NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-.
Introduction
Anyone who has already had chickenpox can develop shingles later on. Both are caused by the same virus, known as the varicella-zoster virus. This virus stays dormant (inactive) in the body after a chickenpox infection. But it can become active again years later and cause shingles (herpes zoster): a rash with blisters. The rash usually forms a band across the skin and is often very painful. It normally only affects one side of the body.
Shingles is particularly common in older people. Although it can be very unpleasant, it’s usually over in about two to four weeks if there are no complications.
In Germany, a shingles vaccination is recommended for people over the age of 60 (since 2018). People who have a weakened immune system or a chronic disease are advised to have the vaccination from the age of 50.
Shingles is contagious, but only for people who have never had chickenpox. In that case the infection only causes chickenpox at first, and not shingles.
At a glance
- Shingles causes a rash that typically forms a band across the skin (often on the torso) and can be very painful.
- It is most common in people over the age of 50.
- The disease is caused by varicella-zoster viruses that have stayed in the body after a chickenpox infection in the past.
- The symptoms usually go away after two to four weeks.
- A shingles vaccination is recommended from the age of 60 – or from the age of 50 in people who have a weakened immune system or certain chronic diseases.
Symptoms
Before the rash breaks out you usually feel tired and run-down. You may also have a slight fever and tingling sensations under your skin. The typical symptoms of shingles start two or three days later:
- moderate to severe stinging or burning pain in the affected area,
- followed by slightly reddish patches of skin with small bumps,
- which then turn into small blisters that may be itchy in just a few hours.
This stage can last up to five days. After that, the blisters dry up in two to ten days, leaving behind yellowish scabs.
The shingles rash generally affects only one side of the body, and typically forms a band across the skin.

Shingles: Typical rash on one side of the body only
Shingles most commonly affects the torso or chest. But it can develop just about anywhere, including your arms, head or face. Sometimes it can also affect your eyes or ears. Blisters may develop over larger areas in some people.
Causes
After a chickenpox infection clears up, the varicella-zoster viruses settle undetected in the nerve roots along the spinal cord or at the base of the skull. They remain there for the rest of your life, but usually go unnoticed.
If the immune system is weakened – for instance, as a result of a cold, extreme stress or older age – the viruses may multiply again and move along the affected nerve, eventually reaching the skin. When the viruses multiply in skin cells, they cause inflammation and the typical shingles rash. The inflammation in the nerve is what causes the pain.
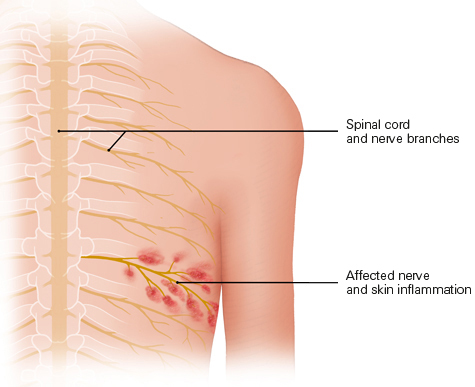
Nerve infected by the virus, and inflamed area of skin
People who have never had chickenpox can be infected with the varicella-zoster virus if they come into contact with the fluid from inside shingles blisters. The infection can then only cause chickenpox at first, and not shingles. You are no longer contagious once all of the blisters have dried up and all of the scabs have fallen off.
People who have been vaccinated against chickenpox can still get shingles – but it seems to be less common than in people who have had chickenpox.
Prevalence
It is estimated that about 2 out of 10 people who have had chickenpox develop shingles sometime later in life. Most people who get shingles are over 50. The risk of shingles increases with age because our immune systems become weaker as we grow older. About 300,000 people get shingles in Germany every year.
Outlook
In normal cases, without complications, shingles usually goes away after two to four weeks in adults. Children and young people generally have milder cases. Most adults only get shingles once in their life.
In very rare cases, the blisters spread to nearby areas of skin or even over the whole body. This may happen if the immune system is very weak, for instance due to a serious disease like cancer or AIDS. Under those circumstances, shingles can be life-threatening.
Effects
Breaking the itchy blisters open by scratching them may lead to a bacterial infection in the skin and leave scars. Other longer-term effects of shingles include overly sensitive skin or changes in skin pigmentation – leaving it darker or lighter than the surrounding skin.
Shingles in the face can spread to the eye too, causing inflammation of the cornea (keratitis). If auditory (hearing) nerves or facial nerves are involved, shingles may also lead to hearing loss or paralysis in the face. This usually goes away once the shingles infection has cleared up.
About 10 to 20 out of 100 people still have quite severe pain from nerve damage even after the rash has gone away. This pain is called "post-herpetic neuralgia." It can last anywhere from a few weeks or months up to several years.
People with a very weak immune system are at greater risk of developing serious complications. The possible complications include a lung infection (pneumonia), inflammation of the membranes covering the brain and spinal cord (meningitis) or a liver inflammation (hepatitis).
Unlike chickenpox, shingles is not dangerous for unborn children during pregnancy.
Diagnosis
Shingles can also be difficult to diagnose in the early stages because the typical rash often only appears after the pain starts. Depending on what part of your body is affected, other causes might be suspected at first, like an inflammation of the appendix (appendicitis) or an inflammation of the gallbladder (cholecystitis), a slipped disk or even a heart attack.
