Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
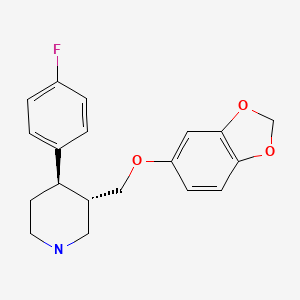
CASRN: 61869-08-7
Drug Levels and Effects
Summary of Use during Lactation
Because of the low levels of paroxetine in breastmilk, amounts ingested by the infant are small and paroxetine has not been detected in the serum of most infants tested. Occasional mild side effects have been reported, especially in the infants of mothers who took paroxetine during the third trimester of pregnancy, but the contribution of the drug in breastmilk is not clear. Most authoritative reviewers consider paroxetine one of the preferred antidepressants during breastfeeding.[1-7] Monitor breastfed infants for agitation, irritability, poor feeding and poor weight gain
Mothers taking an SSRI during pregnancy and postpartum may have more difficulty breastfeeding, although this might be a reflection of their disease state.[8] These mothers may need additional breastfeeding support. Breastfed infants exposed to an SSRI during the third trimester of pregnancy have a lower risk of poor neonatal adaptation than formula-fed infants.
Drug Levels
Maternal Levels. In a pooled analysis of serum levels from published studies and 3 unpublished cases, the authors found 50 mothers taking an average daily dosage of 21 mg (range 10 to 50 mg) had an average milk paroxetine level of 28 mcg/L (range 0 to 153 mcg/L).[1] Using the average dosage and milk level data from this paper, an exclusively breastfed infant would receive an estimated 1.2% of the maternal weight-adjusted dosage of paroxetine.
From data in 6 mothers taking paroxetine in an average daily dosage of 20 mg (range 10 to 30 mg), the authors estimated that an exclusively breastfed infant would receive 1.4% of the maternal weight-adjusted dosage.[9]
At 2 months postpartum, 19 mothers taking an average of 25 mg of paroxetine daily had average milk levels of 13.5 mcg/L at random times after the previous dose. The authors estimated that an exclusively breastfed infant would receive 0.02 mg/kg of paroxetine daily.[10]
A woman had taken paroxetine 15 mg daily during pregnancy. She did not receive a dose in the 22.75 hours before delivery or on the day of delivery. She resumed paroxetine 15 mg daily 24 hours postpartum. At 3.75 hours after the third postpartum dose, her breastmilk paroxetine level was 371 mcg/L.[11]
Four nursing mothers who were 6.5 to 18.5 weeks postpartum were taking paroxetine in doses of 12.5 to 60 mg daily in addition to quetiapine for major depression postpartum. Breastmilk samples that were obtained at various times after the dose had undetectable (<9.9 mcg/L) levels of paroxetine in 3 mothers. One mother who was taking 50 mg daily had a milk paroxetine level of 255 mcg/L.[12]
A woman taking paroxetine 20 mg daily had a breastmilk paroxetine concentration below the lower limit of quantification (<20 mcg/L) at a time that was not stated.[13]
A nursing mother was taking paroxetine 20 mg daily. Foremilk and hindmilk samples taken at 4 weeks postpartum, 7 hours after a dose contained 16 mcg/L and 24 mcg/L, respectively.[14]
Five women treated with paroxetine 7 to 25 mg daily during the third trimester of pregnancy and during breastfeeding provided trough milk samples during the first week postpartum. Paroxetine was undetectable (<5 mcg/L) in the milk of 2 women taking 10 mg daily. In the other 3 women, milk levels ranged from 5.9 to 32.9 mcg/L, with calculated weight-adjusted percentage of maternal dosages ranging from 1.1 to 3.2%. These values might be inaccurate because of the timing of milk sample collection.[15]
Nine mothers taking paroxetine in an average dosage of 29 mg daily (range 5 to 40 mg daily) provided milk samples for analysis. Samples of milk from the complete emptying of one breast were collected 3 times over a 2-day period in at predefined times between just before a dose and 14 hours after a dose, with each participant collecting samples at different times. The average milk concentration was 63 mcg/L resulting in an average infant daily dosage of 5 mcg/kg and a relative infant dosage of 2%.[16]
Infant Levels. Sixteen breastfed infants (2 about 50% breastfed; the others 95% or more breastfed) aged 6 to 13 weeks had undetectable (<1 mcg/L) paroxetine serum levels during maternal therapy with paroxetine in an average daily dosage of 18.75 mg (range 5 to 30 mg).[17]
