Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 508233-74-7
Drug Levels and Effects
Summary of Use during Lactation
Amounts of vortioxetine in milk appear to be low. If vortioxetine is required by the mother, it is not a reason to discontinue breastfeeding. However, until more data are available, vortioxetine should be used with careful infant monitoring during breastfeeding.
Drug Levels
Maternal Levels. Three lactating mothers were taking vortioxetine for depression, two were taking 10 mg once daily and one was taking 20 mg once daily. Milk samples were taken 5 times over a 24-hour period before the dose and at 5, 7, 10, 12, and 24 hours after a dose at steady state. With the dose of 10 mg, the peak concentration of vortioxetine in milk was 13.9 mcg/L at 7 hours after the dose. With the dose of 20 mg, the peak milk concentration was 52.3 mcg/L at 5 hours after the dose. The weight-adjusted infant dosages were 1.1% for 10 mg dose and 1.7% for 20 mg dose.[1]
A woman who was taking a vortioxetine dose of 76.1 mcg/kg daily collected 6 to 8 milk samples over a 24-hour period. The peak milk level was 8.2 mcg/L and the mean concentration was 6 mcg/L. Using the mean value, the absolute infant dose in a fully breastfed infant would be 0.9 mcg/kg daily and the relative infant dose would be 1.2% of the mother’s weight-adjusted dosage.[2]
A Japanese woman with depression was taking vortioxetine 20 mg zolpidem 10 mg, duloxetine 20 mg, rebamipide 100 mg and the Asian herbal medicine Kami-kihi-tou 2.5 grams daily. On day 4 postpartum, she collected a sample of 5 mL of foremilk 2 hours after her vortioxetine dose. The milk sample contained 9.3 mcg/L which the authors used to calculate a relative infant dose of 0.32%.[3] This may not represent the maximum value, because the peak milk level occurred at 7 hours after a dose in another study.[1]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Three lactating mothers were taking vortioxetine for depression, two were taking 10 mg once daily and one was taking 20 mg once daily. All mothers were exclusively breastfeeding their infants aged 1, 2 and 6 months of age. No mothers reported any unusual behavior in their infants.[1]
A woman who was taking a vortioxetine dose of 76.1 mcg/kg daily partially breastfed her infant. She did not observe any adverse effects in her infant.[2]
A postpartum Japanese woman with depression was taking vortioxetine 20 mg zolpidem 10 mg, duloxetine 20 mg, rebamipide 100 mg and the Asian herbal medicine Kami-kihi-tou 2.5 grams daily. She partially (over 50%) breastfed her infant for 3 months. The infant had no detectable drug-related adverse effects on routine follow-up at 1, 3, 5, 7 and 9-months postpartum.[3]
Effects on Lactation and Breastmilk
Vortioxetine has caused hyperprolactinemia and galactorrhea in some patients.[4,5]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[6] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[7] None of the mothers were taking vortioxetine.
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[8]
Alternate Drugs to Consider
References
- 1.
- Marshall K, Datta P, Rewers-Felkins K, et al. Transfer of the serotonin modulator vortioxetine into human milk: A case series. Breastfeed Med 2021;16:843-5. [PubMed: 33861632]
- 2.
- Monfort A, Jutras M, Martin B, et al. Simultaneous quantification of 19 analytes in breast milk by liquid chromatography-tandem mass spectrometry (LC-MS/MS). J Pharm Biomed Anal 2021;204:114236. [PubMed: 34273657]
- 3.
- Kiribayashi M, Suda T, Takahashi M, et al. Vortioxetine exposure during pregnancy and lactation: A Japanese case study of neonatal implications and quantitative milk and plasma analyses. Breastfeed Med 2024;19:659-62. [PubMed: 38726594]
- 4.
- Verma A, Kumar A. Risks associated with vortioxetine in the established therapeutic indication. Curr Neuropharmacol 2021;19:711-7. [PMC free article: PMC8573751] [PubMed: 32811416]
- 5.
- Ozkan HM. Galactorrhea and hyperprolactinemia during vortioxetine use: Case report. Turk Biyokim Derg 2019;44:105-7. doi:10.1515/tjb-2018-0106 [CrossRef]
- 6.
- Venkatesh KK, Castro VM, Perlis RH, et al. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol 2017;37:1003-9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 7.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact 2017;33:701-9. [PubMed: 28984528]
- 8.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand 2022;101:344-54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
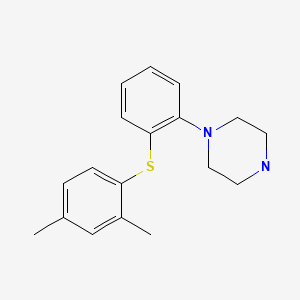
Vortioxetine
CAS Registry Number
508233-74-7
Drug Class
Breast Feeding
Lactation
Milk, Human
Antidepressive Agents
Serotonin Uptake Inhibitors
Serotonin 5-HT1 Receptor Agonists
Serotonin 5-HT1 Receptor Antagonists
Serotonin 5-HT3 Receptor Antagonists
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Vortioxetine for the treatment of major depressive disorder.[Expert Rev Clin Pharmacol. 2014]Review Vortioxetine for the treatment of major depressive disorder.Tritschler L, Felice D, Colle R, Guilloux JP, Corruble E, Gardier AM, David DJ. Expert Rev Clin Pharmacol. 2014 Nov; 7(6):731-45. Epub 2014 Aug 28.
- Review [Pharmacological properties of vortioxetine and its pre-clinical consequences].[Encephale. 2016]Review [Pharmacological properties of vortioxetine and its pre-clinical consequences].David DJ, Tritschler L, Guilloux JP, Gardier AM, Sanchez C, Gaillard R. Encephale. 2016 Feb; 42(1 Suppl 1):1S12-23.
- Transfer of the Serotonin Modulator Vortioxetine into Human Milk: A Case Series.[Breastfeed Med. 2021]Transfer of the Serotonin Modulator Vortioxetine into Human Milk: A Case Series.Marshall K, Datta P, Rewers-Felkins K, Krutsch K, Baker T, Hale TW. Breastfeed Med. 2021 Oct; 16(10):843-845. Epub 2021 Apr 16.
- 5-HTT and 5-HT(1A) receptor occupancy of the novel substance vortioxetine (Lu AA21004). A PET study in control subjects.[Eur Neuropsychopharmacol. 2013]5-HTT and 5-HT(1A) receptor occupancy of the novel substance vortioxetine (Lu AA21004). A PET study in control subjects.Stenkrona P, Halldin C, Lundberg J. Eur Neuropsychopharmacol. 2013 Oct; 23(10):1190-8. Epub 2013 Feb 18.
- Review Cinacalcet.[Drugs and Lactation Database (...]Review Cinacalcet.. Drugs and Lactation Database (LactMed®). 2006
- Vortioxetine - Drugs and Lactation Database (LactMed®)Vortioxetine - Drugs and Lactation Database (LactMed®)
- MULTISPECIES: hypothetical protein [Lysinibacillus]MULTISPECIES: hypothetical protein [Lysinibacillus]gi|501251709|ref|WP_012294727.1|Protein
Your browsing activity is empty.
Activity recording is turned off.
See more...
