Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
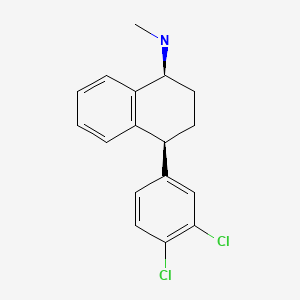
CASRN: 79617-96-2
Drug Levels and Effects
Summary of Use during Lactation
Because of the low levels of sertraline in breastmilk, amounts ingested by the infant are small and is usually not detected in the serum of the infant, although the weakly active metabolite norsertraline (desmethylsertraline) is often detectable in low levels in infant serum. Rarely, preterm infants with impaired metabolic activity might accumulate the drug and demonstrate symptoms similar to neonatal abstinence. Most authoritative reviewers consider sertraline a preferred antidepressants during breastfeeding.[1-9]
Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state.[10] These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Drug Levels
Sertraline is metabolized to norsertraline (desmethylsertraline), which has antidepressant activity of about 10% that of sertraline.
Maternal Levels. In a pooled analysis of serum levels from published studies and 4 unpublished cases, the authors found that 15 mothers taking an average daily dosage of 83 mg (range 25 to 200 mg) had an average breastmilk sertraline level of 45 mcg/L (range 7 to 207 mcg/L).[1] Using the average dosage and milk level data from this paper, an exclusively breastfed infant would receive an estimated 0.5% of the maternal weight-adjusted dosage of sertraline.
Twenty-six women who were an average of 15.8 weeks postpartum (range 5 to 36 weeks) and receiving an average of 124 mg sertraline daily for at least 14 days for severe depression were studied while breastfeeding with extensive milk and serum sampling over a 24-hour period. All milk samples had detectable sertraline (average 129 mcg/L; range 11 to 938 mcg/L) and norsertraline (average 258 mcg/L; range 20 to 1498 mcg/L). Drug concentrations were higher in the hindmilk than the foremilk. Analysis of milk sertraline data from 15 mothers who submitted complete sets of milk samples indicated that the peak concentration of the drug and metabolite occurred 8 to 9 hours after a dose. In these women, the concentration in milk correlated with serum concentration, but not daily dosage. The authors estimated that an exclusively breastfed infant would receive an average of 0.54% of the maternal weight-adjusted dosage and that pumping and discarding milk 8 to 9 hours after the mother's dose would decrease the infant's daily dosage by 17%.[11]
From data in 6 mothers who were 5 to 34 weeks postpartum and taking sertraline in an average daily dosage of 64 mg (range 50 to 100 mg), the authors estimated that an exclusively breastfed infant would receive 0.9% of the maternal weight-adjusted dosage.[12]
At 2 months postpartum, 4 mothers taking an average of 87.5 mg of sertraline daily had average milk levels of 26.4 mcg/L of sertraline and 29 mcg/L of norsertraline at random times after the previous dose. The authors estimated that an exclusively breastfed infant would receive 0.04 mg/kg of sertraline daily.[13]
The mother of a preterm infant was taking sertraline 150 mg daily during pregnancy and postpartum. Her breastmilk levels of sertraline and norsertraline on 3 days at random times averaged 201 and 358 mcg/L, respectively.[14]
One woman taking sertraline 25 mg daily had an average breastmilk sertraline concentration of 29 mcg/L at two times that were not stated. These values equated to an average infant dosage of 4.4 mcg/kg daily or 0.6% of the maternal weight-adjusted dosage. In the same paper, 3 women taking sertraline 50 mg daily had an average breastmilk sertraline concentration of 58 mcg/L at times that were not stated. These values equated to an average infant dosage of 8.7 mcg/kg daily or 1.2% of the maternal weight-adjusted dosage.[15]
A nursing mother was taking sertraline 50 mg daily. Foremilk and hindmilk samples taken at 4 weeks postpartum, 13 hours after a dose contained 26 mcg/L and 46 mcg/L, respectively.[16]
Nine women treated with sertraline 25 to 75 mg daily (7 were taking 50 mg daily) during the third trimester of pregnancy and during breastfeeding provided trough milk samples during the first week postpartum. Sertraline was undetectable (<5 mcg/L) in the milk of 1 woman taking 50 mg daily. In the other 8 women, milk levels ranged from 11.1 to 24.5 mcg/L, with calculated weight-adjusted percentage of maternal dosages ranging from 0.2 to 2.4%. These values might be inaccurate because of the timing of milk sample collection.[17]
