NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Vismodegib is a kinase inhibitor active used in the therapy of unresectable or metastatic basal cell carcinoma. Vismodegib therapy is associated with a low rate or transient elevations in serum aminotransferase during therapy and has been linked to rare cases of clinically apparent acute liver injury.
Background
Vismodegib (vis” moe deg’ ib) is an orally available, kinase inhibitor with specific activity against a key step (activation of smoothened: SMO) in the hedgehog signaling pathway. Hedgehog is a key regulator of embryonic development, cell growth and differentiation. Mutations in this pathway have been identified in several malignant diseases including basal cell carcinoma. Clinical trials of vismodegib in patients with metastatic or locally advanced basal cell carcinoma reported at least partial responses in up to half of patients. Vismodegib, the first hedgehog pathway inhibitor, was approved for use in the United States in 2012. Current indications include metastatic or locally advanced, recurrent or unresectable basal cell carcinoma. Vismodegib is available in capsules of 150 mg under the brand name Erivedge. The typical dose is 150 mg once daily until disease progression or unacceptable toxicity occurs. Side effects are common and often dose limiting, although rarely life threatening. Common side effects include muscle spasms, alopecia, anorexia, dysguesia, weight loss, nausea, diarrhea, fatigue and arthralgias. Potential serious adverse events include severe weight loss, squamous cell skin cancer and embryo-fetal toxicity.
Hepatotoxicity
Most clinical trials of vismodegib included few patients and rates of liver tests abnormalities were usually not reported. The product label for vismodegib includes no mention serum enzyme elevations or hepatotoxicity. However, a subsequent review of all published studies of vismodegib mentions that liver enzyme elevations occurred in 1.4% of a total of 363 patients treated. Since its approval and more general use, reports of clinically apparent liver injury linked to vismodegib have appeared. In one report, an elderly man presented with fatigue, nausea and jaundice 41 days after starting vismodegib with a cholestatic pattern of serum enzyme elevations and rapid improvement on stopping (Case 1). In addition, review of 7 years of spontaneous adverse event reporting to the FDA revealed 94 reports of hepatotoxicity during vismodegib therapy, including 20 that were considered serious and 4 that resulted in hepatic failure. Thus, clinically apparent liver injury from vismodegib occurs, but is somewhat rare.
Likelihood score: C (probable cause of clinically apparent liver injury).
Mechanism of Injury
The cause of liver injury from vismodegib is unknown, but likely due to hypersensitivity. Vismodegib has a prolonged half-life (~19 days) and is metabolized at least in part in the liver via multiple cytochrome P450 enzymes, including CYP 3A4, 2C8, 2C9 and 2C19. While it theoretically should have several drug-drug interactions, there is little clinical data on its effects on other drugs or vice versa.
Outcome and Management
In using kinase inhibitors for treatment of cancer, monitoring of routine liver tests before starting and at intervals during therapy is warranted. Serum aminotransferase elevations above 5 times the upper limit of normal (if confirmed) or any elevations accompanied by jaundice or symptoms should lead to temporary cessation. Restarting vismodegib after cessation for liver test abnormalities should be done with caution and only after the abnormalities have resolved or improved significantly. The various protein kinase inhibitors vary greatly in chemical structure and there is little evidence for cross sensitivity to the liver injury.
Drug Class: Antineoplastic Agents, Protein Kinase Inhibitors
CASE REPORT
Case 1. Cholestatic hepatitis attributed to vismodegib therapy.
[Modified from: Ash MM, Jolly PS. Cholestatic hepatic injury associated with vismodegib, aspirin, and naproxen use: a case study and review of vismodegib safety. Int J Dermatol 2015; 54: 370-4. PubMed Citation]
A 72 year old man with multiple basal cell carcinomas developed worsening nausea, dysgeusia, anorexia, weight loss and muscle cramps followed by appearance of jaundice 5 to 6 weeks after starting vismodegib. He also had a sudden loss of voice, decreased fluid intake and melena without sore throat, fever or rash. He had no history of liver disease or alcohol abuse, and all liver tests had been normal before vismodegib therapy was begun (Table). Medications that he took chronically included tadalafil, amlodipine, and valsartan, and he had recently started naproxen and aspirin because of muscle cramps attributed to vismodegib. On presentation, he was jaundiced and had mild hepatic tenderness. Serum bilirubin was 10.7 mg/dL, ALT 525 U/L, AST 206 U/L, alkaline phosphatase 807 U/L, GGT 550 U/L and INR 1.1. He had a mild increase in serum creatinine (2.2 mg/dL), possibly due to dehydration. Vismodegib was stopped and he was admitted for evaluation and intravenous hydration. Imaging of the liver showed no evidence of gall stones or biliary obstruction. Symptoms and liver test abnormalities began to improve rapidly and two weeks later, jaundice had resolved and liver tests were minimally elevated. Six months later, routine liver tests were all within the normal range.