Many people who have shingles first think that it might be a non-contagious skin condition like eczema. This may delay the diagnosis because they might think that they don’t need to see a doctor about it.
Doctors diagnose shingles based on its typical one-sided rash and the accompanying pain or abnormal sensations. If they aren’t sure whether it’s shingles, the fluid inside the blisters can be tested to see whether it contains the virus. Doctors can also test the blood for antibodies that fight the varicella-zoster virus.
Prevention
As of late 2018, the German Standing Committee on Vaccination (STIKO) recommends that everyone over the age of 60 be vaccinated against shingles with an inactivated herpes zoster vaccine. This inactivated vaccine contains certain parts of the virus instead of weakened viruses. It is already recommended for people aged 50 and over who have chronic diseases such as diabetes, rheumatoid arthritis or a weakened immune system. It consists of two doses, given two to six months apart.
Studies show that the vaccine can significantly lower the risk of healthy people getting shingles. But it’s hard to say whether the protection against shingles lasts longer than four years because the inactivated vaccine is quite new. The vaccination may cause side effects, including reddened skin and rashes, and pain or swelling where the vaccine was injected. These are signs that the body is dealing with the vaccine in a normal way.
In Germany, the costs of this vaccination are covered by statutory health insurers.
Treatment
Symptoms like pain and fever can be relieved with pain-relieving and fever-lowering medication such as acetaminophen (paracetamol). Prescription painkillers like opioids are sometimes used to relieve more severe pain.
Thorough skin care is recommended if you have shingles. Antiseptic or anti-itch lotions, gels and powders are often used to relieve the itching and dry out the blisters. Most of them contain tanins, zinc, menthol or polidocanol. If blisters have already formed, people are sometimes advised to use cooling wet wraps. But there’s no good scientific research on how well these treatments work in shingles.
Special medications for the herpes zoster virus (antiviral drugs) are especially recommended if
- you are over the age of 50,
- the shingles affects your head and neck region,
- you have a weakened immune system,
- you have kidney failure,
- the symptoms are severe,
- or there is a higher risk of complications.
If antiviral medication is taken early on, it can make shingles go away faster and decrease the time that it is painful. So it makes sense to start antiviral therapy no later than 72 hours after the rash appears. In severe cases the medicine can also be given through a drip into a vein (intravenous infusion). If the ear is affected, steroids are often used too. But it still isn’t clear what pros and cons this kind of combination therapy may have.
Everyday life
Box
The blisters should not be scratched open, if possible: The fluid in them is contagious, and blisters that have been torn open can leave scars.
As long as it's still contagious – that is, until the very last blisters have gone away – people who have shingles should avoid direct contact with others if they don't know whether the other people are immune to chickenpox. This is particularly important when it comes to people with a weakened immune system and pregnant women. You can help to stop shingles from spreading by covering the blisters with a bandage.
Further information
When people are ill or need medical advice, they usually go to see their family doctor first. In our "Health care in Germany" topic you can read about how to find the right doctor – and our list of questions can help you to prepare for your appointment.
Sources
- Chen N, Li Q, Yang J et al. Antiviral treatment for preventing postherpetic neuralgia. Cochrane Database Syst Rev 2014; (2): CD006866. [PMC free article: PMC10583132] [PubMed: 24500927]
- Deutsche Dermatologische Gesellschaft (DDG). Diagnostik und Therapie des Zoster und der Postzosterneuralgie (S2k-Leitlinie). AWMF-Registernr.: 013-023. 2019.
- Gagliardi AM, Andriolo BN, Torloni MR et al. Vaccines for preventing herpes zoster in older adults. Cochrane Database Syst Rev 2019; 2019(11). [PMC free article: PMC6836378] [PubMed: 31696946]
- Han Y, Zhang J, Chen N et al. Corticosteroids for preventing postherpetic neuralgia. Cochrane Database Syst Rev 2013; (3): CD005582. [PubMed: 23543541]
- McDonald EM, de Kock J, Ram FS. Antivirals for management of herpes zoster including ophthalmicus: a systematic review of high-quality randomized controlled trials. Antivir Ther 2012; 17(2): 255-264. [PubMed: 22300753]
- Robert Koch-Institut (RKI). Empfehlungen der Ständigen Impfkommission (STIKO) beim Robert Koch-Institut 2022 (Epidemiologisches Bulletin 04/2022). 2022.
- Robert Koch-Institut (RKI). Gürtelrose (Herpes zoster): Antworten auf häufig gestellte Fragen zu Erkrankung und Impfung. 2022.
- Robert Koch-Institut (RKI). RKI-Ratgeber: Windpocken (Varizellen), Gürtelrose (Herpes zoster). 2019.
- Ständige Impfkommission (STIKO). Wissenschaftliche Begründung für die Entscheidung, die Herpeszoster-Lebendimpfung nicht als Standardimpfung zu empfehlen. 2017.
- Ständige Impfkommission (STIKO). Wissenschaftliche Begründung zur Empfehlung einer Impfung mit dem Herpes zoster-subunit-Totimpfstoff. 2018.
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.
- Overview: Shingles - InformedHealth.orgOverview: Shingles - InformedHealth.org
Your browsing activity is empty.
Activity recording is turned off.
See more...
