NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Prucalopride is a serotonin type 4 (5-HT4) receptor agonist that has potent prokinetic activity and is used as therapy for chronic idiopathic constipation. Prucalopride has been associated with a minimal rate of transient serum enzyme elevations during therapy and has not been implicated in cases of clinically apparent liver injury with jaundice.
Background
Prucalopride (proo kal' oh pride) is a highly selective serotonin type 4 (5-HT4) receptor agonist that increases the release of serotonin by the specialized enterochromaffin cells in the mucosa of the gut and stimulates intestinal peristalsis and tone. Serotonin (5-HT) is released in response to chemical and mechanical stimulation and acts through the type 4 receptors that are common in the intestinal mucosa to increase peristalsis and intestinal tone. 5-HT4 receptors are also found in the central nervous system, urinary bladder and atria of the heart, which may explain some of the adverse effects of 5-HT4 receptor agonists. Prucalopride was found to improve symptoms of bloating and gastric distension in patients with gastroparesis and to decrease symptoms of reflux in patients with GERD. Prucalopride was approved in the United States in 2018 for treatment of idiopathic chronic constipation. Prucalopride is available in tablets of 1 and 2 mg under the brand name Motegrity. The recommended dose in adults is 2 mg once daily with a lower dose recommended for patients with renal impairment (creatinine clearance less than 30 mL/min). Adverse events include headache, abdominal pain, nausea, diarrhea, abdominal bloating, dizziness, flatulence and fatigue. Uncommon but potentially severe adverse events include depression, suicidal ideation and behavior and hypersensitivity reactions. Two 5-HT4 receptor agonists were approved for treatment of chronic constipation in the past (cisapride in 1993, tegaserod in 2002), both of which were subsequently withdrawn from general use because of serious adverse events including cardiac arrhythmias and prolongation of the QTc interval. Prucalopride is a more highly selective 5HT4 receptor agonist and has not been linked to an increased rate of these cardiac adverse events.
Hepatotoxicity
Prucalopride therapy was associated with a low rate of serum enzyme elevations during therapy (<1%) that was not different from that of placebo recipients. The elevations noted were mild and transient and did not required dose adjustment. In the many large clinical trials of prucalopride therapy in patients with chronic constipation, there were no reports of clinically apparent liver injury and since its approval there have been no published reports of liver injury attributed to prucalopride.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which prucalopride might cause liver injury is unknown. It is used in low total doses which may explain its relative lack of hepatotoxicity. Prucalopride is metabolized in the liver, largely via CYP 3A4 and is a substrate for P-glycoprotein. Prucalopride is susceptible to drug-drug interactions with agents that induce or inhibit CYP 3A4 or P-glycoprotein.
Drug Classes: Gastrointestinal Agents, Agents for Constipation, Irritable Bowel Syndrome Agents
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Prucalopride – Motegrity®
DRUG CLASS
Gastrointestinal Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Prucalopride | 179474-81-8 | C18-H26-Cl-N3-O3 |
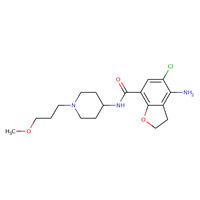 |
ANNOTATED BIBLIOGRAPHY
References updated: 25 April 2019
- Zimmerman HJ. Miscellaneous drugs and diagnostic chemicals. In, Zimmerman, HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999: pp. 717-8.(Expert review of hepatotoxicity published in 1999; mentions that cisapride, a serotonin type 4 receptor agonist, was reported to lead to one case of liver injury [hepatocellular] during a decade of use).
- Sharkey KA, McNaughton WK. Gastrointestinal motility and water flux, emesis, and biliary and pancreatic disease. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 921-44.(Textbook of pharmacology and therapeutics; the serotonin type 4 receptor agonists are used predominantly for treatment of diseases of intestinal motility and irritable bowel syndrome).
