NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Oxaprozin is a long acting nonsteroidal antiinflammatory drug (NSAID) available by prescription only which is used for therapy of chronic arthritis. Oxaprozin has been linked to rare instances of idiosyncratic drug induced liver disease.
Background
Oxaprozin (ox" a proe' zin) belongs to the propionic acid derivative class of NSAIDs similar to naproxen and ibuprofen. Like other NSAIDs, oxaprozin is a potent cyclo-oxygenase (Cox-1 and -2) inhibitor which leads to decrease in synthesis of proinflammatory prostaglandins, which are potent mediators of pain and inflammatory pathways. Oxaprozin has analgesic as well as antipyretic and antiinflammatory activities. Because of its long half-life, oxaprozin can be given once daily. Oxaprozin was approved in the United States in 1992 and is still widely used. Oxaprozin is indicated for the treatment of chronic arthritis due to osteoarthritis, rheumatoid arthritis and juvenile rheumatoid arthritis. Oxaprozin is available in capsules of 600 mg in several generic forms and under the brand name Daypro. The recommended dose in adults is 600 to 1200 mg once daily. As with other NSAIDs, oxaprozin is generally well tolerated, but side effects can include headache, dizziness, somnolence, dyspepsia, nausea, abdominal discomfort, heartburn, peripheral edema and hypersensitivity reactions. Rare but serious adverse events from NSAIDs include gastrointestinal ulceration and bleeding, increased risk for cardiovascular disease, renal dysfunction, exacerbation of asthma and hypersensitivity reactions including anaphylaxis, exfoliative dermatitis and Stevens Johnson syndrome.
Hepatotoxicity
Prospective studies show that up to 15% of patients taking oxaprozin chronically experience at least transient serum aminotransferase elevations. These usually resolve even with drug continuation. Marked aminotransferase elevations (>3 fold elevated) occur in approximately 1% of patients.
Clinically apparent liver injury with jaundice from oxaprozin is rare (~1 per 100,000 person-years of use) and it is rarely listed in large surveys of cases of drug induced liver injury. The usual clinical presentation is an acute hepatitis-like picture arising 2 to 8 weeks after starting the medication. The pattern of injury is typically hepatocellular, but mixed hepatocellular-cholestatic cases have been described. Symptoms may include allergic manifestations such as fever, rash, arthralgias and facial edema. Autoantibody formation is rare. Liver biopsy findings are hepatocellular necrosis with prominent periportal and lobular eosinophilic infiltration suggestive of drug induced acute hepatitis. Recovery may be delayed for several days, but is usually complete within one to two months. At least one case of acute liver failure attributed to oxaprozin has been published.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of oxaprozin hepatotoxicity is not known, but the allergic phenomena that accompany clinically apparent injury suggests an immunoallergic cause. Rechallenge leads to rapid recurrence and should be avoided.
Outcome and Management
Severity ranges from asymptomatic elevations in serum aminotransferase levels, to symptomatic hepatitis with or without jaundice (Case 1), to acute liver failure. Rapid improvement in symptoms and complete recovery are expected after discontinuing the medication. Complete recovery may take several months. Cross sensitivity to liver injury among the various NSAIDs has not been well studied or described, but in several case reports patients with oxaprozin associated hepatotoxicity had previously tolerated therapy with other propionic acid derivative NSAIDs (such as ibuprofen, naproxen or ketoprofen). Nevertheless, patients with oxaprozin induced clinically apparent liver injury should be carefully monitored during the first few weeks of starting a different NSAID.
