NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Naltrexone is a synthetic opioid antagonist used in prevention of relapse of opiate addiction and alcoholism. Naltrexone has been associated with low rates of serum enzyme elevations during therapy and with rare instances of clinically apparent liver injury.
Background
Naltrexone (nal trex' one) is orally available opioid antagonist which blocks the euphoric effects of administered opiates. Naltrexone is a relatively pure antagonist and has no analgesic activity. Naltrexone has been shown to aid in maintenance of an opioid-free state in detoxified patients and to help in other addictions. Naltrexone was approved for use in the therapy of opioid and alcohol dependence in the United States in 1984. Naltrexone is available in tablets of 50 mg in several generic formulations and under the brand name Revia. More recently, injectable suspensions of naltrexone (Vivitrol), injectable implants and solutions of methylnaltrexone (Relistor) have become available for therapy of opioid dependence. Fixed combinations of naltrexone and bupropion (Contrave) have been approved as a weight loss agent. The usually recommended dose of the oral preparation is 50 mg daily. The injectable suspension is given intramuscularly and the solution subcutaneously every 4 weeks. Naltrexone must be started carefully in patients with opioid abuse to avoid precipitous withdrawal reactions. The most common side effects are headache, sleep disturbance, anxiety, dizziness, nausea, diarrhea and rash.
Hepatotoxicity
Naltrexone therapy is typically given to patients with a high background rate of liver disease (injection drug use or alcoholism) and has been associated with variable rates of serum enzyme elevations (0% to 50%), values above 3 times the upper limit of normal occurring in approximately 1% of patients and occasionally leading to drug discontinuation. However, several studies have shown that the rate of ALT elevations during naltrexone therapy is similar to that with placebo. Most serum aminotransferase elevations during naltrexone therapy are mild and self-limiting, resolving even with continuation of therapy. While several rare instances of acute, clinically apparent liver disease have been reported in patients taking naltrexone, the role of the medication in the liver injury has not always been clear and there has been no clear description of the clinical features of the injury. Thus, while often considered hepatotoxic, naltrexone has not been definitively linked to cases of clinically apparent liver injury.
Likelihood score: E* (unproven but suspected cause of clinically apparent liver injury).
Mechanism of Injury
Naltrexone is a relatively pure opioid antagonist and is rapidly metabolized by the liver to inactive forms. The cause of hepatic injury is not known, but may be partially dose dependent direct toxicity.
Agents in clinical use in therapy of alcohol abuse and dependence include acamprosate, disulfiram, methadone, and naltrexone.
Drug Class: Substance Abuse Treatment Agents; Opioid Antagonists
Other Drugs in the Class, Opioid Antagonists: Nalmefene, Naloxegol, Naloxone
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Naltrexone – Generic, Revia®, Vivitrol®
DRUG CLASS
Substance Abuse Treatment Agents; Opioid Antagonists
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Naltrexone | 16590-41-3 | C20-H23-N-O4 |
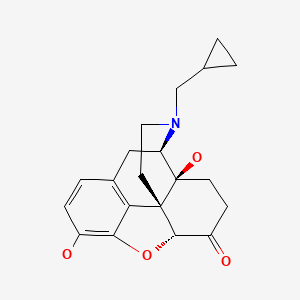
|
ANNOTATED BIBLIOGRAPHY
References updated: 24 March 2020
- Zimmerman HJ. Narcotic analgesics. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 710-11.(Expert review of hepatotoxicity published in 1999; mentions that trials of naltrexone have reported serum aminotransferase elevations in up to 30% of recipients, an effect that appeared to be partially dose dependent).
- Larrey D, Ripault MP. Illegal and recreational compounds. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 456-7.(Review of hepatotoxicity of drugs of abuse, does not discuss naltrexone).
- O’Brien CP. Drug use disorders and addiction. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 433-41.(Textbook of pharmacology and therapeutics).
- Atkinson RL, Berke LK, Drake CR, Bibbs ML, Williams FL, Kaiser DL. Effects of long-term therapy with naltrexone on body weight in obesity. Clin Pharmacol Ther. 1985;38:419–22. [PubMed: 4042525](Modest increases in serum aminotransferase levels occurred in some patients receiving naltrexone in doses of 50-100 mg daily).
- Jonas JM, Gold MS. The use of opiate antagonists in treating bulimia: a study of low-dose versus high-dose naltrexone. Psychiatry Res. 1988;24:195–9. [PubMed: 2841709](Open label study of two doses of naltrexone in 16 patients with bulimia; an effect was found with high dose; one patient had elevated ALT level [64 U/L] at week 6, resolving within 3 weeks of lowering the dose).
