Alcohol: Social damages, abuse, and dependence
Authors
INSERM Collective Expertise Centre.This document presents the summary and recommendations of the group of experts assembled by Inserm as part of the collective expertise procedure in response to the questions raised by the Mission interministérielle de lutte contre la drogue et la toxicomanie (MILDT; the interministerial anti-drug and drug-addiction mission), the Caisse nationale d'assurance maladie des travailleurs salariés (CNAMTS; the national sickness insurance scheme for salaried employees), and the Institut national de prévention et d'éducation pour la santé (INPRES; national institute for prevention and health education (an example is CFES, Comité français d'éducation pour la santé French health education committee)) on consumption habits, social damage, and alcohol abuse and dependency.
The Centre d'expertise collective de l'Inserm (Inserm collective expertise centre) has coordinated this collective expertise strategy with the Département animation et partenariat scientifique (DAPS; leadership and scientific partnership department) for dossier compilation in conjunction with the service of documentation from the Département de l'information scientifique et de la communication (DISC; documentation sector of the scientific information and communication department) as regards the bibliographical research.
Foreword
Alcohol consumption has regularly decreased in recent decades both in France and in Europe as a whole. France nevertheless continues to lead the European states in terms of premature, alcohol-related male deaths. Alcohol abuse is still a major public health problem in France.
Despite a certain harmonisation in Western countries, drinking habits are still firmly steeped in local culture. The type of drinks (wine, beer, spirits) and consumption habits (daily, occasional, massive intake and drunkenness) vary according to age, sex, and social and cultural environment. The hazards are not the same: accidents, impulsive, risky behaviour, violence and trauma associated with drunkenness; cancer, cirrhosis, cardiovascular complications, neurological disorders and dependency associated with excessive chronic alcohol intake. Five million French people currently have first-hand experience with the medical problems and psychological or social difficulties associated with alcohol abuse.
The steps taken to solve this problem still appear inadequate. Despite the Évin Law of 1991, exceptions to the advertising ban on alcoholic drinks have multiplied. Preventive and anti-drunk-driving campaigns have had little impact to date. Inadequately trained, general practitioners rarely broach the subject of alcohol consumption with their patients and rarely apply screening procedures. Despite the well-publicised desire to make combating the harmful effects of alcohol a public health priority, there is still an obvious lack of resources for both the prevention and management of this problem.
The Mission interministérielle de lutte contre la drogue et la toxicomanie (MILDT), the Caisse nationale d'assurance maladie des travailleurs salariés (CNAMTS), and the Institut national de prévention et d'éducation pour la santé (INPES; for example CFES, Comité français d'éducation pour la santé), who are the key players in public policies for the prevention and management of alcohol-related problems, wanted to question Inserm via the collective expertise procedure. This expertise, which continues an initial approach dealing more specifically with the effects of alcohol on health, will provide validated scientific information relating to alcohol-related consumption habits and how these have changed over time, the social damages associated with excessive consumption, the risk factors for abuse and dependency, and the related management problems.
To carry out this second expert appraisal of alcohol, Inserm has set up a multidisciplinary group of experts in the fields of epidemiology, human and social sciences, road safety, psychiatry, and biology. The expert group focused on the following questions:
- What information is available with regard to changes in alcohol consumption over the last 20 years in France and throughout the world? What main trends can be identified in France?
- What information is available regarding the social usage of alcohol (in professional situations as well as in social gatherings with family and friends, etc.)? What is known about the phenomenon of multiple consumption?
- What information is available relating to the social damages associated with excessive alcohol consumption in terms of accidents (accidents at work, road-traffic accidents, domestic), violence, delinquency, and marginalisation?
- What information is available regarding steps to prevent alcohol-related behaviour and what is the outcome of such an approach, especially in adolescents and young adults?
- What information is available regarding the prevalence of alcohol abuse and dependency? What tools are available to identify patients with alcohol-related problems?
- What are the underlying mechanisms involved in alcohol dependency? What is known about the interaction of these mechanisms with risk or protection factors (individual susceptibility, environmental factors)?
- What is the stance of the health authorities in relation to alcohol-dependent diseases? How can the efficacy of the management strategies be assessed?
Over 2,000 articles were selected after searching international databases. During the eight working sessions organised between September 2001 and July 2002, experts presented a critical analysis and a summary of published international and national studies on the various aspects of the expertise specification. The last three sessions were devoted to drawing up the main facts and recommendations. Several papers at the end of this investigation will supplement the expert analysis with French data.
Expert advisory group and authors
Group of experts and authors
Philippe ARVERS, Centre de recherche du service de santé des armées, La Tronche, France (research centre of the army medical corps.)
Jean-Pascal ASSAILLY, Institut national de recherche sur les transports et leur sécurité, Arcueil, France (national institute for research into methods of transport and their safety)
Philippe BATEL, Unité de traitement ambulatoire des maladies addictives, Hôpital Beaujon, Clichy, France (outpatient department for addictive diseases, Beaujon Hospital)
Marie CHOQUET, Epidemiology and Biostatistics, Inserm U 472, Villejuif, France
Thierry DANEL, Service d'addictologie, Centre hospitalier régional universitaire de Lille, Lille France (department of addictology, regional university medical centre)
Martine DAOUST, Unité de recherche sur les adaptations physiologiques et comportementales, Université de Picardie, Amiens, France (research unit, physiological and behavioural adaptation, University of Picardy)
Philippe DE WITTE, Biologie du comportement, Université catholique de Louvain, Louvain-La-Neuve, Belgium (behavioural biology, Louvain Catholic University)
Françoise FACY, Epidemiology of addictive behaviour, Inserm XR 302, Le Vésinet, France
Jean-Dominique FAVRE, Psychiatry Department, Hôpital d'instruction des armées
Percy CLAMART, President of the French Alcohology Society
Eric HISPARD, Department of Internal Medicine, Hôpital Fernand-Widal, Paris, France
Thérèse LEBRUN, Centre de recherches économiques, sociologiques et de gestion (CRESGELABORES), Université catholique de Lille, Lille, France (economic, sociological, and management research centre, Lille Catholic University)
Anne-Marie LEHR-DRYLEWICZ, General Practitioner, Parçay-Meslay, France
Michel LEJOYEUX, Psychiatry Department, Hôpital Louis-Mourier, Colombes, France
Pierre MORMÈDE, Laboratoire de neurogénétique et stress, Unité mixte Inra - Université Victor Segalen Bordeaux II, Institut François Magendie, Bordeaux, France (laboratory of neurogenetics and stress, combined unit of Inra and Victor Segalen Bordeaux II University, François Magendie Institute, Bordeaux)
Véronique NAHOUM-GRAPPE, Centre d'études transdisciplinaires, sociologie, anthropologie, histoire, École des hautes études en sciences sociales - CNRS, Paris, France (centre of transdisciplinary studies, sociology, anthropology, and history; school of advanced studies in social science)
Claudine PÉREZ-DIAZ, Centre de recherche psychotropes, santé mentale, société, CESAMES (UMR 8136), CNRS-Université René Descartes Paris V, Paris, France (research centre for psychotropics, mental health and society, CNRS University)
Myriam TSIKOUNAS, Centre d'histoire sociale du XXe siècle/Credhess (UMR 8058), Université Paris I, Paris, France (centre of the social history of the XXth century, University Paris I)
The following participants presented papers
Patrick AIGRAIN, Office national interprofessionnel des vins - Inra, Paris, France (national interprofessional office for wines)
Jean-Michel COSTES, Observatoire français des drogues et des toxicomanies, Paris, France (French observatory for drugs and drug addiction)
Colette MéNARD, Institut national de prévention et d'éducation pour la santé, Vanves, France (national institute of health-related prevention and education) and Stéphane LEGLEYE, Observatoire français des drogues et des toxicomanies, Paris, (French observatory for drugs and drug addiction)
Michel REYNAUD, Département de psychiatrie et d'addictologie, Hôpital Paul-Brousse, Villejuif, France (Department of psychiatry and addictology, Paul-Brousse Hospital)
Jacques WEILL, Honorary University Professor, Tours, France
Marie ZINS, Epidemiology, public health and professional and general environment, Inserm U 88-IFR 69, Saint-Maurice, France
Scientific and editorial coordination
Élisabeth ALIMI, Head of expertise, Centre d'expertise collective de l'Inserm, faculté de médecine Xavier-Bichat, Paris, France (Inserm collective expertise centre, Xavier-Bichat Faculty of Medicine)
Catherine CHENU, Scientific attaché, Centre d'expertise collective de l'Inserm, faculté de médecine Xavier-Bichat, Paris, France (Inserm collective expertise centre, Xavier-Bichat Faculty of Medicine)
Jeanne ÉTIEMBLE, Director of the Centre d'expertise collective de l'Inserm, faculté de médecine Xavier-Bichat, Paris, France (Inserm collective expertise centre, Xavier-Bichat Faculty of Medicine)
Catherine POUZAT, Scientific attaché, Centre d'expertise collective de l'Inserm, faculté de médecine Xavier-Bichat, Paris, France (Inserm collective expertise centre, Xavier-Bichat Faculty of Medicine)
Bibliographical and technical assistance
Chantal RONDET-GRELLIER, Documentalist, Centre d'expertise collective de l'Inserm, faculté de médecine Xavier-Bichat, Paris, France (Inserm collective expertise centre, Xavier-Bichat Faculty of Medicine)
Claire NGUYEN-DUY, Proofreader, Paris, France
Summary
The alcohol consumption of a population is generally globally estimated in litres of pure alcohol per inhabitant and per year, regardless of age. Although subject to certain biases, these data can, nevertheless, be used to monitor changes in consumption over time and to make comparisons between different countries.
Although almost all French people consume alcohol, consumption habits vary considerably between young people, who mainly consume alcoholic drinks other than wine on weekends, and people over 65 years of age, who drink mostly wine on a daily basis. Consumer habits also differ between girls and boys and between adult men and women. It is therefore important to consider these various factors in order to define more appropriate prevention strategies.
It is also important to distinguish between the dangers of excessive consumption under certain circumstances, such as when driving, carrying out work-related or domestic tasks (with the ensuing consequences—accidents and acts of violence, etc.), and the longer-term risk associated with chronic consumption. The social costs associated with excessive alcohol consumption compared with health costs indicate that this problem should be considered by linking the two dimensions, namely social and health, in a public health approach that encompasses prevention, care, and social reinsertion.
Global alcohol consumption has fallen from almost 18 litres of pure alcohol per year and per inhabitant in 1960 to almost 11 litres in 1999
Two major sources of data allow alcohol consumption to be estimated on an individual and collective level: market studies and consumer surveys.
Market studies allow global alcohol consumption to be estimated per year and per inhabitant (15 years of age and above) based on the production, importing, and exporting of alcohol. Imports are added to the quantities of alcohol produced per country, and exports are deducted. After weighting according to the size of the population, a mean annual consumption rate per inhabitant is obtained, expressed in litres of pure alcohol.
This is a mean value that does not distinguish between sex, age bracket, socio-professional category, or other sociodemographic criteria. Furthermore, even if this is of little relevance to France, it appears that quite a considerable proportion of alcohol production is not taken into account (not declared and, therefore, not registered). This is particularly evident in the Scandinavian countries and Canada, where it can account for up to 30% of alcohol production.
In France, following an increase between 1951 and 1957, global alcohol consumption fell by almost 40% between 1960 (17.7 litres of pure alcohol/year/inhabitant) and 1999 (10.7 litres). In 20 years, wine consumption has fallen by almost 40% and beer consumption by 15%. The consumption of spirits has also declined (with considerable fluctuations over time). This fall in global alcohol consumption is therefore due essentially to a substantial decrease in the consumption of wine.
In 1999, France ranked in fourth position behind Luxemburg, Ireland, and Portugal. Wine consumption is on the decline in Southern Europe but is increasing very markedly in Northern Europe. The differences in alcohol consumption between the Latin countries, which are traditionally wine producers and consumers, and the Anglo-Saxon and Scandinavian countries persist but are increasingly less noticeable.
Table
Alcohol consumption1 in France and Europe (World Drink Trends, 2000).
The countries traditionally recognised for their beer and spirits consumption have also witnessed a very rapid growth in their wine consumption, whereas wine-consuming countries have registered an increase in beer consumption. Beer is a newcomer to Mediterranean countries and is mainly consumed by young people. Alcohol consumption in Europe is thus becoming more evenly distributed. However, the increase in beer consumption does not offset the decrease in wine consumption, hence global alcohol consumption is declining.
Some countries around the world have witnessed an increase in their global alcohol consumption (Brazil, Paraguay, Turkey, and Mexico in particular), while others have noted a significant decrease (United States, Chile, Argentina, and Algeria in particular).
Table
Changes in the consumption of wine, beer, and spirits over the last 20 years (World Drink Trends, 2000).