In a pooled analysis of 40 mother-infant pairs from published and unpublished cases, the authors found that no infants had measurable paroxetine plasma levels.[1]
In 6 breastfed (extent not stated) infants aged 2 to 33 weeks whose mothers were taking paroxetine in an average daily dosage of 20 mg (range 10 to 30 mg), paroxetine was undetectable (<1.6 mcg/L) in all of the infants' serum. One mother taking 20 mg daily and her infant were both poor metabolizers (homozygous for CYP2D6*4), yet no paroxetine was detectable in infant serum.[9]
At 2 months postpartum, the breastfed infants of 19 mothers taking an average of 25 mg of paroxetine daily had an average serum paroxetine level of 0.95 mcg/L which was 5% of the maternal serum level.[10]
Nine breastfed (extent not stated) infants with an average age of 1.7 months (range 1.5 to 9.0 months) whose mothers were taking an average paroxetine dosage of 29 mg daily (range 5 to 40 mg daily) had one blood sample taken for analysis. Their average serum level of paroxetine was <6 mcg/L (range <6 to 6.4 mcg/L).[16]
Effects in Breastfed Infants
Agitation and difficulty feeding in one infant (age and other details not reported) that were possibly related to paroxetine in breastmilk were reported to the Australian Adverse Drug Reaction Advisory Committee.[18]
In a controlled cohort study of mothers who took paroxetine during pregnancy (diagnoses not reported), 36 mothers took paroxetine during the third trimester and breastfed their infants. Of these, 8 reported side effects in their infants including alertness (6), constipation (3), sleepiness (1), and irritability (1). There were no reports of side effects in the control group of mothers who breastfed and did not use paroxetine in the third trimester or during nursing. The relative contribution of transplacental and breastmilk acquisition of the drug could not be determined.[19]
In a study comparing the infants of mothers who took an SSRI during pregnancy for major depression with the infants of depressed mothers who did not take an SSRI, mental development and most motor development was normal at follow-up averaging 12.9 months in both groups. Four of the treated mothers took paroxetine in doses averaging 28.6 mg daily for an average of 7.8 months while breastfeeding (extent not stated) their infants. Psychomotor development was slightly delayed compared to controls, but the contribution of breastfeeding to abnormal development could not be determined.[20]
A prospective cohort study evaluated 27 infants whose mothers took paroxetine (diagnoses not reported) at an average dose of 20.7 mg daily for at least 2 weeks during breastfeeding (extent not stated). Two control groups consisted of two groups of mothers who neither breastfed nor took an SSRI. All but 7 of the 27 mothers took paroxetine during some part of pregnancy. Weight at 3 months was less in the paroxetine group, but multivariate analysis indicated that maternal paroxetine use was not the determining factor. Weights at 6 and 12 months were not different from the control groups and other developmental milestones were reached at the normal times. One of the paroxetine-exposed infants (age not stated) was reported by the mother to be irritable.[21]
Fifteen mothers who took an average paroxetine dosage of 20.4 mg daily for depression or anxiety starting no later than 4 weeks postpartum, breastfed their infants exclusively for 4 months and at least 50% during months 5 and 6. Their infants had 6-month weight gains that were normal according to national growth standards and mothers reported no abnormal effects in their infants.[22]
In 6 breastfed (extent not stated) infants aged 2 to 33 weeks whose mothers were taking paroxetine 10 to 30 mg daily, no adverse reactions were noted clinically at the time of the study.[9]
An infant born to a mother taking paroxetine had serum paroxetine levels about one-third that of the mother's at birth. The infant was a genetic poor metabolizer, which apparently was the cause of the high serum levels. Although the infant had symptoms attributed to paroxetine obtained in utero, the mother continued taking paroxetine 30 mg daily and breastfeeding (extent not stated). At 4 months of age, the infant had gained weight normally and had no evidence of neurological side effects.[23]