- Mitchell JE. Naltrexone and hepatotoxicity. Lancet. 1986;1:1215. [PubMed: 2871452](Among 26 patients with obesity treated with naltrexone [300 mg/day] for 3 weeks, 5 had serum aminotransferase elevations, all of which resolved on drug discontinuation; no details provided).
- Dixon R, Gentile J, Hsu HB, Hsiao J, Howes J, Garg D, Weidler D. Nalmefene: safety and kinetics after single and multiple oral doses of a new opioid antagonist. J Clin Pharmacol. 1987;27:233–9. [PubMed: 3680580](Phase 1 study of safety of single injections and 7 day courses of nalmefene in different doses found no increases in serum aminotransferase levels).
- Campbell M, Anderson LT, Small AM, Locascio JJ, Lynch NS, Choroco MC. Naltrexone in autistic children: a double-blind and placebo-controlled study. Psychopharmacol Bull. 1990;26:130–5. [PubMed: 2196621](Controlled trial of naltrexone for 14 days in 18 autistic children; "liver function tests ... remained within normal limits").
- Hetrick WP, Krutzik MN, Taylor DV, Sandman CA, Rusu L, Martinazzi VP. Naltrexone has no hepatotoxic effects in a self-injurious patient with chronic hepatitis. J Clin Psychopharmacol. 1993;13:453–4. [PubMed: 8120161](28 year old male self-injurious patient with chronic hepatitis B was monitored carefully during 4 month course of oral naltrexone and had no worsening of serum enzymes or bilirubin levels).
- Sax DS, Kornetsky C, Kim A. Lack of hepatotoxicity with naltrexone treatment. J Clin Pharmacol. 1994;34:898–901. [PubMed: 7983232](Prospective monitoring of liver tests in 10 patients with chorea treated with naltrexone for 10 to 36 months found no overall change in mean ALT or AST levels, but minor elevations in 2 patients [peak ALT 80 and 105 U/L] that resolved despite continuing therapy at increasing doses).
- Mason BJ, Ritvo EC, Morgan RO, Salvato FR, Goldberg G, Welch B, Mantero-Atienza E. A double-blind, placebo-controlled pilot study to evaluate the efficacy and safety of oral nalmefene HCl for alcohol dependence. Alcohol Clin Exp Res. 1994;18:1162–7. [PubMed: 7847600](Controlled trial of 12 weeks of nalmefene or placebo in 21 alcohol dependent patients, found no difference in laboratory measures during therapy, serum ALT levels decreasing in abstinent patients).
- Kolmen BK, Feldman HM, Handen BL, Janosky JE. Naltrexone in young autistic children: a double-blind, placebo-controlled crossover study. J Am Acad Child Adolesc Psychiatry. 1995;34:223–31. [PubMed: 7896655](Controlled trial in 13 children with autism found no differences in hepatic enzymes during therapy with naltrexone vs placebo).
- Croop RS, Faulkner EB, Labriola DF. The safety profile of naltrexone in the treatment of alcoholism. Results from a multicenter usage study. The Naltrexone Usage Study Group. Arch Gen Psychiatry. 1997;54:1130–5. [PubMed: 9400350](Controlled trial of naltrexone vs placebo in 865 alcohol dependent patients; common side effects were nausea and headache; ALT levels tended to decrease during therapy and were similar in the two groups: "No clinically important abnormalities were noted...", but 3 patients stopped naltrexone early because of ALT elevations [156, 162 and 563 U/L at weeks 2-8 of therapy], which resolved rapidly thereafter).
- Marrazzi MA, Wroblewski JM, Kinzie J, Luby ED. High-dose naltrexone and liver function safety. Am J Addict. 1997;6:21–9. [PubMed: 9097868](Controlled cross-over trial of 6 weeks of naltrexone [200-400 mg/day] vs placebo in 21 patients with eating disorders, found no elevations in aminotransferase levels during therapy).
- Foss JF, O'Connor MF, Yuan CS, Murphy M, Moss J, Roizen MF. Safety and tolerance of methylnaltrexone in healthy humans: a randomized, placebo-controlled, intravenous, ascending-dose, pharmacokinetic study. J Clin Pharmacol. 1997;37:25–30. [PubMed: 9048269](Single, ascending dose study of methyl-naltrexone [which does not cross the blood-brain barrier] in 8 healthy volunteers found no changes in liver tests; dose limiting side effects being dizziness and orthostatic hypotension).