Over 80% of all the alcoholic beverages exported come from European countries. France remains the leading exporter of alcohol (25.9% of the world's trade), while the United States is by far the leading importer.
Consumption surveys highlight indicators that enable homogeneous groups of the population to be followed over time and allow changes in attitude toward alcohol to be studied according to sex, age, and other sociobiographical criteria.
The tools used, the approach adopted, the person carrying out the survey, and the interviewee are all factors that are taken into account when assessing consumption. Depending on the way in which a questionnaire is administered (face to face, over the telephone, or via a self-questionnaire), the information relating to consumption and the level of non-response can vary.
The traditional cause of error mostly observed in consumer surveys is underdeclaration. This can be either intentional, because occasional drinkers have been overlooked, or because the frequency of consumption has, in fact, been underestimated. Consumer surveys therefore underestimate the quantity consumed by 40% to 60%. The response rate to questions asked is lowest for face-to-face surveys, increasing with telephone surveys, and reaching a peak for self-questionnaires (where the relevance of the responses cannot be corrected). However, because the validity of the questionnaires has been assessed in numerous studies over the last 20 years or so, it has come to light that, regardless of the method used to validate them, there is a good correlation between declarations of alcohol consumption.
The data obtained during these surveys show that more men drink than women. They consume alcohol in larger quantities (overall and on separate occasions) and more often than women. They become inebriated more frequently than women. This male-female discrepancy is evident in all international surveys in terms of both quantity and frequency. People tend to drink more frequently as they get older, but consume smaller quantities. This is particularly true of men.
By monitoring subjects in the same cohort over time, a distinction can be made between the specific effect of age and that of belonging to a specific generation. Because it is difficult to study cohorts of individuals over time, “pseudo-cohorts” are formed. These are individuals who, as far as possible, present the same (sex, age bracket, and socio-professional) characteristics.
From 20 years of age, more than one French person in two consumes alcohol at least once a week
In France, the Baromètre santé 2000 1 estimated the daily, weekly, monthly, and more occasional consumption habits of the French population between 12 and 75 years of age.
Among these French people, 3.5% declared that they had never drunk any alcohol in their lives. The proportion of abstainers decreases as a function of age (17% at 12–14 years and almost 2% at 45–54 years). Women abstain more frequently than men.
Over the last 12 months, 90% of the 12–75-year-olds admitted to having drunk at least one alcoholic drink.
Among the 12–75-year-olds, almost 20% admit to drinking alcohol every day—28% of men and 11% of women. This daily consumption pattern starts to appear in young people from the ages of 20–25 years, increasing with age and reaching a peak between 65 and 75 years of age, affecting 65% of men and 33% of women.
Among the 12–75-year-olds, almost 40% admitted to consuming alcohol at least once a week but not every day (44% of men and 34% of women). Weekly consumption is more prevalent among the younger generations and is, indeed, the major consumer trend among the group 20–44 years of age (60% of men and 40% of women). On average, more than one of two French people drink alcohol at least once a week from 20 years of age onward (7 of 10 men and 4 of 10 women). This weekly consumption, however, gives way to daily consumption among the older generations.
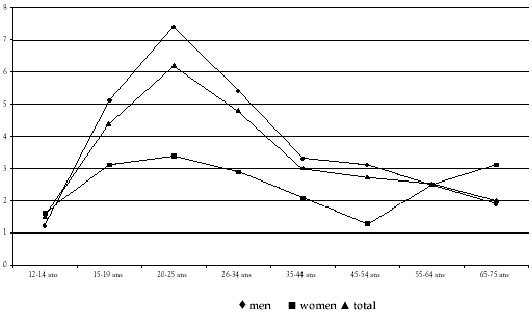
Figure
Alcohol consumption over the last twelve months according to frequency of intake and age (Baromètre santé 2000, CFES).
Figure
Proportion of daily alcohol consumers over the last twelve months according to sex and age (Baromètre santé 2000, CFES).
Of the 12–75-year-olds, 16% admit to consuming alcohol at least once a month but less than once a week. This monthly or occasional consumption mainly concerns young people.
Wine is the most widely consumed alcoholic drink. 17.5% of the 12–75-year-olds consume it on a daily basis (25% of men and 10% of women). This increases with age (62% of men between 65 and 75 years of age and 32% of women in the same age bracket).
Figure
Daily consumption of various types of alcoholic beverage over the last twelve months, according to age bracket (Baromètre santé 2000, CFES).
Daily beer consumption concerns almost 3% of the 12–75-year-olds (5% of men and 0.5% of women). Weekly consumption is most frequent. Only 0.8% of the 12–75-year-olds consume spirits on a daily basis. This is essentially limited to men over 45 years of age. Weekly, monthly, or occasional consumption is the most frequent, with each category concerned with approximately 19% of the 12–75-year-olds.
Generally speaking, weekend consumption is higher (in terms of variety and quantity of drinks) than during the week for all age brackets and for both sexes. This particular trait certainly helps to explain why inebriation is more common among weekly consumers (young people between 18 and 25 years of age drink 5.6 glasses on a Saturday compared with 1.9 glasses in the case of the over 55-year-olds) than among daily consumers who, on average, drink more.
Table
Average number of glasses drunk in an evening according to socio-professional category (Baromètre santé 2000, CFES).
The average number of glasses drunk in an evening is higher in the "craftsmen, tradesmen and Company Director" category (averaging 3.4 glasses).
Inebriation is most commonplace among young people. The difference between the sexes is most apparent in the 20–25 age bracket: 40% of men between the ages of 20 and 25 repeatedly become drunk (more than three times per year) compared with 24.5% of women in this particular age bracket.

Figure
Average number of cases of inebriation over the last 12 months per sex and per age (Baromètre santé 2000, CFES).
Interviews during which people were asked about their risk of alcohol dependency, both past and present, show that 1 of 10 adults is affected, men being involved three times more often than women (13.5% versus 4%); the difference between the sexes increases with age.
Although the Baromètres santé (surveys) of 1992, 1995, and 2000 were modified in the questionnaires, some indicators can be compared. A slight decrease in consumption frequency and the quantity consumed can be noted for men and women over 20 years of age. On the other hand, changes in terms of inebriation are not significant.
In the working environment, men drink twice as much alcohol as women
In France, several studies have been carried out in recent years to assess the prevalence of alcohol consumption in the working environment. First and foremost, it should be noted that the collection of objective and systematic data is ethically difficult within the scope of occupational medicine. Furthermore, it should also be noted that acceptable blood alcohol levels change over time—not least by current legislation for road users—which is 0.5 g/l at the present time (law dated 13 November 1996).
According to an IPSOS survey conducted in September 2001, 71% of those interviewed consume alcohol during business lunches/dinners, with 35% consuming more alcohol than usual. Alcohol consumption in a professional context is evident in physically demanding professions, such as building, farming, and maintenance works, as well as in professions dealing with the general public.
On the basis of a 1999 study involving work doctors in the Paris region, almost one of four employees regularly consumes alcohol at work with colleagues or clients.
In all cases and regardless of age, the average number of glasses consumed by men in a working environment is 1.5 to 2 times higher than that of women. According to the results of the Gazel cohort study (over 20,000 EDF-GDF (gas and electricity) employees), 18.3% of men admitted to drinking 3 to 4 glasses of alcohol every day and 12.3% of men admitted to 5 glasses and more per day. The equivalent percentages in women are 3.5% and 1.2%, respectively.
Surveys carried out by teams of work doctors have also facilitated assessment of the number of people experiencing alcohol-related problems. In the iron and steel sector, doctors confirmed in 1983 that 10% of workers were excessive drinkers and 8% alcoholics. In Lorraine, the occupational medicine departments estimated in 1983 that 3% of the workforce were excessive drinkers and alcoholics. As regards a sample of national defence workers, doctors found that 15% were excessive drinkers and 7% alcoholics in 1989. A 1991 survey conducted in a postal sorting centre revealed that 16% of employees drank to excess, whereas 8% were alcoholics. In 1997, a survey focusing on the workforce in the municipality of Saint-Étienne revealed that 10% were alcohol dependent. The inter-company survey conducted in 1997 in Lower Normandy showed that 3.4% of the employees had been identified as excessive drinkers and 1.1% as alcoholics. These figures can be compared against those recorded in an initial survey carried out in this same region in 1980 in which 8% of the workforce were alcoholics. The survey carried out in 1991 found that 3% drank to excess and 2% were alcoholics. According to the most recent survey, almost all professional sectors are affected by excessive alcohol consumption, although the building-public works' sector remains particularly susceptible.
In young people, repeated bouts of inebriation are often associated with regular alcohol or cannabis consumption
On the basis of surveys conducted in French schools between 1993 and 1999 (ESPAD 2 ), experimenting with alcohol has slightly increased in France, rising from 81% to 86% in 16-year-old boys and from 79% to 85% in girls of the same age. Repeated usage (at least 10 uses in the course of one month) does not appear to have increased. As regards inebriation, the number of young people who, between 1993 and 1999, admitted to having experienced at least 10 episodes of drunkenness over a 12-month period has remained stable in the 14–16-year-old bracket (5% in the boys) but has slightly fallen among the 17- and 18-year-olds (from 14% to 10% in boys 18 years of age and from 3% to 2% in girls of the same age).
In 1999, the proportion of French pupils who consumed alcohol during the previous 12 months was below the average figure obtained for all European countries (77% versus 83%). The same applied to the proportion of French pupils who had been inebriated in the last 12 months (36% versus 52%).
The French survey, ESCAPAD, 3 shows that 17-year-old girls had their first taste of alcohol at 13.6 years, i.e., on average 6 months later than boys (13.1 years). Alcohol preceded smoking. The first experience of inebriation occurred approximately 2 years after initial alcohol consumption, regardless of age and sex. Girls declared having been inebriated for the first time on average 5 months after boys of their own age.
Table
The frequency of alcohol consumption over the last 30 days in 17-year-old girls and boys between 17 and 19 years of age (Escapad 2000, OFDT).
Behaviour differs between the sexes. The prevalence of smoking, alcohol consumption, and inebriation appears to be linked to the early onset of experimentation. As regards concomitant usage, cannabis and alcohol are mostly linked.
Table
Frequency of inebriation throughout life (Escapad 2000, OFDT).
According to longitudinal studies conducted in the United States and Europe focusing on adolescent alcohol consumption, the first risk factor for consumption, at the end of adolescence or the onset of adulthood, is the early onset of consumption. The onset of alcohol consumption at 12–14 years of age is a predictive factor for alcohol consumption at 16 years of age or even alcohol abuse, whereas the onset of alcohol consumption at 16 years of age is marginally predictive for adult consumption. This applies to both boys and girls.
One-third of young people between 16 and 17 years of age has experimented with alcohol, smoking, and cannabis. There is a gradual shift toward experimenting with one or even two substances, followed by all three substances.
One young person in five regularly uses one of these substances. Polyconsumption increases appreciably with age, especially in the case of 19-year-old boys, 14% of whom take several substances on a regular basis.
Outings and evening functions are a fundamental aspect of a young person's life and often lead to alcohol consumption. However, being a consumer may entice a young person to go to functions. According to Escapad, young people who frequent "techno" events account for less than 1% of the study population. Consequently, most of the alcohol consumers, smokers, and people who become inebriated are recruited from among youngsters who have never been to a "techno" event.
The correlation (measured by the odds ratio(OR)) between the regular consumption of cannabis and regular alcohol consumption or smoking is high (3 < OR > 5) for boys and even higher (OR > 5) for girls. For both males and females, the link between repeated inebriation and regular alcohol or cannabis consumption is very marked. It is, however, more marked for girls than for boys. Overall, the risk of regular cannabis consumption is higher among female smokers than male smokers and among female drinkers than male drinkers. The risk of having been inebriated several times over the last 30 days is higher in girls who consume alcohol on a regular basis or take cannabis than among boys with similar habits.
Certain sociodemographic and educational factors are more closely linked with a high alcohol consumption. The same applies to absenteeism from school. The pupil's behaviour at school (absenteeism, school results, and liking for school) is more closely linked with alcohol consumption than familial characteristics ("intact", single-parent, restructured family), regardless of the type of school establishment (priority education area, public, private, town, or rural location). Violent, delinquent behaviour (major violence, theft, and disputes), running away, and attempted suicide are associated with regular alcohol consumption. Consumption is not linked more frequently with major violence than it is with other problems, such as attempted suicide or running away. The links between regular consumption and risky behaviour are always more noticeable for girls than for boys. Finally, those who do not practise any sport or who practise for more than 8 hours per week are more likely to become regular consumers of alcohol than others.
