Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 38396-39-3
Drug Levels and Effects
Summary of Use during Lactation
Because of the low levels of bupivacaine in breastmilk, and it is not orally absorbed, amounts received by the infant are small and it has not caused any adverse effects in breastfed infants.
Bupivacaine during labor and delivery with other anesthetics and analgesics has been reported by some to interfere with breastfeeding. However, this assessment is controversial and complex because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used and deficient design of many of the studies. In contrast, epidural bupivacaine begun after clamping of the umbilical cord appears to enhance breastfeeding success because of improved pain control. Overall, it appears that with good breastfeeding support epidural bupivacaine with or without fentanyl or one of its derivatives has little or no adverse effect on breastfeeding success.[1-6] Labor pain medication may delay the onset of lactation.
Drug Levels
Maternal Levels. Bupivacaine milk levels were measured in 5 women who were given epidural bupivacaine analgesia (dosage not stated) for vaginal delivery. Bupivacaine was undetectable (<20 mcg/L) in all samples taken at 2, 8, 24 and 48 hours postpartum.[7]
One woman received intrapleural bupivacaine 50 mg, followed in 1 hour by a continuous infusion of 25 mg/hour for 5 days for operative and postoperative analgesia. Four milk samples were taken during the infusion. The milk bupivacaine level was 400 mcg/L at 6 hours after the bolus dose and approximately 200 mcg/L at 24, 48 and 72 hours after the bolus dose.[8]
Twenty-seven women received epidural lidocaine 2% and bupivacaine 0.5% for pain control during cesarean delivery. Bupivacaine dosage averaged 82 mg (range 25 to 168 mg). Average milk bupivacaine concentrations were 90 mcg/L at 2 hours after delivery, 60 mcg/L at 4 hours after delivery and 40 mcg/L at 12 hours after delivery.[9]
Twenty women undergoing cesarean section deliveries with epidural anesthesia were randomized to receive either bupivacaine 0.5% (n = 10) or levobupivacaine 0.5% (n = 10) in a single-blinded study. The drugs were given as 0.5 mL (2.5 mg) boluses as needed up to 150 mg (mean 82.5 mg). Blood and milk samples were obtained before and 0.5, 1, 2, 6, 12 and 24 hours after administration of the drugs. Bupivacaine was detected in breastmilk 30 minutes after administration, with the peak milk concentration of about 0.2 mg/L occurring at about 2 hours after administration. Levobupivacaine was almost at baseline level by 7 hours and absent from milk (<5 mcg/L) by 24 hours after the dose. The passage of levobupivacaine into breastmilk was virtually identical.[10]
Thirty patients who underwent cesarean section received a bilateral transverses abdominus plane block using of a mixture of 52 mg bupivacaine hydrochloride 0.25% and 266 mg liposomal bupivacaine 1.3%. Simultaneous blood and milk samples were collected at either 2, 12 and 48 hours after the dose or at 6, 24, 72 and 96 hours after the dose. The peak concentration in breastmilk averaged 58 mcg/L at 6 hours after the dose, then slowly declined to an average of 5.2 mcg/L at 96 hours after the dose. The authors estimated that an exclusively breastfed infant would receive a total weight-adjusted dosage of about 0.4% of the mother’s dosage over 96 hours, although this value might be artificially high because milk volume is smaller than average in the first 3-4 days postpartum.[11]
Infant Levels. One woman who was 10 months postpartum received intrapleural bupivacaine 50 mg, followed in 1 hour by a continuous intrapleural infusion of 25 mg/hour for 5 days for operative and postoperative analgesia. Breastfeeding resumed postoperatively 22 hours after the start of the infusion. A serum sample taken from the infant 5 hours after the morning feeding on day 3 postoperatively (52.5 hours after the bolus dose) contained undetectable (lower limit not stated) amounts of bupivacaine by gas chromatography.[8]
Effects in Breastfed Infants
Bupivacaine administered to the mother by the epidural route for labor analgesia had no apparent adverse effect on 13 breastfed infants.[9]
Thirty patients who underwent cesarean section received a bilateral transverses abdominus plane block using of a mixture of 52 mg bupivacaine hydrochloride 0.25% and 266 mg liposomal bupivacaine 1.3%. Two of the infants had transient tachypnea, but causality could not be determined. None of the infants required hospital readmission during the 14-day follow-up period.[11]
