NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-.
Introduction
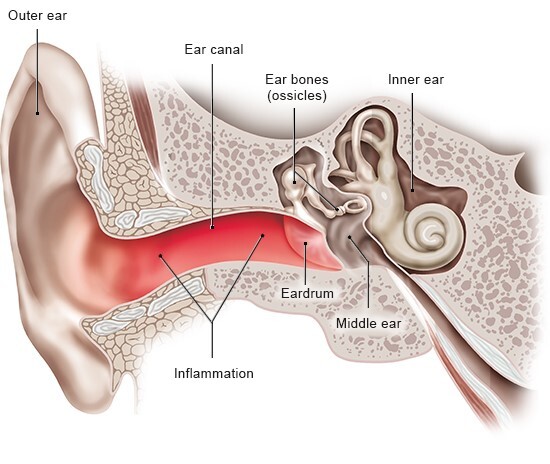
Outer ear infections typically lead to redness and swelling in the ear. They are among the most common causes of earache. In many cases they are caused by bacteria. But fungi, viruses or allergies are sometimes to blame too.
The outer ear includes the part of the ear you can see (the auricle) and the outer ear canal. The outer ear canal leads from the eardrum to the auricle. The medical term for inflammations of the outer ear is “otitis externa.” They are usually caused by infections.
At a glance
- Outer ear infections often lead to severe earache.
- They are caused by bacteria or other germs that get into the ear, for example when we go swimming.
- The infection – sometimes called "swimmer's ear” – usually goes away on its own after a few days or weeks.
- Until that happens, you can use painkillers and antibacterial ear drops to relieve the symptoms.
Outer ear infection
Symptoms
Outer ear infections are often very painful– especially when you touch or tug on your earlobe. Itching is common too.
The skin in the ear canal is red and swollen, and sometimes also sheds skin flakes or oozes a liquid. The ear might then become blocked, making it difficult to hear properly.
In about 1 out of 3 people the symptoms are so severe that it affects their everyday lives. About 1 out of 5 people have to stay home from work or school for a few days because of the infection.
Causes and risk factors
Outer ear infections are usually caused by bacteria. They are sometimes caused by a fungus, such as a yeast, but that’s less common. Viral illnesses like the flu or a certain type of shingles affecting the ear (Zoster oticus) may also lead to an outer ear infection. And sometimes allergic reactions – for instance, to a shampoo – are to blame.
Outer ear infections are also often called “swimmer's ear” because germs can easily get into the ear canal while you're swimming. This means that people who swim a lot are more likely to get outer ear infections.
Minor injuries to the ear – for instance, through the use of cotton ear buds to clean your ear, or regularly wearing headphones that you stick inside your ear (“in-ear headphones”) – can increase the risk too. People who have already had an outer ear infection or are generally prone to infections are also more likely to get outer ear infections.
Prevalence and outlook
Outer ear infections are especially common in adults: About 1 out of 10 people will have one at some point in their life.
The infection is usually mild and clears up on its own after a few days or weeks. But it sometimes lasts longer. In rare cases it may spread to nearby tissue.
Prevention
In order to prevent outer ear infections, it's important not to irritate or damage the ear canal. Pointed objects should never be inserted into the ear canal.
But simply trying to clean your ears with cotton ear buds can cause damage to the ear canal too. There's no need to use cotton ear buds anyway because your ears clean themselves by producing earwax. When the earwax comes out of your ears, you can remove it (and the dirt inside it) with a tissue. If larger amounts build up or a hard “plug” develops, the earwax can be softened, for instance with olive oil, allowing it to leave the ear more easily.
It is important to take care, though. If you are unsure, it might be better to get a doctor to flush out your ear and suck out the built-up earwax or carefully remove it with a thin, hook-like instrument.
The following things can also help to prevent outer ear infections:
- A snug-fitting swimming cap helps to keep water from entering the ear while swimming, showering or having a bath.
- People who use earplugs while swimming should make sure that they are soft and fit properly.
- If water does get into your ear, you usually just need to tilt your head to the side to let the water flow out. Gently pulling your earlobe and jumping up and down a little can help. You can also carefully dry your ear using a hairdryer at a low setting.
- If you often have problems with earwax buildup, it's a good idea to have your ear cleaned by a doctor before going on any trips where you might do a lot of swimming.
- If you have sensitive ear canals, don't use earplugs to protect your ears from noise, dust or water too often. That's also true for the use of in-ear headphones when you listen to music or make phone calls. It might be better to try different headphones if you're prone to outer ear infections.
If you've noticed that certain shampoos, soaps or other cosmetic products lead to ear infections, it's best to try out other products instead.
Treatment
The medications that are commonly used to treat outer ear infections include painkillers and disinfectant ear drops or sprays. These are available from pharmacies without a prescription. Acute outer ear infections that are caused by bacteria are often treated using special ear drops that have to be prescribed by a doctor. If the symptoms don't improve within a few days, it's advisable to see a doctor.
If the infection is severe or lasts for several weeks, your doctor might clean your ear and place a little sponge or a strip of gauze soaked in ear drop fluid into your ear canal. Sometimes other kinds of medication are needed too – for instance, if the ear infection was caused by shingles.
Further information
When people are ill or need medical advice, they usually go to see their family doctor first. You can read about how to find the right doctor in our topic "Health care in Germany" – and our list of questions can help you to prepare for your appointment.
Sources
- Burton MJ, Singer M, Rosenfeld RM. Extracts from The Cochrane Library: Interventions for acute otitis externa. Otolaryngol Head Neck Surg 2010; 143(1): 8-11. [PubMed: 20620612]
- Deutsche Gesellschaft für Allgemeinmedizin und Familienmedizin (DEGAM). Ohrenschmerzen (S2k-Leitlinie, in Überarbeitung). AWMF-Registernr.: 053-009. 2019.
- Hajioff D, MacKeith S. Otitis externa. BMJ Clin Evid 2015: pii: 0510. [PMC free article: PMC4466798] [PubMed: 26074134]
- Kaushik V, Malik T, Saeed SR. Interventions for acute otitis externa. Cochrane Database Syst Rev 2010; (1): CD004740. [PubMed: 20091565]
- Lenarz T, Boenninghaus HG. Hals-Nasen-Ohren-Heilkunde. Berlin: Springer; 2012.
- Wiegand S, Berner R, Schneider A et al. Otitis Externa: Diagnostik und evidenzbasierte Therapie. Dtsch Arztebl Int 2019; 116(13): 224-234. [PMC free article: PMC6522672] [PubMed: 31064650]
IQWiG health information is written with the aim of helping people understand the advantages and disadvantages of the main treatment options and health care services.
Because IQWiG is a German institute, some of the information provided here is specific to the German health care system. The suitability of any of the described options in an individual case can be determined by talking to a doctor. informedhealth.org can provide support for talks with doctors and other medical professionals, but cannot replace them. We do not offer individual consultations.
Our information is based on the results of good-quality studies. It is written by a team of health care professionals, scientists and editors, and reviewed by external experts. You can find a detailed description of how our health information is produced and updated in our methods.