Alcohol plays a key role in the contemporary youth party scene
The creation of a social link often implies gestures that ritualise alcohol consumption in our society: drinking is a must to celebrate a financial market or a sporting or professional success. Festive drinking, i.e., that which implies excess as standard, is required to mark a change in lifestyle (a birth, a marriage, a retirement, a move) or Christmas/New Year festivities. This drinking tradition pervades individual space, private moments, and the collective social scene. Drinking is an invitation to enforce this social link. But “excessive drinking” also implies “social unhappiness” in our culture and is often associated with an unhappy love affair or images of economic and social decline. The social function of drinking is heightened by that of its economy. The alcohol trade, in all its forms, comes from a long history of wine and is characterised by resistance to historical and social change, to wars and periods of recession. The need for social drinking firmly consolidates a market that has been extended worldwide for more than 20 centuries. Investigating alcohol in public health terms involves identifying this historical, economical, and sociological focus for social drinking.
How have the consumption habits of today's youth changed? The quality of preventive messages is linked with this awareness.
At the end of the 19th century, writers of folklore and romantic interludes between girls and boys in conventional French societies explained that ways of celebrating, gestures and attitudes, excesses and boundaries for transgression are coded by the community. In fact, these traditions, customs, habits, and codes define parameters for the young people of the village, for the environment, and for close relationships between young people allowing them to choose their partners with or without parental consent. In this culture, sexual restrictions must be maintained, especially for the girls. Young people must therefore obtain permission and are subject to collective constraints before going off to party.
Nowadays, trends relating to going out and different types of “partying” are constantly changing among young people in favour of an urbanised lifestyle, even in the countryside, where the emphasis is on freedom and mobility. Today, festive occasions differ in terms of what to wear (party clothes or not), the venues, itinerary (drinking, dancing, singing, eating and hanging around, etc.), the pace and time-scale which tend to invade the week and to “fall” toward the end of the night or sometimes the next day. The choice is no longer a party, but three or four “bars” or “nightclubs” between which young people flit to and fro at top speed. They sometimes choose the town pavement to party, like in Madrid, along the lines of “Botellon”.
Drinks are being invented all the time, with unprecedented names and blends of ingredients. Overconsumption intervenes at every stage through the evening, from planning the evening ahead through to the last drop consumed in the small hours of the morning. Alcohol consumption is often accompanied by the use of other legal or illegal psychotropic substances in an excessively noisy atmosphere.
In the absence of any social framework based on traditions, the group of young people is sociologically isolated in the collective invention of the party scene. Within this context, extreme behaviour may be a tactic leading to an amorous or sexual encounter. The freedom of these outings can also be paid for with the risk of boredom, of a social vacuum, which, itself, is associated with the desire and need for psychotropic substances.
Prevention must take into account what is really at stake behind this restructuring of the young contemporary party scene: comprehensive research into social sciences is needed here.
The advertising or health-related message is perceived and accepted much more readily when coming from a source that is appreciated by the recipient
In France, as regards alcohol and drinkers, advertisers are still nowadays reworking the clichés that, for the most part, were created under the July Monarchy, a period of generalisation of industrial alcohols. This imagery, forged by certain doctors specialising in hygiene, compare good and bad alcohol, good and bad drinkers, and good and bad alcohol consumption.
According to designers, good alcohol awakens the senses and stimulates the intelligence. It is a panacea and contributes to national wealth. The middle class who sample such beverages, discretely and from a connoisseur standpoint, do not allow themselves to be dominated by the drink, but dominate it themselves. At the other end of the spectrum, poor alcohol, which is consumed mainly by those from a more humble background—soldiers, the down-and-outs, peasants, and labourers in particular—hamper the senses and are poisons that give the people who drink it brutal, animal instincts and, finally, reify them.
In the 1840's, a few “humanists” contested these stereotypes that confused addiction and inebriation. But their comments, which were not welcome because they denounced chronic, middle class alcoholism, were not understood. The message was not taken up by physicians belonging to anti-alcohol leagues until the period between the two world wars.
Up until the mid-1950s, all the prevention posters were the same. The drinker, always portrayed as a man and a labourer, is a criminal devoid of human traits and engenders morons. Stories accentuate the harmful effects of alcohol on health.
Advertising in favour of alcohol obviously portrays the opposite: happy drinkers, stylishly dressed, often personified by the stars of politics, the cinema, or fashion. Slogans emphasise the “therapeutic” virtues of alcoholic beverages.
During the Glorious Thirties, the number of labourers decreased, and images of alcohol changed. At the same time, however, from this time onward, artists and doctors discovered the female drinker beneath the guise of the woman with a good job, who not only took over a man's role but also his “vices”, i.e., a woman who smoked and drank. Going beyond appearances, this upper class female drinker and the “young person” who replaced her in the late 1970s, present a number of similarities with the labourer drinker of the 19th century—they too drank spirits, which were consumed like psychotropic substances, in an attempt to quickly change the state of mind.
Prevention and promotion campaigns will adapt to these new images. In terms of health, designers are breaking tradition with hygiene-related strategies to reply, point by point, to alcohol consumers to overcome the false ideas portrayed by advertisements and to bring the consumer back to reality. In legends, the message stipulates that alcohol is not warming, is not a real food, does not boost strength, is not associated with life and health but with disease and death, it is not synonymous with freedom and evasion but with prison, and does not allow you to face up to situations but to lose face. Persons in charge of health campaigns, who from now on are addressing all social categories, no longer seek to portray the drinker as guilty but to make him/her responsible, to give him/her choices, such as “drink or drive”. They are no longer portrayed as “against”, i.e., against alcohol, against inebriation, or against the drinker's attitude but suggest an alternative to alcoholic drinks with advertisements “for” fruit juices and grape juice in particular.
Pro-alcohol advertising is also changing, not only to bring itself into line with the latest train of thought but also because it is about to be seriously regulated. The law of November 29th, 1960, which prevents alcohol from being associated with sport or driving and which does not allow the stimulating, aphrodisiac, or sedative properties of alcohol to be emphasised, conducted particularly sober advertising campaigns up to 1968 when alcohol advertising made its debut on the small screen. Despite the television media ban from 1975 onward, advertisers launched a major offensive to persuade their audience that alcohol promotes communication between people of different ages, gender, and social classes, that alcohol could be drunk without any hesitation in the workplace because it was a performance factor. After 1987, however, the messages changed. Alcohol is now only consumed between peer groups and people of the same age, at home and especially in the evening.
Table
Communication measures implemented by the Ministry for Health and the CFES in the form of audiovisual campaigns.
From 1990 onward, drinkers left the limelight as though advertisers were already prepared to adopt the restrictive measures that did not come into force until January 1991 (Évin law). Until 1995, artists were feeling their way, and advertisements were sober, unoriginal, and few in number. Finally, they succeeded in playing their game well while remaining within the strict framework imposed by the Évin law. They understand that the objective is less to show drinkers and alcohol as to create images and slogans that channel the recipient's thoughts via a slow, automated perception process, utilising all the graphic and photographic techniques available. At the present time, no country has surveys that can accurately determine the impact of these pro- or anti-alcohol images on their audience. Given the numerous variables involved, which are not only of an advertising but also of a commercial and sociocultural nature, it is difficult to establish a marked cause–effect relationship between advertising and alcohol consumption. Until now, research has been deployed in two complementary ways: experimental research and opinion polls that tend to establish correlations between individual exposure to advertising and consumption schedules.
Psychologists have tested the effects of pro-alcohol advertising on spectators chosen for their ability to express themselves and their diversity in terms of consumption. They showed them slides or advertisements promoting alcohol and observed their physical reactions during the broadcast and their “alcoholic” behaviour at the end of the presentation. Many epidemiologists have carried out two-pronged, selected surveys focusing mainly on young people and involving: exposure to a series of repeat press announcements followed by semi-directive interviews (or questionnaires) centred on memories of advertisements. Surveys on health campaigns are few and far between, hardly sophisticated, and all point to the same conclusions: daily drinkers levy even more criticism against these images than occasional drinkers.
These investigations raise several problems: the subjects are placed in a very difficult situation compared with that of an ordinary spectator who never sees 15 or 20 images of alcoholic drinks in succession. Furthermore, most experimental studies are carried out in a laboratory specialising in drug- or alcohol-related research.
Although several surveys have led to conflicting conclusions—some proving and others invalidating the effect of advertising on alcohol consumption—several results, on the other hand, are consistent, and certain recurring trends appear to be significant:
- Longitudinal studies prove that, firstly, young people are prejudiced against alcohol, but as they become adolescents, they change their opinion toward drinking. The reasons for this change in attitude cannot, however, be determined.
- It takes more than exposure to an advertisement to trigger an impact upon beliefs and behaviour. The audience must be aware of the fact that they are looking at an advertisement for a specific product and not simply at just any image. Children, unlike adults, generally think of advertisements as films.
- The advertising or health message is perceived and accepted more readily when it comes from a source that is appreciated by the spectator. The best-remembered advertisements appear to be those that star celebrities from the world of show business or sport. The health posters that are best received are those shown to young people by DJs or leading celebrities.
- The ads that are best remembered are those that employ attention-drawing techniques to their full capacity: slow motion and detailed images, extensive work on the soundtrack, particularly the reconfiguration of music and famous, patriotic songs, etc. Audiovisual advertising broadcast in a room or on the small screen, therefore, appears to have more impact than press announcements composed of fixed images and slogans.
A few isolated researchers have carried out textual analyses of press releases, slogans, and televised broadcasts. They have set themselves the task of understanding, through a detailed study of the composition of the image and possibly of the text, the characteristics of drinkers and the techniques used to influence the audience. They have set out not only to detect what is said and shown but also to establish the way in which the message is portrayed and the various graphical, linguistic, and pictorial experiments used in an attempt to grasp the audience's attention.
Studies that focus directly on pro-alcohol advertising highlight any trickery. Thus, in France, kept off-camera since the Évin law, the consumer-presence is implied rather than shown. In a large number of advertisements, the camera lens is installed instead of the public, in front of a table or a counter on which can be found glasses and a bottle photographed according to scale. With subtle lighting, the photographer succeeds in recreating the composition of the materials (the creamy foam, the sparkling bubbles, and a freshly misted glass, etc.); and there, you have it, an incentive to drink. An analysis of advertisements for alcohol-free drinks shows how designers convey messages of inebriation without displaying alcoholic drinks. Ever since the Évin law, alcohol manufacturers who often produce mineral waters, beers, and alcohol-free aperitifs as well, focus, in an advertisement for a soft drink, on venues traditionally associated with “drinking to excess”, namely bars and discotheques, and include doubles of famous singers (Edith Piaf) or actors (James Cagney, Humphrey Boggart) renowned for their overindulgence. They portray inebriated persons without alcohol, who stagger along, reel, and are the victims of hallucinations but who are intoxicated not with alcohol but with a risky sport.
Other researchers have analysed TV films and televised series watched mainly by young people. They portray drinkers as having two major traits: they are systematically personified by stars who made a positive social image at the end of their career and benefit from the highest social status in history.
At best, textual analysis has enabled researchers to discover the intentions, deliberate or otherwise, of advertisements. These investigations nevertheless have their uses in an area where designers do not necessarily confess their intentions.
Alcohol is involved three times more often in road-traffic accidents than in accidents in the workplace
Numerous studies have investigated the presence of alcohol in various types of accident to establish any correlation between blood alcohol levels and the accident.
Although alcohol is associated with various types of road-traffic accidents, it also plays a major role in domestic accidents, accidents at work, in fights and in drownings, etc. In 1992 in the United States, alcohol was found to be involved in 50% of the road-traffic accidents and in fewer than 20% of accidents occurring in the workplace.
In France, a multicentre study involving almost 5,000 accident victims admitted to 21 hospitals between October 1982 and March 1983 allowed the blood alcohol levels of the victims and two biological indicators, namely gamma-glutamyltransferase (GGT) and mean corpuscular volume (MCV), to be examined at the same time, confirming significant and chronic alcohol consumption. The results indicate that alcohol is very often involved in fights and road-traffic accidents: 60% of men involved in fights have a blood alcohol level exceeding 0.50 g/l. Sporting accidents and accidents in the workplace represent the lowest incidences of elevated blood alcohol levels (5% in men). In women, high blood alcohol levels are mainly evident in domestic accidents and fights.
Table
Alcohol-related accidents in the United States (according to Cherpitel, 1992).
Table
Alcohol-related accidents in France (report by the High Committee for the alcohol-related investigation and information, 1985).
