NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Vortioxetine is a serotonergic antidepressant used for major depression disorders. Vortioxetine has been associated with a low rate of minor serum aminotransferase elevations during treatment, but has not been linked to instances of clinically apparent acute liver injury.
Background
Vortioxetine (vor" tye ox' e teen) is a unique serotonergic antidepressant that is believed to have a bimodal activity, inhibiting serotonin reuptake, but also acting as a mixed agonist and antagonist directly on serotonin (5-HT) receptors. Vortioxetine has been shown to be effective in alleviating symptoms of depression in patients with major depression disorder. Vortioxetine was approved for use in the United States in 2013 for use in treatment of major depression disorders. There is limited clinical experience with its use. Vortioxetine is available in tablets of 5, 10, 15 and 20 mg under the commercial name Trintellix. The recommended dose is 10 mg once daily initially, with subsequent increase to as much as 20 mg daily based upon efficacy and tolerance. Doses of 5 mg can be used if 10 mg doses are not tolerated. Common side effects include nausea, constipation, dizziness, somnolence, headache and dry mouth. Less common and rare side effects include mood disorders, suicidal ideation, sexual dysfunction, serotonin syndrome, discontinuation syndrome, increased risk of bleeding, hypersensitivity reactions and precipitation of manic episodes.
Hepatotoxicity
Liver test abnormalities occur in a small proportion of patients (<1%) on long term therapy with vortioxetine, but elevations are usually mild, asymptomatic and transient, reversing even with continuation of medication. No instances of acute liver injury with jaundice have been reported attributable to vortioxetine, but the total experience with its use has been limited. However, most other SSRIs have been implicated in rare instances of clinically apparent liver injury. The latency to onset is typically 1 to 8 weeks and the pattern of enzyme elevations varies, ranging from cholestatic to hepatocellular. Mild signs and symptoms of hypersensitivity (rash, fever, eosinophilia) are common, but usually not prominent. Autoantibody formation is rare. The course is generally self-limited and mild-to-moderate in severity, but fatalities have been reported with some SSRIs. However, vortioxetine itself has not been implicated in similar cases.
Likelihood score: E* (unproven but suspected rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which vortioxetine might cause serum aminotransferase elevations or liver injury is not known. Vortioxetine is metabolized by the liver via the cytochrome P450 system (predominantly CYP 2D6) and is susceptible to drug-drug interactions with agents that induce (rifampin, carbamazepine, phenytoin) or inhibit (bupropion, fluoxetine, quinidine) CYP 2D6 activity. Combination of vortioxetine with other serotonergic agents may precipitate the serotonin syndrome marked by fever, tachycardia, hypertension and agitation and can be accompanied by mild serum aminotransferase elevations.
Outcome and Management
The serum aminotransferase elevations that occur on vortioxetine therapy are usually self-limited and do not require dose modification or discontinuation of therapy. No instances of acute liver failure or vanishing bile duct syndrome due to vortioxetine have been reported. There is no information on cross sensitivity to liver injury between vortioxetine and other antidepressants, but switching to another antidepressant after clinically apparent liver injury during vortioxetine therapy should be done with caution and adequate monitoring.
Drug Class: Antidepressant Agents
Other Drugs in the Subclass, SNRIs/SSRIs: Citalopram, Escitalopram, Duloxetine, Fluoxetine, Fluvoxamine, Levomilnacipran, Paroxetine, Sertraline, Venlafaxine, Vilazodone
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vortioxetine – Trintellix®
DRUG CLASS
Antidepressant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Vortioxetine | 508233-74-7 | C18-H22-N2-S |
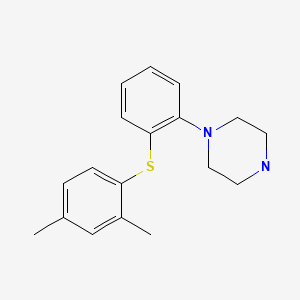
|
ANNOTATED BIBLIOGRAPHY
References updated: 08 April 2020
Abbreviations: MAO inhibitor, monoamine oxidase inhibitor; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor.