Drug Class: Nonsteroidal Antiinflammatory Drugs
CASE REPORT
Case 1. Acute immunoallergic hepatitis due to oxaprozin.(1)
A 45 year old woman was given oxaprozin (1200 mg once daily) for painful “tennis elbow” (epicondylitis). She had a past medical history of asthma and an allergic reaction to sulfonamides. After 3 weeks of taking oxaprozin, she developed dark urine, anorexia, high fevers and right upper quadrant pain. All of her medications were stopped, but in the next few days she developed worsening symptoms, itching and a maculopapular rash. Physical examination revealed tenderness over the liver and spleen. Tests for viral hepatitis and autoimmune markers were negative. An abdominal ultrasound showed enlargement of the liver and spleen and gallstones, but no dilatation of bile ducts. CT scan was normal. A liver biopsy showed severe lobular hepatitis with mixed inflammatory response and numerous eosinophils. One month after stopping oxaprozin, her symptoms had resolved and ALT and alkaline phosphatase levels had improved. Two months after stopping, all liver tests were normal.
Key Points
| Medication: | Oxaprozin (1200 mg daily for 14 days) |
|---|---|
| Pattern: | Hepatocellular (R=7.5) |
| Severity: | 1+ (bilirubin less than 2.5 mg%) |
| Latency: | 3 weeks |
| Recovery: | Rapid and complete |
| Other medications: | Albuterol, fluticasone, ethinyl estradiol/levonorgestrel |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| Pre | 20 | ||||
| 0 | Oxaprozin started [1200 mg daily] | ||||
| 22 days | 76 | 30 | 0.5 | Dark urine, RUQ pain | |
| 24 days | 0 | 242 | 107 | 0.8 | Oxaprozin stopped |
| 28 days | 4 days | 551 | 254 | 1.9 | |
| 31 days | 8 days | 476 | 287 | 1.8 | Rash and pruritis |
| 35 days | 12 days | Liver biopsy | |||
| 41 days | 18 days | 775 | 274 | 1.4 | |
| 2 months | 1 month | 234 | 147 | 1.1 | |
| 3 months | 2 months | 35 | 95 | 0.7 | |
| 7 months | 6 months | 18 | 88 | ... | |
| Normal Values | <42 | <115 | <1.2 | ||
Comment
The sudden onset of mild, but symptomatic liver disease with rash and fever within a month of starting oxaprozin suggests an allergic hepatitis-like syndrome and not merely a benign elevation in serum aminotransferase levels. Indeed, serum ALT and bilirubin levels continued to climb and remained high for several weeks after stopping oxaprozin. While the patient reported jaundice and dark urine, serum total bilirubin levels were never recorded to be above 2.5 mg/dL – the level typically used to define jaundice. Liver test abnormalities returned to baseline within 2 months of onset. In view of the allergic components of the hepatotoxicity, rechallenge is best avoided. Interestingly, she had received naproxen (a propionic acid derivative like oxaprozin) in the past without incident, so that rechallenge with another NSAID with careful monitoring might be appropriate, particularly in view of the ubiquity of these agents and the high likelihood that she would receive one in the future.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Oxaprozin – Generic, Daypro®
DRUG CLASS
Nonsteroidal Antiinflammatory Drugs
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Oxaprozin | 21256-18-8 | C18-H15-N-O3 |
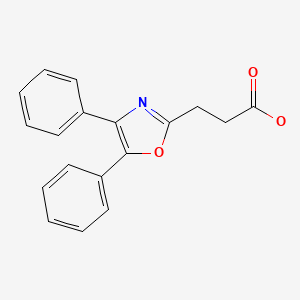
|
CITED REFERENCES
- 1.
- Schmeltzer PA, Kosinski AS, Kleiner DE, Hoofnagle JH, Stolz A, Fontana RJ, Russo MW., Drug-Induced Liver Injury Network (DILIN). Liver injury from nonsteroidal anti-inflammatory drugs in the United States. Liver Int. 2016;36:603–9. [PMC free article: PMC5035108] [PubMed: 26601797]
ANNOTATED BIBLIOGRAPHY
References updated: 20 March 2020
Abbreviations: NSAIDs, nonsteroidal antiinflammatory drugs.