According to this study, a high proportion of victims present with laboratory signs of significant and chronic alcohol consumption. This applies to 27% of men and 32% of women, taking all accident victims into account. Victims presenting with acute alcohol intake in the absence of any signs of chronicity are fewer in number and may be qualified as occasional drinkers (slightly over 10% in men and 2% in women). The average age is 32 years for men and 39 years for women. Among the accident victims presenting with signs of chronic alcohol intake, the average age is 41 years for men and 48 years for women. In cases of blood alcohol levels equal to or greater than 0.8 g/l, one-third reaches or exceeds 2 g/l in men and women less than 30 years of age. The size of the group of accident victims presenting with raised blood alcohol levels illustrates that the risk of accident is higher depending on blood alcohol levels. A more recent study in the United States (1996) involving over 3,000 patients in four emergency departments also shows the increase in various types of accident depending on alcohol consumption (quantity and frequency).
Table
Accidents according to alcohol consumption, based on an American study (according to Cherpitel, 1996).
Alcohol is responsible for approximately 1,900 deaths per year on the road
In France at the present time, alcohol is involved in one-third of fatal road-traffic accidents. The total number of people killed on the road in one year is around 5,700 (2003 update), and the number injured, 110,000. Alcohol is linked with around 1,900 deaths and 16,000 injuries on the road each year. In 1970, alcohol played a role in 40% of fatal accidents.
In France, 60% of the accidents where drivers have an illegal level of alcohol in the blood (>0.5 g/l) occur between midnight and 04.00. The number of alcohol-related cases in which women are responsible for fatal accidents is always 3 to 4 times less than that of men. However, the number of female drivers arrested for breaking the law and nighttime accidents involving one single vehicle is on the increase among women in Anglo-Saxon countries. Preventive actions should take into consideration the behavioural differences between men and women before driving.
The relative risk on the road for a given blood alcohol level decreases with age in both men and women. At equal blood alcohol levels, the risk of a road-traffic accident is higher for a young person than for an adult. Road-traffic accidents are a major cause of premature mortality in young people.
Experimental studies concerning the effects of alcohol on driving show that ability is adversely affected from a level of 0.2 g/l, generalising from 0.5 g/l for multiple functions: reduction in peripheral vision, in-depth vision, prolonged reaction time, poor judgement of distances and speed, difficulty to judge distance from parked vehicles and to follow mobile vehicles; impaired processing of information; alteration in immediate and differed visual memory; poor co-ordination of manoeuvres. Low doses of alcohol also have an effect on vigilance and attention especially for tasks that require the spatial processing of driving-related information, especially during periods of drowsiness in the afternoon or at night. Moreover, if cognitive function is disrupted, as is the case with heavy drinkers, then visual performance is also impaired.
Table
The increase in the relative risk (RR) of a fatal accident associated with an increase in the blood alcohol level of 0.2 g/l according to age and sex (according to Zador et al., 2000).
A link between the early onset of alcohol consumption and alcohol-related road-traffic accidents has been highlighted in certain longitudinal American studies. These studies show that people who started to drink before the legal age of consent (21 in the United States) present an additional risk of alcohol-related accident, regardless of the family history of alcohol dependence, frequency of consumption, and different variables associated with age and consumption.
Table
Evaluation of the "additional risk" of accident associated with the age of onset of consumption (according to Hingson, 2000).
Drivers of motor vehicles are not the only ones to be affected by the problem. The prevalence of alcohol consumption also has a significant impact on pedestrians, (motor) cyclists, and adult or children passengers. The significant mortality rate associated with the latter category is particularly due to the fact that passengers do not always wear a seat belt when the driver is under the influence of alcohol.
Table
Proportion of blood alcohol levels exceeding 0.8 g/l per category of users and per number of people involved (according to "Alcohol and accidents", High Committee for the investigation of and information on alcoholism, 1985).
In accidents where only one person is involved, motorcyclists are the group under the least influence of alcohol (there is, on average, a high proportion of young drivers who are more sober). On the other hand, in accidents involving several people, the differences are less marked with pedestrians being mostly under the influence of alcohol and cyclists to less of an extent.
Compared with our European neighbours, the SARTRE (Social attitudes related to traffic risk in Europe) surveys show that the French most often take to the wheel after consuming alcohol. Furthermore, alcohol intake by young French people is heading toward an Anglo-Saxon model (namely "binge drinking" or "celebratory" drinking on a Saturday night) with different alcohols and other psychotropic substances being combined more often, thus constituting one of the trigger factors in exacerbating accidental risk in young people.
One of the reasons accounting for the extent of road rage and mortality in our country lies in the historical delay in our culture with regard to implementing risk management and preventive strategies. The Scandinavians, who have one of the lowest road mortality rates in the world, realised, at a very early stage, those elements involved in road safety and implemented educational and preventive strategies. Norway was the first country in the world to adopt a maximum legal blood alcohol limit. In 1936, this was 0.5 g of alcohol per litre of blood (the current legal level in France, adopted in 1995), and the consequences of breaking the law were three weeks' imprisonment and a two-year driving ban. The School of Legal Philosophy in Uppsala, which recommended a tougher crackdown on offenders, stated that the law served an educational purpose: initially, drivers comply with the law due to the threat perceived or a fear of the police, then take this law on board, over time, so that it becomes a social and individual standard. Thus, the law no longer needs to be enforced as shown in current Norwegian data.
Globally, all the control-sanction models have been inspired by risk models of the Scandinavian type. These methods state that, in order to change drivers' behaviour, their perception of the risk—probability—of being checked or punished must be enhanced. This is the subjective risk. To do this, the risk of actually being checked must be accentuated. Therefore, the number of controls and punishments must be increased. This is the objective risk. All of these models seek to reduce the discrepancy between these two risks so that an objective risk can be internalised into a subjective risk aimed at modifying behaviour. The objective risk must be publicised at the same time. In Canada, it is the frequency of checks combined with moderate, yet repeated sanctions that supposedly reduces the incidence of law-breaking behaviour. In the United States, the influence of these two models would be applied alternately. In Australia, the controls should be carried out sufficiently often to trigger dissuasion by friends and family. As for the British, since the early 20th century, they have sought to involve drivers in decisions and apply control and sanctions. The American, Canadian, and Australian studies have demonstrated the preventive efficacy of lowering the legal blood alcohol limit for a few years in the case of newly qualified drivers.
Behaviour under the influence of alcohol is governed by complex, determining factors
Alcohol consumption prior to driving a vehicle is tantamount to taking a risk for which the psychological benefits are considered higher than the risks incurred. Thus, if alcohol is consumed by drivers then positive (euphoria and no inhibitions) and negative (arrests, accidents and conflicts, etc.) expectations conflict with each other. The risk may be badly perceived, if at all, if the blood alcohol level is estimated subjectively and in the presence of perceptive, cognitive and motor disruptions due to alcohol. Furthermore, the expectations of alcohol consumption differ between men and women, and according to the socio-cultural context. Passengers who have to travel in a vehicle whose driver is under the influence of alcohol perceive the risk. The latter is undertaken – it is not investigated voluntarily but simply accepted under the circumstances.
The preventive strategies applied to the problem of alcohol must, therefore, incorporate these various risk aspects: some should certainly focus on risk-taking by attempting to reinforce the positive aspects of alternatives to inebriation. Others may observe the risk perceived by emphasising the discrepancy between subjective estimates of alcohol consumption and the reality of the blood alcohol level. Other strategies may target peer group pressure, with individuals being forced to accept a risk that they do not really wish to take.
Behaviour while under the influence of alcohol, traditionally considered as a predicting factor for accidents, is now also considered as a sign of alcohol dependency. In fact, an illegal blood alcohol level very often suggests an alcohol-related problem as well. Every year, the 100,000 road convictions in France could, therefore, be considered as providing numerous opportunities for treatment. This opportunity is in the hands of the legal sector in particular. Driving while under the influence of alcohol is, in fact, one of the biggest offences dealt with by the legal profession (24% of all offences are road-related offences). Access to treatment via an incentive or a legal obligation seems to encourage patients to undertake a voluntary cure.
The discrepancy between positive blood alcohol levels and offences is offset by contraventions associated with a blood alcohol level ranging from 0.5 to 0.8 g/l, sentences covering offences and contraventions. In 94% of cases, the sentenced are males with an average age of 38 years. In 10 years, the number of 18- to 24-year-olds sentenced has fallen substantially from more than 20% to 13%, whereas the proportion of over 40-year-olds has increased by more than one-third, reaching 43% in 1999. Taking all these sentences into account, 10 % concern habitual offenders, the number of which is constantly increasing. The number of drivers sentenced for manslaughter committed under the influence of alcohol has been decreasing since the 1980s. Prison sentences were awarded in 98% of cases (half of which are partly closed or closed prisons). The number of sentences for involuntary wounding has also fallen since the 1990s. Prison sentences were given in 80% of these cases with closed imprisonment in less than 10% of cases.
Although preventive and repressive actions have been reinforced in France, the role of alcohol in fatal accidents and the “extreme risk” for young people has, nevertheless, scarcely changed. A differential approach to prevention is apparently needed in order to adapt the strategy to the type of offence. The law, by definition, applies to all drivers, but a single measure does not have the same effect on all. The group of offenders who commit crimes while under the influence of alcohol is not uniform. It comprises sub-groups with specific characteristics that therefore require appropriate, preventive treatment. Let's reconsider the principal factors involved:
- Age: Some approaches are effective for young people, but not for adults and vice-versa.
- Sex: The motivations underlying alcohol intake and offences appear to highlight differences between men and women.
- Anti-sociality: A fraction of the population of offenders has also been sentenced for offences and contraventions that do not involve road traffic. Once again, it seems obvious that a driver who occasionally consumes alcohol and who is well integrated socially cannot be dealt with in the same way as a driver with a criminal record who has already been charged with various offences.
- Psychopathology: A fraction of offenders present with related problems that compromise the efficacy of overly “light” approaches, such as awareness training periods to highlight certain aspects, and therefore benefit from an enhanced psychotherapeutic approach.
Alcohol could be responsible for 10% to 20% of accidents in the workplace
Although this is a recurring problem in the working environment, there have been no recent, precise studies of the implication of alcohol in accidents in the workplace. Some American studies reported in an international working review (Organisation internationale du travail (OIT); international working organisation) that alcohol and drugs trigger between 20% and 25% of accidents in the workplace and up to 30% of work-related deaths.
In France, according to the Association nationale de prévention de l'alcoolisme (Anpa, 2000–2001; national association for the prevention of alcoholism), alcohol is directly responsible for between 10% and 20% of accidents in the work place, taking all socioprofessional categories into account.
At the SNCF (French railway), alcohol is thought to be involved in 20% of the 13,500 work-related accidents that occur each year, although it has been noted that most of the accidents involved non-alcohol-dependent agents.
An extensive study including a systematic assay of blood alcohol levels in the workplace was carried out in France more than 40 years ago. The incidence of alcohol intake on the frequency of accidents in the workplace and the repetition thereof was evaluated in six companies involving over 3,000 controls and over 1,000 victims. According to the companies and sampling time, alcohol consumption exceeding 1 g/l affected between 1% and 5% of the control employees and 2.5% to 11.5% of the victims.
Two more recent studies carried out in the hospital emergency departments in Tours in 1982 and in Nancy in 1988 allowed the extent of alcohol consumption to be assessed in victims, regardless of the nature of the accident.
The Tours study focused on over 2,000 wounded admitted to emergency departments (road-traffic accidents, brawls, domestic or sport-related accidents, accidents at work, or travelling accidents). There were as many working or travelling accidents (to and from work) as road-traffic accidents (excluding travelling accidents). Alcohol blood levels were the lowest in victims of accidents in the workplace). In the case of the latter, 10.3% presented with a blood alcohol level exceeding 0.40 g/l, 1.2% had a blood alcohol level greater than 2 g/l, whereas 9.3% of the victims, taking all accidents into account, had a blood alcohol level greater than 2 g/l. In the study conducted at the CHRU, Nancy, almost 150 of the blood alcohol levels measured concerned victims injured in the workplace or on the way to work. The percentage of victims injured in the workplace with a detectable blood alcohol level below 0.80 g/l was 9.1%, and 2% presented with a blood alcohol level exceeding 2 g/l. The figures were higher for accidents on the way to work (3.6% and 14.3%, respectively).
Based on the 1983 study carried out by the High Committee for the investigation of and information on alcoholism, the influence of alcohol in the workplace would mainly involve accidents in which the victim would fall. In fact, based on this study, 14% of the victims sustaining a fall in the workplace had a blood alcohol level equal to or greater than 0.5 g/l.
Table
Distribution of blood alcohol levels in accidents sustained in the workplace1 in men and women (according to HCEIA, 1985).
As regards alcohol intake, company practice is not always applied
The problems of alcohol in the working environment have not been discussed for many years. In the last 10 years or so, however, the experiences encountered by employers' doctors with regard to this problem have been published in the literature.
Fifty years ago, alcohol consumption in the working environment was often associated with physically difficult working conditions (working in heat, dust, the difficulty of the task at hand, and the risk of poisoning, etc.), and alcohol was used as a means of hydration. Employers' doctors, at this particular time, set out to improve the conditions at work and, in doing so, to reduce the factors for alcohol consumption. Changes in working tools over these last 20 years have replaced the physical exertion of the job by a substantial increase in mental exertion associated with psychological problems and stress where alcohol consumption can “alleviate” these new difficulties.