Random milk samples were obtained from 6 women taking a median dosage of 50 mg (range 25 to 50 mg) of sertraline daily had a median sertraline milk concentration of 11.3 mcg/L (range 3.6 to 35.7 mcg/L). The authors calculated that this represents a median infant dosage of 1.6 (range 0.5 to 5.4) mcg/kg daily. No correlation was found between maternal dosage and milk sertraline level.[18]
A population pharmacokinetic model was constructed using blood and milk samples from breastfeeding mothers. Simulations suggested that the median daily infant dosage after a 50 mg maternal dose of sertraline would be 0.007 mg/kg or 0.9% of the weight-adjusted maternal dose. Over a 6-month period with a daily maternal dose of 150 mg, an exclusively breastfed infant would ingest a sertraline median cumulative dose of 21.2 mg (range 1.5-138.1 mg). Increased milk fat increased the passage of the drug into milk.[19]
Infant Levels. Of 30 breastfed infants (19 exclusively, 11 breastfed 50% or more) aged 6 to 13 weeks, 22 had undetectable (<1 mcg/L) sertraline serum levels during maternal therapy with sertraline dosages of 25 to 200 mg daily. Of the 8 infants who had detectable serum levels, their average sertraline serum level was 7.9 mcg/L. Their mothers, who were taking an average of 109 mg daily, had an average serum level of 52.8 mcg/L.[20]
In a pooled analysis of 53 mother-infant pairs from published and unpublished cases, the authors found that infants had an average of 2% (range 0 to 15%) of the sertraline plasma levels of the mothers'; 3 of the infants had a plasma level greater than 10% of the mothers' which was defined by the authors as being elevated.[1]
Twenty-two breastfed (20 exclusively) infants with an average age of 16.6 weeks (range 4 to 28 weeks) whose mothers were receiving an average of 124 mg sertraline daily for at least 14 days for severe depression were studied. Infant serum levels were measured 2.2 hours (range 0.5 to 5 hours) after nursing. Four infants had detectable sertraline (>2 mcg/L) and 11 infants had detectable norsertraline in their serum with an average concentration of 22 mcg/L. One 11-week-old infant who was being treated for acute asthma with albuterol, inhaled corticosteroids and hydroxyzine had serum levels higher than its mother's, even though 4 other infants received higher doses of sertraline and norsertraline through milk.[11]
In 6 breastfed (extent not stated) infants aged 5 to 34 weeks whose mothers were taking sertraline in an average daily dosage of 15 mg (range 5 to 34 mg), sertraline and norsertraline were undetectable (<3.4 mcg/L).[12]
In a study of mothers given sertraline prophylactically for recurrent postpartum depression, 7 opted to breastfeed. Infant serum was tested at 4 weeks of age with a maternal dosage of 50 mg daily. Sertraline (<2 mcg/L) and norsertraline (<12 mcg/L) were undetectable in the serum of any infant.[21]
In a study comparing sertraline to nortriptyline for postpartum depression, 13 infants were breastfed by mothers taking sertraline (dosage and extent of nursing were not stated). After a constant maternal sertraline dosage for at least 14 days, infants had their serum concentrations measured. The infants were an average of 5.9 weeks old at the time of serum sampling. Sertraline was not detectable (<2 mcg/L) in any of the infants' serum; norsertraline serum levels ranged from undetectable (<2 mcg/L) to 6 mcg/L.[22]
At 2 months postpartum, the breastfed infants of 4 mothers taking an average of 87.5 mg of sertraline daily had undetectable (<0.1 mcg/L) serum levels of sertraline and norsertraline.[13]
A 33-week preterm infant was exclusively breastfed by a mother who was taking sertraline 150 mg daily during gestation, at delivery and postpartum. Because of symptoms similar to neonatal abstinence syndrome, the infant's serum concentrations of sertraline and desmethylsertraline were measured on day 5 postpartum. Levels were 13 and 52 mcg/L, respectively. Because of ongoing symptoms, breastfeeding was stopped on day 9 and the infant's serum levels reportedly dropped, although specific values were not presented in the paper. The infant was later found to have genetically intermediate metabolism of two of the CYP450 enzymes involved in sertraline metabolism.[14]
Authors of a metaanalysis on sertraline reported infant serum levels of sertraline and norsertraline in 25 infants who were breastfed by mothers taking sertraline. Ten of the infants were exclusively breastfed, two were 80% breastfed and the breastfeeding status of the others was not reported. Only two infants, both exclusively breastfed, had detectable serum sertraline levels of 2.1 and 2.4 mcg/L. The other infants had undetectable (<2 mcg/L) sertraline levels. Four other infants had detectable norsertraline levels ranging from 2.6 to 4.7 mcg/L. Sampling times were not reported.[6]