- Metze D, Reimann S, Beissert S, Luger T. Efficacy and safety of naltrexone, an oral opiate receptor antagonist, in the treatment of pruritus in internal and dermatological diseases. J Am Acad Dermatol. 1999;41:533–9. [PubMed: 10495371](Among 50 patients with pruritus of varying etiologies treated with open-label naltrexone for up to 12 months, side effects included nausea, fatigue, dizziness and diarrhea; liver tests were done, but results were not discussed).
- Bergasa NV, Schmitt JM, Talbot TL, Alling DW, Swain MG, Turner ML, Jenkins JB, et al. Open-label trial of oral nalmefene therapy for the pruritus of cholestasis. Hepatology. 1998;27:679–84. [PubMed: 9500694](Open label trial of nalmefene for 2-26 months in 14 patients with liver disease and pruritus found "no consistent effect of nalmefene on the severity of cholestasis, as assessed by routine serum biochemical markers").
- Wong GY, Wolter TD, Croghan GA, Croghan IT, Offord KP, Hurt RD. A randomized trial of naltrexone for smoking cessation. Addiction. 1999;94:1227–37. [PubMed: 10615738](Among 100 cigarette smokers receiving placebo or naltrexone with or without nicotine patches, side effects included headache and sleep disturbance, but no mention of effects on laboratory tests).
- Chick J, Anton R, Checinski K, Croop R, Drummond DC, Farmer R, Labriola D, et al. A multicentre, randomized, double-blind, placebo-controlled trial of naltrexone in the treatment of alcohol dependence or abuse. Alcohol Alcohol. 2000;35:587–93. [PubMed: 11093966](Among 175 patients with alcoholism treated with naltrexone vs placebo for 12 weeks, ALT levels were no different in the two groups, while GGT levels were lower with naltrexone therapy).
- Gastpar M, Bonnet U, Böning J, Mann K, Schmidt LG, Soyka M, Wetterling T, et al. Lack of efficacy of naltrexone in the prevention of alcohol relapse: results from a German multicenter study. J Clin Psychopharmacol. 2002;22:592–8. [PubMed: 12454559](Controlled trial of 12 weeks of naltrexone vs placebo in 171 detoxified alcoholic patients found similar rates of abstinence in the two groups, but greater decrease in GGT levels with naltrexone; one placebo recipient had significant ALT elevations).
- Terg R, Coronel E, Sordá J, Muñoz AE, Findor J. Efficacy and safety of oral naltrexone treatment for pruritus of cholestasis, a crossover, double blind, placebo-controlled study. J Hepatol. 2002;37:717–22. [PubMed: 12445410](Placebo controlled cross over trial of 2 weeks of naltrexone for pruritus of liver disease in 20 patients; side effects were dizziness, nausea, headache and abdominal cramps; ALT and AST values decreased).
- Romach MK, Sellers EM, Somer GR, Landry M, Cunningham GM, Jovey RD, McKay C, et al. Naltrexone in the treatment of alcohol dependence: a Canadian trial. Can J Clin Pharmacol. 2002;9:130–6. [PubMed: 12422250](Open labeled study of naltrexone in 120 alcohol dependent patients; 12% had ALT elevations, but most were attributed to alcoholic liver disease rather than drug).
- Guardia J, Caso C, Arias F, Gual A, Sanahuja J, Ramíz M, Mengual I, et al. A double-blind, placebo-controlled study of naltrexone in the treatment of alcohol-dependence disorder: results from a multicenter clinical trial. Alcohol Clin Exp Res. 2002;26:1381–7. [PubMed: 12351933](Controlled trial of naltrexone vs placebo for 12 weeks in 282 alcohol dependent patients found no hepatic complications and that GGT levels decreased in both groups).
- Mason BJ. Acamprosate and naltrexone treatment for alcohol dependence: an evidence-based risk-benefits assessment. Eur Neuropsychopharmacol. 2003;13:469–75. [PubMed: 14636963](Review of literature on efficacy and safety of naltrexone and acamprosate for alcohol dependence, mentions that the naltrexone package insert states that it shows a dose dependent hepatotoxicity).
- Brewer C, Wong VS. Naltrexone: report of lack of hepatotoxicity in acute viral hepatitis, with a review of the literature. Addict Biol. 2004;9:81–7. [PubMed: 15203443](23 year old male heroin abuser developed acute hepatitis B while being treated with depot naltrexone, but subsequently recovered completely without complications; also had chronic hepatitis C).