Effects on Lactation and Breastmilk
Thirty women who delivered by cesarean section received either spinal anesthesia (not defined) alone (n = 15) or spinal anesthesia plus bupivacaine (n = 15) by extradural infusion after clamping the umbilical cord. A bupivacaine bolus of 12.5 mg was followed by a continuous infusion of 17.5 mg/hour for 3 days postpartum. Patients who received bupivacaine had better pain relief as indicated by lower pain scores and a lower consumption of supplemental diclofenac for pain. Bupivacaine-treated patients also produced more milk per day than the untreated women, a difference that was statistically significant from day 3 to the end of the study on day 11 postpartum. The authors concluded that improved pain relief improved breastfeeding performance.[12]
Twenty women who delivered by cesarean section received either bupivacaine alone or bupivacaine plus buprenorphine by extradural infusion after clamping the umbilical cord. A bupivacaine bolus of 12.5 mg was followed by a continuous infusion of 17.5 mg/hour for 3 days. The buprenorphine was given as a bolus of 200 mcg followed by 8.4 mcg/hour for 3 days. Patients started breastfeeding as soon as they were able to sit up. Both the amount of milk fed and infant weight increased in both groups over the first 10 days postpartum; however, the increases were greater in those who received bupivacaine alone.[13]
A prospective cohort study compared women who received no analgesia (n = 63) to women who received continuous epidural analgesia with fentanyl and either bupivacaine 0.05 to 0.1% (n = 39) or ropivacaine (n = 13) during labor and delivery. The total dosage of bupivacaine was 31 to 62 mg and the average total infusion time from start to delivery was 219 minutes. The study found no differences between the groups in breastfeeding effectiveness or infant neurobehavioral status at 8 to 12 hours postpartum or the number exclusively or partially breastfeeding at 4 weeks postpartum.[14]
A randomized, prospective study measured infant breastfeeding behavior following epidural or intravenous fentanyl during delivery in 100 multiparous mothers undergoing cesarean section and delivering full-term, healthy infants. The epidural group received epidural bupivacaine 100 mg initially, followed by a continuous infusion of 25 mg/hour. The intravenous fentanyl group received a spinal injection of 15 to 20 mg of bupivacaine. A slight difference was seen in breastfeeding behavior between the groups, with the infants in the intravenous fentanyl group performing slightly worse than those in the epidural group. However, all mothers were able to breastfeed their infants at 24 hours. None had severe breastfeeding problems; 10 women in the epidural group reported mild or moderate problems and 7 women in the intravenous group reported breastfeeding problems. Twenty mothers in the epidural group and 14 in the intravenous group used supplemental bottle feeding, with the difference not statistically significant.[15]
A randomized, but nonblinded, study in women undergoing cesarean section compared epidural anesthesia with bupivacaine to general anesthesia with intravenous thiopental 4 mg/kg and succinylcholine 1.5 mg/kg for induction followed by nitrous oxide and isoflurane. The time to the first breastfeed was significantly shorter (107 vs 228 minutes) with the epidural anesthesia than with general anesthesia. This difference was probably caused by the anesthesia's effects on the infant, because the Apgar and neurologic and adaptive scores were significantly lower in the general anesthesia group of infants.[16]
A randomized, multicenter trial compared the initiation rate and duration of breastfeeding in women who received high-dose epidural bupivacaine alone, or one of two low-dose combinations of bupivacaine plus fentanyl. A nonepidural matched control group was also compared. No differences in breastfeeding initiation rates or duration were found among the epidural and nonmedicated, nonepidural groups.[17]
A nonrandomized study in low-risk mother-infant pairs found that there was no difference overall in the amount of sucking by newborns, whether their mothers received bupivacaine plus fentanyl, or fentanyl alone by epidural infusion in various dosages, or received no analgesia for childbirth. In a subanalysis by sex and number of sucks, female infants were affected by high-dose bupivacaine and high-dose fentanyl, but male infant were not.[18] However, the imbalance of many factors between the study groups makes this study difficult to interpret.