A survey published in the United States in 1995 showed that men with stressful jobs were 27.5 times more likely to develop alcohol dependence if their jobs gave them no scope for decision-making but imposed marked, psychological pressure, and 3.4 times more likely to develop alcohol dependence in a job with no responsibility but warranting substantial physical effort. This survey did not reveal any risk of alcohol dependency for women carrying out the same type of work.
The employer's doctor must investigate the suitability of an employee for a given post. In this particular context, he/she must constantly examine the risk of alcohol consumption in the employee in relation to the risk inherent in the job (safety of the work) warranting vigilance and precision, or a certain rhythm (shift work or nights). The employer's doctor must also define optimum ergonomic conditions, be attentive to physiological and psychological rhythms depending on increasing difficulties associated with the demands for performance, profitability, and constant changes to current working tools, regardless of the professional context. One of these key issues, regardless of the risks of driving under the influence of alcohol, will also be to preserve the mental integrity of the employee by protecting his cognitive functions in particular, hence the importance of collective and individual preventive measures within the context of occupational medicine: informing all personnel of the risks associated with alcohol by calling on approved organisations, forming link groups within the company by involving various players (staff representatives, trade unions, CHSCT (committee for hygiene, safety and working conditions), human resources directorate and medico-social services, etc.). It is, in fact, essential to perpetuate these actions to ensure their long-term efficacy. Numerous experiments with media coverage in certain establishments help to modify the mentality (alcohol-free day, action taken in company restaurants, alcohol-free drinks, etc.) Some large companies have even drafted an alcohol charter defining regulations relating to alcohol consumption within the company (drafting of a charter on the prevention of alcohol-related risks at the CHU, Bordeaux, specifying the approach to adopt in various situations where a member of staff has a problem related with alcohol consumption).
It should be noted that the code of practice, even if outmoded, is often not applied when it comes to alcohol consumption. This legislation is old (partly dating back to 1913) and inappropriate ("No-one is allowed to bring into the company any alcohol beverages to be drunk by staff other than wine, beer, cider, perry and mead"). The internal regulation, when it exists, often fails to include prevention of the alcohol-related risk. Similarly, the problem of employee reinsertion or continuation of his/her professional activity is not considered. However, information relating to alcohol and its consequences is available increasingly often in the medical practice, with emphasis on national campaigns. The suggestion of a self-questionnaire, for example, can help to trigger debate on this subject in the working environment.
According to victims of violence, approximately 30% of the perpetrators had consumed alcohol
Studies carried out by the emergency departments in numerous countries show that victims of violence are more often under the influence of alcohol than those injured accidentally, with higher levels of consumption and more significant alcohol-related problems. In 1994, the emergency departments in the United States received 1,400,000 victims of personal violence (i.e., 0.6% of the total population), only one of the parties involved (perpetrator or victim) having drunk in 13% of cases according to the information provided by this population.
A Canadian survey of victimisation published in 1991 and completed in the late 1980s of a representative sample of adults in an average-sized Ontario town is interesting because it focuses on the entire life of the persons included in the survey. It relates violent events, and the persons questioned were either the victims or the witnesses. 51% of the perpetrators and 30% of the victims had drunk at the time of the events. Alcohol was present not only during legally repressed acts of violence but also in minor acts of daily aggression. There appears to be a continuum between daily violence and major violence. These facts apply to the population as a whole and not to a specific group: 60% of men and 40% of women admit to having been victims, threatened, or witnesses of violence, and 10% of men and women have been victims of violence. The men were often victims during their youth, whereas women relate more recent events. Alcohol-related incidents did not result in more injuries than aggressive behaviour when alcohol was not present. Conversely, the risk of injury increases with the victim's alcohol consumption. The latter varies according to the sex of the perpetrator of the violence and the victim. Alcohol is involved in 62% of conflicts between male protagonists, in 53% of cases where the victim is a woman and the perpetrator a man, and in 27% of cases where the aggressor is a woman.
Based on victimisation surveys carried out among United States residents over 12 years of age, there were an estimated 11.1 million victims of violence every year between 1992 and 1995. These victims of violence represent 4.4% of the overall population 4 (250 million inhabitants). Simple aggression also includes verbal threats. A quarter of the victims of violence were certain that the perpetrator had been drinking.
Slightly less than one-third of perpetrators of non-sexual aggression would have drunk alcohol, either alone or in conjunction with other products, the latter being few and far between (4% to 7%). The perpetrators of violent rapes consume fewer psychotropic substances than other aggressors. In the case of sexual aggression, alcohol, either alone or combined with other drugs, is involved in 37% of cases. This figure is increased to 41% if sexual aggression committed under the influence of other drugs is included.
Regardless of the relationships between the protagonists, the use of alcohol is more widespread than that of drugs. The prevalence of alcohol increases with the proximity between protagonists. Aggressors who attack their partner have consumed alcohol on two occasions of three, either alone or in conjunction with other psychoactive products.
Table
Prevalence of consumption by the aggressor according to links with the victim – according to 7.7 million victims who are certain of the reports they have given (according to Greenfeld, 1998).
Those who attack their family members have been drinking in one of two cases. Those people who attack a relation, a friend, or an unknown person have consumed alcohol in approximately one of three cases, either alone or in conjunction with other psychoactive products.
In France in 1969, a one-month study focusing on sentenced offences in which at least one of the protagonists had chronic or acute alcohol consumption revealed a high prevalence of alcohol in homicides and arson.
Table
Prevalence of chronic or acute alcohol intake by the parties involved (perpetrators or victims) for certain groups of offences in France (according to Bombet, 1970).
In 2000, a national victimisation survey involving a representative sample of 7,000 women between 20 and 59 years of age analysed the violence to which they had been subjected over the previous 12 months. One-third of these 7,000 women declared themselves to be victims of “domestic violence” (perpetrated by a partner) and, in most cases, involved insults, emotional blackmail, and psychological pressure (30% of victims); physical or sexual aggression accounted for 3.4% of cases of violence. At least one of the protagonists had been drinking in 36% of the violent cases experienced—only the man in 27% of cases and the woman in 5% of cases. In the remaining 4% of cases, both had been drinking. The perpetrator had been drinking in 31% of the most serious cases of physical aggression.
Alcohol consumption affects social status: quality of study, type of employment, employee level
Various authors are interested in the impact of alcohol on social status in terms of employee level, personal and family income, and the job itself, based on data collated during American national studies.
Generally speaking, a positive correlation between alcohol and the level of income was found up to daily consumption of one glass of alcohol. This correlation changed, however, beyond 5 glasses a day. Some studies show that, in households with an alcohol problem, the average income is cut by 31% compared with other households. The relationship between consumption and personal income varies in the studies according to the duration of dependency or abuse for both men and women. Alcohol abuse and dependency cut income by 1% in the case of subjects between 18 and 24 years of age (men or women) and by up to 10% for those between 55 and 64 years of age, the impact being greater for women than for men.
The impact of alcohol use on work is also analysed in empirical studies. The difference between full-time employment in non-alcoholics and alcoholics is significant for men between 30 and 44 years of age and between 45 and 59 (88% versus 73% in the younger group and 86% versus 68% in the older group). According to some studies, alcohol consumption is associated with significantly more absenteeism.
Some studies have investigated the impact of alcohol consumption during youth on study level. The authors note that the early symptoms of alcohol consumption during youth are associated with a reduction in study level. Frequent consumption among students is manifested by an average reduction of 2.3 years in higher education. As regards the impact of alcohol problems on the choice of a job, the authors note that excessive drinkers are more often “blue-collar workers”. In the “white-collar” professions, excessive drinkers earn 15% less than their non-alcoholic peers. The indirect effects of consumption and the problems associated with this consumption can therefore be just as significant as the direct effects. More targeted research in this domain should provide information on the extent and nature of the indirect effects that can impact upon the quality and level of studies, training, the choice of a partner and friends, the level and quality of experience in the working context, and other components of human significance.
In France according to the Gazel survey (20,000 GDF-EDF employees), the major consumers (five glasses per day and above) are found more frequently among production staff (17.3%) and those working outdoors. Their consumption did, however, fall between 1992 and 1998 (–1.8 glasses). Abstainers and the heavy drinkers are those with poorer career prospects. Single, divorced, and separated men and men living alone consume three times more alcohol than married or remarried men. Men who have a poor perception of their health, or who take medication to sleep, consume more. A follow-up of re-treated persons shows that the number of glasses consumed weekly increased one year after retirement in all retired people (production staff, foremen, and executives).
The cost of loss of income associated with illness or premature death costs four times more than health expenditure
Analysis of the economic consequences associated with excessive alcohol consumption is an area of vast, fertile research (most of these publications nevertheless originating from Anglo-Saxon countries). The diversity of the potential effects of alcoholism on the economy in fact implies studies that exceed the strict framework of assessing the repercussions of the disease on the health of individuals. In addition to the costs of the disease, expenditure attributed to alcohol-related criminal offences and road-traffic accidents is also taken account in similar research.
Evaluation of the cost of alcohol consumption is based on the use of aetiological ratios and the documentation of the costs of consequences, health or otherwise, linked with alcohol consumption. Traditionally, a distinction is made between direct medical costs (recourse to treatments) or non-medical costs (criminal offences and road-traffic accidents) and indirect costs (loss of potential income or production associated with morbidity and /or premature mortality).
Studies carried out abroad highlight the significant financial impact of alcohol on hospitals and institutions. The cost of alcoholism and its repercussions was thus estimated at 148 billion dollars in 1992, in the United States.
Table
The social cost of alcoholism in the United States in 1992, in millions of dollars (according to Harwood et coll., 1998) .
This study, supported by several others, emphasises the importance of indirect costs to the overall cost. 47% and 21%, respectively, of this cost, are, in fact represented by loss of income associated with illness or premature death. Conversely, health expenditure amounts to only 8.9% of the overall cost.
Another important question for the economist is that of knowing who bears the costs generated by alcoholism. This refers to the notion of “external costs”. These are costs that abusers make non-abusers pay for. According to the studies, external costs predominate, the person responsible for the excessive consumption of alcohol or his/her partner covering only 45% of the cost of alcoholism and its consequences.
In France, several studies have been devoted to investigating the cost of alcoholism. One of the studies estimates the direct medical costs of alcoholism at 2.4 billion Euros in 1996. Another study exceeds the restrictive framework of analysing care and also includes, in addition to loss of income and production, expenses incurred by criminal offences and road-traffic accidents as well as loss of mandatory samples due to excessive alcohol consumption. The overall amount of losses attributable to alcohol is thus estimated at 17.6 billion Euros. Health costs represent 15% of this total, thus far behind the loss of income and production (50%) and the expenses that road-traffic accidents incur for insurance companies (20%).
These studies, conducted both in France and abroad, emphasise the heavy toll of alcoholism on society and the extent of indirect costs. Conversely, direct medical costs, which are mostly investigated, represent only 10% to 15% of the overall cost of alcoholism according to the studies. These studies also demonstrate the importance of carrying out sound, epidemiological studies to estimate the aetiological ratios of costs.
Approximately 15% of alcohol consumers present with a symptom of dependency
The tools used to assess the health of individuals and, consequently, populations, have changed considerably, and the International Disease Classification is in its tenth version (IDC-10). It is organised according to disease as a function of aetiological classes, anatomical classifications, and external causes of trauma. When applied to large populations, it can be used to investigate the factors that impact upon state of health and the reasons for involving the health services.
See heading F10–F19 completed by its subdivisions to distinguish products (F10 = alcohol) and symptoms to highlight the problems associated with the harmful uses of psychoactive substances.
Table
The fourth subdivision characteristic used in ICD-10 (after F followed by two figures) allows behaviour associated with the use of a psychoactive substance to be classified.
The specific literature referring to studies in the area of abuse and dependency involving psychoactive substances reveals the importance and diversity of measuring tools, using classification as the dominant approach. The main systems are the international classification systems (DSM-IV and ICD-10) used in psychiatry and general medicine where dependency is a psychopathological entity the same as abuse. The major American surveys use these tools. At the present time, public health requirements are in favour of internationally validated tools to facilitate comparison between treated populations and the assessment of the procedures implemented.
Table
Substance abuse according to the DSM-IV.
Table
Substance dependency according to DSM-IV.
The prevalence of alcohol abuse and dependency is estimated on the basis of studies conducted among the general population and for which the same methodological comments can be made as for the consumer studies: representative sample; concealed group; maintenance methods; nature of questions, risks of non-response that are added to the under-estimation of self-reported consumption.
