Breastfeeding Prevalence |
|---|---|---|
| Proportion who ever breastfed | 81.9 | 81.1 |
| Proportion breastfed at 6 months | 60.6 | 51.8 |
| Proportion breastfed at 1 year | 34.1 | 30.7 |
| Proportion exclusively breastfed at 3 months | 46.2 | 44.4 |
| Proportion exclusively breastfed at 6 months | 25.5 | 22.3 |
TABLE 2-7Prevalence of Ever Breastfeeding and Breastfeeding at 6-Months Postpartum by Race: 2009 and 2013
| Breastfeeding Prevalence (%) | ||||
|---|---|---|---|---|
| Ever Breastfed | Still Breastfeeding at 6 Months | |||
| Race/Ethnicity | 2009 | 2013 | 2009 | 2013 |
| Hispanic | 80.1 | 83.0 | 47.4 | 45.6 |
| Non-Hispanic white | 77.7 | 84.3 | 48.6 | 57.9 |
| Non-Hispanic African American | 60.7 | 66.3 | 33.4 | 39.1 |
| Non-Hispanic Asian | 86.3 | 83.8 | 65.2 | 64.4 |
| Non-Hispanic American Indian/Alaska Native | 69.1 | 68.3 | 39.4 | 41.3 |
| Two or more races | 72.9 | 79.0 | 44.4 | 51.0 |
NOTES: Data are not adjusted for income.
SOURCE: CDC, 2016b.
TABLE 2-86-Month Breastfeeding Prevalence (%) in the United States by Income from 2008 to 2013
| Income Relative to Poverty Level | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 |
|---|---|---|---|---|---|---|
| Less than 100% | 33.5 | 35.7 | 38.1 | 37.8 | 37.7 | 38.2 |
| 100–199% | 41.3 | 44.7 | 42.5 | 45.5 | 49.1 | 47.0 |
| 200–399% | 50.0 | 53.4 | 55.1 | 57.7 | 59.5 | 60.4 |
| 400–599% | 55.1 | 61.1 | 59.3 | 61.9 | 66.3 | 65.9 |
| 600% or greater | 60.2 | 61.7 | 65.4 | 67.9 | 70.4 | 70.1 |
SOURCE: National Immunization Survey Data, as analyzed by the Centers for Disease Control and Prevention (CDC, 2016b).
TABLE 2-9WIC Program Costs, 2005–2015
| Year | Participation (millions) | Program Costs for Food (millions of dollars) | Average Monthly Food Cost Per Person (dollars) |
|---|---|---|---|
| 2005 | 8,023 | 3,602.80 | 37.42 |
| 2006 | 8,088 | 3,597.50 | 37.07 |
| 2007 | 8,285 | 3,881.10 | 39.04 |
| 2008 | 8,705 | 4,534.00 | 43.40 |
| 2009 | 9,122 | 4,640.90 | 42.40 |
| 2010 | 9,175 | 4,561.80 | 41.43 |
| 2011 | 8,961 | 5,020.20 | 46.69 |
| 2012 | 8,908 | 4,810.50 | 45.00 |
| 2013 | 8,663 | 4,497.10 | 43.26 |
| 2014 | 8,258 | 4,324.40 | 43.64 |
| 2015 | 8,024 | 4,176.20 | 43.37 |
NOTES: Participation data are annual averages in millions. In addition to food and nutrition services and administrative costs, total expenditures include funds for program evaluation, Farmers' Market Nutrition Program (FY1989 onward), special projects and infrastructure. Nutrition services includes nutrition education, preventative and coordination services (such as health care), and promotion of breastfeeding and immunization. FY2015 data are preliminary; all data are subject to revision.
SOURCE: USDA/FNS, 2016b.
TABLE 2-10WIC Infant Formula and Food Rebates, 2005–2015
| Fiscal Year | Rebates (millions of dollars) |
|---|---|
| 2005 | 1,709.77 |
| 2006 | 1,774.95 |
| 2007 | 1,902.74 |
| 2008 | 2,006.80 |
| 2009 | 1,937.42 |
| 2010 | 1,692.04 |
| 2011 | 1,314.10 |
| 2012 | 1,688.17 |
| 2013 | 1,876.85 |
| 2014 | 1,812.34 |
| 2015 | 1,799.20 |
NOTES: Data for 2008–2011 are rebates billed during the fiscal year. Data for 2012–2015 are rebates received during a fiscal year. Values reflect rebates on infant formula and, to a lesser extent, infant food.