In a prospective cohort study, 87 multiparous women who received epidural bupivacaine and fentanyl for pain control during labor and vaginal delivery. A loading dose of 0.125% bupivacaine with fentanyl 50-100 mcg. Epidural analgesia is maintained using 0.0625% bupivacaine and fentanyl 0.2 mcg/mL. The median dose of fentanyl received by the women was 151 mcg (range 30 to 570 mcg). The women completed questionnaires at 1 and 6 weeks postpartum regarding breastfeeding. Most women had prior experience with breastfeeding, support at home and ample time off from work. All women were breastfeeding at 1 week postpartum and 95.4% of women were breastfeeding at 6 weeks postpartum.[19]
A national survey of women and their infants from late pregnancy through 12 months postpartum compared the time of lactogenesis II in mothers who did and did not receive pain medication during labor. Categories of medication were spinal or epidural only, spinal or epidural plus another medication, and other pain medication only. Women who received medications from any of the categories had about twice the risk of having delayed lactogenesis II (>72 hours) compared to women who received no labor pain medication.[20]
A randomized study compared the effects of cesarean section using general anesthesia, spinal anesthesia, or epidural anesthesia, to normal vaginal delivery on serum prolactin and oxytocin as well as time to initiation of lactation. Spinal anesthesia used bupivacaine 10 to 11 mg of hypertonic 5% bupivacaine solution and epidural anesthesia used 10 mL (50 mg) of 0.5% bupivacaine. After delivery, patients in all groups received an infusion of oxytocin 30 international units in 1 L of saline, and 0.2 mg of methylergonovine if they were not hypertensive. Patients in the general anesthesia group (n = 21) had higher post-procedure prolactin levels and a longer mean time to lactation initiation (25 hours) than in the other groups (10.8 to 11.8 hours). Postpartum oxytocin levels in the nonmedicated vaginal delivery group were higher than in the general and spinal anesthesia groups and serum oxytocin in the epidural group were higher than those in the spinal group.[21]
A retrospective study in a Spanish public hospital compared the infants of mothers who received an epidural during labor that contained fentanyl and either bupivacaine or ropivacaine. Infants of mothers who received an epidural had a lower frequency of early breastfeeding.[22]
A randomized, double-blind study compared three epidural maintenance solutions for labor analgesia in women receiving epidural analgesia during labor: bupivacaine 1 mg/mL, bupivacaine 0.8 mg/mL with fentanyl 1 mcg/mL, or bupivacaine 0.625 mg/mL with fentanyl 2 mcg/mL. At 6 weeks postpartum, the breastfeeding rate was 94% or greater in all groups, with no difference among them. All mothers delivered full-term infants and were highly motivated to breastfeed and almost all had vaginal deliveries.[23]
A prospective cohort study in 1204 Israeli women on the effect of labor epidural analgesia during labor, the following protocol was used: bupivacaine 0.1% 15 mL and fentanyl 100 mcg in 5-mL increments, followed by an epidural infusion of bupivacaine 0.1% 10 mL and fentanyl 2 mcg/mL, with a patient-controlled epidural analgesia modality with 5 mL bolus with a lock-out time of 15 minutes. At 6 weeks postpartum, the breastfeeding and exclusive breastfeeding rates were lower (74% and 52%, respectively) in mothers who received the epidural analgesia than in those who did not (83% and 68%, respectively). However, the difference was mostly accounted for by parity, with the intervention having little effect on multiparous women.[24]
A retrospective study of women in a Turkish hospital who underwent elective cesarean section deliveries compared women who received bupivacaine spinal anesthesia (n = 170) to women who received general anesthesia (n = 78) with propofol for induction, sevoflurane for maintenance and fentanyl after delivery. No differences in breastfeeding rates were seen between the groups at 1 hour and 24 hours postpartum. However, at 6 months postpartum, 67% of women in the general anesthesia group were still breastfeeding compared to 81% in the spinal anesthesia group, which was a statistically significant difference.[25]
A study of 169 pregnant women randomized them to receive one of three solutions as epidural anesthesia during labor. Bupivacaine 0.1% or 0.125% was combined with sufentanil 5 mcg and bupivacaine 0.1% was combined with sufentanil 10 mcg, each in 15 mL. No difference in average LATCH score was found among the infants in the 3 groups.[26]
An observational study in Sweden compared nursing behaviors of the infants of mothers who received intravenous oxytocin or intramuscular oxytocin with or without receiving epidural analgesia with sufentanil (median dose 10 mcg) and bupivacaine (median dose 17.5 mg). Infants of mothers who received oxytocin infusions alone during labor breastfed as well as those of mothers who had no interventions during labor. Mothers who received oxytocin plus epidural analgesia had reduced breastfeeding behaviors and more weight loss at 2 days postpartum than those who did not receive epidural analgesia. The mothers of infants who breastfed well had greater variability in serum oxytocin than those whose infants did not breastfeed well.[27]
A nonrandomized, nonblinded study in a Serbian hospital of women near term who underwent cesarean section compared general anesthesia (n = 284) to spinal or epidural anesthesia (n = 249). Spinal anesthesia consisted of hyperbaric bupivacaine 12 mg and fentanyl 0.01 mg; epidural anesthesia consisted of isobaric bupivacaine 0.5% (0.5 mg per 10 cm height) and fentanyl 0.05 mg. General anesthesia consisted of propofol 2.3 mg/kg and succinylcholine 1.5 mg/kg for induction and intubation, followed by an anesthetic gas mixture and oxygen. Reportedly, nitric oxide (possibly nitrous oxide) was 50% of the gas before delivery and 67% after delivery. Sevoflurane was also used in some cases. After delivery and cord clamping, mothers received fentanyl 3 mcg/kg and rocuronium 0.5 mg/kg intravenously for placental delivery. After surgery, neuromuscular block reversal was performed with neostigmine and atropine. All patients received 1 mg/kg of diclofenac every 8 h for 24 hours after delivery and 98% of general anesthesia patients also received 100 mg of tramadol and 78.5% received acetaminophen 1 gram. No regional anesthesia patients received tramadol or acetaminophen. Patients receiving one of the regional anesthetic protocols established lactation sooner (56% and 29% after 18 and 24 hours, respectively), while 86% of women receiving general anesthesia did not establish lactation until 36 to 48 hours after surgery.[28]
Alternate Drugs to Consider
References
- 1.