Effects in Breastfed Infants
Two side effects possibly related to sertraline in breastmilk have been reported to the Australian Adverse Drug Reaction Advisory Committee. Benign neonatal sleep myoclonus occurred in one 4-month-old infant and agitation that spontaneously resolved was reported in another infant.[23,24]
None of 26 infants with an average age of 16.6 weeks (range 4 to 28 weeks) whose mothers were receiving an average of 124 mg sertraline daily had any detectable acute adverse reactions to sertraline in breastmilk. All had been breastfeeding for at least 3 weeks.[11]
Whole blood serotonin levels were measured in 14 mothers and their breastfed infants after 6 to 16 weeks of sertraline therapy. Maternal dosages ranged from 25 to 200 mg daily. Although maternal serotonin levels were decreased from 159 mcg/L to 19 mcg/L by sertraline therapy, infant serotonin levels averaged 227 mcg/L before and 224 mcg/L after maternal therapy. The authors concluded that these findings indicate that the amount of sertraline ingested by the infants was not sufficient to affect platelet serotonin uptake in breastfed infants. Platelets and neurons both have the same serotonin transporter, so this lack of effect was seen as indirect evidence of safety of sertraline use during breastfeeding. None of the infants experienced any adverse effects from sertraline in breastmilk, including 6 exclusively breastfed infants under 3 months of age.[25]
Twenty-five mothers who took an average sertraline dosage of 82.4 mg daily breastfed their infants exclusively for 4 months and breastfed at least 50% during months 5 and 6. Their infants had 6-month weight gains that were normal according to national growth standards and the mothers reported no abnormal effects in their infants.[26]
In 6 infants aged 5 to 34 weeks whose mothers were taking sertraline 50 to 100 mg daily, no adverse reactions were noted clinically at the time of the study.[12]
No adverse effects were seen in 7 infants who were 4 weeks old and whose mothers had been taking sertraline 50 mg daily since day 4 postpartum.[21]
One study of side effects of SSRI antidepressants in nursing mothers found no adverse reactions that required medical attention among 2 infants whose mother was taking sertraline. No specific information on maternal sertraline dosage, extent of breastfeeding or infant age was reported.[27]
A small study compared the reaction to pain in infants of depressed mothers who had taken an SSRI during pregnancy alone or during pregnancy and nursing, to a control group of unexposed infants of nondepressed mothers. Infants exposed to an SSRI either prenatally alone or prenatally and postnatally via breastmilk had blunted responses to pain compared to control infants. Four of the 30 infants were exposed to sertraline. Because there was no control group of depressed, nonmedicated mothers, an effect due to maternal behavior caused by depression could not be ruled out. The authors stressed that these findings did not warrant avoiding drug treatment of depression during pregnancy or avoiding breastfeeding during SSRI treatment.[13]
An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation.[28]
In a telephone follow-up study, 124 mothers who took a benzodiazepine while nursing reported whether their infants had any signs of sedation. One mother who was taking sertraline 50 mg daily, zopiclone 2.5 mg about every 3 days as needed, and also took alprazolam 0.25 mg on 2 occasions, reported sedation in her breastfed infant.[29]
A mother was taking sertraline 150 mg daily during gestation, at delivery and postpartum while exclusively breastfeeding her infant. Her preterm infant born by cesarean section at 33 weeks gestation developed hyperthermia, muscle tone regulation disorders, and high-pitched crying during the first 24 hours after birth. The symptoms worsened on the 4th day of life, but breastfeeding was continued. On day 5, the infant had serum concentrations of sertraline and its metabolite that are in the reported therapeutic range in adults. Breastfeeding was discontinued on day 9 postpartum and the infant's symptoms dissipated, serum drug levels decreased and the infant thrived over several months. The infant was later found to have genetically intermediate metabolism of two of the CYP450 enzymes involved in sertraline metabolism. The authors attributed the infant's symptoms to serotonergic overstimulation caused by persistently high sertraline levels from breastfeeding and reduced metabolism.[14] The reaction was probably caused by sertraline.