SOURCES: USDA/FNS, 2016b (years 2008–2015); Personal communication, V. Oliveira, USDA-ERS, July 23, 2014 (years 2005–2007).
TABLE 2-11Trends in Food Consumption from Selected Food Groups: Mean Intakes for U.S Women, 20 Years and Older, NHANES 2005–2012
| Food Group | Mean Intake Per Day | Percent Change from Before to After the 2009 FP Changes (2007–2008 to 2011–2012)b | |||
|---|---|---|---|---|---|
| 2005–2006a | 2007–2008 | 2009–2010 | 2011–2012 | ||
| Total fruit (c-eq) | 0.88 | 0.92 | 1.06 | 0.96 | 4 |
| Total vegetables (c-eq) | 1.48 | 1.42 | 1.46 | 1.51 | 6 |
| Whole grains (oz-eq) | 0.67 | 0.68 | 0.81 | 0.91 | 34 |
| Refined grains (oz-eq) | 4.87 | 4.71 | 4.75 | 4.92 | 4 |
| Seafood low omega-3 (oz-eq) | 0.43 | 0.31 | 0.46 | 0.39 | 26 |
| Seafood high omega-3 (oz-eq) | 0.16 | 0.12 | 0.15 | 0.12 | 0 |
| Eggs (oz-eq) | 0.42 | 0.41 | 0.43 | 0.43 | 5 |
| Soy products (oz-eq) | 0.06 | 0.10 | 0.08 | 0.07 | −30 |
| Nuts and seeds (oz-eq) | 0.54 | 0.54 | 0.58 | 0.69 | 28 |
| Total protein foods (oz-eq) | 4.89 | 4.72 | 4.87 | 4.82 | 2 |
| Milk (c-eq) | 0.85 | 0.75 | 0.78 | 0.70 | −7 |
| Cheese (c-eq) | 0.59 | 0.57 | 0.63 | 0.63 | 11 |
| Yogurt (c-eq) | 0.06 | 0.06 | 0.08 | 0.07 | 17 |
| Total dairy (c-eq) | 1.51 | 1.41 | 1.50 | 1.43 | 1 |
| Oils (g-eq) | 19.20 | 19.06 | 19.92 | 22.83 | 20 |
| Solid fat (g-eq) | 33.94 | 33.02 | 30.84 | 30.64 | −7 |
| Added sugars (tsp-eq) | 14.83 | 15.80 | 15.24 | 15.37 | −3 |
NOTES: c-eq = cup-equivalents; FP = food package; g-eq = gram-equivalents; oz-eq = ounce-equivalents; tsp-eq = teaspoon-equivalents.
- a
During this time period, the revised food packages were conceived by the Institute of Medicine committee (see IOM, 2006).
- b
The direction of these changes varies if different sets of survey years are compared. The changes are not associated with the WIC food packages.
SOURCES: USDA/ARS, 2005–2012; USDA/ARS, 2014.