- Reynolds F. Labour analgesia and the baby: Good news is no news. Int J Obstet Anesth 2011;20:38-50. [PubMed: 21146977]
- 2.
- Loubert C, Hinova A, Fernando R. Update on modern neuraxial analgesia in labour: A review of the literature of the last 5 years. Anaesthesia 2011;66:191-212. [PubMed: 21320088]
- 3.
- Shrestha B, Devgan A, Sharma M. Effects of maternal epidural analgesia on the neonate--a prospective cohort study. Ital J Pediatr 2014;40:99. [PMC free article: PMC4297456] [PubMed: 25492043]
- 4.
- Zuppa AA, Alighieri G, Riccardi R, et al. Epidural analgesia, neonatal care and breastfeeding. Ital J Pediatr 2014;40:82. [PMC free article: PMC4335561] [PubMed: 25432659]
- 5.
- French CA, Cong X, Chung KS. Labor epidural analgesia and breastfeeding: A systematic review. J Hum Lact 2016;32:507-20. [PubMed: 27121239]
- 6.
- Heesen P, Halpern SH, Beilin Y, et al. Labor neuraxial analgesia and breastfeeding: An updated systematic review. J Clin Anesth 2021;68:110105. [PubMed: 33069970]
- 7.
- Naulty JS, Ostheimer G, Datta S, et al. Bupivacaine in breast milk following epidural anesthesia for vaginal delivery. Reg Anesth 1983;8:44-5.
- 8.
- Baker PA, Schroeder D. Interpleural bupivacaine for postoperative pain during lactation. Anesth Analg 1989;69:400-2. [PubMed: 2774239]
- 9.
- Ortega D, Viviand X, Lorec AM, et al. Excretion of lidocaine and bupivacaine in breast milk following epidural anesthesia for cesarean delivery. Acta Anaesthesiol Scand 1999;43:394-7. [PubMed: 10225071]
- 10.
- Bolat E, Bestas A, Bayar MK, et al. Evaluation of levobupivacaine passage to breast milk following epidural anesthesia for cesarean delivery. Int J Obstet Anesth 2014;23:217-21. [PubMed: 24953218]
- 11.
- Mustafa HJ, Wong HL, Al-Kofahi M, et al. Bupivacaine pharmacokinetics and breast milk excretion of liposomal bupivacaine administered after cesarean birth. Obstet Gynecol 2020;136:70-6. [PMC free article: PMC7316148] [PubMed: 32541292]
- 12.
- Hirose M, Hara Y, Hosokawa T, et al. The effect of postoperative analgesia with continuous epidural bupivacaine after cesarean section on the amount of breast feeding and infant weight gain. Anesth Analg 1996;82:1166-9. [PubMed: 8638785]
- 13.
- Hirose M, Hosokawa T, Tanaka Y. Extradural buprenorphine suppresses breast feeding after cesarean section. Br J Anaesth 1997;79:120-1. [PubMed: 9301399]
- 14.
- Chang ZM, Heaman MI. Epidural analgesia during labor and delivery: Effects on the initiation and continuation of effective breastfeeding. J Hum Lact 2005;21:305-14. [PubMed: 16113019]
- 15.
- Goma HM, Said RN, El-Ela AM. Study of the newborn feeding behaviors and fentanyl concentration in colostrum after an analgesic dose of epidural and intravenous fentanyl in cesarean section. Saudi Med J 2008;29:678-82. [PubMed: 18454213]
- 16.