An infant was being breastfed (extent not stated) by a mother who began taking sertraline 50 mg daily and methylphenidate after 5 weeks postpartum. Dosage was started at 10 mg daily with an immediate-release product and gradually increased to 72 mg daily of an extended-release product. At 14 weeks of age, the infant was developing normally with no feeding difficulties. Examinations at 6 months and 1 year of age found no developmental problems in the child.[30]
In a study of sertraline for postpartum depression, 11 women completed the full 7-week duration of the study out of 36 who were entered. Six mothers reported breastfeeding their infants (extent not stated) and 5 did not breastfeed their infants. The average sertraline dose at week 7 was 100 mg daily. No side effects were reported for any of the infants in the sertraline or placebo groups at this time.[31]
Authors of a metaanalysis on sertraline reported 25 infants who were breastfed by mothers taking sertraline. Ten of the infants were exclusively breastfed, two were 80% breastfed and the breastfeeding status of the others was not reported. No adverse reactions occurred.[6]
A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. Sixty-eight of the infants were exposed to sertraline in utero.[32]
A retrospective study of 30 nursing mothers who had been seen at a psychiatric outpatient facility, followed for at least 8 weeks, and prescribed sertraline found that adverse effects were reported in 5 (13%) of their infants. One mother was taking 25 mg daily, 3 mothers were taking 50 mg daily and 1 was taking 100 mg daily. The most commonly reported adverse events in the infants were insomnia and restlessness; constant crying and poor feeding were less commonly reported. All of the adverse effects developed within the first 2 weeks after initiation of maternal treatment and disappeared within the 3 days after drug discontinuation. Adverse effects failed to disappear in one infant after reducing the maternal dosage from 50 mg daily to 25 mg daily. There was no difference in prevalence of adverse effects between these infants and those in the same study whose mothers were prescribed paroxetine.[33]
A 12-day-old exclusively breastfed male infant presented with severe weight loss and hypernatremic dehydration because of inadequate milk intake and a 30% weight loss since birth. The infant's mother was being treated for bipolar disorder with lamotrigine 250 mg orally once daily, aripiprazole 15 mg orally once daily, and sertraline 100 mg orally once daily. She was also taking levothyroxine 50 mcg once daily, a prenatal multivitamin, and folic acid. On initial evaluation in the emergency department, he was pale, with marbled skin, dry mucous membranes, decreased skin turgor, and bluish feet with prolonged capillary refill. The right foot eventually became darker with blackened toes and he developed gangrene of the right lower limb, which did not respond to medical therapy and required amputation of all five toes and surgical debridement of the metatarsals. Necrosis was attributed to arterial microthrombi caused by disseminated intravascular coagulation after severe dehydration. The authors considered the mother's medications as a possible cause of the dehydration and related problems.[34]
A mother who was exclusively breastfeeding a 2-month-old infant began taking sertraline 50 mg daily for depression. Six days later, restlessness and a dramatic decrease in the duration of sleep in the baby was reported. Sertraline was discontinued and the symptoms completely resolved within 3 days. No abnormalities were seen on physical examination or laboratory tests. The infant subsequently developed severe constipation with maternal paroxetine use, but tolerated maternal citalopram use.[35]
A mother who was 3 months postpartum was treated for depression with sertraline 50 mg in the morning and olanzapine 1.25 mg at night at night for sleep. After 2 weeks, the sertraline dosage was increased to 25 mg in the morning and 50 mg at night. Five days after the dosage increase, her breastfed infant began having diarrhea about 15 minutes after each feeding. She continued the medication and provided oral rehydration solution to the infant. The diarrhea resolved after 2 weeks. The diarrhea was probably caused by sertraline in breastmilk.[36]