An 18-month-old infant with a 2-week history of vomiting was found to have hypokalemia, hypochloremic alkalosis and mild dehydration. The infant had been admitted twice previously 2 and 3 months before with a similar picture. Serum renin and aldosterone were normal. The infant's mother had been taking paroxetine 40 mg daily for about 1 year for depression and breastfeeding the infant (extent not stated). Paroxetine was detected, but not quantified, in the mother's breastmilk and infant's serum. Breastfeeding was discontinued and the infant was thriving 6 weeks later with a normal metabolic profile. The authors attributed the infant's metabolic abnormalities to paroxetine-induced syndrome of inappropriate secretion of antidiuretic hormone.[24] The reaction was possibly caused by paroxetine in breastmilk, but strong evidence was lacking and other possible causes cannot be ruled out.
A small study compared the reaction to pain in infants of depressed mothers who had taken an SSRI during pregnancy alone or during pregnancy and nursing, to a control group of unexposed infants of nondepressed mothers. Infants exposed to an SSRI either prenatally alone or prenatally and postnatally via breastmilk had blunted responses to pain compared to control infants. Nineteen of the 30 infants were exposed to paroxetine. Because there was no control group of depressed, nonmedicated mothers, an effect due to maternal behavior caused by depression could not be ruled out. The authors stressed that these findings did not warrant avoiding drug treatment of depression during pregnancy or avoiding breastfeeding during SSRI treatment.[10]
One study of side effects of SSRI antidepressants in nursing mothers found no adverse reactions that required medical attention among 3 infants whose mother was taking paroxetine. No specific information on maternal paroxetine dosage, extent of breastfeeding or infant age was reported.[25]
A nursing mother with bipolar disorder began taking 20 mg of paroxetine at 4 months postpartum and was then started on quetiapine 200 mg twice daily at 6 months postpartum. She breastfed regularly (extent not stated) and no obvious adverse effects were noted in the infant.[26]
Four nursing mothers who were 6.5 to 18.5 weeks postpartum were taking paroxetine in doses of 12.5 to 60 mg daily in addition to quetiapine for major depression postpartum. Their breastfed infants' development were tested at 9 to 18 months of age with the Bayley Scales. Measurements were slightly low on the mental and psychomotor development scale in one infant and on the mental development scale in another; both infants had undetectable (<9.9 mcg/L) serum paroxetine levels. All other infants had scores that were within normal limits. The authors concluded that the low scores of the two infants were probably not caused by the drugs received by the infants in breastmilk.[12]
An uncontrolled online survey compiled data on 930 mothers who nursed their infants while taking an antidepressant. Infant drug discontinuation symptoms (e.g., irritability, low body temperature, uncontrollable crying, eating and sleeping disorders) were reported in about 10% of infants. Mothers who took antidepressants only during breastfeeding were much less likely to notice symptoms of drug discontinuation in their infants than those who took the drug in pregnancy and lactation.[27]
A cohort of 247 infants exposed to an antidepressant in utero during the third trimester of pregnancy were assessed for poor neonatal adaptation (PNA). Of the 247 infants, 154 developed PNA. Infants who were exclusively given formula had about 3 times the risk of developing PNA as those who were exclusively or partially breastfed. Forty-nine of the infants were exposed to paroxetine in utero.[28]