TABLE 2-12Trends in Food Consumption from Selected Food Groups: Mean Intakes for U.S. Children, 2 to 5 Years of Age, NHANES 2005–2012
| Food Group | Mean Intake Per Day | Percent Change from Before to After the 2009 FP Changes (2007–2008 to 2011–2012)b | |||
|---|---|---|---|---|---|
| 2005–2006a | 2007–2008 | 2009–2010 | 2011–2012 | ||
| Total fruit (c-eq) | 1.38 | 1.49 | 1.46 | 1.41 | −5 |
| Total vegetables (c-eq) | 0.74 | 0.70 | 0.67 | 0.66 | −6 |
| Whole grains (oz-eq) | 0.49 | 0.46 | 0.70 | 0.67 | 46 |
| Refined grains (oz-eq) | 4.20 | 4.05 | 4.03 | 4.41 | 9 |
| Seafood low omega-3 (oz-eq) | 0.17 | 0.11 | 0.12 | 0.13 | 18 |
| Seafood high omega-3 (oz-eq) | 0.04 | 0.01 | 0.03 | 0.02 | 100 |
| Eggs (oz-eq) | 0.28 | 0.34 | 0.31 | 0.32 | −6 |
| Soy products (oz-eq) | 0.03 | 0.03 | 0.04 | 0.03 | 0 |
| Nuts and seeds (oz-eq) | 0.27 | 0.24 | 0.32 | 0.29 | 21 |
| Total protein foods (oz-eq) | 2.86 | 2.90 | 3.00 | 2.90 | 0 |
| Milk (c-eq) | 1.63 | 1.67 | 1.70 | 1.62 | −3 |
| Cheese (c-eq) | 0.47 | 0.49 | 0.59 | 0.56 | 14 |
| Yogurt (c-eq) | 0.07 | 0.06 | 0.08 | 0.11 | 83 |
| Total dairy (c-eq) | 2.18 | 2.23 | 2.38 | 2.30 | 3 |
| Oils (g-eq) | 13.83 | 13.23 | 13.03 | 15.00 | 13 |
| Solid fat (g-eq) | 29.21 | 29.88 | 28.96 | 29.77 | 0 |
| Added sugars (tsp-eq) | 13.72 | 12.96 | 12.45 | 12.92 | 0 |
NOTES: c-eq = cup-equivalents; FP = food package; g-eq = gram-equivalents; oz-eq = ounce-equivalents; tsp-eq = teaspoon-equivalents.
- a
During this time period, the revised food packages were conceived by the Institute of Medicine committee (see IOM, 2006).
- b
The direction of these changes varies if different sets of survey years are compared. The changes are not associated with the WIC food packages.
SOURCES: USDA/ARS, 2005–2012; USDA/ARS, 2014.
TABLE 2-13USDA Food Intake Patterns for Kcal Levels of Interest: Comparison of 2005 and 2015–2020 DGA
| Food Group | Units | Kcal Pattern | |||||
|---|---|---|---|---|---|---|---|
| 1,300a | 2,300b | 2,600 | |||||
| 2005 | 2015–2020 | 2005 | 2015–2020 | 2005 | 2015–2020 | ||
| Fruits | c-eq/d | 1¼ | 1¼ | 2 | 2 | 2 | 2 |
| Vegetables | c-eq/d | 1½ | 1½ | 3 | 3 | 3½ | 3½ |
| Dark green | c-eq/wk | 1½ | 1 | 3 | 2 | 3 | 2½ |
| Red/orange | c-eq/wk | 1 | 3 | 2 | 6 | 2½ | 7 |
| Dry beans and peasc | c-eq/wk | 1 | ½ | 3 | 2 | 3½ | 2½ |
| Starchy | c-eq/wk | 2½ | 3½ | 6 | 6 | 7 | 7 |
| Other | c-eq/wk | 4½ | 2½ | 7 | 5 | 8½ | 5½ |
| Grains | oz-eq/d | 4½ | 4½ | 7½ | 7½ | 9 | 9 |
| Whole grains | oz-eq/d | 2¼ | 2¼ | 3¾ | 3¾ | 4½ | 4½ |
| Other grains | oz-eq/d | 2¼ | 2¼ | 3¾ | 3¾ | 4½ | 4½ |
| Protein Foods d | 3½ | 3½ | 6¼ | 6¼ | 6½ | 6½ | |
| Meat, poultry, eggs | oz-eq/wk | 16½ | 29½ | 31 | |||
| Seafood | oz-eq/wk | 5 | 9½ ↓e | 10 | |||
| Nuts, seeds, soy (oz-eq/wk) | oz-eq/wk | 2½ ↑ e | 5 | 5 | |||
| Dairy | c-eq/d | 2 | 2½ | 3 | 3 | 3 | 3 |
| Oils | g/d | 17 | 17 | 30 | 30 | 34 | 34 |
| Limits for: | |||||||
| Calories for Other Uses f | kcal | 171 | 105 | 326 | 315 | 410 | 380 |
| (% of calories) f | % | 13 | 8 | 14 | 14 | 16 | 15 |
NOTES: c-eq = cup-equivalents; DGA = Dietary Guidelines for Americans; oz-eq = ounce-equivalents.
- a
Serving equivalents for the 1,300-kcal food pattern are the average of the 1,200- and 1,400-kcal patterns.
- b
Serving equivalents for the 2,300-kcal food pattern are the average of the 2,200- and 2,400-kcal patterns.