Nine women treated with sertraline 25 to 75 mg daily (7 were taking 50 mg daily) during the third trimester of pregnancy and during breastfeeding. Pediatric evaluations including neurologic assessments and brain ultrasound were conducted during the first 24 hours postpartum. Further follow-up was conducted at 6 or more months of age. Infant clinical status was comparable to unexposed infants from the same pediatric department.[17]
A case-control study in Israel compared 280 infants of nursing mothers taking long-term psychotropic drugs to the infants of 152 women taking antibiotics. Infant sleepiness at 3 days of age was reported by 1 mother taking sertraline during pregnancy and breastfeeding and by none taking antibiotics. The sleepiness resolved within 24 hours with no developmental effect.[37]
Effects on Lactation and Breastmilk
Sertraline has caused galactorrhea in nonpregnant, nonnursing patients.[38-42] However, in a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, sertraline was not found to have an increased risk of causing hyperprolactinemia compared to other drugs.[43] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
A midwife observed 6 patients who reported a decrease in milk supply after starting sertraline (dosages not reported). One of the mothers had been taking sertraline since the 6th month of pregnancy. She reported an increase in milk supply when she stopped sertraline for one week at 4 months postpartum. When she restarted sertraline, her milk supply reportedly decreased. In all of the women, the milk supply increased in 2 to 3 days after increasing fluid and the frequency of nursing.[44]
In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior in the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum.[45]
A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups.[46]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[47] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575; sertraline n = 200) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[48]
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[49]
Alternate Drugs to Consider
References
- 1.
- Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry 2004;161:1066-78. [PubMed: 15169695]
- 2.
- The Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #18: Use of antidepressants in nursing mothers. Breastfeed Med 2008;3:44-52. [PubMed: 18333769]
- 3.
- Berle JO, Spigset O. Antidepressant use during breastfeeding. Curr Womens Health Rev 2011;7:28-34. [PMC free article: PMC3267169] [PubMed: 22299006]
- 4.
- Larsen ER, Damkier P, Pedersen LH, et al. Use of psychotropic drugs during pregnancy and breast-feeding. Acta Psychiatr Scand Suppl 2015;445:1-28. [PubMed: 26344706]
- 5.
- Orsolini L, Bellantuono C. Serotonin reuptake inhibitors and breastfeeding: A systematic review. Hum Psychopharmacol 2015;30:4-20. [PubMed: 25572308]
- 6.
- Pinheiro E, Bogen DL, Hoxha D, et al. Sertraline and breastfeeding: Review and meta-analysis. Arch Womens Ment Health 2015;18:139-46. [PMC free article: PMC4366287] [PubMed: 25589155]
- 7.
- McAllister-Williams RH, Baldwin DS, Cantwell R, et al. British Association for Psychopharmacology consensus guidance on the use of psychotropic medication preconception, in pregnancy and postpartum 2017. J Psychopharmacol 2017;31:519-52. [PubMed: 28440103]
- 8.
- Molenaar NM, Kamperman AM, Boyce P, Bergink V. Guidelines on treatment of perinatal depression with antidepressants: An international review. Aust N Z J Psychiatry 2018;52:320-27. [PMC free article: PMC5871019] [PubMed: 29506399]
- 9.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther 2021;28:e118-e126. [PubMed: 30601177]
- 10.
- Grzeskowiak LE, Leggett C, Costi L, et al. Impact of serotonin reuptake inhibitor use on breast milk supply in mothers of preterm infants: A retrospective cohort study. Br J Clin Pharmacol 2018;84:1373-9. [PMC free article: PMC5980248] [PubMed: 29522259]
- 11.
- Stowe ZN, Stowe MD, Hostetter AL, et al. The pharmacokinetics of sertraline excretion into human breast milk: Determinants of infant serum concentrations. J Clin Psychiatry 2003;64:73-80. [PubMed: 12590627]
- 12.
- Berle JØ, Steen VM, Aamo TO, et al. Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: Infant exposure, clinical symptoms, and cytochrome P450 genotypes. J Clin Psychiatry 2004;65:1228-34. [PubMed: 15367050]
- 13.
- Oberlander TF, Grunau RE, Fitzgerald C, et al. Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics 2005;115:411-25. [PubMed: 15687451]
- 14.
- Müller MJ, Preuß C, Paul T, et al. Serotonergic overstimulation in a preterm infant after sertraline intake via breastmilk. Breastfeed Med 2013;8:327-9. [PubMed: 23249132]
- 15.