A retrospective study of 42 nursing mothers who had been seen at a psychiatric outpatient facility, followed for at least 8 weeks, and prescribed paroxetine found that adverse effects were reported in 5 (12%) of their infants. One mother was taking 10 mg daily and 4 mothers were taking 20 mg daily. The most commonly reported adverse events in the infants were insomnia and restlessness; constant crying and poor feeding were less commonly reported. All of the adverse effects developed within the first 2 weeks after initiation of maternal treatment and disappeared within the 3 days after drug discontinuation. Adverse effects disappeared in one infant after reducing the maternal dosage from 20 mg daily to 10 mg daily. There was no difference in prevalence of adverse effects between these infants and those in the same study whose mothers were prescribed sertraline.[29]
A mother who was exclusively breastfeeding a 2-month-old infant began taking paroxetine 20 mg daily for depression. After paroxetine was begun, the mother reported severe constipation in the infant, which resolved within 2 days after discontinuing paroxetine with no treatment. No abnormalities were seen on physical examination or laboratory tests. The infant had previously developed agitation and sleeplessness with maternal sertraline use. The infant subsequently tolerated maternal citalopram use.[30]
Five women were treated with paroxetine 7 to 25 mg daily during the third trimester of pregnancy and during breastfeeding. Pediatric evaluations including neurologic assessments and brain ultrasound were conducted during the first 24 hours postpartum. Further follow-up was conducted at 6 or more months of age. Infant clinical status was comparable to unexposed infants from the same pediatric department.[15]
A case series reported 8 women who received paroxetine 20 mg and mirtazapine 15 mg daily for various psychiatric disorders. The women breastfed (extent not stated) their infants who averaged 4.3 weeks of age. Follow-up of the infants after 3 to 6 weeks when mirtazapine was discontinued identified one infant who experienced restlessness after 5 days of therapy according to the mother. Discontinuation of mirtazapine had no effect, but the symptoms disappeared when paroxetine was discontinued. No other infants had other adverse effects observed.[31]
Effects on Lactation and Breastmilk
Paroxetine can cause galactorrhea, usually with increased prolactin levels, in nonpregnant, nonnursing patients.[32-41] In a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, paroxetine was found to have a 3.1-fold increased risk of causing hyperprolactinemia compared to other drugs.[42] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
In a small prospective study, 8 primiparous women who were taking a serotonin reuptake inhibitor (SRI; 3 taking fluoxetine and 1 each taking citalopram, duloxetine, escitalopram, paroxetine or sertraline) were compared to 423 mothers who were not taking an SRI. Mothers taking an SRI had an onset of milk secretory activation (lactogenesis II) that was delayed by an average of 16.7 hours compared to controls (85.8 hours postpartum in the SRI-treated mothers and 69.1 h in the untreated mothers), which doubled the risk of delayed feeding behavior in the untreated group. However, the delay in lactogenesis II may not be clinically important, since there was no statistically significant difference between the groups in the percentage of mothers experiencing feeding difficulties after day 4 postpartum.[43]
A case control study compared the rate of predominant breastfeeding at 2 weeks postpartum in mothers who took an SSRI antidepressant throughout pregnancy and at delivery (n = 167) or an SSRI during pregnancy only (n = 117) to a control group of mothers who took no antidepressants (n = 182). Among the two groups who had taken an SSRI, 33 took citalopram, 18 took escitalopram, 63 took fluoxetine, 2 took fluvoxamine, 78 took paroxetine, and 87 took sertraline. Among the women who took an SSRI, the breastfeeding rate at 2 weeks postpartum was 27% to 33% lower than mother who did not take antidepressants, with no statistical difference in breastfeeding rates between the SSRI-exposed groups.[44]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[45] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575; paroxetine n = 53) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[46]
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[47]
Alternate Drugs to Consider
References
- 1.
- Weissman AM, Levy BT, Hartz AJ, et al. Pooled analysis of antidepressant levels in lactating mothers, breast milk, and nursing infants. Am J Psychiatry 2004;161:1066-78. [PubMed: 15169695]
- 2.
