Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 58-73-1
Drug Levels and Effects
Summary of Use during Lactation
Small, occasional doses of diphenhydramine would not be expected to cause any adverse effects in breastfed infants. Larger doses or more prolonged use may cause effects in the infant or decrease the milk supply, particularly in combination with a sympathomimetic such as pseudoephedrine or before lactation is well established. Single bedtime doses after the last feeding of the day may be adequate for many women and will minimize any effects of the drug. The nonsedating antihistamines are preferred alternatives.
Drug Levels
Maternal Levels. One old study that used a biologic assay system reported that after a 100 mg intramuscular dose of diphenhydramine in four women, drug levels in milk were undetectable in two and 42 and 100 mcg/L in two others at one hour after the dose. Five hours after the dose, milk levels were undetectable in two women and 20 and 100 mcg/L in two others.[1] No studies using modern assay methods have been reported.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
In one telephone follow-up study, mothers reported irritability and colicky symptoms 10% of infants exposed to various antihistamines and drowsiness was reported in 1.6% of infants. None of the reactions required medical attention. In this study, drowsiness was reported in 1 infant of 12 exposed to diphenhydramine in breastmilk.[2]
Effects on Lactation and Breastmilk
Antihistamines in relatively high doses given by injection can decrease basal serum prolactin in nonlactating women and in early postpartum women.[3,4] However, suckling-induced prolactin secretion is not affected by antihistamine pretreatment of postpartum mothers.[3] Whether lower oral doses of diphenhydramine have the same effect on serum prolactin or whether the effects on prolactin have any consequences on breastfeeding success have not been studied. The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
One woman became dependent on dimenhydrinate (which is 55% diphenhydramine) during her first pregnancy and continued to take it in a dose of 150 mg (83 mg diphenhydramine) daily while she breastfed her infant for 3 months. The infant did well except for a febrile seizure at 2 years of age, which was probably unrelated to dimenhydrinate. During her second pregnancy, she took dimenhydrinate 300 mg (165 mg diphenhydramine) daily during the pregnancy and while breastfeeding her infant for 2 years.[5]
Alternate Drugs to Consider
References
- 1.
- Rindi V. La eliminazione degli antistaminici di sintesi con il latte e l'azione latto-goga de questi. Riv Ital Ginecol. 1951;34:147–57.
- 2.
- Ito S, Blajchman A, Stephenson M, et al. Prospective follow-up of adverse reactions in breast-fed infants exposed to maternal medication. Am J Obstet Gynecol. 1993;168:1393–9. [PubMed: 8498418]
- 3.
- Pontiroli AE, De Castro e Silva E, Mazzoleni F, et al. The effect of histamine and H1 and H2 receptors on prolactin and luteinizing hormone release in humans: Sex differences and the role of stress. J Clin Endocrinol Metab. 1981;52:924–8. [PubMed: 7228996]
- 4.
- Messinis IE, Souvatzoglou A, Fais N, et al. Histamine H1 receptor participation in the control of prolactin secretion in postpartum. J Endocrinol Invest. 1985;8:143–6. [PubMed: 3928731]
- 5.
- Kaya FD. A patient with dimenhydrinate dependence: A case report. Klin Psikofarmakol Bull. 2014;24:184–7. [CrossRef]
Substance Identification
Substance Name
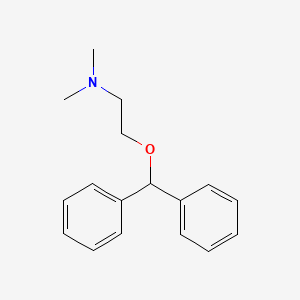
Diphenhydramine
CAS Registry Number
58-73-1
Drug Class
Breast Feeding
Lactation
Antihistamines
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.