NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Flurbiprofen is a nonsteroidal antiinflammatory drug (NSAID) used in treatment of mild-to-moderate pain and symptoms of chronic arthritis. Flurbiprofen has been linked to a low rate of serum enzyme elevations during therapy and to rare instances of clinically apparent acute liver injury.
Background
Flurbiprofen (flur" bi proe' fen) belongs to the propionic acid derivative class of NSAIDs, similar to fenoprofen, naproxen and ibuprofen. Like other NSAIDs, flurbiprofen is a cyclo-oxygenase (Cox-1 and -2) inhibitor that blocks the formation of prostaglandins that are important in pain and inflammatory pathways. Flurbiprofen has analgesic as well as antipyretic and antiinflammatory activities. Flurbiprofen was approved in the United States in 1988. Current indications include chronic joint pain due to osteoarthritis and rheumatoid arthritis, as well as mild-to-moderate acute pain. The recommended dose in adults with chronic arthritis is 50 to 100 mg two to four times daily, with a maximum dose of 300 mg daily. Flurbiprofen is available by prescription in the form of capsules or tablets of 50 and 100 mg in both generic and trade formulations (Ansaid). As with other NSAIDs, flurbiprofen is generally well tolerated, but side effects can include headache, dizziness, somnolence, gastrointestinal upset, nausea, abdominal discomfort, diarrhea, edema and hypersensitivity reactions.
Hepatotoxicity
Prospective studies show that mild elevations in serum aminotransferase levels can occur in up to 15% of patients taking flurbiprofen, but these are generally transient, mild and asymptomatic, often resolving even with drug continuation. Marked aminotransferase elevations (>3 fold elevated) occur in <1% of patients. Clinically apparent liver injury with jaundice from flurbiprofen is rare and only individual case descriptions have been published. The latency to onset is within 1 to 4 weeks of starting. The pattern of enzyme elevations is typically cholestatic, but hepatocellular cases have been described. Immunoallergic features are present in some cases (low grade fever, rash), but are generally not prominent, and autoantibody formation is rare. Most cases resolve promptly on stopping therapy. Flurbiprofen is not mentioned in large case series on drug induced liver injury or acute liver failure from the United States, but was listed as the second most common agent implicated in drug-induced liver injury in a case series from Turkey, one of which was fatal.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism of flurbiprofen hepatotoxicity is not known, but likely to be due to an idiosyncratic hypersensitivity reaction to an intermediate of its metabolism. Flurbiprofen is extensively metabolized by the liver, largely through the cytochrome P450 pathway (CYP 2C9).
Outcome and Management
Severity ranges from asymptomatic elevations in serum aminotransferase levels, to symptomatic hepatitis with or without jaundice, to acute liver failure and death. There are no convincing cases of chronic hepatitis or vanishing bile duct syndrome attributable to flurbiprofen use in the published literature. Patients with clinically apparent flurbiprofen induced liver injury should avoid other propionic acid derivatives such as fenoprofen, ibuprofen, ketoprofen and naproxen.
Drug Class: Nonsteroidal Antiinflammatory Drugs
CASE REPORT
Case 1. Cholestatic hepatitis due to flurbiprofen.