- Sener EB, Guldogus N, Karakaya D, et al. Comparison of neonatal effects of epidural and general anesthesia for cesarean section. Gynecol Obstet Invest 2003;55:41-5. [PubMed: 12624551]
- 17.
- Wilson MJ, Macarthur C, Cooper GM, et al. Epidural analgesia and breastfeeding: A randomised controlled trial of epidural techniques with and without fentanyl and a non-epidural comparison group. Anaesthesia 2010;65:145-53. [PubMed: 19912160]
- 18.
- Bell AF, White-Traut R, Medoff-Cooper B. Neonatal neurobehavioral organization after exposure to maternal epidural analgesia in labor. J Obstet Gynecol Neonatal Nurs 2010;39:178-90. [PubMed: 20409118]
- 19.
- Wieczorek PM, Guest S, Balki M, et al. Breastfeeding success rate after vaginal delivery can be high despite the use of epidural fentanyl: An observational cohort study. Int J Obstet Anesth 2010;19:273–7. [PubMed: 20627690]
- 20.
- Lind JN, Perrine CG, Li R. Relationship between use of labor pain medications and delayed onset of lactation. J Hum Lact 2014;30:167-73. [PMC free article: PMC4684175] [PubMed: 24451212]
- 21.
- Kutlucan L, Seker IS, Demiraran Y, et al. Effects of different anesthesia protocols on lactation in the postpartum period. J Turk Ger Gynecol Assoc 2014;15:233-8. [PMC free article: PMC4285212] [PubMed: 25584032]
- 22.
- Herrera-Gómez A, García-Martínez O, Ramos-Torrecillas J, et al. Retrospective study of the association between epidural analgesia during labour and complications for the newborn. Midwifery 2015;31:613-6. [PubMed: 25819707]
- 23.
- Lee AI, McCarthy RJ, Toledo P, et al. Epidural labor analgesia-fentanyl dose and breastfeeding success: A randomized clinical trial. Anesthesiology 2017;127:614-24. [PubMed: 28926440]
- 24.
- Orbach-Zinger S, Landau R, Davis A, et al. The effect of labor epidural analgesia on breastfeeding outcomes: A prospective observational cohort study in a mixed-parity cohort. Anesth Analg 2019;129:784-91. [PubMed: 31425221]
- 25.
- Karasu D, Yilmaz C, Ozgunay SE, et al. A comparison of the effects of general anaesthesia and spinal anaesthesia on breastfeeding. C R Acad Bulg Sci 2018;71:993-1000. doi:10.7546/CRABS.2018.07.17 [CrossRef]
- 26.
- Wang T, Lu Y, Zhou P, et al. A randomized controlled comparison of epidural analgesia onset time and adverse reactions during labor with different dose combinations of bupivacaine and sufentanil. Clin J Pain 2020;36:612-7. [PubMed: 32349005]
- 27.
- Takahashi Y, Uvnäs-Moberg K, Nissen E, et al. Epidural analgesia with or without oxytocin, but not oxytocin alone, administered during birth disturbs infant pre-feeding and sucking behaviors and maternal oxytocin levels in connection with a breastfeed two days later. Front Neurosci 2021;15:673184. [PMC free article: PMC8276259] [PubMed: 34267623]
- 28.
- Stanisic DM, Kalezic N, Rakic A, et al. Comparison of post-cesarean pain perception of general versus regional anesthesia, a single-center study. Medicina (Kaunas) 2022;59:44. [PMC free article: PMC9866267] [PubMed: 36676668]
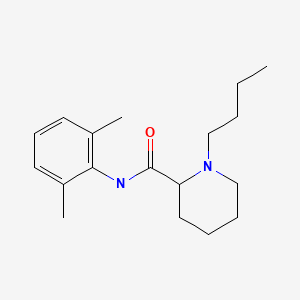
Substance Identification
Substance Name
Bupivacaine
CAS Registry Number
38396-39-3
Drug Class
Breast Feeding
Lactation
Milk, Human
Anesthetics, Local
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Levobupivacaine.[Drugs and Lactation Database (...]Review Levobupivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Ropivacaine.[Drugs and Lactation Database (...]Review Ropivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Review Lidocaine.[Drugs and Lactation Database (...]Review Lidocaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Mepivacaine.[Drugs and Lactation Database (...]Review Mepivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Bupivacaine - Drugs and Lactation Database (LactMed®)Bupivacaine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
