NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-.

LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet].
Show detailsOVERVIEW
Introduction
Degarelix is a parenterally administered, gonadotropin releasing hormone (GnRH) antagonist that effectively blocks androgen production and is used to treat advanced prostate cancer. Degarelix therapy is associated with serum enzyme elevations during therapy, but has yet to be linked to instances of clinically apparent acute liver injury.
Background
Degarelix (deg" a rel' ix) is a synthetic decapeptide antagonist of gonadotropin releasing hormone (GnRH) that blocks GnRH stimulation of luteinizing hormone (LH) and follicular stimulating hormone (FSH) production by the pituitary gland, thereby decreasing the synthesis of testosterone by the testes in men and estrogen by the ovaries in women. Degarelix has been found to be palliative in advanced prostate cancer with equivalent efficacy to the GnRH agonists, such as leuprolide and goserelin. Because degarelix is an antagonist of GnRH, it does not cause the initial increase in testosterone synthesis that occurs with use of GnRH agonists. Degarelix was approved for use in the United States in 2008, and current indications are limited to therapy of advanced prostate cancer. GnRH analogues have also been used off label for precocious puberty, infertility, and as a part of gender affirming therapy. Degarelix is available under the brand name Firmagon as a powder for reconstitution in 80 and 120 mg vials. The typical dose is 240 mg initially, with maintenance doses of 80 mg every 28 days. Common side effects include injection site reactions and symptoms typical of hypogonadism such as hot flashes, decreased libido, erectile dysfunction, nausea, diarrhea, weight gain and fluid retention. Potential severe adverse reactions include acute hypersensitivity reactions.
Hepatotoxicity
Degarelix therapy has been associated with serum enzyme elevations in up to one-third of patients. The elevations, however, are generally mild and self-limited, resolving even without dose adjustment. ALT values above 3 times the ULN occur in less than 1% of patients. Occasional patients require drug discontinuation because of serum enzyme elevations, but no instances of liver injury with jaundice or clinically apparent acute liver injury were reported in the initial clinical trials of degarelix. Since its approval and more widescale use, there have been no published reports of clinically apparent liver injury attributed to degarelix, although its general use has been limited.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which degarelix might cause liver injury is unknown. It is a decapeptide and is metabolized by many tissues to individual amino acids. It has no effect on cytochrome P450 activity and has not been implicated in drug-drug interactions.
Outcome and Management
While serum aminotransferase elevations during degarelix therapy are common, they rarely require dose adjustment or drug discontinuation. Routine monitoring of liver tests is not recommended except in patients with known, preexisting liver disease. There is no evidence of cross sensitivity to liver injury among the various GnRH analogues.
Drug Class: Antineoplastic Agents, GnRH Analogues
Other Drugs in the Subclass, GnRH Analogues: Goserelin, Histrelin, Leuprolide, Relugolix, Triptorelin
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Degarelix – Firmagon®
DRUG CLASS
Antineoplastic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
CHEMICAL FORMULA AND STRUCTURE
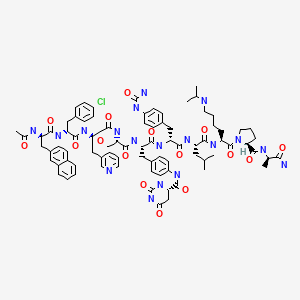
| DRUG | CAS REGISTRY NO. | MOLECULAR FORMULA | STRUCTURE |
|---|---|---|---|
| Degarelix | 214766-78-6 | C82-H103-Cl-N18-O16 |
|
ANNOTATED BIBLIOGRAPHY
References updated: 28 May 2023
Abbreviations: FSH, follicle stimulating hormone; GnRH, gonadotropin releasing hormone; LH, luteinizing hormone; PSA, prostate specific antigen.
- Zimmerman HJ. Hepatotoxic effects of oncotherapeutic and immunosuppressive agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 699.(Expert review of hepatotoxicity published in 1999; the GnRH analogues such as degarelix are not discussed).
- Chitturi S, Farrell GC. Estrogen receptor antagonists. Adverse effects of hormones and hormone antagonists on the liver. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 610-2.(Review of hepatotoxicity of hormonal products, does not discuss the GnRH analogues such as leuprolide, goserelin and degarelix).
- Levin ER, Vitek WS, Hammes SR. Estrogens, progestins, and the female reproductive tract. In, Brunton LL, Halal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 803-31.(Textbook of pharmacology and therapeutics).
- Snyder PJ. Androgens and the male reproductive tract. In, Brunton LL, Halal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 833-43.(Textbook of pharmacology and therapeutics).
- Isaacs C, Wellstein A, Riegel AT. Hormones and related agents in the therapy of cancer. In, Brunton LL, Halal-Dandan R, Knollman BC, eds. Goodman & Gilman's the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 1237-47.(Textbook of pharmacology and therapeutics).