- https://www
.accessdata .fda.gov/drugsatfda_docs /nda/2018/210166Orig1s000TOC.cfm . (FDA Drug Approvals website that has product labels [package inserts], letters of approval and full FDA scientific review of the new drug application for safety and efficacy; mentions that review of 6 studies in more than 3000 treated patients did not raise clinical safety concerns and that there was no evidence of drug induced liver injury). - Camilleri M, Kerstens R, Rykx A, Vandeplassche L. A placebo-controlled trial of prucalopride for severe chronic constipation. N Engl J Med 2008; 358: 2344-54. [PubMed: 18509121](Among 620 adults with chronic idiopathic constipation treated with prucalopride [2 or 4 mg] vs placebo once daily for 12 weeks, response rates were 31% and 28% vs 12% and adverse events included diarrhea [13.5% and 18.6% vs 5.3%] and nausea [22% vs 8%], but there were no differences in changes in clinical test results among the different treatment groups).
- Camilleri M, Beyens G, Kerstens R, Robinson P, Vandeplassche L. Safety assessment of prucalopride in elderly patients with constipation: a double-blind, placebo-controlled study. Neurogastroenterol Motil 2009; 21: 1256-e117. [PubMed: 19751247](Among 89 elderly nursing home residents treated with prucalopride [0.5, 1 and 2 mg] vs placebo once daily for 28 days, adverse events included diarrhea, abdominal pain but there were “no clinically relevant changes or dose-related effects in the clinical laboratory parameters”).
- Camilleri M, Van Outryve MJ, Beyens G, Kerstens R, Robinson P, Vandeplassche L. Clinical trial: the efficacy of open-label prucalopride treatment in patients with chronic constipation - follow-up of patients from the pivotal studies. Aliment Pharmacol Ther 2010; 32: 1113-23. [PubMed: 21039673](Among 1455 patients with chronic idiopathic constipation enrolled in a continuation trial of prucalopride [2 or 4 mg daily], satisfaction with bowel function remained high [57% to 67%] and adverse events leading to discontinuation included headache, nausea, diarrhea and abdominal pain; no mention of ALT elevations or hepatotoxicity).
- Sloots CE, Rykx A, Cools M, Kerstens R, De Pauw M. Efficacy and safety of prucalopride in patients with chronic noncancer pain suffering from opioid-induced constipation. Dig Dis Sci 2010; 55: 2912-21. [PMC free article: PMC2943574] [PubMed: 20428949](Among 196 patients with opioid induced constipation treated with prucalopride or placebo for 4 weeks, response rates were higher with prucalopride [2 mg 36%, 4 mg 40% vs placebo 23%] and “there were no clinically relevant differences between groups in…laboratory measures”).
- Müller-Lissner S, Rykx A, Kerstens R, Vandeplassche L. A double-blind, placebo-controlled study of prucalopride in elderly patients with chronic constipation. Neurogastroenterol Motil 2010; 22: 991-8. [PubMed: 20529205](Among 300 elderly persons with chronic idiopathic constipation treated with prucalopride [1,2 or 4 mg] vs placebo daily for 4 weeks, clinical responses were more frequent with the higher doses of prucalopride and adverse events were typically headache and gastrointestinal complaints, while there were no clinically significant differences in laboratory assessments).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were attributed to prokinetic agents or the 5-HT4 receptor agonists).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol 2010; 70: 721-8. [PMC free article: PMC2997312] [PubMed: 21039766](Among 624,673 adverse event reports in children between 2000 and 2006 in the WHO VigiBase, 1% were hepatic, but no prokinetic agent or 5-HT4 receptor agonist was listed among the 41 most commonly implicated agents).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 114: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none were attributed to prokinetic agents or the 5-HT4 receptor agonists).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol 2014; 13: 231-9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, none of which were attributed to prokinetic agents or 5-HT4 receptor agonists).
- Mugie SM, Korczowski B, Bodi P, Green A, Kerstens R, Ausma J, Ruth M, et al. Prucalopride is no more effective than placebo for children with functional constipation. Gastroenterology 2014; 147: 1285-95. [PubMed: 25239590](Among 213 children with idiopathic constipation treated with prucalopride or placebo for 8 weeks, response rates were similar in both groups [17% vs 18%] as were adverse event rates [70% vs 61%], and changes in clinical chemistry results were minimal and similar in the two groups).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, one case was attributed to metoclopramide, but none to other prokinetic agents).