- Zimmerman HJ. Drugs used to treat rheumatic and musculospastic disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 517-53.(Expert review of hepatotoxicity published in 1999; overt hepatitis due to oxaprozin is rare, but there have been several unreported cases of hepatocellular jaundice during oxaprozin use).
- Lewis JH, Stine JG. Nonsteroidal anti-inflammatory drugs and leukotriene receptor antagonists: pathology and clinical presentation of hepatotoxicity. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd Edition. Amsterdam: Elsevier, 2013. pp. 370-402.(Review of hepatotoxicity of NSAIDs mentions that overt hepatitis due to oxaprozin is rare, but two case reports have been published).
- Grossner T, Smyth EM, Fitzgerald GA. Pharmacotherapy of inflammation, fever, pain, and gout. In, Brunton LL, Hilal-Dandan R, Knollman BC. Goodman & Gilman’s The pharmacological basis of therapeutics, 13th ed. New York: McGraw-Hill, 2018. pp. 685-709.(Textbook of pharmacology and therapeutics).
- Janssen FW, Jusko WJ, Chiang ST, Kirkman SK, Southgate PJ, Coleman AJ, et al. Metabolism and kinetics of oxaprozin in normal subjects. Clin Pharmacol Ther. 1980;27:352–62. [PubMed: 7357792](Extensive review of the pharmacokinetics of oxaprozin showing that it is well absorbed orally, metabolized by the liver, excreted in the urine and has a long serum half-life, perhaps because it is highly protein bound; long half-life allows for once daily dosing).
- Zimmerman HJ. Hepatic effects of oxaprozin. Semin Arthritis Rheum. 1986;15 Suppl 2:35–9.(Classic analysis of hepatic injury in the large clinical studies of oxaprozin, reporting some degree of AST elevation in 15.4% of 1135 subjects, usually transient, mild and asymptomatic; elevations >3x ULN occurred in 12 [1.1%] patients with values 95-433 U/L, one subject developed symptoms, but no jaundice).
- Freeland GR, Northington RS, Hedrich DA, Walker BR. Hepatic safety of two analgesics used over the counter: ibuprofen and aspirin. Clin Pharmacol Ther. 1988;43:473–9. [PubMed: 3365912](Prospective study of safety of ibuprofen, aspirin and oxaprozin in 1468 patients; AST elevations occurred in 5-15% of those on oxaprozin, 6-16% aspirin and 3% ibuprofen, but were above 3 times ULN in only 0.4-1% on oxaprozin, 5% aspirin and none ibuprofen).
- Miller LG. Oxaprozin: a once-daily nonsteroidal anti-inflammatory drug. Clin Pharm. 1992;11:591–603. [PubMed: 1617910](Thorough summary of chemistry, pharmacology, pharmacokinetics, clinical efficacy and safety of oxaprozin based upon prelicensure studies; no new information on hepatotoxicity).
- Purdum PP 3rd, Shelden SL, Boyd JW, Shiffman ML. Oxaprozin-induced fulminant hepatitis. Ann Pharmacother. 1994;28:1159–61. [PubMed: 7841569](56 year old woman developed jaundice 6 weeks after switching from ketoprofen to oxaprozin [bilirubin 32.1 mg/dL, ALT 4325 U/L, Alk P 335 U/L], with progressive hepatic failure and death).
- Weaver A, Rubin B, Caldwell J, McMahon FG, Lee D, Makarowski W, et al. Comparison of the efficacy and safety of oxaprozin and nabumetone in the treatment of patients with osteoarthritis of the knee. Clin Ther. 1995;17:735–45. [PubMed: 8565037](Review of safety of oxaprozin without new information on hepatotoxicity).
- Manoukian AV, Carson JL. Nonsteroidal anti-inflammatory drug-induced hepatic disorders. Incidence and prevention. Drug Saf. 1996;15:64–71. [PubMed: 8862964](Review of hepatotoxicity of NSAIDs, recapitulation of oxaprozin data presented by Zimmerman [1986]).