- Salazar FR, D'Avila FB, de Oliveira MH, et al. Development and validation of a bioanalytical method for five antidepressants in human milk by LC-MS. J Pharm Biomed Anal 2016;129:502-8. [PubMed: 27497651]
- 16.
- Weisskopf E, Panchaud A, Nguyen KA, et al. Simultaneous determination of selective serotonin reuptake inhibitors and their main metabolites in human breast milk by liquid chromatography-electrospray mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 2017;1057:101-9. [PubMed: 28511118]
- 17.
- Pogliani L, Baldelli S, Cattaneo D, et al. Selective serotonin reuptake inhibitors passage into human milk of lactating women. J Matern Fetal Neonatal Med 2019;32:3020-5. [PubMed: 29557689]
- 18.
- Schoretsanitis G, Augustin M, Sassmannshausen H, et al. Antidepressants in breast milk; Comparative analysis of excretion ratios. Arch Womens Ment Health 2019;22:383-90. [PubMed: 30116895]
- 19.
- Cardoso E, Monfort A, Eap C, et al. A population pharmacokinetic model for sertraline in depressive patients during the perinatal period: prediction of infant drug exposure through human milk. Gynecol Obstet Invest 2023;88:24-5. doi:10.1159/000531140 [CrossRef]
- 20.
- Hendrick V, Fukuchi A, Altshuler L, et al. Use of sertraline, paroxetine and fluvoxamine by nursing women. Br J Psychiatry 2001;179:163-6. [PubMed: 11483479]
- 21.
- Sunder KR, Wisner KL, Hanusa BH, Perel JM. Postpartum depression recurrence versus discontinuation syndrome: Observations from a randomized controlled trial. J Clin Psychiatry 2004;65:1266-8. [PubMed: 15367055]
- 22.
- Wisner KL, Hanusa BH, Perel JM, et al. Postpartum depression: A randomized trial of sertraline versus nortriptyline. J Clin Psychopharmacol 2006;26:353-60. [PubMed: 16855451]
- 23.
- Rohan A. Drug distribution in human milk. Aust Prescr 1997;20:84.
- 24.
- Mammen OK, Perel JM, Rudolph G, et al. Sertraline and norsertraline levels in three breastfed infants. J Clin Psychiatry 1997;58:100-3. [PubMed: 9108810]
- 25.
- Epperson N, Czarkowski KA, Ward-O'Brien D, et al. Maternal sertraline treatment and serotonin transport in breast-feeding mother-infant pairs. Am J Psychiatry 2001;158:1631-7. [PubMed: 11578995]
- 26.
- Hendrick V, Smith LM, Hwang S, et al. Weight gain in breastfed infants of mothers taking antidepressant medications. J Clin Psychiatry 2003;64:410-2. [PubMed: 12716242]
- 27.
- Lee A, Woo J, Ito S. Frequency of infant adverse events that are associated with citalopram use during breast-feeding. Am J Obstet Gynecol 2004;190:218-21. [PubMed: 14749663]
- 28.
- Hale TW, Kendall-Tackett K, Cong Z, et al. Discontinuation syndrome in newborns whose mothers took antidepressants while pregnant or breastfeeding. Breastfeed Med 2010;5:283-8. [PubMed: 20807106]
- 29.
- Kelly LE, Poon S, Madadi P, Koren G. Neonatal benzodiazepines exposure during breastfeeding. J Pediatr 2012;161:448-51. [PubMed: 22504099]
- 30.
- Bolea-Alamanac BM, Green A, Verma G, et al. Methylphenidate use in pregnancy and lactation: A systematic review of evidence. Br J Clin Pharmacol 2014;77:96-101. [PMC free article: PMC3895350] [PubMed: 23593966]
- 31.
- Hantsoo L, Ward-O'Brien D, Czarkowski KA, et al. A randomized, placebo-controlled, double-blind trial of sertraline for postpartum depression. Psychopharmacology (Berl) 2014;231:939-48. [PMC free article: PMC3945214] [PubMed: 24173623]
- 32.
- Kieviet N, Hoppenbrouwers C, Dolman KM, et al. Risk factors for poor neonatal adaptation after exposure to antidepressants in utero. Acta Paediatr 2015;104:384-91. [PubMed: 25559357]
- 33.