Key Points
| Medication: | Vismodegib (300 mg daily) |
| Pattern: | Cholestatic (R=1.2) |
| Severity: | 3+ (jaundice and hospitalization) |
| Latency: | 5-6 weeks |
| Recovery: | ~4 weeks |
| Other medications: | Aspirin and naproxen acutely; tadalifil, amlodipine and varsartan chronically. |
Laboratory Values
Comment
An elderly man with multiple basal cell carcinomas developed dysgeusia and muscle cramps within a month of starting vismodegib and was found to have mild serum ALT and AST elevations. In the following two weeks, however, he developed worsening symptoms and jaundice and was found to have a cholestatic hepatitis. He had also developed worsening side effects of treatment, dehydration, laryngitis and mild gastrointestinal bleeding. Upon hospital admission and stopping vismodegib he improved rapidly, most liver tests being normal or near normal two weeks later. Information on hepatitis serology, autoantibodies and eosinophil counts was not provided, but immunoallergic features were not present, and the clinical course and outcome were entirely compatible with a drug induced cholestatic hepatitis. While most cases of acute liver injury attributed to kinase inhibitors have been described as hepatocellular, the actual aminotransferase and alkaline phosphatase values are often not provided. Even this case might have been considered hepatocellular (ALT 525 U/L) had the other values not been available.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Vismodegib – Erivedge®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Vismodegib | 879085-55-9 | C19-H14-Cl2-N2-O3-S |
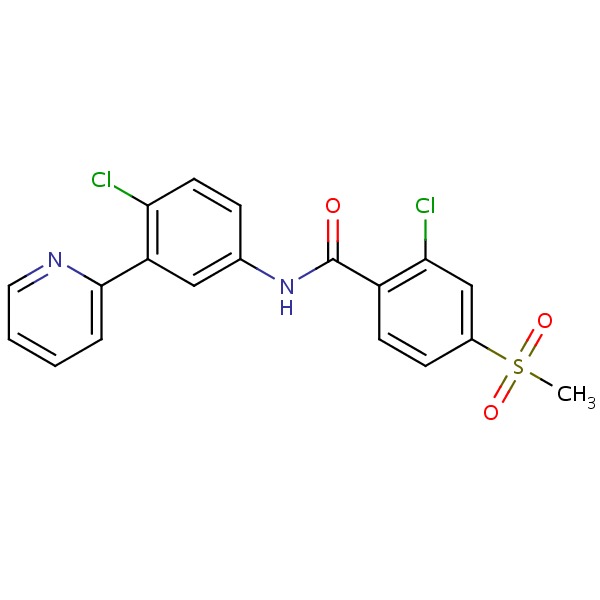 |
ANNOTATED BIBLIOGRAPHY
References updated: 25 June 2018
- Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999.(Review of hepatotoxicity published in 1999 before the availability of tyrosine kinase receptor inhibitors such as vismodegib).
- DeLeve LD. Erlotinib. Cancer chemotherapy. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 556.(Review of hepatotoxicity of cancer chemotherapeutic agents discusses several tyrosine kinase inhibitors including imatinib, gefitinib, erlotinib and crizotinib, but not vismodegib).
- Chabner BA, Barnes J, Neal J, Olson E, Mujagic H, Sequist L, Wilson W, et al. Targeted therapies: tyrosine kinase inhibitors, monoclonal antibodies, and cytokines. In, Brunton LL, Chabner BA, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 1731-54.(Textbook of pharmacology and therapeutics).
- Von Hoff DD, LoRusso PM, Rudin CM, Reddy JC, Yauch RL, Tibes R, Weiss GJ, et al. Inhibition of the hedgehog pathway in advanced basal-cell carcinoma. N Engl J Med 2009; 361: 1164-72. [PubMed: 19726763](Among 33 patients with metastatic or locally advanced basal cell carcinoma treated with vismodegib in varying doses, 18 [55%] had an objective response and adverse events included fatigue, hyponatremia, weight loss, dyspnea and prolonged QTc interval; no mention of ALT elevations, but one patient had an Alk P elevation ≥3 times ULN).