- Bouza C, Angeles M, Muñoz A, Amate JM. Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review. Addiction 2004; 99: 811-28. Erratum in Addiction. 2005;100:573. Magro, Angeles [corrected to Angeles, Magro] [PubMed: 15200577](Systematic review of 33 studies of acamprosate and naltrexone; naltrexone therapy was associated with improvements in GGT and AST levels; no mention of hepatotoxicity).
- Galloway GP, Koch M, Cello R, Smith DE. Pharmacokinetics, safety, and tolerability of a depot formulation of naltrexone in alcoholics: an open-label trial. BMC Psychiatry. 2005;5:18. [PMC free article: PMC1087493] [PubMed: 15804355](Open label trial of depot naltrexone for 6 weeks in 16 alcohol dependent patients; no serious adverse events were reported and no mention was made of hepatotoxicity or ALT elevations).
- Yen MH, Ko HC, Tang FI, Lu RB, Hong JS. Study of hepatotoxicity of naltrexone in the treatment of alcoholism. Alcohol. 2006;38:117–20. [PubMed: 16839858](Open label study of 12 weeks of oral naltrexone in 74 alcoholic patients; ALT levels decreased on naltrexone, but one patient had rise of ALT from 12 to 391 U/L; no details provided).
- Kim SW, Grant JE, Yoon G, Williams KA, Remmel RP. Safety of high-dose naltrexone treatment: hepatic transaminase profiles among outpatients. Clin Neuropharmacol. 2006;29:77–9. [PubMed: 16614539](Open label study of high doses of naltrexone in 41 patients with impulse control disorder, found no change in ALT or AST levels on therapy).
- Comer SD, Sullivan MA, Yu E, Rothenberg JL, Kleber HD, Kampman K, Dackis C, et al. Injectable, sustained-release naltrexone for the treatment of opioid dependence: a randomized, placebo-controlled trial. Arch Gen Psychiatry. 2006;63:210–8. [PMC free article: PMC4200530] [PubMed: 16461865](Controlled trial of 8 weeks of depot naltrexone in 60 heroin dependent patients; ALT and GGT levels were stable; 2 patients with significant ALT elevations both had chronic hepatitis C).
- Lobmaier P, Kornø Kunø Bjøl A. Sustained-release naltrexone for opioid dependence. Cochrane Database Syst Rev. 2008;(2):CD006140. [PubMed: 18425938](Systematic review of efficacy of naltrexone for opioid dependence; no mention of hepatotoxicity).
- Lucey MR, Silverman BL, Illeperuma A, O'Brien CP. Hepatic safety of once-monthly injectable extended-release naltrexone administered to actively drinking alcoholics. Alcohol Clin Exp Res. 2008;32:498–504. [PubMed: 18241321](Controlled trial of 6 months of naltrexone by monthly depot injection in 624 patients with alcohol dependence, found no differences in mean ALT or bilirubin levels, but GGT levels were lower on naltrexone; ALT elevations occurred in 9-12% of those on naltrexone vs 15% on placebo).
- Garbutt JC. Efficacy and tolerability of naltrexone in the management of alcohol dependence. Curr Pharm Des. 2010;16:2091–7. [PubMed: 20482515](Review of safety and efficacy of naltrexone for alcohol dependence: in studies of more than 4000 patients, "hepatotoxicity has not emerged as a clinical problem").
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none to naltrexone or other agents used to treated substance abuse).
- Yoon G, Kim SW, Thuras P, Westermeyer J. Safety, tolerability, and feasibility of high-dose naltrexone in alcohol dependence: an open label study. Hum Psychopharmacol. 2011;26:125–32. [PubMed: 21437991](Among 24 patients undergoing alcohol withdrawal treated with high doses of naltrexone for 12 weeks, serum ALT and bilirubin levels did not change and GGT values fell slightly).
- Tetrault JM, Tate JP, McGinnis KA, Coulet JL, Sullivan LE, Bryant K, Justice AC, Fiellin DA., Veterans Aging Cohort Study Team. Hepatic safety and antiretroviral effectiveness in HIV-infected patients receiving naltrexone. Alcohol Clin Exp Res. 2012;36(2):318–24. [PMC free article: PMC3221963] [PubMed: 21797892](Retrospective analysis of the Veterans Administration database revealed 114 patients with HIV infection who were treated with naltrexone for alcohol dependence for at least 7 days [57% with HCV co-infection, 52% on antiretroviral therapy] showed that ALT levels remained low during naltrexone therapy and only 2 patients had elevations possibly related [Case 1, ALT 225 U/L at day 30 falling to baseline within 2 months of stopping: Case 2, ALT 152 U/L 33 days after stopping, resolving within 4 months]).