- Uguz F, Arpaci N. Short-term safety of paroxetine and sertraline in breastfed infants: A retrospective cohort study from a university hospital. Breastfeed Med 2016;11:487-9. [PubMed: 27575664]
- 34.
- Morin C, Chevalier I. Severe hypernatremic dehydration and lower limb gangrene in an infant exposed to lamotrigine, aripiprazole, and sertraline in breast milk. Breastfeed Med 2017;12:377-80. [PubMed: 28481632]
- 35.
- Uguz F. Better tolerance of citalopram in a breastfed infant who could not tolerate sertraline and paroxetine. Breastfeed Med 2018;13:89-90. [PubMed: 29185803]
- 36.
- Uvais NA. Self-limiting diarrhea in an infant exposed to sertraline in breast milk. J Family Med Prim Care 2017;6:876-7. [PMC free article: PMC5848419] [PubMed: 29564284]
- 37.
- Kronenfeld N, Ziv Baran, T, Berlin M, et al. Chronic use of psychotropic medications in breastfeeding women: Is it safe? PLoS One 2018;13:e0197196. [PMC free article: PMC5962050] [PubMed: 29782546]
- 38.
- Lesaca TG. Sertraline and galactorrhea. J Clin Psychopharmacol 1996;16:333-4. [PubMed: 8835712]
- 39.
- Bronzo MR, Stahl SM. Galactorrhea induced by sertraline. Am J Psychiatry 1993;150:1269-70. [PubMed: 8093119]
- 40.
- Nebhinani N. Sertraline-induced galactorrhea: case report and review of cases reported with other SSRIs. Gen Hosp Psychiatry 2013;35:576.e3-5. [PubMed: 23260337]
- 41.
- Suthar N, Pareek V, Nebhinani N, Suman DK. Galactorrhea with antidepressants: A case series. Indian J Psychiatry 2018;60:145-6. [PMC free article: PMC5914246] [PubMed: 29736080]
- 42.
- Luo T, Liu QS, Yang YJ, Wei B. Aripiprazole for the treatment of duloxetine-induced hyperprolactinemia: A case report. J Affect Disord 2019;250:330-2. [PubMed: 30875676]
- 43.
- Trenque T, Herlem E, Auriche P, Drame M. Serotonin reuptake inhibitors and hyperprolactinaemia: A case/non-case study in the French pharmacovigilance database. Drug Saf 2011;34:1161-6. [PubMed: 22077504]
- 44.
- Holland D. An observation of the effect of sertraline on breast milk supply. Aust N Z J Psychiatry 2000;34:1032. [PubMed: 11127615]
- 45.
- Marshall AM, Nommsen-Rivers LA, Hernandez LL, et al. Serotonin transport and metabolism in the mammary gland modulates secretory activation and involution. J Clin Endocrinol Metab 2010;95:837-46. [PMC free article: PMC2840848] [PubMed: 19965920]
- 46.
- Gorman JR, Kao K, Chambers CD. Breastfeeding among women exposed to antidepressants during pregnancy. J Hum Lact 2012;28:181-8. [PubMed: 22344850]
- 47.
- Venkatesh KK, Castro VM, Perlis RH, Kaimal AJ. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol 2017;37:1003-9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 48.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact 2017;33:701-9. [PubMed: 28984528]
- 49.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand 2022;101:344-54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
Sertraline
CAS Registry Number
79617-96-2
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Nortriptyline.[Drugs and Lactation Database (...]Review Nortriptyline.. Drugs and Lactation Database (LactMed®). 2006
- Review Lovastatin.[Drugs and Lactation Database (...]Review Lovastatin.. Drugs and Lactation Database (LactMed®). 2006
- Review Paroxetine.[Drugs and Lactation Database (...]Review Paroxetine.. Drugs and Lactation Database (LactMed®). 2006
- Review Diclofenac.[Drugs and Lactation Database (...]Review Diclofenac.. Drugs and Lactation Database (LactMed®). 2006
- Review Metolazone.[Drugs and Lactation Database (...]Review Metolazone.. Drugs and Lactation Database (LactMed®). 2006
- Sertraline - Drugs and Lactation Database (LactMed®)Sertraline - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