[Modified from: Dogan S, Celikbilek M, Demirkan K, Yilmaz S, Deniz K, Gursoy S, Yucesoy M. Prolonged Cholestatic Jaundice Associated With Flurbiprofen. J Pharm Pract 2013; 27: 396-398. PubMed Citation]
A 28 year old man developed pruritus and jaundice 3 to 4 weeks after starting flurbiprofen (100 mg twice daily) for posttraumatic muscle and joint pains. He denied rash, fever and abdominal pain. He had no previous history of liver disease, alcohol abuse or risk factors for viral hepatitis. He took no other medications or herbal supplements and had no history of drug allergies. On presentation, he was jaundiced, but had no hepatic tenderness, organomegaly or signs of chronic liver disease. Laboratory testing showed a total bilirubin of 18.4 mg/dL (direct 10.0 mg/dL), ALT 75 U/L, AST 68 U/L, GGT 480 U/L and alkaline phosphatase 574 U/L (Table). A complete blood count, INR and albumin levels were normal. Tests for hepatitis A, B, C and E were negative as were autoantibodies. Abdominal ultrasound was normal and without evidence of biliary obstruction, which was verified by magnetic resonance cholangiopancreatography (MRCP). Flurbiprofen was stopped, but his liver tests worsened over the following week. A liver biopsy showed intrahepatic cholestasis without fibrosis, steatosis or features of extrahepatic obstruction. He was treated with prednisolone, ursodiol and cholestyramine and began to improve. These agents were tapered and eventually stopped, but his liver tests remained abnormal until 6 months after stopping flurbiprofen.
Key Points
| Medication: | Flurbiprofen (200 mg daily for ~1 month) |
| Pattern: | Cholestatic (R=0.5) |
| Severity: | 3+ (jaundice, hospitalization) |
| Latency: | 3 to 4 weeks |
| Recovery: | Complete recovery 6 months after stopping |
| Other medications: | None |
Laboratory Values
| Time After Starting | Time After Stopping | ALT (U/L) | Alk P (U/L) | Bilirubin (mg/dL) | Other |
|---|---|---|---|---|---|
| 0 | Flurbiprofen (200 mg daily) started for joint pain | ||||
| 4 weeks | 0 | 75 | 574 | 18.4 | Flurbiprofen stopped |
| 5 weeks | 1 week | 74 | 587 | 26.4 | Liver biopsy |
| 4 months | 3 months | 54 | 246 | 10.0 | Prednisolone stopped |
| 7 months | 6 months | 35 | 124 | 1.3 | Ursodiol stopped |
| Normal Values | <35 | <128 | <1.2 | ||
Comment
This was a convincing case of cholestatic hepatitis arising a month after starting flurbiprofen. No other medications were being taken, and clinical evaluation including MRCP identified no other cause of acute cholestatic jaundice. The course was moderately severe and protracted, but recovery was eventually complete. Clinically apparent liver injury from NSAIDs varies greatly in clinical features and outcomes. Some agents are associated with hepatocellular injury that can be severe (diclofenac, etodolac) and others with cholestatic hepatitis (meloxicam, celecoxib), and some agents with a long latency and autoimmune features (diclofenac, etodolac) and others with a short latency and immunoallergic features (oxaprozin, celecoxib). The NSAIDs are some of the most frequently taken medications worldwide, and hepatotoxicity from their use is clearly quite rare and generally only mild-to-moderate in severity and self-limited in course.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Flurbiprofen – Generic, Ansaid®
DRUG CLASS
Nonsteroidal Antiinflammatory Drugs
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
| DRUG | CAS REGISTRY NUMBER | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Flurbiprofen | 5104-49-4 | C15-H13-F-O2 |
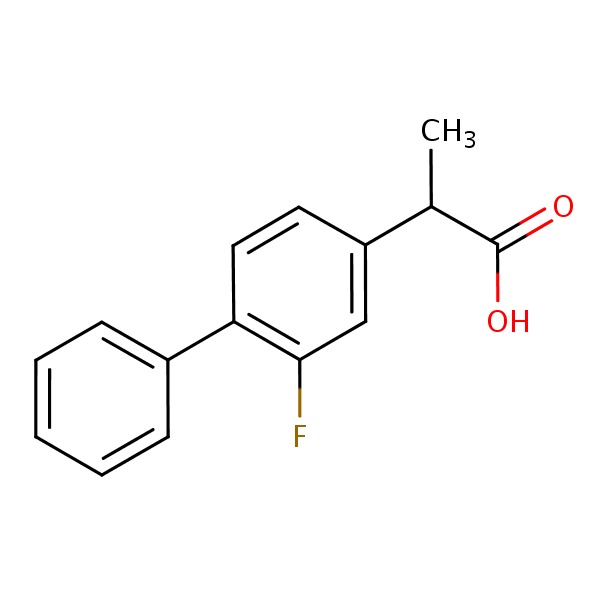 |
ANNOTATED BIBLIOGRAPHY
References updated: 25 January 2018
- Zimmerman HJ. Drugs used to treat rheumatic and musculospastic disease. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 517-53.(Expert review of hepatotoxicity published in 1999; flurbiprofen is listed as having a very low incidence of hepatotoxicity which is typically hepatocellular).