- Kethu SR, Rukkannagari S, Lansford CL. Oxaprozin-induced symptomatic hepatotoxicity. Ann Pharmacother. 1999;33:942–4. [PubMed: 10492496](41 year old man developed jaundice 6 weeks after starting oxaprozin for shoulder pain [bilirubin 3.7 mg/dL, ALT 1950 U/L, Alk P 357 U/L], resolving within 8 weeks of stopping).
- Lapeyre-Mestre M, de Castro AM, Bareille MP, Garcia del Pozo J, Requejo AA, Arias LM, Montastruc J-L, et al. Non-steroidal anti-inflammatory drug-related hepatic damage in France and Spain: analysis from national spontaneous reporting systems. Fundam Clin Pharmacol. 2006;20:391–5. [PubMed: 16867024](Survey of NSAID adverse drug reaction reports in Spain and France between 1982 and 2001; oxaprozin is not listed among 24 NSAIDs analyzed).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, NSAIDs were implicated as a sole agent in 8 cases [4 diclofenac, 2 celecoxib, 1 meloxicam and 1 oxaprozin] and as one of several agents in 3 cases [1 diclofenac, 1 celecoxib, 1 ibuprofen]: Case 1).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury and 7 to NSAIDs, including 4 to bromfenac, 2 diclofenac and 1 etodolac, but none to oxaprozin, ibuprofen or naproxen).
- Bessone F. Non-steroidal anti-inflammatory drugs: What is the actual risk of liver damage? World J Gastroenterol. 2010;16:5651–61. [PMC free article: PMC2997980] [PubMed: 21128314](Review of estimated frequency of drug induced liver injury due to NSAIDs from large published epidemiological studies; oxaprozin not discussed).
- Suzuki A, Andrade RJ, Björnsson E, Lucena MI, Lee WM, Yuen NA, Hunt CM, et al. Drugs associated with hepatotoxicity and their reporting frequency of liver adverse events in VigiBase: unified list based on international collaborative work. Drug Saf. 2010;33:503–22. [PubMed: 20486732](The combination of several large data sources identified 385 different drugs to be linked to liver injury and 107 to acute liver failure, the most commonly implicated NSAIDs being diclofenac, ibuprofen, naproxen, nimesulide, piroxicam, and sulindac; oxaprozin not mentioned).
- Zhou Y, Yang L, Liao Z, He X, Zhou Y, Guo H. Epidemiology of drug-induced liver injury in China: a systematic analysis of the Chinese literature including 21 789 patients. Eur J Gastroenterol Hepatol. 2013;25:825–9. [PubMed: 23510965](Search of 3 electronic databases of the Chinese medical literature from 1994-2011 identified 279 reports on a total of 24,111 patients with drug induced liver injury, the most commonly implicated being antituberculosis agents [31%], HDS products [19%], antibiotics [10%] and NSAIDs [7.6%], and the most frequent individual NSAIDs being acetaminophen, ibuprofen, indometacin, aspirin and phenylbutazone).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](Prospective analysis of all cases of drug induced liver injury in Iceland between 2010-11 identified 97 cases [19 per 100,000 inhabitants], 6 of which were attributed to diclofenac; no other NSAID mentioned).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, the most common class of implicated agents being NSAIDs [n=62, 32%], and specific agents were nimesulide [n=53], piroxicam [5], diclofenac [2], gold salts [1], and naproxen [1]).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 28 were attributed to NSAIDs [Schmeltzer 2016]).
- Schmeltzer PA, Kosinski AS, Kleiner DE, Hoofnagle JH, Stolz A, Fontana RJ, Russo MW., Drug-Induced Liver Injury Network (DILIN). Liver injury from nonsteroidal anti-inflammatory drugs in the United States. Liver Int. 2016;36:603–9. [PMC free article: PMC5035108] [PubMed: 26601797](Among 1221 cases of drug induced liver injury enrolled in a prospective, US database between 2004 and 2014, 30 cases [2.5%] were attributed to NSAIDs, most commonly diclofenac [n=16], but also celecoxib [3], meloxicam [3], etodolac [2], ibuprofen [2], oxaprozin [2], valdecoxib [1] and sulindac [1]).