- Vergara-Rodriguez P, Tozzi MJ, Botsko M, Nandi V, Altice F, Egan JE, O'Connor PG, et al. BHIVES Collaborative. Hepatic safety and lack of antiretroviral interactions with buprenorphine/naloxone in HIV-infected opioid-dependent patients. J Acquir Immune Defic Syndr. 2011;56 suppl 1:S62–7. [PubMed: 21317596](Among 141 HIV infected subjects treated with buprenorphine/naloxone for 6 months, median serum ALT and AST values did not change and no patient developed clinically apparent liver injury; 3 had transient ALT elevations during treatment [383, 123 and 218 U/L], but all resolved either spontaneously or with drug discontinuation).
- Mitchell MC, Memisoglu A, Silverman BL. Hepatic safety of injectable extended-release naltrexone in patients with chronic hepatitis C and HIV infection. J Stud Alcohol Drugs. 2012;73:991–7. [PubMed: 23036218](Among 250 opiate dependent patients with high rates of hepatitis C and HIV infection treated with monthly injections of naltrexone or placebo, ALT elevations >3 times ULN occurred in 20% of naltrexone vs 13% of placebo recipients, but all resolved even with continuing the medication).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to naltrexone or other opioid antagonist).
- Vagenas P, Di Paola A, Herme M, Lincoln T, Skiest DJ, Altice FL, Springer SA. An evaluation of hepatic enzyme elevations among HIV-infected released prisoners enrolled in two randomized placebo-controlled trials of extended release naltrexone. J Subst Abuse Treat. 2014;47:35–40. [PMC free article: PMC4042403] [PubMed: 24674234](Among 84 individuals with HIV infection recently released from prison who were treated for alcohol or opioid dependency with monthly injections of naltrexone or placebo, none developed clinically apparent liver injury but one subject with HCV co-infection discontinued naltrexone when ALT levels were found to have risen from 27 to 394 U/L after 4 injections).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America: an analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Among 176 reports of drug induced liver injury from Latin America published between 1996 and 2012, none were attributed to naltrexone or other opioid antagonist).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to naltrexone or other opioid antagonist).
- Chaignot C, Zureik M, Rey G, Dray-Spira R, Coste J, Weill A. Risk of hospitalisation and death related to baclofen for alcohol use disorders: Comparison with nalmefene, acamprosate, and naltrexone in a cohort study of 165 334 patients between 2009 and 2015 in France. Pharmacoepidemiol Drug Saf. 2018;27:1239–48. [PMC free article: PMC6282718] [PubMed: 30251424](Analysis of the French Health Insurance claims database of patients initiating alcohol use disorder therapies found an increased risk of hospitalization [+13%] and death [+31%] compared to exposure to approved drugs such as acamprosate, naltrexone and nalmefene).
- Opioids for pain. Med Lett Drugs Ther. 2018;60(1544):57–64. [PubMed: 29664446](Concise review of the efficacy, safety and costs of opioids used for pain mentions that the 3 opioid antagonists that are used to treat opioid-induced constipation-methylnaltrexone, naloxegol and nalmedine-have similar degrees of efficacy and toxicities).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Opioids.[LiverTox: Clinical and Researc...]Review Opioids.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Naltrexone-Bupropion.[LiverTox: Clinical and Researc...]Review Naltrexone-Bupropion.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review [Limited role of naltrexone in the treatment of opiate addiction].[Ned Tijdschr Geneeskd. 2001]Review [Limited role of naltrexone in the treatment of opiate addiction].van Brussel GH. Ned Tijdschr Geneeskd. 2001 Jul 28; 145(30):1452-6.
- What you need to know: addiction--prescribing naltrexone.[Singapore Med J. 1997]What you need to know: addiction--prescribing naltrexone.Yeo BK. Singapore Med J. 1997 Feb; 38(2):92-3.
- Review Naltrexone extended-release injection: an option for the management of opioid abuse.[Subst Abuse Rehabil. 2011]Review Naltrexone extended-release injection: an option for the management of opioid abuse.Taylor R Jr, Raffa RB, Pergolizzi JV Jr. Subst Abuse Rehabil. 2011; 2:219-26. Epub 2011 Dec 6.
- Naltrexone - LiverToxNaltrexone - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...