- Lewis JH, Stine JG. Nonsteroidal anti-inflammatory drugs and leukotriene receptor antagonists: pathology and clinical presentation of hepatotoxicity. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd. Amsterdam: Elsevier, 2013, pp. 369-401.(Review of hepatotoxicity of NSAIDs mentions that only a single case of hepatotoxicity from flurbiprofen has been reported [Kotowski 1982]).
- Grosser T, Smyth E, FitzGerald GA. Anti-inflammatory, antipyretic, and analgesic agents; pharmacotherapy of gout. In, Brunton LL, Chabner B, Knollman B, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 12th ed. New York: McGraw-Hill, 2011, pp. 959-1004.(Textbook of pharmacology and therapeutics).
- Kotowski KE, Grayson MF. Side effects of non-steroidal anti-inflammatory drugs. Br Med J (Clin Res Ed) 1982; 285 (6338): 377. [PMC free article: PMC1498992] [PubMed: 6807485](56 year old woman with mixed connective tissue disease developed abdominal pain, fever, rash and jaundice 3 months after restarting flurbiprofen [bilirubin 1.3 mg/dL, AST >1200 U/L, Alk P 150 U/L], resolving within 7 weeks of stopping; authors mention two other cases reported by the manufacturer, one with jaundice and recurrence on rechallenge).
- Zimmerman HJ. Update of hepatotoxicity due to classes of drugs in common clinical use: non-steroid drugs, anti-inflammatory drugs, antibiotics, antihypertensives, and cardiac and psychotropic agents. Semin Liver Dis 1990; 10: 322-8. [PubMed: 2281340](Extensive review of NSAID related liver injury states that flurbiprofen has only rarely been linked to liver injury).
- Ruiz-Rebollo ML, Delgado-Fontaneda E, Testillano-Tarrero M, Moretó-Canela M. [Cholestasis caused by hypersensitivity to flurbiprofen]. Rev Esp Enferm Dig 1992; 82: 130-1. Spanish. [PubMed: 1389551](63 year old woman developed fatigue, fever and rash within a day of starting flurbiprofen and subsequently developed jaundice 20 days later [bilirubin 14.6 mg/dL, ALT 86 U/L, Alk P 478 U/L], resolving rapidly upon stopping).
- Walker AM. Quantitative studies of the risk of serious hepatic injury in persons using nonsteroidal antiinflammatory drugs. Arthritis Rheum 1997; 40: 201-8. [PubMed: 9041931](Review of population based studies of NSAID use and hepatic injury; frequency of clinically apparent liver injury from NSAIDs overall was ~10 cases per 100,000 patient-years of use; flurbiprofen is not specifically discussed).
- Lacroix I, Lapeyre-Mestre M, Bagheri H, Pathak A, Montastruc JL; Club de Reflexion des cabinets de Groupe de Gastro-Enterologie (CREGG); General Practitioner Networks. Nonsteroidal anti-inflammatory drug-induced liver injury: a case-control study in primary care. Fundam Clin Pharmacol 2004; 18: 201-6. [PubMed: 15066135](Case controlled study of patients presenting with suspected drug induced liver injury in a general practice context in Southern France found 88 cases which were matched with 178 controls; 22 cases vs 16 controls had been exposed to NSAIDs; 5 diclofenac, 4 ibuprofen, 4 ketoprofen, 2 niflumic acid, 1 flurbiprofen and 1 meloxicam, rest to salicylates which were as frequently used in controls as cases; there were no fatalities and cases were more common in women than men).