- The Academy of Breastfeeding Medicine Protocol Committee. ABM clinical protocol #18: Use of antidepressants in nursing mothers. Breastfeed Med 2008;3:44-52. [PubMed: 18333769]
- 3.
- Lanza di Scalea T, Wisner KL. Antidepressant medication use during breastfeeding. Clin Obstet Gynecol 2009;52:483-97. [PMC free article: PMC2902256] [PubMed: 19661763]
- 4.
- Berle JO, Spigset O. Antidepressant use during breastfeeding. Curr Womens Health Rev 2011;7:28-34. [PMC free article: PMC3267169] [PubMed: 22299006]
- 5.
- Orsolini L, Bellantuono C. Serotonin reuptake inhibitors and breastfeeding: A systematic review. Hum Psychopharmacol 2015;30:4-20. [PubMed: 25572308]
- 6.
- Larsen ER, Damkier P, Pedersen LH, et al. Use of psychotropic drugs during pregnancy and breast-feeding. Acta Psychiatr Scand Suppl 2015;445:1-28. [PubMed: 26344706]
- 7.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther 2021;28:e118-e126. [PubMed: 30601177]
- 8.
- Grzeskowiak LE, Leggett C, Costi L, et al. Impact of serotonin reuptake inhibitor use on breast milk supply in mothers of preterm infants: A retrospective cohort study. Br J Clin Pharmacol 2018;84:1373-9. [PMC free article: PMC5980248] [PubMed: 29522259]
- 9.
- Berle JØ, Steen VM, Aamo TO, et al. Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: Infant exposure, clinical symptoms, and cytochrome P450 genotypes. J Clin Psychiatry 2004;65:1228-34. [PubMed: 15367050]
- 10.
- Oberlander TF, Grunau RE, Fitzgerald C, et al. Pain reactivity in 2-month-old infants after prenatal and postnatal serotonin reuptake inhibitor medication exposure. Pediatrics 2005;115:411-25. [PubMed: 15687451]
- 11.
- Knoppert DC, Nimkar R, Principi T, et al. Paroxetine toxicity in a newborn after in utero exposure: clinical symptoms correlate with serum levels. Ther Drug Monit 2006;28:5-7. [PubMed: 16418684]
- 12.
- Misri S, Corral M, Wardrop AA, et al. Quetiapine augmentation in lactation: A series of case reports. J Clin Psychopharmacol 2006;26:508-11. [PubMed: 16974194]
- 13.
- Salazar FR, D'Avila FB, de Oliveira MH, et al. Development and validation of a bioanalytical method for five antidepressants in human milk by LC-MS. J Pharm Biomed Anal 2016;129:502-8. [PubMed: 27497651]
- 14.
- Weisskopf E, Panchaud A, Nguyen KA, et al. Simultaneous determination of selective serotonin reuptake inhibitors and their main metabolites in human breast milk by liquid chromatography-electrospray mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 2017;1057:101-9. [PubMed: 28511118]
- 15.
- Pogliani L, Baldelli S, Cattaneo D, et al. Selective serotonin reuptake inhibitors passage into human milk of lactating women. J Matern Fetal Neonatal Med 2019;32:3020-5. [PubMed: 29557689]
- 16.
- Den Besten-Bertholee D, Touw DJ, Damer EA, et al. Sertraline, citalopram and paroxetine in lactation: passage into breastmilk and infant exposure. Front Pharmacol 2024;15:1414677. [PMC free article: PMC11150716] [PubMed: 38841362]
- 17.
- Hendrick V, Fukuchi A, Altshuler L, et al. Use of sertraline, paroxetine and fluvoxamine by nursing women. Br J Psychiatry 2001;179:163-6. [PubMed: 11483479]
- 18.
- Rohan A. Drug distribution in human milk. Aust Prescr 1997;20:84.
- 19.
- Costei AM, Kozer E, Ho T, et al. Perinatal outcome following third trimester exposure to paroxetine. Arch Pediatr Adolesc Med 2002;156:1129-32. [PubMed: 12413342]
- 20.