The prevalence of alcohol abuse-dependency has been evaluated in major American national surveys: Epidemiologic Catchment Area (ECA), National Longitudinal Alcohol Epidemiologic Survey (NLAES), National Co-morbidity Survey (NCS), National Household Survey on Drug Abuse (NHSDA). The prevalence-life of alcohol dependency in a representative population of America, between 15 and 54 years of age, is estimated at 14% in the overall sample and 15% among consumers. 20% was recorded in men (21% of consumers) and 8% in women (9% among consumers). By way of comparison, in the same survey, the prevalence-life for dependency on smoking is 24% in the overall population and 32% among users.
In France, there is an obvious lack of major national survey with validated tools. Comparative groups are often described, but there are many biases in terms of selection, thus limiting extrapolation. According to the Baromètre santé 2000 data, 8.6% of people in the 12- to 75-year-old bracket are or have been at risk of excessive consumption (according to the DETA questionnaire): 13.3% of men and 4% of women. The highest prevalence is in the 45- to 54-years-of-age bracket. There is a link between the frequency of inebriation, smoking, and cannabis. There was no change in dependency (according to DETA) between 1992, 1995, and 2000 for those over 20 years of age.
Almost 40% of alcohol-dependent subjects present with another mental disorder
Major American surveys have also investigated the frequency of mental disorders and concomitant alcohol abuse or dependency. According to the Epidemiologic Catchment Area in 1990, among those individuals diagnosed as having a mental disorder (22.5% of prevalence-life in the population), the prevalence-life of a disorder associated with a psychoactive substance was 29% (including the overlap of 22% for alcohol and 15% for the other drugs). Conversely, in the case of subjects presenting with an alcohol-related disorder (13.5% of the population), the level of co-morbidity with another mental disorder was 37%. The highest level of co-morbidity was recorded in those presenting with another drug-related disorder (6% of the population): more than half (53%) of these presented with the concomitant diagnosis of mental disorder. The presence of a mental disorder is thus associated with a two-fold higher risk of having an alcohol-related disorder, and a four-fold higher risk of drug abuse.
Compared with the general population, the schizophrenic population is 3 times more prone to developing alcohol dependency and 6 times more prone to that of other drugs, the risk of dependency being 11 times greater in the bipolar population.
Among alcohol-dependent subjects, the prevalence of schizophrenia would be 3 to 4 times greater (6 times greater in abusers or those dependent on other drugs) than in the general population. The prevalence of bipolar disorder would be 5 times greater than in the general public. As regards antisocial personality, this is 20 times more frequent in alcohol abusers and alcohol-dependent subjects than in the general population. The probability of experiencing co-morbidity is multiplied by 4 for men and by 12 for women.
Table
Prevalence-life of abuse and dependency in the United States clinical population (according to the 1990 ECA survey).
Co-morbidity levels are thus particularly high in the case of severe mental disorders and substantially complicate the treatment. Patients with a dual diagnosis are just as often in the drug-addiction treatment system than in the mental health system.
Some temperamental traits are indicative of excessive alcohol consumption
The predictive models or excessive alcohol consumption highlight three factors:
- the search for sensations
- the age at which the patient first consumed alcohol
- resistance to alcohol-mediated effects
Primary alcoholism refers to all the forms of alcoholic behaviour representing the first disorder experienced in the subject. The onset of associated psychiatric disorders, after the onset of alcoholism, suggests that these disorders should be considered secondary to alcohol habits. Secondary alcoholism implies the co-existence of alcohol-related behaviour and psychiatric disorders, regardless of type, before the onset of alcohol abuse or alcohol-related independence. Psychiatric disorders in cases of secondary alcoholism occur regardless of the alcoholism and are present especially during prolonged withdrawal periods.
Alcoholic behaviour truly secondary to a psychiatric disorder is relatively rare apart from alcoholism secondary to mania, depression in women, or a social phobia. The existence of an untreated, concomitant psychiatric disorder (with depression or anxiety) is mostly pejorative to changes in alcoholic behaviour.
This has, for instance, been demonstrated for depression. The presence of depression secondary to alcoholism accentuates family rifts. Moreover, the alcoholic's depression potentiates the risk of suicide and perpetuates dependency (alcohol used in the self-medication of depression), thus inhibiting any therapeutic approach undertaken (lack of motivation, negative interactions of anti-depressive therapies and alcohol).
The American psychologist, Marvin Zuckerman, developed the “search for sensations” concept and adapted this to alcoholism. In 1964, he perfected a specific scale known as the “Search for Sensations Scale”. This was a self-questionnaire that could be used to evaluate the frequency and severity of searches for stimulation. The four principal factors on which this scale is based are: the search for danger and adventure, the search for experiences, disinhibition, and susceptibility to boredom.
The tendency to search for new things and sensation has been linked, like extroversion, to a low level of basic cerebral activity. Those “seeking sensations” could thus attempt to raise their level of interaction and cerebral vigilance through new and complex experiences.
Studies carried out using this questionnaire have highlighted the particularly high frequency of this series of characteristics in the most impulsive alcoholics and in patients presenting with other dependency behaviour. Studies involving the general population and notably pupils at French lycées (equivalent of UK secondary schools) have allowed a correlation to be established between the scores obtained on the Zuckermann scale and the average consumption of drugs or alcohol. More specifically, the amount of alcohol consumed by boys is correlated with the “search for danger and adventure” and “disinhibition” factors and, in girls, with one single factor, namely “disinhibition”. Sensation-seeking is thus one of the key trigger factors for early alcohol consumption, especially in younger subjects. Correlated with disinhibition, impulsiveness, and intolerance to frustration, sensation-seeking could represent a fundamental aspect of the personality of certain alcoholics, inciting them to repeated toxic experiences. Zuckerman summarised the links between alcoholism and sensation-seeking as follows: “An initial, so-called experimental period seems to be strongly motivated by sensation-seeking in all its behavioural guises and especially susceptibility to boredom, disinhibition and the search for experiences7rdquo;. The later period corresponding to the onset of dependency is triggered less by sensation-seeking than by adaptive needs with regard to anxiety associated with withdrawal, stress, and family problems secondary to alcohol dependency.
Over the last 20 years, psychiatrist Marc Schuckit, who specialises in alcohol-related problems, has demonstrated the impact of alcohol resistance in the risk of dependency. His work focused on the sons of alcoholics (students between 18 and 25 years of age) at the start of the survey. They consumed alcohol without being dependent upon it. Susceptibility to alcohol was investigated in a standardised manner. The subjective effects of alcohol consumption were quantified using a scale analysing sensations of euphoria, intoxication, drowsiness, hesitation, and nausea. The psychomotor effects of alcohol were also evaluated in a standardised manner. The authors followed up these sons of alcoholics for more than 10 years. They noted a very strong correlation between resistance to the effects of alcohol observed at the start of the study 10 years earlier and the risk of becoming an alcoholic. A low level of response to alcohol consumption (resistance to the mental effects of alcohol) at the age of 20 was associated 10 years later with a 4-fold greater risk of dependency. Among the children of alcohol-dependent subjects, who were resistant to the mental effects of alcohol consumption, 56% became dependent compared with only 14% in the group of subjects deemed to be “susceptible” to the effects of alcohol. This resistance was not accompanied by an enhanced risk of other psychiatric diseases or dependency on illegal drugs (drug addiction).
Predisposition to alcoholism in alcohol-resistant subjects also involves social factors. Those subjects who, in society, display optimum alcohol “resistance” undoubtedly tend to drink more to enter a state of inebriation comparable to that of their peers. “Alcohol-resistant” subjects are not warned of the extent of their consumption by behavioural signals such as drowsiness or motor instability.
There is an interaction between environmental and genetic factors in the process of alcohol dependency
The possibility of a genetic origin of alcohol dependency dates back many years, and in 1972, Schuckit showed that the children of dependent subjects presented the same dependency as their parents, regardless of whether or not they were raised within their biological families.
Familial studies conducted worldwide have, in fact, highlighted a varying resemblance between relatives in terms of alcohol-related problems. According to the recent data obtained in the Collaborative study on the genetics of alcoholism, the prevalence of abuse or dependency involving a psychoactive substance in the close relatives of alcohol-dependent subjects was 44%. Amongst these, 80% presented with alcohol abuse or dependency. The risk of alcohol dependency in relatives is greater when the subject is dependent on alcohol rather than on another substance.
The studies of twins consist in comparing the degree of resemblance between monozygous twins and dizygous twins in terms of alcohol abuse and dependency. Numerous studies performed in varying geographical locations reveal greater concordance for monozygous twins compared with dizygous twins with regard to alcohol abuse and dependency. The genetic influence appeared to be more important in the first study with male, alcohol-dependent twins.
Fewer studies have been carried out on the genetic epidemiology of alcohol abuse and alcoholic dependency in sample populations of adopted individuals, and the data obtained are less reliable. The studies suggest a link between the characteristics of dependency in the biological father and that of the son adopted by other parents. These results confirm the hypothesis that genetic factors are transmitted from father to son. The results of studies carried out in women differ to a greater extent. All of these studies focusing on families, twins, and adoption tend to show that alcoholism, which is etiologically complex, is partly hereditary. This inheritance is estimated to be between 40% and 60% in men.
Progress is still needed to analyse the role of crucial genetic and environmental factors in alcohol consumption. Studies involving twins and focusing on alcohol consumption are generally all heading virtually in the same direction. Monozygous twins are more similar than dizygous twins in terms of alcohol consumption. The convergence of results points to a genetic influence in alcohol consumption. Some studies carried out in adolescent twins and their parents have facilitated analysis of the respective impact of genetic inheritance and the environment on alcohol consumption. These studies have demonstrated the influence of the family environment in the use of alcohol in adolescents between 15 and 16 years of age. This parental influence does not, however, exist in older adolescents. The crucial genetic factors thus take precedence over environmental parameters.
The environment can promote the development of abuse and dependency in genetically predisposed subjects. The testing of these predisposing genetic factors has become a key component for understanding the aetiology of the disease on the one hand, and for identifying varying expressions of dependency on the other hand.
The phenotyping of dependency is based on the classification criteria nowadays defined in the DSM-IV. In genetic studies, it is, in fact, extremely important to homogenise groups of individuals and therefore to possess tools that are as objective as possible to identify the disease phenotype.
Furthermore, an understanding of the processes of reward underlying dependency has allowed neurotransmission systems sensitive to psychoactive substances and involved in the acquisition and maintenance of dependence to be identified. This has triggered research into candidate genes likely to be involved in the aetiology of alcohol dependence. The principal mediators involved in dependency are dopamine, opiates, serotonin, and GABA (gamma-aminobutyric acid). This list is certainly far from exhaustive but has paved the way for research into candidate genes.
Particular attention has focused on the dopamine D2 receptor gene located on chromosome 11 since the early 1990s. The implication of the dopaminergic system in regulating the reward systems justified this research. The results, however, differ considerably in terms of the association between the presence of the A1 allele of receptor D2 and dependency. The recent findings of the Collaborative study on the genetics of alcoholism clearly show that there is no link between two polymorphisms investigated of the D2 receptor gene and alcohol dependency.
Other systems have been investigated to establish if they represented risk factors or highlighted dependency. One German study confirmed the significantly high frequency of the presence of the polymorphism of the transporter gene of serotonin (5-HTT) (short allele) in dependent patients relating to the control group, but the Collaborative study on the genetics of alcoholism does not corroborate this finding. The latter has reported a modest link between dependency and the presence of the muted allele of the type μ opiate receptor (OPRM), only in the Caucasian population. Two German teams did not discover any link with this polymorphism.
Finally, the uncontested role of the GABAergic system not only in susceptibility to alcohol but also in withdrawal has justified genetic studies in dependent subjects. The findings of these studies are modest. A relationship between the presence of a muted allele of the α6 subunit of the GABAA receptor and alcohol dependency has been demonstrated in a group of patients presenting with anti-social personalities. Moreover, a Scottish study revealed a significant association between the presence of muted alleles of several subunits (α6, β2, and γ2) involved in regulating alcohol tolerance, mainly in patients presenting with Korsakoff syndrome.
Although these results appear deceiving compared with expectations, they nevertheless confirm that alcohol dependency is a complex, multifactorial disease. The link between the functioning of a single gene or single system with the phenotype of dependency cannot be envisaged. The genetic factor appears to be an additional risk factor in the dynamic interaction with environmental factors.
This begs the question as to whether, in addition to alcohol consumption, other dependency-related phenotypes exist and whether these can be inherited.