- Piessevaux H, Corazziari E, Rey E, Simren M, Wiechowska-Kozlowska A, Kerstens R, Cools M, et al. A randomized, double-blind, placebo-controlled trial to evaluate the efficacy, safety, and tolerability of long-term treatment with prucalopride. Neurogastroenterol Motil 2015; 27: 805-15. [PubMed: 25808103](Among 361 adults with chronic idiopathic constipation treated with prucalopride [2 mg daily] vs placebo for 24 weeks, clinical response rates were similar in both groups [25% vs 21%] as were adverse events [42% vs 42%]; there were no hepatic serious adverse events and no mention of ALT elevations or hepatotoxicity).
- Yiannakou Y, Piessevaux H, Bouchoucha M, Schiefke I, Filip R, Gabalec L, Dina I, et al. A randomized, double-blind, placebo-controlled, phase 3 trial to evaluate the efficacy, safety, and tolerability of prucalopride in men with chronic constipation. Am J Gastroenterol 2015; 110: 741-8. [PMC free article: PMC4424376] [PubMed: 25869393](Among 374 men with chronic idiopathic constipation treated with prucalopride or placebo, clinical responses were more frequent with prucalopride [38% vs 18%] as were adverse events [42% vs 34%], and mean changes from baseline in clinical laboratory results were “generally small” and were not considered clinically relevant).
- Camilleri M, Piessevaux H, Yiannakou Y, Tack J, Kerstens R, Quigley EM, Ke M, et al. Efficacy and safety of prucalopride in chronic constipation: an integrated analysis of six randomized, controlled clinical trials. Dig Dis Sci 2016; 61: 2357-72. [PMC free article: PMC4943977] [PubMed: 27056037](Pooled analysis of 7 placebo controlled trials of prucalopride in chronic idiopathic constipation identified 2484 patients among whom response rates were higher with prucalopride [28% vs 13%] and adverse events [mean duration of exposure=87 days] more frequent with prucalopride [63% vs 53%], but were mostly mild and none were fatal, while rates of abnormalities of laboratory tests were low and similar in both groups).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Use of prucalopride in adults with chronic idiopathic constipation.[Expert Rev Clin Pharmacol. 2019]Review Use of prucalopride in adults with chronic idiopathic constipation.Vijayvargiya P, Camilleri M. Expert Rev Clin Pharmacol. 2019 Jul; 12(7):579-589. Epub 2019 May 23.
- Review Clinical Efficacy and Safety Profile of Prucalopride in Chronic Idiopathic Constipation.[Cureus. 2019]Review Clinical Efficacy and Safety Profile of Prucalopride in Chronic Idiopathic Constipation.Tameez Ud Din A, Khan AH, Bajwa H, Maqsood MH, Malik MN. Cureus. 2019 Apr 4; 11(4):e4382. Epub 2019 Apr 4.
- Review Efficacy and safety of prucalopride in adults and children with chronic constipation.[Expert Opin Pharmacother. 2015]Review Efficacy and safety of prucalopride in adults and children with chronic constipation.Diederen K, Mugie SM, Benninga MA. Expert Opin Pharmacother. 2015 Feb; 16(3):407-16. Epub 2014 Dec 24.
- Review Serotonin 5-HT4 Receptor Agonists.[LiverTox: Clinical and Researc...]Review Serotonin 5-HT4 Receptor Agonists.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Prucalopride is a partial agonist through human and porcine atrial 5-HT4 receptors: comparison with recombinant human 5-HT4 splice variants.[Naunyn Schmiedebergs Arch Phar...]Prucalopride is a partial agonist through human and porcine atrial 5-HT4 receptors: comparison with recombinant human 5-HT4 splice variants.Krobert KA, Brattelid T, Levy FO, Kaumann AJ. Naunyn Schmiedebergs Arch Pharmacol. 2005 Jun; 371(6):473-9. Epub 2005 Jul 13.
- Prucalopride - LiverToxPrucalopride - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...