- c
In the USDA food patterns, dry beans and peas are first counted toward the protein foods group until recommendations for that group are met, then are counted toward the dry beans and peas vegetable subgroup (USDA, 2015).
- d
In 2005, key protein sources were categorized as “lean meats and beans,” without protein subgroups.
- e
An arrow indicates that the recommended food group amount changed from 2010 to 2015–2020 by 1 unit in the specified direction. Other 2015–2020 food pattern amounts are unchanged from 2010.
- f
In 2005, solid fats and added sugars were built into a “discretionary calorie allowance” instead of specific gram levels of intake. These values are shown as a comparator to “calories for other uses” from the 2015–2020 DGA, which include added sugars, alcohol, added refined starches, saturated (solid) fats, or more than the recommended amount of nutrient-dense foods.
SOURCES: USDA/HHS, 2005, 2010, 2016.
TABLE 2-14Shortfall Nutrients and Nutrients of Public Health Concern Noted in the Dietary Guidelines for Americans: 2005, 2010, and 2015–2020
| 2005 | 2010 | 2015–2020 | |
|---|---|---|---|
| Adults | |||
| Calcium | ✓* | ✓* | ✓* |
| Potassium | ✓* | ✓* | ✓* |
| Choline | ✓ | ||
| Fiber | ✓* | ✓* | ✓* |
| Magnesium | ✓ | ✓ | |
| Vitamin A | ✓ | ✓ | ✓ |
| Vitamin C | ✓ | ✓ | ✓ |
| Vitamin E | ✓* | ✓ | ✓ |
| Vitamin D | ✓* | ✓* | |
| Vitamin K | ✓ | ||
| Folate | ✓ | ✓ | |
| Children and Adolescents | |||
| Calcium | ✓* | ✓* | ✓* |
| Potassium | ✓* | ✓* | ✓* |
| Fiber | ✓* | ✓* | ✓* |
| Magnesium | ✓ | ✓ | |
| Phosphorus | ✓ | ||
| Vitamin A | ✓ | ✓ | |
| Vitamin C | ✓ | ✓ | |
| Vitamin E | ✓* | ✓ | ✓ |
| Vitamin D | ✓* | ✓* | |
| Women of Reproductive Age | |||
| Iron | ✓* | ✓* | ✓* |
| Folate | ✓* | ✓* | ✓ |
NOTES: ✓ = shortfall nutrient; ✓* = nutrient of public health concern; nutrients of public health concern are those shortfall nutrients that are linked to adverse health outcomes.
SOURCES: USDA/HHS, 2005, 2010, 2015.
TABLE 2-15Redemption of WIC Foods, 2013–2016
| WIC Food Category | Average Percent Redemption (Range) | Relevant Food Package(s) |
|---|---|---|
| Infant formula | 94 (88–98)a,b,c | I, II |
| Eggs | 80 (71–85)e | IV through VII |
| Cash value voucher | 77 (69–89)e | IV through VII |
| Whole milk | 75 (63–84)a,b,d | IV-Ah |
| Juice | 70 (53–80)e | IV through VII |
| Cheese | 70 (54–80)a,b,d,f | IV through VII |
| Fish | 69 (54–65)e | VII |
| WIC-eligible medical foods | 66 (57–75)a,g | All packages |
| Low-fat milk | 65 (49–75)e | IV-Bi through VII |
| Breakfast cereal | 60 (46–69)e | IV through VII |
| Whole grain bread | 53 (39–65)e | IV through V and VII |
| Infant food fruits/vegetables | 51 (34–65)a,b,d,g | II |
| Peanut butter/legumes | 51 (44–66)e | IV through VII |
| Infant cereal | 47 (38–59)a,b,d,g | II |
| Infant food meats | 31 (24–43)a,b,d,f,g | II |
NOTES: The following prioritization was applied to select redemption rates for the current food package nutrient and cost profiles: First priority = the average of redemption data from 5 unidentified states, provided to the committee by FNS; if not available, second priority = the average of redemption data provided to the committee by individual states. Data span several months or an entire year, but provide a general picture of the typical food category redemption. The “average percent redemption” indicates the value applied in the nutrient and cost profiles, with the source indicated by superscript. The range indicates the range considering all values made available to the committee.
- a
Average and range include data from Massachusetts for 2015.
- b
Average and range include data from Kentucky for 2015.