A specific wave of cortical electrical activity, namely wave P300, is defined by its amplitude and time of onset, which are characteristic of and specific to every individual. The profile of this wave can be inherited, and its amplitude has been seen to be weak in dependent patients and their descendants. The features of the EEG tracings of alcoholic patients appear to be reliable tools for highlighting dependency. Their specificity is all the more marked because recent studies have shown that the frequency of cortical waves was associated with the presence of the α2 subunit of the GABAA receptor. The expression of the α2 subunit gene reflects activation of the central nervous system in which GABAA receptors would act as a pacemaker. The phenotypical identification of these waves corresponds to the highlighting of a genetic locus. For the first time, in the light of these studies, a correlation can be made between a tool used to highlight dependency and gene expression.
Although the test for the specific genetic mutations of alcohol dependency is significant when implementing identification tools, it must not be forgotten that the lack of specificity highlighted by the studies can also reveal the existence of an aetiological community between all forms of dependency on the one hand and between alcohol dependency and other behavioural disorders on the other hand. Co-morbidity between alcohol dependency and other mental disorders could reflect the sharing of the same genetic heritage.
The expression of enzyme genes involved in alcohol metabolism may affect alcohol dependency. Two systems control alcohol metabolism: alcohol dehydrogenase (ADH), which metabolises alcohol into acetaldehyde; and aldehyde dehydrogenase (ALDH), which converts the toxic intermediate, acetaldehyde, into acetate.
Approximately half of the Asian population presents with functional polymorphisms of genes ADH2, ADH3, and ALDH2. The mutant allele, ALDH2*2, reduces the activity of the ALDH2 liver enzyme triggering somatic disorders such as nausea, palpitations, and facial flushes during alcohol consumption. The high frequency of homozygous ALDH2*1 individuals in dependent Asian populations could imply that the ALDH2*2 allele protects against dependency. This allele is, however, very rare in non-Asians (Caucasians). Various studies carried out in specific populations suggest that the presence of muted alleles could constitute a protection in the form of behavioural avoidance of the deleterious effects of acetaldehyde. Thus, the carriers of muted alleles who avoid alcohol would therefore be less prone to developing dependency.
Based on current knowledge, it is not, therefore, feasible to make a distinct correlation between alcohol dependency and one or more genetic mutation(s) among the systems studied. New areas of research should focus on environmental factors that influence the expression of different genes, thus promoting an understanding of the mechanisms of individual susceptibility to alcohol and developing new tools for highlighting and evaluating the risk of dependency. The tools used for genetic analysis should also be adapted in line with the polygenic characteristics of the variations observed.
In animals, forced dependency modifies certain receptors and disrupts neurotransmitter balance
There is no animal model that incorporates all of the neurobiological and behavioural characteristics of alcoholism in humans. Nevertheless, our knowledge of several components of alcoholism is based on animal models. In fact, there are “active research” alcohol models that have been genetically defined or which are based on behaviour acquired through conditioning.
Thus, by gradually selecting the animals, several research teams have obtained lines of rodents preferring to drink an aqueous alcoholic solution instead of water alone. These lines (UchA and UchB for the Chilean strain, A and ANA for the Finnish strain, P and NP for an American strain, for example) indicate the genetic basis of preference toward alcohol. These lines of rats, genetically selected for their preference for alcohol, nevertheless vary in terms of a series of important characteristics which separate and enhance preference, namely: the initial susceptibility to alcohol, the level of anxiety, basic cerebral neurotransmitter level. These results therefore suggest that the various genotypes control the preference for alcohol and that the contribution of each one varies according to the lines selected.
Preference for alcohol can also be obtained by learning, with the animal self-administering an increasingly high quantity of alcohol. Procedures such as alcohol deprivation following access ad libitum, the ingestion of a low dose of alcohol or even the onset of a stressful situation are techniques that motivate and temporarily enhance predilection for alcohol. Moreover, these procedures can accumulate. Stress and a low dose of alcohol, for instance, will subsequently trigger a higher alcohol intake.
The environment can also be used to assess the appealing or repulsive impact of repeated alcohol administration. Generally speaking, in rodents, no dose level of alcohol triggers an appeal for the environment in question, whereas an increasing dose of alcohol triggers greater corresponding repulsion.
In the alcohol preference model, regardless of whether this is genetically selected, acquired through learning, or environmentally conditioned, alcohol consumption does not exceed the limits of enzymatic oxidation in the species study, i.e., around 7g/kg/day of alcohol in the laboratory rodent. Animal experiments have corroborated the link between two characteristics for defining alcohol consumption rather than for defining dependency simply by the presence of tangible signs of withdrawal on discontinuing alcohol. Both these characteristics show a marked preference for alcohol if the animal has a choice between alcohol and water on the one hand, and, on the other hand, alcohol consumption exceeding the oxidation capacity of the species. Naturally, even in genetically selected rodents, these two characteristics are not encountered at the same time. For this, forced dependency must be established, and alcohol administration via inhalation seems to be a reliable and reproducible method for achieving this. These forced dependency techniques have clearly shown the involvement of an amino acid derivative, GABA. Moreover, the structure of the GABAA receptor is modified by alcohol under conditions of forced alcohol consumption. Among the psychoactive substances, those having this same GABAA receptor as a target, as in the case of barbiturates and benzodiazepines, are associated with the sedative and anxiolytic effects of alcohol by sharing the same characteristics of euphoria, disinhibition, sedation, and reduced anxiety.
Although alcohol does not possess a specific receptor in the central nervous system, the changes to several subunits of the GABAA receptor will trigger concomitant adaptation of neuroexcitatory transmission by enhancing this, chiefly via glutamate and its NMDA receptor. While alcohol is present, this cerebral balance will be maintained. However, because metabolic and nervous tolerance is rapidly instituted, the dose levels of alcohol must be increased to maintain this balance. During withdrawal, the brain is in a state of hypofunctioning in terms of inhibitor amino acid receptors and reactional hyperfunctioning of excitatory amino acid receptors. This state is perceived as very unpleasant. A significant drop in intracerebral dopamine is also observed, inducing what is known as “anhedonia” (total loss of feeling of pleasure). In all animal models, alcohol is the best means (immediate and effective) for both erasing the physical signs of withdrawal and detecting the positive reinforcement, i.e., its appeal during withdrawal and prolonged abstinence. Withdrawal is perceived as a stressful moment, and a neuropeptide, CRF (corticotropin releasing factor), is thus activated in the central nucleus of the amygdala. This CRF significantly increases anxiety and can be blocked by the infusion of specific antagonists into the amygdala. This neuropeptide is a key factor in the behavioural response to withdrawal-induced, undesirable emotions. Moreover, repeated withdrawal with intermittent alcohol consumption results in a cerebral “kindling” effect, characterised by hyperstimulation of NMDA receptors in conjunction with a marked alteration in the subunits of the GABAA receptor, making treatment increasingly difficult and hazardous. These results demonstrate the ability of alcohol to trigger progressive, functional adaptations in the brain during chronic alcohol consumption but especially during repeated withdrawal.
In fact, animal tests show that initial dependency reduces the following thresholds for acquiring dependence: the animals undergoing repeated withdrawal with repeated introduction of alcohol present with increasingly accentuated withdrawal symptoms. These studies suggest that frequent “alcoholic experiences” trigger a series of increasingly marked alterations. These prolonged neuroadaptive changes must be better understood and corroborated through more extensive research.
In animals, variations in emotional reactivity influence alcohol consumption
The relationship between stress and alcohol consumption raises several questions. Is there a link between the individual characteristics of stress-induced reactivity and alcohol consumption? Do stressful situations influence alcohol consumption? Does alcohol influence the response to stress? What is the role of dopaminergic systems, which are both highly reactive to stress and involved in the positive reinforcement process?
Reference should initially be made to the difficulty in defining emotional reactivity in animals. The multi-faceted models developed by psychologists in humans are still scarcely used in experimental psychology, and the results obtained in the various tests, even if they are supposed to reflect the same aspect of reactivity, are difficult to compare. On the other hand, all of the experimental results concern consumption studies without taking the possible existence of vulnerability to dependency into account. Finally, the marked sensitivity of experimental results, both in the definition of reactivity profiles and in measurements of alcohol consumption, to test procedures and environmental factors that are well controlled to a varying degree, compound the characterisation of stable “traits” specific to animals in relation to variations dependent upon environmental conditions.
The relationships between emotional reactivity and alcohol consumption have been analysed by investigating individual correlations in heterogeneous animal populations or by comparing strains selected either for their varying alcohol consumption or for behavioural reactivity criteria. Generally speaking, the strains spontaneously consuming the most alcohol have a reduced level of emotional reactivity (excluding any alcoholic saturation).
Rather coherent results highlight the relationship between sensitivity to gustatory reinforcements (sweet taste of saccharin or the bitter taste of quinine) and alcohol consumption. This relationship has been demonstrated both in humans and in laboratory animals. It can be used to characterise a process of dependency in animals spontaneously consuming large quantities of alcohol. The simultaneous presentation of highly appetising solutions will reduce alcohol consumption all the less in animals that have developed a more pronounced dependency. These data draw attention to the importance of taking the following into account in the analysis: individual differences in alcohol consumption and reinforcement factors of gustatory origin compared with direct effects on the central nervous system.
The influence of stress hormones, and of glucocorticosteroids in particular, on addictive substance consumption has been clearly established. Some of their effects involve action on the dopaminergic system, which contains numerous receptors to these hormones. Individual differences in neuroendocrine reactivity can thus underlie the various vulnerabilities to the development of addiction. The best-documented example is that of Lewis and Fischer 344 strains of rats highlighting major differences in terms of activity/reactivity of the corticotropic axis and a propensity to develop the consumption of addictive substances. The link between these two characteristics has not, however, been corroborated, and molecular mechanisms have yet to be explored.
Like stress, alcohol activates the corticotropic axis in a dose-dependent manner, and the response is gradually attenuated during repeated administration, whereas the response to restrictive stress is not altered. This phenomenon is reminiscent of the process of functional tolerance, which has been thoroughly investigated in terms of the behavioural effects of alcohol. In the long term, alcohol consumption reduces the activity and reactivity of the corticotropic axis in humans, and this can continue for a long time after withdrawal. In return, the glucocorticosteroid hormones can influence alcohol consumption.
Several studies show that alcohol consumption is influenced to a considerable extent by social status, animals in a submissive position consuming greater quantities of alcohol. The isolation of animals previously reared in a group also increases alcohol consumption. Apart from their interest in highlighting those factors influencing spontaneous alcohol consumption, these studies also provide important information for defining conditions for the testing and breeding of laboratory animals, which must be borne in mind in order to interpret the published results.
Much of the literature focuses on the effect of all types of unpleasant stimuli on alcohol consumption, although no precise information is given. The effects observed (decrease or increase) depend, among other things, on the type of stimulus, the time of application in relation to the consumption test, and probably other experimental conditions that have not been identified. In all cases, the intensity of the effect of stress is limited without measuring against interindividual variations of genetic origin, for example.
The dopaminergic systems are a target for the pharmacological action of abused drugs and are often considered to be the principal neurobiological support of their reinforcing properties. These same systems are involved in the reinforcing properties of natural stimuli such as feeding, drinking, and sexual activity. These neurochemical systems are also activated by stress and unpleasant stimulations. They therefore play a specific role in research into addictology.
Intraperitoneal administration of alcohol to the rat activates dopamine (and serotonin) release measured by in vivo microdialysis in the accumbens nucleus, but this effect remains variable and limited. It is apparent only after administration of the highest dose levels (1 and 2 g/kg), and the action of the alcohol does not differ significantly between strains of rats selected for their preference to alcohol (HAD/LAD or AA/ANA). Conversely, a similar study conducted in Lewis (consumers) and Fischer 344 (non-consumers) rats showed that the Lewis rat is entirely resistant to alcohol on dopamine release. In another series of selected strains, the effect of alcohol on the tissue concentrations of dopamine metabolites (which constitute a system activation index) was more marked in the strain with a predilection for alcohol (sP) than in the abstinent strain (sNP). These results tend to show that the dopamine-releasing ability of alcohol is not directly associated with spontaneous preference.
On the other hand, several studies conducted in mice and rats have shown that animals consuming more alcohol presented with lower concentrations of dopamine, its metabolites, and its receptors. These results are consistent with the hypothesis of the existence of a “hedonic system” involving dopamine, the hypoactivity of which would be a risk factor vis-à-vis the consumption of substances activating this system.
However, numerous experimental data tend to limit the importance of the dopaminergic system in the physiopathology of alcohol-related behaviour. The lesion of dopaminergic neurones of the ventral section of skin or of the accumbens nucleus via a specific neurotoxin (6OHDA) does not affect alcohol consumption or its intravenous self-administration, although certain authors indicated a decrease or increase in consumption. The reactivity of dopaminergic neurones tested by the intensity of the locomotor response to amphetamine is more marked in alcohol-consuming rats than in abstinent Wistar rats that can be distinguished by their spontaneous alcohol consumption. These rats are also more reactive at low doses of apomorphine, a dopaminergic stimulant. The alcohol-consuming rats of selected strains that have not had previous contact with alcohol have also proved more reactive to amphetamine than abstinent strains. The susceptibility of dopaminergic neurones after repeated administration of cocaine does not affect alcohol consumption.