- Casper RC, Fleisher BE, Lee-Ancajas JC, et al. Follow-up of children of depressed mothers exposed or not exposed to antidepressant drugs during pregnancy. J Pediatr 2003;142:402-8. [PubMed: 12712058]
- 21.
- Merlob P, Stahl B, Sulkes J. Paroxetine during breast-feeding: Infant weight gain and maternal adherence to counsel. Eur J Pediatr 2004;163:135-9. [PubMed: 14745552]
- 22.
- Hendrick V, Smith LM, Hwang S, et al. Weight gain in breastfed infants of mothers taking antidepressant medications. J Clin Psychiatry 2003;64:410-2. [PubMed: 12716242]
- 23.
- Laine K, Kytola J, Bertilsson L. Severe adverse effects in a newborn with two defective CYP2D6 alleles after exposure to paroxetine during late pregnancy. Ther Drug Monit 2004;26:685-7. [PubMed: 15570195]
- 24.
- Abdul Aziz A, Agab WA, Kalis NN. Severe paroxetine induced hyponatremia in a breast fed infant. J Bahrain Med Soc 2004;16:195-8.
- 25.
- Lee A, Woo J, Ito S. Frequency of infant adverse events that are associated with citalopram use during breast-feeding. Am J Obstet Gynecol 2004;190:218-21. [PubMed: 14749663]
- 26.
- Ritz S. Quetiapine monotherapy in post-partum onset bipolar disorder with a mixed affective state. Eur Neuropsychopharmacol 2005;15 (Suppl 3):S407. doi:10.1016/S0924-977X(05)80825-9 [CrossRef]
- 27.
- Hale TW, Kendall-Tackett K, Cong Z, et al. Discontinuation syndrome in newborns whose mothers took antidepressants while pregnant or breastfeeding. Breastfeed Med 2010;5:283-8. [PubMed: 20807106]
- 28.
- Kieviet N, Hoppenbrouwers C, Dolman KM, et al. Risk factors for poor neonatal adaptation after exposure to antidepressants in utero. Acta Paediatr 2015;104:384-91. [PubMed: 25559357]
- 29.
- Uguz F, Arpaci N. Short-term safety of paroxetine and sertraline in breastfed infants: A retrospective cohort study from a university hospital. Breastfeed Med 2016;11:487-9. [PubMed: 27575664]
- 30.
- Uguz F. Better tolerance of citalopram in a breastfed infant who could not tolerate sertraline and paroxetine. Breastfeed Med 2018;13:89-90. [PubMed: 29185803]
- 31.
- Uguz F. Short-term safety of paroxetine plus low-dose mirtazapine during lactation. Breastfeed Med 2019;14:131-2. [PubMed: 30489153]
- 32.
- Davenport E, Velamoor R. A case of paroxetine-induced galactorrhea. Can J Psychiatry 2002;47:890-1. [PubMed: 12500767]
- 33.
- Morrison J, Remick RA, Leung M, et al. Galactorrhea induced by paroxetine. Can J Psychiatry 2001;46:88-9. [PubMed: 11221498]
- 34.
- Bonin B, Vandel P, Sechter D, et al. Paroxetine and galactorrhea. Pharmacopsychiatry 1997;30:133-4. [PubMed: 9271780]
- 35.
- González E, Minguez L, Sanguino RM. Galactorrhea after paroxetine treatment. Pharmacopsychiatry 2000;33:118. [PubMed: 10855465]
- 36.
- Egberts AC, Meyboom RH, De Koning FH, et al. Non-puerperal lactation associated with antidepressant drug use. Br J Clin Pharmacol 1997;44:277-81. [PMC free article: PMC2042834] [PubMed: 9296322]
- 37.
- Chakraborty S, Sanyal D, Bhattacharyya R, et al. A case of paroxetine-induced galactorrhoea with normal serum prolactin level. Indian J Pharmacol 2010;42:322-3. [PMC free article: PMC2959219] [PubMed: 21206628]
- 38.