- c
Average and range include data from California for 2015.
- d
Average and range include data from Chickasaw Nation for 2015.
- e
Average represents the average of redemption from 5 unidentified states, fiscal year 2013–2014, data provided by USDA-FNS. A description of this data source is available in Chapter 7 and Appendix R. Range includes data from all sources made available to the committee.
- f
Average and range include data from Texas for 2015.
- g
Average and range include data from Wyoming, late 2015 to early 2016.
- h
Food package IV-A is for children ages 1 to less than 2 years.
- i
Food package IV-B is for children ages 2 to less than 5 years.
SOURCES: USDA/ERS, 2014b; other data referenced are available in the public access file for this study (Email: paro@nas
.edu).
TABLE 2-16Changes and Challenges Since the IOM 2006 Review: Key Findings and Conclusions
| Challenge or Environmental Change Evaluated | Finding(s) and Conclusion(s) |
|---|---|
| Adaptation to the 2009 Food Package Implementation | State and local agencies, vendors, and manufacturers were largely able to adapt; some continuing challenges are related to sizes available in the marketplace. Consideration to the feasibility of potential food package changes from the perspective of states, local agencies, vendors, and manufacturers is critical for implementation success. Evidence indicates that targeted nutrition education in advance of food package changes can result in positive behavior change. This strategy could be applied at the state level to future food package changes. |
| Changes in WIC Participation | WIC participation has been declining since 2010, although the proportions of participants according to food package categories have remained consistent. The underlying cause of the decline is not clear but is not related to the 2009 food package changes (see Appendix F). Attention to retention of the program's value and reduction of participation barriers is warranted. Inasmuch as children ages 1 to less than 5 years comprise the majority of the WIC-participating population, changes to this food package (IV) will have the greatest effect on overall program costs for food. |
| Food Expenditures of WIC Participants | WIC benefits cover an important share of food expenditures for participating households. Despite some limitations to the data, the new evidence shows WIC-participating households spend more on WIC food items than do other households with low income. |
| Changes in Breastfeeding Prevalence | Breastfeeding prevalence among WIC participants is lower than that of other low-income women. Evidence is inconclusive about whether the 2009 food package changes affected the choice to breastfeed. |
| Associations Between WIC Participation and Breastfeeding | WIC participation was associated with a lower likelihood of breastfeeding initiation, duration, and exclusivity. Available data indicate that breastfeeding promotion and support among WIC participants is associated with the choice to breastfeed. These activities may improve breastfeeding prevalence in WIC when linked closely to food package changes. Evidence suggests that the 2009 food package policy that limited formula in the first month resulted in more women being issued the full formula-feeding package. Allowing a greater degree of flexibility in formula issuance in the first month may better support any degree of breastfeeding for women who choose a mixed-feeding option. |
| Ability of the Current Food Packages to Meet Participants' Needs | The current food packages offer a degree of flexibility both at the state and participant level. Available information suggests that the current food packages are satisfactory and meet needs, but redemption data suggest that improvements can be made. |
| Changes in Dietary Guidance | Key changes to the Dietary Guidelines for Americans, guidance for individuals less than 2 years of age, and to Dietary Reference Intakes have been made since the IOM 2006 review. These changes may have implications for both amounts of and specifications for foods in the WIC food packages. |
| Nationwide Availability of WIC Foods | The marketplace has expanded substantially since 2006 and now includes a wider variety of dairy and grain products, which may have improved the nationwide availability of foods that meet WIC specifications. Although most WIC participants shop at larger stores, smaller stores may be the only option for some WIC participants. Availability of WIC foods at both types of stores remains important. |
Boxes
BOX 2-1Summary of Literature Findings on Barriers to WIC Participation and Redemption
Barriers to Participation
- Long wait times; crowded physical environment
- Lack of transportation
- Belief that family is ineligible; changing eligibility restrictions
- Program requires too much effort, difficult paperwork
- Language barriers
Barriers to Redemption
- Embarrassment, negative interactions in stores
- Gaps in knowledge (e.g., determining amount of F/V with CVV)
- Limited selection of WIC foods at local vendors; products not available in allowable forms
- Vendor challenges anticipating demand and maintaining adequate supply of some WIC foods
- Maintaining food freshness at the vendor (particularly small vendors)
SOURCE: See Appendix G, Table G-1.