- Van Poppel H, Tombal B, de la Rosette JJ, Persson BE, Jensen JK, Kold Olesen T. Degarelix: a novel gonadotropin-releasing hormone (GnRH) receptor blocker--results from a 1-yr, multicentre, randomised, phase 2 dosage-finding study in the treatment of prostate cancer. Eur Urol. 2008;54:805–13. [PubMed: 18538469](Among 187 men with advanced prostate cancer treated with degarelix at different initial [200 or 240 mg] and maintenance [80, 120 or 160 mg monthly] doses for one year, testosterone and PSA levels fell rapidly without an initial surge and remained suppressed; ALT levels were above 3 times ULN in 10 patients [5%] but were transient and resolved despite continuing drug).
- Whelan P. Editorial comment on: Degarelix: a novel gonadotropin-releasing hormone (GnRH) receptor blocker-results from a 1-yr, multicentre, randomised, phase 2 dose-finding study in the treatment of prostate cancer. Eur Urol. 2008;54:815. [PubMed: 18538468](Editorial in response to Van Poppel [2008], questioning whether degarelix is more effective and as safe as surgical castration or GnRH agonist therapy).
- Gittelman M, Pommerville PJ, Persson BE, Jensen JK, Olesen TK., Degarelix Study Group. A 1-year, open label, randomized phase II dose finding study of degarelix for the treatment of prostate cancer in North America. J Urol. 2008;180:1986–92. [PubMed: 18801505](Among 127 patients with advanced prostate cancer treated with degarelix for 1 year, testosterone levels were rapidly suppressed without an initial surge; ALT elevations occurred in 16% and 33% of subjects, but all elevations were less than 3 times ULN and resolved without dose adjustment or discontinuation).
- Klotz L, Boccon-Gibod L, Shore ND, Andreou C, Persson BE, Cantor P, Jensen JK, Olesen TK, Schrö FH. The efficacy and safety of degarelix: a 12-month, comparative, randomized, open-label, parallel-group phase III study in patients with prostate cancer. BJU Int. 2008;102:1531–8. [PubMed: 19035858](Among 610 patients with advanced prostate cancer treated with degarelix or leuprolide, common adverse events included injection site reactions [40% vs <1%], hot flashes [26% vs 21%], weight gain [10% vs 12%], and ALT elevations [9% vs 5%]; one patient on degarelix stopped therapy because of liver test abnormalities, but there were no instances of clinically apparent liver injury or liver injury with jaundice).
- Frampton JE, Lyseng-Williamson KA. Degarelix. Drugs. 2009;69:1967–76. [PubMed: 19747011](Review of the structure, mechanism of action, pharmacology, clinical efficacy and safety of degarelix mentions that it is "generally well tolerated", with adverse events largely due to subcutaneous injections and androgen deprivation and that ALT elevations above 3 times the ULN occurred in 7% of degarelix- vs 6% of leuprolide-treated patients).
- Degarelix (firmagon) for prostate cancer. Med Lett Drugs Ther. 2009;51(1323):82–3. [PubMed: 19838145](Concise review of the mechanism of action, rationale, clinical efficacy, safety and costs of degarelix as therapy for prostate cancer shortly after its approval in the US; mentions that "increases in hepatic transaminases" are common adverse events).
- Boccon-Gibod L, van der Meulen E, Persson BE. An update on the use of gonadotropin-releasing hormone antagonists in prostate cancer. Ther Adv Urol. 2011;3:127–40. [PMC free article: PMC3159401] [PubMed: 21904569](GnRH antagonists such as degarelix have similar efficacy to GnRH agonists in therapy of prostate cancer but have a more rapid onset of action and do not cause the initial testosterone surge that occurs with the agonists, which can be particularly troublesome in patients with a large tumor burden).
- Van Poppel H, Klotz L. Gonadotropin-releasing hormone: an update review of the antagonists versus agonists. Int J Urol. 2012;19:594–601. [PubMed: 22416801](Review of androgen deprivation therapy for prostate cancer using GnRH agonists and antagonists, stressing the more rapid onset of action and similar if not better safety profile of GnRH antagonists).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, but none of the 96 were attributed to degarelix or other GnRH analogues).
- Crawford ED, Shore ND, Moul JW, Tombal B, Schrö FH, Miller K, Boccon-Gibod L, et al. Long-term tolerability and efficacy of degarelix: 5-year results from a phase III extension trial with a 1-arm crossover from leuprolide to degarelix. Urology. 2014;83:1122–8. [PubMed: 24661333](Among participants in the initial controlled trial of degarelix vs leuprolide [Klotz 2008], 544 were then treated with degarelix for up to 5 years and generally continued to have potent suppression of testosterone and PSA levels; ALT elevations occurred in 6% of patients, but there was no mention of cases of clinically apparent liver injury).