- Rubenstein JH, Laine L. Systematic review: the hepatotoxicity of non-steroidal anti-inflammatory drugs. Aliment Pharmacol Ther 2004; 20: 373-80. [PubMed: 15298630](NSAIDs are the most commonly used drugs in the US and account for a large proportion of cases of hepatic injury, but the frequency is quite rare. Among 7 population based studies, hospitalization occurred in 22.4/100,000 patient-years of NSAID use [rate ratio=1.5] and deaths from liver injury occurred in ~1/100,000 patient-years; frequency of injury did not increase with age and was no more common in women than men; in case controlled studies, higher odds ratio for liver injury was found with sulindac, indomethacin, piroxicam and diclofenac; no mention of flurbiprofen).
- Björnsson E, Jerlstad P, Bergqvist A, Olsson R. Fulminant drug-induced hepatic failure leading to death or liver transplantation in Sweden. Scand J Gastroenterol 2005; 40: 1095-1101. [PubMed: 16165719](Survey of all cases of fatal drug induced liver injury from Swedish Adverse Drug Reporting system from 1966-2002; among 103 cases, none were attributed to flurbiprofen).
- Lapeyre-Mestre M, de Castro AM, Bareille MP, Garcia del Pozo J, Requejo AA, Arias LM, Montastruc J-L, et al. Non-steroidal anti-inflammatory drug-related hepatic damage in France and Spain: analysis from national spontaneous reporting systems. Fundam Clin Pharmacol 2006; 20: 391-5. [PubMed: 16867024](Analysis of reports of liver injury from NSAIDs from France and Spain from 1982-2001; flurbiprofen is not specifically mentioned).
- Arellano FM, Yood MU, Wentworth CE, Oliveria SA, Rivero E, Verman A, Rothman K. Use of cyclo-oxygenase 2 inhibitors (COX-2) and prescription non-steroidal anti-inflammatory drugs (NSAIDS) in UK and USA populations Implications for COX-2 cardiovascular profile. Pharmacoepidemiol Drug Saf 2006; 15: 861-72. [PubMed: 17086563](Surveys from the UK and USA indicate that ibuprofen, naproxen and diclofenac were the most commonly used NSAIDs; flurbiprofen was not among the top 10 agents used).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J; Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology 2008; 135: 1924-34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, NSAIDs were implicated as a sole agent in 8 cases [4 diclofenac, 2 celecoxib, 1 meloxicam and 1 oxaprozin] and as one of several agents in 3 cases [1 diclofenac, 1 celecoxib, 1 ibuprofen]; none were attributed to flurbiprofen).
- Bessone F. Non-steroidal anti-inflammatory drugs: What is the actual risk of liver damage? World J Gastroenterol 2010; 16: 5651-61. [PMC free article: PMC2997980] [PubMed: 21128314](Review of estimated frequency of drug induced liver injury due to NSAIDs from large published epidemiological studies; no discussion of flurbiprofen).
- Reuben A, Koch DG, Lee WM; Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology 2010; 52: 2065-76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury and 7 to NSAIDs, including 4 to bromfenac, 2 diclofenac and 1 etodolac, but none to other NSAIDS including flurbiprofen, ibuprofen and naproxen).
- Dogan S, Celikbilek M, Demirkan K, Yilmaz S, Deniz K, Gursoy S, Yucesoy M. Prolonged Cholestatic Jaundice Associated With Flurbiprofen. J Pharm Pract 2013; 27: 396-8. [PubMed: 24381241](28 year old man developed pruritus and jaundice 1 month after starting flurbiprofen [bilirubin 18.4 mg/dL, ALT 75 U/L, Alk P 574 U/L], resolving slowly over the 6 months after stopping: Case 1).