- LoRusso PM, Rudin CM, Reddy JC, Tibes R, Weiss GJ, Borad MJ, Hann CL, et al. Phase I trial of hedgehog pathway inhibitor vismodegib (GDC-0449) in patients with refractory, locally advanced or metastatic solid tumors. Clin Cancer Res 2011; 17: 2502-11. [PMC free article: PMC5244484] [PubMed: 21300762](Among 68 patients with locally advanced or metastatic solid tumors treated with vismodegib, tumor responses occurred in 20 patients [29%], all but one with basal cell carcinoma; difficult side effects included hyponatremia, abdominal pain and fatigue; no mention of liver injury).
- Sekulic A, Migden MR, Oro AE, Dirix L, Lewis KD, Hainsworth JD, Solomon JA, et al. Efficacy and safety of vismodegib in advanced basal-cell carcinoma. N Engl J Med 2012; 366: 2171-9. [PMC free article: PMC5278761] [PubMed: 22670903](Among 96 patients with advanced or metastatic basal cell cancer treated with vismodegib, the response rate was 40% and side effects were common including muscle spasms, alopecia, dysgeusia, weight loss, fatigue, nausea and diarrhea, and were severe in 26% of patients).
- Tang JY, Mackay-Wiggan JM, Aszterbaum M, Yauch RL, Lindgren J, Chang K, Coppola C, et al. Inhibiting the hedgehog pathway in patients with the basal-cell nevus syndrome. N Engl J Med 2012; 366: 2180-8. [PMC free article: PMC4362529] [PubMed: 22670904](Among 41 patients with basal cell nevus syndrome, vismodegib therapy was associated with a lower rate of new tumors and decrease in size of existing tumors compared to placebo, but was associated with a high rate of side effects and 54% stopped therapy because of side effects; no mention of ALT elevations or hepatotoxicity).
- Vismodegib (Erivedge) for basal cell carcinoma. Med Lett Drugs Ther 2012; 54 (1394): 53-4. [PubMed: 22777303](Concise summary of mechanism of action, efficacy, safety and cost of vismodegib for basal cell carcinoma shortly after its approval in the US mentions that side effects are common, but not life-threatening).
- Spraggs CF, Xu CF, Hunt CM. Genetic characterization to improve interpretation and clinical management of hepatotoxicity caused by tyrosine kinase inhibitors. Pharmacogenomics 2013; 14: 541-54. [PubMed: 23556451](Review of genetic associations of serum ALT and bilirubin elevations during therapy with tyrosine kinase inhibitors, focusing on lapatinib and pazopanib).
- Shah RR, Morganroth J, Shah DR. Hepatotoxicity of tyrosine kinase inhibitors: clinical and regulatory perspectives. Drug Saf 2013; 36: 491-503. [PubMed: 23620168](Review of the hepatotoxicity of 18 tyrosine kinase inhibitors approved for use in cancer in the US as of 2013; vismodegib is not discussed).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Sonidegib.[LiverTox: Clinical and Researc...]Review Sonidegib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review A comprehensive review of the role of the hedgehog pathway and vismodegib in the management of basal cell carcinoma.[Curr Med Res Opin. 2015]Review A comprehensive review of the role of the hedgehog pathway and vismodegib in the management of basal cell carcinoma.Erdem GU, Sendur MA, Ozdemir NY, Yazıcı O, Zengin N. Curr Med Res Opin. 2015 Apr; 31(4):743-56. Epub 2015 Mar 17.
- Review Vismodegib and the hedgehog pathway: a new treatment for basal cell carcinoma.[Clin Ther. 2012]Review Vismodegib and the hedgehog pathway: a new treatment for basal cell carcinoma.Cirrone F, Harris CS. Clin Ther. 2012 Oct; 34(10):2039-50. Epub 2012 Oct 1.
- Inhibiting the hedgehog pathway in patients with the basal-cell nevus syndrome.[N Engl J Med. 2012]Inhibiting the hedgehog pathway in patients with the basal-cell nevus syndrome.Tang JY, Mackay-Wiggan JM, Aszterbaum M, Yauch RL, Lindgren J, Chang K, Coppola C, Chanana AM, Marji J, Bickers DR, et al. N Engl J Med. 2012 Jun 7; 366(23):2180-8.
- Review Futibatinib.[LiverTox: Clinical and Researc...]Review Futibatinib.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Vismodegib - LiverToxVismodegib - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...