Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 84057-95-4
Drug Levels and Effects
Summary of Use during Lactation
Ropivacaine passes into milk poorly and is not orally absorbed by breastfed infants. Infants appear not to be affected by the small amounts of drug in breastmilk.
Local anesthetics administered during labor and delivery with other anesthetics and analgesics have been reported by some to interfere with breastfeeding. However, this assessment is controversial and complex because of the many different combinations of drugs, dosages and patient populations studied as well as the variety of techniques used. Published data on the use of ropivacaine and fentanyl used during labor and delivery in a small number of women found little or no adverse effect on breastfeeding in one study, but decreased milk production and reduced rate of breastfeeding in another.[1,2] Although not well studied specifically with ropivacaine, it appears that with good breastfeeding support, epidural local anesthetics with or without fentanyl or one of its derivatives has little or no adverse effect on breastfeeding success.[3] Labor pain medication may delay the onset of lactation.
Drug Levels
Maternal Levels. Twenty-five women undergoing cesarean section received ropivacaine 0.15% and fentanyl 2 mcg/mL for patient-controlled epidural analgesia at a basal rate of 6 mL (9 mg of ropivacaine)/hour and a demand dose of 4 mL (6 mg ropivacaine)/20 minutes. The cumulative maternal dosages of ropivacaine at 18 and 24 hours averaged 188 mg (range 69 to 296 mg), and 248 mg (131 to 378 mg), respectively. At 18 and 24 hours postpartum, colostrum ropivacaine concentrations averaged 246 mcg/L and 301 mcg/L, respectively.[4] Using these results, a neonate who ingests about 40 mL of colostrum during the first 24 hours of life would receive only 10 to 12 mcg of ropivacaine.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Twenty-five infants whose mothers received a combination of ropivacaine and fentanyl for patient-controlled epidural analgesia for pain associated with cesarean section had normal Apgar and Neurological and Adaptive Capacity scores. No adverse effects were noted in any of the infants.[4]
Effects on Lactation and Breastmilk
A prospective cohort study compared women who received no analgesia (n = 63) to women who received continuous epidural analgesia with fentanyl and either 0.08 or 0.2% ropivacaine (n = 13) or bupivacaine (n = 39) during labor and delivery. The total dosage of ropivacaine was 50 to 124 mg and the average total infusion time from start to delivery was 219 minutes. The study found no differences between the groups in breastfeeding effectiveness or infant neurobehavioral status at 8 to 12 hours postpartum or the number exclusively or partially breastfeeding at 4 weeks postpartum.[5]
A randomized, prospective study compared mothers who received epidural labor analgesia with ropivacaine (n = 75) to mothers who did not receive labor analgesia (n = 49). In the treatment group, 3 mL of ropivacaine 0.125% was injected epidurally, followed in some mothers by an additional 12 mL. In all treated mothers, 5 mL per hour was then given as a continuous epidural infusion. Although serum prolactin concentrations were somewhat lower in the group who received ropivacaine, no difference was seen between the groups in time of lactation onset, number of women with extensive lactation, and the decrease in infant weight reduction.[6]
A nonrandomized study at one Italian hospital compared primiparous mothers undergoing vaginal delivery who received epidural analgesia (n = 64) to those who did not (n = 64). Mothers who requested the epidural analgesia received an initial dose of 100 mcg of fentanyl diluted to 10 mL with saline. After the initial fentanyl, doses of 15 to 20 mL of 0.1% ropivacaine were administered, if needed; however, the number of women who received ropivacaine was not reported. The only difference between the groups of mothers was a longer duration of labor among the treated mothers. The quality of infant nursing was equal between the 2 groups of infants on several measures; however, more infants in the treated group breastfed for less than 30 minutes at the first feeding.[7]
A national survey of women and their infants from late pregnancy through 12 months postpartum compared the time of lactogenesis II in mothers who did and did not receive pain medication during labor. Categories of medication were spinal or epidural only, spinal or epidural plus another medication, and other pain medication only. Women who received medications from any of the categories had about twice the risk of having delayed lactogenesis II (>72 hours) compared to women who received no labor pain medication.[8]
A nonrandomized convenience sample of women who did (n = 209) or did not (n = 157) receive epidural analgesia during labor was analyzed to determine whether epidurals affected the onset of lactation. Although not standardized, the typical procedure used sufentanil 10 to 15 mg together with either ropivacaine 0.1% or levobupivacaine 0.0625% epidurally, supplemented by epidural boluses of ropivacaine 0.1% or levobupivacaine 0.0625% about every 2 hours. No difference was found in the time of lactation onset between the two groups. Although women in both groups stated they wished to breastfeed prior to delivery, exclusive breastfeeding at 20 days postpartum was less frequent in the women who received an epidural (43%) than in women who did not (57%).[9]
A retrospective study in a Spanish public hospital compared the infants of mothers who received an epidural during labor that contained fentanyl and either bupivacaine or ropivacaine. Infants of mothers who received an epidural had a lower frequency of early breastfeeding.[10]
A study in China compared an epidural infusion of ropivacaine 700 mcg/hour (n = 76) to sufentanil 1.75 mcg/hour plus ropivacaine 700 mcg/hour (n = 81) during normal vaginal delivery. The combined ropivacaine and sufentanil provided better pain control than ropivacaine alone. Onset of lactation was shorter and lactation adequacy (milk volume) was better in the combined group than in the ropivacaine-only group.[11]
In a study of primiparous women with an uncomplicated pregnancy, some women received epidural analgesia with ropivacaine (dose not specified) and fentanyl in a median dose of 121 mcg (IQR 77 to 192 mcg), some received oxytocin alone and other received neither. Breastfeeding outcomes in the three groups were compared at 3 days, 1 month and 4 months postpartum. The study found no relationship between low-dose oxytocin use and breastfeeding success, but that epidermal analgesia lowered milk supply at 3 days and 1 month postpartum, and decreased rates of breastfeeding at 4 months postpartum.[2]
Alternate Drugs to Consider
References
- 1.