- Sertcelik S, Bakim B, Karamustafalioglu O. High dose paroxetine-induced galactorrhea with normal serum prolactin level: A case report. Bull Clin Psychopharmacol 2012;22:355-6. doi:10.5455/bcp.20120812015108 [CrossRef]
- 39.
- Kumar PNS, Gopalakrishnan A. Paroxetine induced galactorrhoea - A case report. Asian J Psychiatr 2018;34:31-2. [PubMed: 29631147]
- 40.
- Mishra S, Nath S, Mishra BR, et al. Euprolactinemic galactorrhea with paroxetine: Exploring the missing link. Indian J Psychol Med 2019;41:395-7. [PMC free article: PMC6657480] [PubMed: 31391677]
- 41.
- Bhattacharjee S, Biswas R, Mandal N. Selective serotonin reuptake inhibitor-induced galactorrhea with hyperprolactinemia. Indian J Psychiatry 2021;63:613-6. [PMC free article: PMC8793705] [PubMed: 35136264]
- 42.
- Trenque T, Herlem E, Auriche P, et al. Serotonin reuptake inhibitors and hyperprolactinaemia: A case/non-case study in the French pharmacovigilance database. Drug Saf 2011;34:1161-6. [PubMed: 22077504]
- 43.
- Marshall AM, Nommsen-Rivers LA, Hernandez LL, et al. Serotonin transport and metabolism in the mammary gland modulates secretory activation and involution. J Clin Endocrinol Metab 2010;95:837-46. [PMC free article: PMC2840848] [PubMed: 19965920]
- 44.
- Gorman JR, Kao K, Chambers CD. Breastfeeding among women exposed to antidepressants during pregnancy. J Hum Lact 2012;28:181-8. [PubMed: 22344850]
- 45.
- Venkatesh KK, Castro VM, Perlis RH, et al. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol 2017;37:1003-9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 46.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact 2017;33:701-9. [PubMed: 28984528]
- 47.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand 2022;101:344-54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
Paroxetine
CAS Registry Number
61869-08-7
Drug Class
Breast Feeding
Lactation
Milk, Human
Antidepressive Agents
Serotonin Uptake Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Citalopram.[Drugs and Lactation Database (...]Review Citalopram.. Drugs and Lactation Database (LactMed®). 2006
- Pharmacologic factors associated with transient neonatal symptoms following prenatal psychotropic medication exposure.[J Clin Psychiatry. 2004]Pharmacologic factors associated with transient neonatal symptoms following prenatal psychotropic medication exposure.Oberlander TF, Misri S, Fitzgerald CE, Kostaras X, Rurak D, Riggs W. J Clin Psychiatry. 2004 Feb; 65(2):230-7.
- Sertraline, citalopram and paroxetine in lactation: passage into breastmilk and infant exposure.[Front Pharmacol. 2024]Sertraline, citalopram and paroxetine in lactation: passage into breastmilk and infant exposure.Den Besten-Bertholee D, Touw DJ, Damer EA, Mian P, Ter Horst PGJ. Front Pharmacol. 2024; 15:1414677. Epub 2024 May 22.
- Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: infant exposure, clinical symptoms, and cytochrome p450 genotypes.[J Clin Psychiatry. 2004]Breastfeeding during maternal antidepressant treatment with serotonin reuptake inhibitors: infant exposure, clinical symptoms, and cytochrome p450 genotypes.Berle JØ, Steen VM, Aamo TO, Breilid H, Zahlsen K, Spigset O. J Clin Psychiatry. 2004 Sep; 65(9):1228-34.
- Review Desvenlafaxine.[Drugs and Lactation Database (...]Review Desvenlafaxine.. Drugs and Lactation Database (LactMed®). 2006
- Paroxetine - Drugs and Lactation Database (LactMed®)Paroxetine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