- Zimmerman HJ. Antidepressants. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 493-8.(Expert review of hepatotoxicity of antidepressants published in 1999; vortioxetine is not discussed).
- Larrey D, Ripault MP. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 443-62.(Review of antidepressant hepatotoxicity; vortioxetine is not discussed).
- O'Donnell JM, Bies RR, Shelton RC. Drug therapy of depression and anxiety disorders. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 267-77.(Textbook of pharmacology and therapeutics: vortioxetine is not mentioned).
- Katona C, Hansen T, Olsen CK. A randomized, double-blind, placebo-controlled, duloxetine-referenced, fixed-dose study comparing the efficacy and safety of Lu AA21004 in elderly patients with major depressive disorder. Int Clin Psychopharmacol. 2012;27:215–23. [PubMed: 22572889](Among 452 patients with major depression treated with vortioxetine, duloxetine or placebo for 8 weeks, no patient developed a liver related serious adverse event and "no clinically relevant changes over time or differences between treatment groups were seen in clinical laboratory test results").
- Vortioxetine (Brintellix) for depression. Med Lett Drugs Ther. 2013;55(1430):93–5. [PubMed: 24276501](Concise review of mechanism of action, efficacy, adverse effects and costs of vortioxetine mentions that the most common adverse effects were nausea, vomiting and constipation; weight gain is uncommon and sexual dysfunction can occur in both women and men; no mention of ALT elevations or hepatotoxicity).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, Presentation and Outcomes in Patients with Drug-Induced Liver Injury in the General Population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to vortioxetine).
- Park SH, Ishino R. Liver injury associated with antidepressants. Curr Drug Saf. 2013;8:207–23. [PubMed: 23914755](Review of drug induced liver injury due to antidepressants; vortioxetine is not mentioned).
- Montgomery SA, Nielsen RZ, Poulsen LH. Häströ. A randomised, double-blind study in adults with major depressive disorder with an inadequate response to a single course of selective serotonin reuptake inhibitor or serotonin-noradrenaline reuptake inhibitor treatment switched to vortioxetine or agomelatine. Hum Psychopharmacol. 2014;29:470–82. [PMC free article: PMC4265248] [PubMed: 25087600](Among 495 patients with major depression not responding adequately to SSRI therapy who were treated with either vortioxetine or agomelatine for 12 weeks, one patient on agomelatine was withdrawn from therapy because of ALT elevations [>3 times ULN], but there were no other "clinically relevant changes over time or differences between treatment groups" in clinical laboratory results).
- McIntyre RS, Lophaven S, Olsen CK. A randomized, double-blind, placebo-controlled study of vortioxetine on cognitive function in depressed adults. Int J Neuropsychopharmacol. 2014;17:1557–67. [PMC free article: PMC4162519] [PubMed: 24787143](Among 591 patients with major depressive disorders treated with vortioxetine [10 or 20 mg daily] or placebo for 8 weeks, common side effects were nausea and headache, and laboratory test results showed no "clinically relevant changes over time or differences between treatment groups").
- Mahableshwarkar AR, Jacobsen PL, Serenko M, Chen Y. A randomized, double-blind, fixed-dose study comparing the efficacy and tolerability of vortioxetine 2.5 and 10 mg in acute treatment of adults with generalized anxiety disorder. Hum Psychopharmacol. 2014;29:64–72. [PubMed: 24424707](Among 457 patients with generalized anxiety disorder treated with vortioxetine [2.5 or 20 mg] or placebo daily for 8 weeks, there were no improvements in measures of anxiety in the drug treated groups and no differences in clinical laboratory values nor "trends warranting safety concerns").
- Mahableshwarkar AR, Jacobsen PL, Chen Y, Simon JS. A randomised, double-blind, placebo-controlled, duloxetine-referenced study of the efficacy and tolerability of vortioxetine in the acute treatment of adults with generalised anxiety disorder. Int J Clin Pract. 2014;68:49–59. [PubMed: 24341301](In a controlled trial of 8 weeks of vortioxetine [2.5, 5 or 10 mg daily], duloxetine or placebo is 781 patients with generalized anxiety disorder, no liver related serious adverse reactions were reported and "changes in serum chemistry... parameters were distributed evenly across vortioxetine and placebo groups" with "no discernible patterns of concern").