- French CA, Cong X, Chung KS. Labor epidural analgesia and breastfeeding: A systematic review. J Hum Lact 2016;32:507-20. [PubMed: 27121239]
- 2.
- Takahata K, Horiuchi S, Miyauchi A, et al. A longitudinal study of the association of epidural anesthesia and low-dose synthetic oxytocin regimens with breast milk supply and breastfeeding rates. Sci Rep 2023;13:21146. [PMC free article: PMC10689802] [PubMed: 38036700]
- 3.
- Heesen P, Halpern SH, Beilin Y, et al. Labor neuraxial analgesia and breastfeeding: An updated systematic review. J Clin Anesth 2021;68:110105. [PubMed: 33069970]
- 4.
- Matsota PK, Markantonis SL, Fousteri MZ, et al. Excretion of ropivacaine in breast milk during patient-controlled epidural analgesia after cesarean delivery. Reg Anesth Pain Med 2009;34:126-9. [PubMed: 19282712]
- 5.
- Chang ZM, Heaman MI. Epidural analgesia during labor and delivery: Effects on the initiation and continuation of effective breastfeeding. J Hum Lact 2005;21:305-14. [PubMed: 16113019]
- 6.
- Chen YM, Li Z, Wang AJ, Wang JM. Effect of labor analgesia with ropivacaine on the lactation of paturients. Zhonghua Fu Chan Ke Za Zhi 2008;43:502-5. [PubMed: 19080512]
- 7.
- Gizzo S, Di Gangi S, Saccardi C, et al. Epidural analgesia during labor: Impact on delivery outcome, neonatal well-being, and early breastfeeding. Breastfeed Med 2012;7:262-8. [PubMed: 22166068]
- 8.
- Lind JN, Perrine CG, Li R. Relationship between use of labor pain medications and delayed onset of lactation. J Hum Lact 2014;30:167-73. [PMC free article: PMC4684175] [PubMed: 24451212]
- 9.
- Mauri PA, Contini NN, Giliberti S, et al. Intrapartum epidural analgesia and onset of lactation: A prospective study in an Italian birth centre. Matern Child Health J 2015;19:511-8. [PubMed: 24894732]
- 10.
- Herrera-Gómez A, García-Martínez O, Ramos-Torrecillas J, et al. Retrospective study of the association between epidural analgesia during labour and complications for the newborn. Midwifery 2015;31:613-6. [PubMed: 25819707]
- 11.
- Wen X, Huang B, Liang X. Effect of ropivacaine and sufentanil in epidural labor analgesia. Am J Transl Res 2021;13:7001-7007. [PMC free article: PMC8290753] [PubMed: 34306455]
Substance Identification
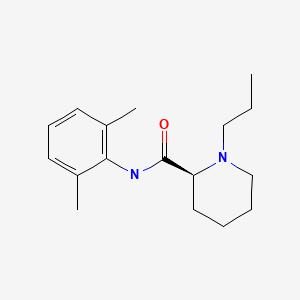
Substance Name
Ropivacaine
CAS Registry Number
84057-95-4
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Levobupivacaine.[Drugs and Lactation Database (...]Review Levobupivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Bupivacaine.[Drugs and Lactation Database (...]Review Bupivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Mepivacaine.[Drugs and Lactation Database (...]Review Mepivacaine.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Review Lidocaine.[Drugs and Lactation Database (...]Review Lidocaine.. Drugs and Lactation Database (LactMed®). 2006
- Ropivacaine - Drugs and Lactation Database (LactMed®)Ropivacaine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