- Carter NJ, Keam SJ. Degarelix: a review of its use in patients with prostate cancer. Drugs. 2014;74:699–712. [PubMed: 24756432](Review of mechanism of action, clinical efficacy and safety of degarelix for advanced prostate cancer mentions that liver test abnormalities occur but are usually mild and transient and that ALT elevations above 3 times ULN occurred in less than 1% of treated patients).
- Miller K, Simson G, Goble S, Persson BE. Efficacy of degarelix in prostate cancer patients following failure on luteinizing hormone-releasing hormone agonist treatment: results from an open-label, multicentre, uncontrolled, phase II trial(CS27). Ther Adv Urol. 2015;7:105–15. [PMC free article: PMC4485413] [PubMed: 26161141](Among 37 patients with advanced prostate cancer who had failed therapy with a GnRH agonist, switching to degarelix for up to 1 year yielded a low rate of response [8%] with poor tolerance and a high dropout rate; changes in clinical chemistry results were "small, with no consistent trends").
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, none were attributed to GnRH analogues such as degarelix).
- Dearnaley DP, Saltzstein DR, Sylvester JE, Karsh L, Mehlhaff BA, Pieczonka C, Bailen JL, et al. The oral gonadotropin-releasing hormone receptor antagonist relugolix as neoadjuvant/adjuvant androgen deprivation therapy to external beam radiotherapy in patients with localised intermediate-risk prostate cancer: a randomised, open-label, parallel-group phase 2 trial. Eur Urol. 2020;78:184–192. [PubMed: 32273183](Among 103 men with prostate cancer receiving radiotherapy who were treated with androgen deprivation therapy with relugolix [120 mg tablets daily] or degarelix [80 mg injections monthly], suppression of testosterone and PSA levels were similar in the two groups and adverse events were slightly fewer with relugolix [86% vs 97%], ALT elevations arising in none vs 13% but none were greater than 5 times ULN).
- Sawazaki H, Kitamura Y, Yagi K, Arai Y. Impact of androgen deprivation therapy on non-alcoholic fatty liver disease in patients with prostate cancer: a CT evaluation. Urol Int. 2020;104:425–430. [PubMed: 32396918](Among 77 patients with prostate cancer treated with androgen deprivation therapy [32 with leuprolide and 45 degarelix] for 6 months, computerized tomography demonstrated development of fatty liver in 7 patients but little change in body weight).
- Wallach JD, Deng Y, McCoy RG, Dhruva SS, Herrin J, Berkowitz A, Polley EC, et al. Real-world cardiovascular outcomes associated with degarelix vs leuprolide for prostate cancer treatment. JAMA Netw Open. 2021;4:e2130587. [PMC free article: PMC8536955] [PubMed: 34677594](Among 2226 men with advanced prostate cancer who initiated degarelix or leuprolide therapy between 2007 and 2019 who were propensity-matched for risk factors, major adverse cardiovascular event [MACE] rates were similar in the two groups [10.2 vs 8.6 per 100-patient years], although degarelix was associated with a high rate of death from any cause).
- Lopes RD, Higano CS, Slovin SF, Nelson AJ, Bigelow R, Sørensen PS, Melloni C, et al. PRONOUNCE Study Investigators. Cardiovascular safety of degarelix versus leuprolide in patients with prostate cancer: the primary results of the PRONOUNCE randomized trial. Circulation. 2021;144:1295–1307. [PMC free article: PMC9004319] [PubMed: 34459214](Among 545 men with prostate cancer and concurrent atherosclerosis cardiovascular disease treated with degarelix or leuprolide for at least one year, major cardiovascular adverse events [MACE} arose in 5.5% vs 4.1% and rates of testosterone suppression, disease progression, discontinuations for adverse events and serious adverse event rates were similar in both groups).
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Relugolix.[LiverTox: Clinical and Researc...]Review Relugolix.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Leuprolide.[LiverTox: Clinical and Researc...]Review Leuprolide.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Review Gonadotropin Releasing Hormone (GnRH) Analogues.[LiverTox: Clinical and Researc...]Review Gonadotropin Releasing Hormone (GnRH) Analogues.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- A comparative study on the efficacies of gonadotropin-releasing hormone (GnRH) agonist and GnRH antagonist in neoadjuvant androgen deprivation therapy combined with transperineal prostate brachytherapy for localized prostate cancer.[BMC Cancer. 2016]A comparative study on the efficacies of gonadotropin-releasing hormone (GnRH) agonist and GnRH antagonist in neoadjuvant androgen deprivation therapy combined with transperineal prostate brachytherapy for localized prostate cancer.Miki K, Sasaki H, Kido M, Takahashi H, Aoki M, Egawa S. BMC Cancer. 2016 Sep 1; 16(1):708. Epub 2016 Sep 1.
- Review Goserelin.[LiverTox: Clinical and Researc...]Review Goserelin.. LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. 2012
- Degarelix - LiverToxDegarelix - LiverTox
Your browsing activity is empty.
Activity recording is turned off.
See more...