- Boulenger JP, Loft H, Olsen CK. Efficacy and safety of vortioxetine (Lu AA21004), 15 and 20 mg/day: a randomized, double-blind, placebo-controlled, duloxetine-referenced study in the acute treatment of adult patients with major depressive disorder. Int Clin Psychopharmacol. 2014;29:138–49. [PMC free article: PMC3979887] [PubMed: 24257717](Among 608 patients with major depression treated for 8 weeks with vortioxetine [15 or 20 mg daily], duloxetine or placebo, there were no "clinically relevant changes over time or differences between treatment groups" in clinical laboratory test results).
- Alam MY, Jacobsen PL, Chen Y, Serenko M, Mahableshwarkar AR. Safety, tolerability, and efficacy of vortioxetine (Lu AA21004) in major depressive disorder: results of an open-label, flexible-dose, 52-week extension study. Int Clin Psychopharmacol. 2014;29:36–44. [PMC free article: PMC4235387] [PubMed: 24169027](Among 834 patients with major depression participating in short term controlled trials of vortioxetine who were then treated with a further 52 weeks of flexible doses of the drug, the most frequent adverse events were mild-to-moderate nausea, headache, pharyngitis, diarrhea and dizziness; ALT elevations above 3 times ULN occurred in 0.4% and AST elevations in 0.7%, but these were asymptomatic and did not require drug discontinuation).
- Voican CS, Corruble E, Naveau S, Perlemuter G. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry. 2014;171:404–15. [PubMed: 24362450](Review of the frequency and clinical features of drug induced liver injury due to antidepressants; SSRIs such as venlafaxine, fluoxetine, sertraline and paroxetine are discussed, but not vortioxetine).
- Hernández N, Bessone F, Sáhez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, one of which was attributed to an antidepressant [amitriptyline], but none were attributed to vortioxetine).
- Zhang J, Mathis MV, Sellers JW, Kordzakhia G, Jackson AJ, Dow A, Yang P, et al. The US Food and Drug Administration's perspective on the new antidepressant vortioxetine. J Clin Psychiatry. 2015;76:8–14. [PubMed: 25562777](FDA summary of safety and efficacy analyses of data submitted on 7666 volunteers and patients treated with vortioxetine [5 to 20 mg daily] discusses 6 deaths [none liver related] and common non-serious adverse events [nausea, vomiting, constipation], without mentioning ALT elevations or hepatotoxicity).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 20 cases were attributed to antidepressants, including 5 to SSRIs [fluoxetine, escitalopram, sertraline], 9 to SNRIs [duloxetine, trazodone, nefazodone], but none to vortioxetine).
- Jacobsen PL, Harper L, Chrones L, Chan S, Mahableshwarkar AR. Safety and tolerability of vortioxetine (15 and 20 mg) in patients with major depressive disorder: results of an open-label, flexible-dose, 52-week extension study. Int Clin Psychopharmacol. 2015;30:255–64. [PMC free article: PMC4525811] [PubMed: 26020712](In an open label study of 1075 patients treated with vortioxetine for 52 weeks, "The increased risk for hepatotoxicity that was reported with agomelatine treatment was not observed on long-term exposure to vortioxetine").
- Mahableshwarkar AR, Zajecka J, Jacobson W, Chen Y, Keefe RS. A randomized, placebo-controlled, active-reference, double-blind, flexible-dose study of the efficacy of vortioxetine on cognitive function in major depressive disorder. Neuropsychopharmacology. 2015;40:2025–37. [PMC free article: PMC4839526] [PubMed: 25687662](Among 602 patients with major depression treated with vortioxetine, duloxetine or placebo for 8 weeks, there were no "clinically significant findings within or differences between groups" in clinical chemistry results).