- Gulmez SE, Larrey D, Pageaux GP, Lignot S, Lassalle R, Jové J, Gatta A, et al. Transplantation for acute liver failure in patients exposed to NSAIDs or paracetamol (acetaminophen): the multinational case-population SALT study. Drug Saf 2013; 36: 135-44. [PMC free article: PMC3568201] [PubMed: 23325533](Among 600 patients undergoing liver transplantation for acute liver failure at 52 European liver transplant centers between 2005 and 2007, 301 were considered idiopathic and had received a medication within 30 days of onset, including acetaminophen in 192 and NSAIDs in 40, but no specific mention of flurbiprofen).
- Lapeyre-Mestre M, Grolleau S, Montastruc JL; Association Française des Centres Régionaux de Pharmacovigilance (CRPV). Adverse drug reactions associated with the use of NSAIDs: a case/noncase analysis of spontaneous reports from the French pharmacovigilance database 2002-2006. Fundam Clin Pharmacol 2013; 27: 223-30. [PubMed: 21929527](Analysis of serious adverse events reporting to a French pharmacovigilance database found highest cumulative rates for liver related reports for nimesulide [0.15 per million defined daily doses], followed by diclofenac [0.09], ketoprofen [0.09], piroxicam [0.06], naproxen [0.04] and meloxicam [0.03] being significant in case/non-case analyses for nimesulide, diclofenac and piroxicam only; no mention of flurbiprofen).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology 2013; 144: 1419-25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, including 6 attributed to diclofenac (ranking 2nd), but none were due to flurbiprofen).
- Dağ MS, Aydınlı M, Oztürk ZA, Türkbeyler IH, Koruk I, Savaş MC, Koruk M, et al. Drug- and herb-induced liver injury: a case series from a single center. Turk J Gastroenterol 2014; 25: 41-5. [PubMed: 24918129](Among 82 cases of drug or herbal product induced liver injury seen at a single referral center in Turkey between 2008 and 2012, NSAIDs were the most common class of agents implicated, accounting for 19 cases [23%] of which 7 were due to flubroprofen, one of which resulted in acute liver failure).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al.; United States Drug Induced Liver Injury Network. Features and Outcomes of 899 Patients With Drug-Induced Liver Injury: The DILIN Prospective Study. Gastroenterology 2015; 148: 1340-52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 28 cases were attributed to an NSAID including 15 to diclofenac, 3 celecoxib, 3 meloxicam, 2 oxaprozin, 2 etodolac, and 1 each for ibuprofen, sulindac and valdecoxib, but none for flurbiprofen or fenoprofen).
- Schmeltzer PA, Kosinski AS, Kleiner DE, Hoofnagle JH, Stolz A, Fontana RJ, Russo MW; Drug-Induced Liver Injury Network (DILIN). Liver injury from nonsteroidal anti-inflammatory drugs in the United States. Liver Int 2016; 36: 603-9. [PMC free article: PMC5035108] [PubMed: 26601797](Among 1231 cases of suspected drug induced liver injury enrolled in a prospective study in the US between 2004 and 2014, 30 [2%] were considered due to an NSAID, including diclofenac [n=16], celecoxib [3], meloxicam [3], etodolac [2], oxaprozin [2], ibuprofen [2] and sulindac [1], while none were attributed to flurbiprofen).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Ketoprofen.[LiverTox: Clinical and Researc...]Review Ketoprofen.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Fenoprofen.[LiverTox: Clinical and Researc...]Review Fenoprofen.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Diclofenac.[LiverTox: Clinical and Researc...]Review Diclofenac.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Piroxicam.[LiverTox: Clinical and Researc...]Review Piroxicam.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Tolmetin.[LiverTox: Clinical and Researc...]Review Tolmetin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Flurbiprofen - LiverToxFlurbiprofen - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...