- Donati M, Conforti A, Lenti MC, Capuano A, Bortolami O, Motola D, Moretti U, et al. DILI-IT Study Group. Risk of acute and serious liver injury associated to nimesulide and other NSAIDs: data from drug-induced liver injury case-control study in Italy. Br J Clin Pharmacol. 2016;82:238–48. [PMC free article: PMC4917796] [PubMed: 26991794](Among 179 cases of acute liver injury and 1770 controls admitted to 9 Italian hospitals between 2010 and 2014, NSAIDs used more frequently in cases compared to controls included nimesulide [17% vs 10%: odds ratio 1.88] and ibuprofen [14% vs 10%: odds ratio 1.59] and risk was higher in those taking higher doses).
- Zoubek ME, González-Jimenez A, Medina-Cáliz I, Robles-Díaz M, Hernandez N, Romero-Gómez M, Bessone F, et al. High Prevalence of ibuprofen drug-induced Liver injury in Spanish and Latin-American registries. Clin Gastroenterol Hepatol. 2018;16:292–4. [PubMed: 28782674](Analysis of a Spanish and Latin-American registries identified 73 cases of NSAID induced liver injury, the most common agents being nimesulide [38%], diclofenac [34%] and ibuprofen [17%]; other agents not mentioned).
- Tujios SR, Lee WM. Acute liver failure induced by idiosyncratic reaction to drugs: challenges in diagnosis and therapy. Liver Int. 2018;38:6–14. [PMC free article: PMC5741491] [PubMed: 28771932](Review of acute liver failure and the contribution of drug induced liver injury, of which 5% were due to NSAIDs, most commonly diclofenac and etodolac).
- Meunier L, Larrey D. Recent advances in hepatotoxicity of non-steroidal anti-inflammatory drugs. Ann Hepatol. 2018;17:187–91. [PubMed: 29469052](Review of the hepatotoxicity of NSAIDS mentions the most commonly implicated are diclofenac, nimesulide, sulindac, ibuprofen, piroxicam, naproxen and aspirin).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Nabumetone.[LiverTox: Clinical and Researc...]Review Nabumetone.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Oxaprozin-induced symptomatic hepatotoxicity.[Ann Pharmacother. 1999]Oxaprozin-induced symptomatic hepatotoxicity.Kethu SR, Rukkannagari S, Lansford CL. Ann Pharmacother. 1999 Sep; 33(9):942-4.
- Oxaprozin-induced fulminant hepatitis.[Ann Pharmacother. 1994]Oxaprozin-induced fulminant hepatitis.Purdum PP 3rd, Shelden SL, Boyd JW, Shiffman ML. Ann Pharmacother. 1994 Oct; 28(10):1159-61.
- Oxaprozin and piroxicam, nonsteroidal antiinflammatory drugs with long half-lives: effect of protein-binding differences on steady-state pharmacokinetics.[J Clin Pharmacol. 1997]Oxaprozin and piroxicam, nonsteroidal antiinflammatory drugs with long half-lives: effect of protein-binding differences on steady-state pharmacokinetics.Karim A, Noveck R, McMahon FG, Smith M, Crosby S, Adams M, Wilton J. J Clin Pharmacol. 1997 Apr; 37(4):267-78.
- Review Oxaprozin: a once-daily nonsteroidal anti-inflammatory drug.[Clin Pharm. 1992]Review Oxaprozin: a once-daily nonsteroidal anti-inflammatory drug.Miller LG. Clin Pharm. 1992 Jul; 11(7):591-603.
- Oxaprozin - LiverToxOxaprozin - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...