- Baldwin DS, Chrones L, Florea I, Nielsen R, Nomikos GG, Palo W, Reines E. The safety and tolerability of vortioxetine: Analysis of data from randomized placebo-controlled trials and open-label extension studies. J Psychopharmacol. 2016;30:242–52. [PMC free article: PMC4794082] [PubMed: 26864543](Pooled analysis of 11 controlled trials and 5 extension studies of vortioxetine in 5701 patients with major depression found the most common adverse events was nausea [21% to 31%] and that it had “no effect relative to placebo on clinical laboratory parameters”).
- Nishimura A, Aritomi Y, Sasai K, Kitagawa T, Mahableshwarkar AR. Randomized, double-blind, placebo-controlled 8-week trial of the efficacy, safety, and tolerability of 5, 10, and 20 mg/day vortioxetine in adults with major depressive disorder. Psychiatry Clin Neurosci. 2018;72:64–72. [PubMed: 28858412](Among 600 Japanese patients with major depression treated with vortioxetine [5, 10 or 20 mg] or placebo daily for 8 weeks, response rates were not significantly higher in the treated arms and side effects that were more common with vortioxetine included nausea, dizziness and insomnia; one patient discontinued therapy early because of abnormal liver tests, but details not provided).
- Lochmann D, Richardson T. Selective serotonin reuptake inhibitors. Handb Exp Pharmacol. 2019;250:135–44. [PubMed: 30838457](Overview of the SSRIs mentioned that they have similar efficacy in treating depression and similar rates and adverse event profile which largely represents the effects of serotonin excess: nausea, diarrhea, dizziness, somnolence, insomnia, sweating, tremor anxiety, dry mouth, anxiety and restlessness; they can also cause weigh gain and sex dysfunction as well as activate mania and cause withdrawn symptoms).
- Schwasinger-Schmidt TE, Macaluso M. Other antidepressants. Handb Exp Pharmacol. 2019;250:325–55. [PubMed: 30194544](Review of mechanism of action, pharmacology, clinical efficacy and side effects of atypical antidepressants including vortioxetine which is a mixed serotonin receptor agonist and antagonist which results in an increase in serotonergic transmission, whose major side effects are nausea and diarrhea and can cause increase risk of bleeding and hyponatremia; no discussion of hepatic side effects).
- Drugs for depression. Med Lett Drugs Ther. 2020;62(1592):25–32. [PubMed: 32320387](Concise review of the mechanism of action, clinical efficacy, safety and costs of drugs for depression; hepatotoxicity is mentioned only for nefazodone [now rarely used because of severe hepatotoxicity] and duloxetine [in heavy drinkers]).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Vortioxetine for depression in adults.[Cochrane Database Syst Rev. 2017]Review Vortioxetine for depression in adults.Koesters M, Ostuzzi G, Guaiana G, Breilmann J, Barbui C. Cochrane Database Syst Rev. 2017 Jul 5; 7(7):CD011520. Epub 2017 Jul 5.
- Review Flibanserin.[LiverTox: Clinical and Researc...]Review Flibanserin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review VORTIOXETINE - THE NEW ANTIDEPRESSANT AGENT WITH PROCOGNITIVE PROPERTIES.[Acta Pol Pharm. 2016]Review VORTIOXETINE - THE NEW ANTIDEPRESSANT AGENT WITH PROCOGNITIVE PROPERTIES.Dziwota E, Olajossy M. Acta Pol Pharm. 2016 Nov; 73(6):1433-1437.
- Effect of Vortioxetine vs. Escitalopram on Sexual Functioning in Adults with Well-Treated Major Depressive Disorder Experiencing SSRI-Induced Sexual Dysfunction.[J Sex Med. 2015]Effect of Vortioxetine vs. Escitalopram on Sexual Functioning in Adults with Well-Treated Major Depressive Disorder Experiencing SSRI-Induced Sexual Dysfunction.Jacobsen PL, Mahableshwarkar AR, Chen Y, Chrones L, Clayton AH. J Sex Med. 2015 Oct; 12(10):2036-48. Epub 2015 Aug 31.
- Review Amoxapine.[LiverTox: Clinical and Researc...]Review Amoxapine.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Vortioxetine - LiverToxVortioxetine - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...