NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-.
Regularly doing pelvic floor exercises can improve problems caused by a pelvic organ prolapse. Vaginal pessaries can also help, but they aren’t suitable for every woman.
If the connective tissue in a woman's pelvic floor weakens, her womb, bladder or the last part of the bowel may slip down. Known as pelvic organ prolapse, this can cause a feeling of pressure, problems urinating (peeing), and pain. Many women find that doing pelvic floor exercises and/or using a vaginal pessary is enough to improve the symptoms.
But there’s no guarantee that these treatments will make the symptoms go away. Especially pelvic floor exercises may have a limited effect if the organs have already slipped down far. Surgery may then be an option. In studies on pelvic floor exercises, between 3 and 10 out of 100 women ended up deciding to have surgery after all.
Our decision aid may help when deciding which treatment is most suitable. It summarizes the main advantages and disadvantages of the various treatment options.
What are pelvic floor exercises?
Pelvic floor exercises – sometimes also called Kegel exercises – strengthen the muscles in the lower part of the pelvis. These are the muscles that help to support the womb and the bladder. The exercises are particularly suitable for women who have mild bladder leakage (stress incontinence) and feelings of pressure in their abdomen. They involve actively tensing the muscles in the pelvic floor. Each session includes various exercises that last a few minutes and are repeated one to three times per day. It is best to learn the exercises from a physiotherapist so that they are right for your specific situation. In Germany, statutory health insurers pay for this.
How effective are pelvic floor exercises?
Pelvic floor exercises can improve the symptoms in mild and moderate cases (first- to third-degree prolapse) and sometimes also prevent the organs from slipping down further. The beneficial effects may already be noticeable after a few weeks. But these exercises don’t always help. Some women still have problems despite doing them. To increase the chances of success, it’s important to do the exercises as instructed – and especially to do them regularly. To stick to the exercises over the long term, it's a good idea to make them part of your daily routine. Pelvic floor exercises usually don't have any side effects.
The exercises are more effective if the prolapsed organs are in the front part of the pelvis, where the bladder and urethra (urine tube) are found. If you have had prolapse surgery, pelvic floor exercises probably won’t help much more – at least not in the first few years after the operation. Studies in this area have found that pelvic floor exercises don’t make a difference in women who have already had prolapse surgery. But it’s not clear whether the exercises might prevent the organs from dropping down again in the long term.
What are vaginal pessaries?
Vaginal pessaries for the treatment of prolapse – not to be confused with contraceptive pessaries – are small cubes, rings or saucer-shaped devices made of rubber or silicone. They are inserted into the vagina with the aim of providing the pelvic organs with support. So although pessaries don’t treat the cause of the prolapse, they can keep the affected organs in their natural position. Doctors also think that using a pessary might help to strengthen the pelvic floor muscles.
Pessaries are available in different shapes and sizes. People often have to try out a number of different pessaries before finding one that works. If possible, doctors usually prescribe cube pessaries that women can insert, remove and clean themselves. If other types of pessaries are used, these steps have to be performed at the doctor's office – typically every 6 to 8 weeks.
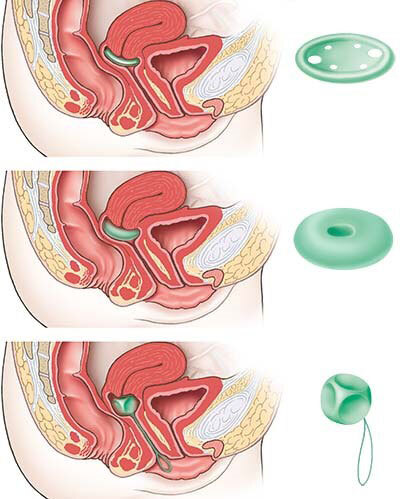
From top to bottom: “saucer-shaped” ring pessary with support, ring pessary without support, and cube pessary.
How effective are pessaries?
Well-fitting pessaries can support the pelvic organs in a way that reduces bladder and bowel problems or even makes them go away completely. They don’t fix prolapses. But women don’t always find a suitable pessary that is effective enough.
The use of a pessary is considered if, for instance, a woman wishes to avoid or delay surgery. About half of all women who use a pessary get by with it so well that they use it for several years or more. Pessaries can also be a good idea if pelvic floor exercises don’t help enough on their own.
Do pessaries have disadvantages?
Women who use a vaginal pessary need regular appointments to have the pessary checked and their vagina examined by a doctor.
Because pessaries push against the lining of the vagina, they can irritate the mucous membranes there and even lead to pressure sores. These cause symptoms such as pain and bleeding. Pessaries can also lead to problems with bowel movements or increase the likelihood of vaginal infections. With some pessaries, it’s not possible to penetrate the vagina during sex – with others it is, but they might cause discomfort. Cube pessaries can be removed before having sex.
To avoid side effects, it’s important that the pessary is well positioned and also changed and cleaned regularly. A lubricant gel can make it easier to insert the pessary. After menopause, women who use a pessary are advised to protect the lining of their vagina with a hormone cream – unless they have already had cancer in a reproductive organ or breast cancer.
Sources
- Barber MD. Pelvic organ prolapse. BMJ 2016; 354: i3853. [PubMed: 27439423]
- Bugge C, Adams EJ, Gopinath D et al. Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev 2020; (11): CD004010. [PMC free article: PMC8094172] [PubMed: 33207004]
- Deutsche Gesellschaft für Gynäkologie und Geburtshilfe (DGGG). Weiblicher Descensus genitalis, Diagnostik und Therapie (S2e-Leitlinie). AWMF-Registernr.: 015-006. 2016.
- Haya N, Feiner B, Baessler K et al. Perioperative interventions in pelvic organ prolapse surgery. Cochrane Database Syst Rev 2018; 8: CD013105. [PMC free article: PMC6513581] [PubMed: 30121957]
- Li C, Gong Y, Wang B. The efficacy of pelvic floor muscle training for pelvic organ prolapse: a systematic review and meta-analysis. Int Urogynecol J 2016; 27(7): 981-992. [PubMed: 26407564]
- Wu YM, McInnes N, Leong Y. Pelvic Floor Muscle Training Versus Watchful Waiting and Pelvic Floor Disorders in Postpartum Women: A Systematic Review and Meta-analysis. Female Pelvic Med Reconstr Surg 2018; 24(2): 142-149. [PubMed: 29474288]
- Zhang FW, Wei F, Wang HL et al. Does pelvic floor muscle training augment the effect of surgery in women with pelvic organ prolapse? A systematic review of randomized controlled trials. Neurourol Urodyn 2016; 35(6): 666-674. [PubMed: 25932625]
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
- Pelvic organ prolapse: Learn More – Pelvic floor exercises and vaginal pessaries...Pelvic organ prolapse: Learn More – Pelvic floor exercises and vaginal pessaries - InformedHealth.org
Your browsing activity is empty.
Activity recording is turned off.
See more...