All of these experimental data recorded in rodents highlight the complexity of individual factors and environmental factors likely to influence alcohol consumption. Although the existence of significant variations of genetic origin has been confirmed—even if the molecular mechanisms are still unknown—the influence of environmental factors and individual variations in emotional reactivity are still poorly defined. These data reveal the importance of breeding and testing conditions, which must be taken into account when developing a heuristic study model. Moreover, it should be noted that the vast majority of these studies concern alcohol consumption without the onset of dependency being taken into account.
In humans, questionnaires and biological markers can be used to assess the problems associated with alcohol consumption
A certain number of tools are available to healthcare professionals to enable them to broach the subject of alcohol consumption and its potential repercussions. In fact, in view of the medical, psychological, social, and family consequences of alcohol misuse, it is vitally important that the risks incurred and the damage caused be detected and assessed in consumers. It is a well known fact that many professionals find it difficult to engage in discussion on alcohol consumption. The use of validated tools may, therefore, prove useful. A distinction can be made between two types of tools: questionnaires and the assay of biological markers. Among these questionnaires, the declared alcohol consumption, the AUDIT questionnaire (Alcohol use disorders test) and the DETA questionnaire (Diminuer, Entourage, Trop, Alcool )—the French translation (version) of the "CAGE" (Cut down, annoyed, guilty, eye-opener) questionnaire—have proven their efficacy. The declared alcohol consumption can be used to estimate the statistical risks taken by the subject in terms of consumption. It is important that this declared consumption assesses the quantity of alcohol consumed, the frequency of consumption, and the circumstances under which alcohol is consumed.
The AUDIT questionnaire investigates the last 12 months in a person's life. The items have been compiled especially to highlight people whose consumption habits put them at risk of causing future damage in terms of both physical and mental health, and those subjects whose consumption profile has already triggered problems. The AUDIT questionnaire was validated in both the general population and specific groups (road-accident prevention, young people, pregnant women, and patients presenting with mental disorders, etc.). AUDIT therefore appears to be a relevant questionnaire for identifying subjects whose alcohol consumption poses a risk with susceptibility ranging from 51% to 97% and specificity from 78% to 96%.
The DETA comprises four questions resolutely targeted toward research into alcohol misuse and exploring the subject's entire life. It is more adapted to detecting disorders associated with the use of alcohol (abuse or dependency) with a sensitivity of 43% to 94% and specificity ranging from 70% to 97%. It does not appear to perform as well as AUDIT in detecting alcohol consumption posing a risk in the general population. In particular, reduced sensitivity in terms of its potential to screen alcohol-related problems in adolescents has been reported by several authors. The latter are investigating the need to develop specific questionnaires targeted at adolescents and young people.
The regulations governing use, which have been put forward by the NIAAA (National Institute on Alcohol Abuse and Alcoholism) in the United States and by the WHO (World Health Organisation) as regards safety standards for daily and weekly consumption rates (not more than 4 glasses for men and 2 glasses for women per day and not more than 5 days a week) cannot be applied to all groups. In some cases, it is the situation and not the quantity that is all-important. In pregnant women, patients suffering from viral hepatitis (C in particular), children and adolescents, the subject receiving specific treatment, the alcohol-dependent person, etc., the safety standard is abstinence.
Although the AUDIT and DETA questionnaires have been formulated to identify those people misusing alcohol (to identify patients presenting with risk-related consumption in the first instance, and those presenting with abuse or dependency in the second instance), it should be noted that in no way are these diagnostic tools.
The assay of biological markers indicative of alcohol consumption poses the problem of the usage context in particular. In fact, the intention to use the results is an essential precursor to interpretation.
Recent alcohol consumption can be detected by assaying ethanol in the biological fluids (blood, urine, expired air, and saliva) using enzymatic or chromatographic methods. Clinically, ethanol is assayed via enzymatic methods, these methods being rapid, automated, and reliable. In a forensic context (road traffic, autopsies), gas-phase chromatography with flame ionisation detection (GPC/FID) has been the official method since 1986 and the international reference.
In the general population, the markers of chronic alcohol consumption are less relevant than the questionnaires to highlight and trigger a help relationship with persons experiencing alcohol-related difficulties. On the other hand, their use in alcohol-related management, especially as motivational feedback, is of current, relevant usage. On the other hand, these markers are of certain interest in assessing the damage induced by consumption when these are markers of alcohol-related disease. However, the biological markers are not, in any way, the only markers of dependency.
Table
Biological markers of substantial alcohol consumption (according to Allen and Litten, 2001).
GGT measurements combined with MCV are frequently used in France and enhances screening efficacy compared with a single marker. Other composite scores are proposed, such as G-CDT, comprising the results of the CDT and GGT and the EDAC (Early detection of alcohol consumption score), which is based on the regrouping and data processing of 36 current biological assay constants usually modified by alcohol consumption. Other markers are being researched at the present time: assay of adducts formed between acetaldehyde and serum proteins; assay of circulating, anti-adduct antibodies; acetaldehyde haemoglobin assay (HbAch); blood acetate assay; assay of mitochondrial aspartate aminotransferase (ASTm); hyaluronic acid assay; and the assay of 5-hydroxytryptophol and beta-hexosaminidase.
The tools proposed are, above all, tools that must be integrated in a management procedure as an element for the initial evaluation of a situation and as an element for assessing changes in that situation.
The general practitioner plays a key role in the screening and management of patients with alcohol-related problems.
Every year, general practitioners are in contact with 75% of the French population and therefore play a crucial role in the identification of patients presenting with an alcohol-related problem. Many studies have highlighted the merits of early screening, which allows simple, codified advice to be systematically given for reducing the alcohol-related risk within the context of secondary prevention.
However, the role of prevention and screening in general medicine is scarcely recognised, if at all, by the public authorities. General practitioners perceive the therapeutic management of patients as a long, drawn-out process with often partial, seldom definitive results.
Brief interventions (averaging 5 minutes) have been validated in individuals most often identified in general medicine. Although they address all categories of users (use involving risk, harmful use, use with dependency), their efficacy has nevertheless been shown, chiefly in subjects associated with use involving risk and harmful use, without alcohol dependency.
The very general principle of brief intervention is to provide the subject at risk with good advice, the long-term effect of which should enable him/her to bring about a lasting change in his/her attitude toward alcohol.
The structure of brief interventions varies considerably. The common denominator is to adopt a cognitive-behavioural approach, which makes the patient the key player in his change, although discussions are held at the carer's initiative. A brief intervention usually comprises :
- an evaluation of the subject's relationship with alcohol (AUDIT)
- information relating to the acute and chronic effects of alcohol consumption on health
- recommendations based on cautious thresholds after having expressed rationality
- suggestions of various tactics aimed at reducing alcohol consumption
- accentuation of the patient's role in this alcohol-reducing strategy
The tools of intervention (information booklet, brochure, and self-questionnaire) are available in French ("Boire moins c'est mieux"—drink less—it's better ), drafted in collaboration with INPES (formerly CFES), Anpa, and the sickness insurance funds.
Randomised evaluation studies involving various groups have highlighted the consistent efficacy of these approaches, especially in women, as well as efficacy in terms of cost-benefit and cost-efficacy.
Within the scope of the Eureca opinion poll (European network on strategies to engage general practitioners in cancer prevention) carried out in five countries (Belgium, Spain, France, Italy, and Portugal), the involvement of general practitioners in the screening and prevention of dependencies (smoking, alcohol) has been assessed.
Table
Results of the Eureca poll.
In France, this survey has shown that doctors have certainly incorporated the action of primary prevention in their daily practice, even though they are more at ease in cancer screening.
The best technique for contacting patients with alcohol-related problems for early interventions was explored within the scope of the international Strand study (Alcohol and health: some preventive measures and some early interventions). In France, this study was carried out by the Association pour le développement et la recherche en médecine générale de Nantes (ADERMG; association for the development and research of general medicine in Nantes). Even if two of three doctors involved in the study considered alcohol to be a genuine public health problem, general practitioners, overall, are still very reticent to broach the subject of alcohol consumption. In a liberal system, the patient is the practitioner's “client” and an approach toward the “alcohol” problem may trigger conflict between the patient/carer.
According to the data collected in the survey conducted by the Observatoire de la médecine générale de la Société française de médecine générale (1994–1995; observatory of general medicine of the French society for general medicine), 76% of doctors used the term “alcoholism” and 24% never used it in the compilation of consultation results. “Alcoholism” ranked 56th among the consultation results, taking all age brackets into account (the first 25 places corresponded to 50% of the activity). This blind spot in terms of perception and/or use has been confirmed by other studies, whereas the prevalence of disorders associated with established alcohol consumption in France in general medicine is 20%.
These three studies show that general practitioners have integrated prevention and screening in their daily practice, although the alcohol-related risk is underestimated. Rationalisation and suitable tools (data-processing of medical dossiers, advisory documents for patients and the AUDIT test) are essential in order to obtain far-reaching results. The general practitioners request information on this subject as well as official recognition in their screening and preventive role.
Less than 20% of people presenting with alcohol dependency seek professional advice within an average of 10 years after the initial symptoms.
The morbid model of alcohol dependency can be assimilated to an acquired, multi-faceted behavioural disorder developing over a variable timescale in favour of vulnerability factors currently being identified. The generally chronic advance of this adaptive disorder throughout a person's entire life is marked by alternating periods of activity and remission. The therapeutic strategies are aimed at promoting the implementation and maintenance of sequences for extinguishing the process of pathological alcohol-consumption over prolonged periods. Authentication in the biographies of alcohol-dependent subjects of so-called “spontaneous” remissions because they do not follow on from a specific intervention has introduced the concept of “natural cure”, which has yet to be confirmed by longitudinal, long-term stability studies. The performance (generally deemed mediocre) of therapeutic interventions aimed at altering the course of alcohol dependency must be confronted not only with the lack of interventions (this is the case in randomised studies) but also with the frequency of spontaneous involution of the morbid process.
To be considered in “natural” remission, an alcohol-dependent subject must not have presented with the DSM-IV criteria of alcohol dependency for more than 1 year (American psychiatric association, 1994). The “natural” or “spontaneous” character of this remission is determined by the absence of any specific therapeutic intervention, i.e., implication in a programme of outpatient or residential care or any psychotherapeutic assistance involving a professional. Participation in a self-help group is recognised by some authors as virtually complete treatment and yet by others as an absence of treatment.
The level of “spontaneous” remissions is estimated as being of the order of 4% per year. The predictive factors essentially associated with a significant improvement (abstinence) are the severity of the disorder, good social insertion and life-changing events. Spontaneous remissions are more often associated with the lack of social pressure and a fear of the onset of bodily damage in women rather than men. In 15%to 25% of cases, a partial improvement is associated with a return to controlled consumption, the main predictive factors of which are the existence of a moderate form of pathological alcohol consumption and a good level of social function.
Long-term mortality observed in alcohol-dependent subjects identified in the general population cohorts is 3 to 5 times that calculated in theory in non-alcohol-dependent subjects.
Recourse to a therapeutic aid is generally rare and delayed in alcohol-dependent subjects. Fewer than 20% of them seek professional advice over a period averaging 10 years after the onset of symptoms. The decision to integrate a care programme and inclusion on a waiting list can alone trigger stable abstinence in 11% of cases, thus validating the efficacy of a motivational factor that is difficult to evaluate. Although most therapeutic projects offered to alcohol-dependent subjects propose long-term (several months) accompaniment, the retention level in care programmes remains low, often making it difficult to assess their efficacy beyond 6 months. Several longitudinal follow-up studies of long-term (>5 years) alcohol-dependent patients during withdrawal (generally in hospital) witness an improvement in consumption criteria generally classed according to three levels: total abstinence, partial improvement (damage-free consumption), and failure. “Continuous” abstinence (>5 years) is generally stable and can be considered virtually definitive because fewer than 5% of these abstinent subjects resume consumption within the following 5 years. The level of these stable remissions increases with age and remains higher in patients presenting with severe factors of alcohol dependence prior to treatment.
Rare prospective studies have compared the change in alcohol-dependent subjects depending on whether or not they have been treated. The level of abstinence was twice as high and the incidence of consumption twice as low, without diagnosing misuse, in treated patients compared with non-treated patients.
On the other hand, the persistence of misuse criteria was higher among the treated patients, thus suggesting a more severe disease. However, all types of treatment improved the prognosis of abstinence with particular efficacy for groups of former drinkers.
Table
Comparison of sociodemographical data and variables relating to the consumption of alcohol and drugs in alcohol-dependent subjects with or without periods of abstinence (according to Schuckit et al., 1997).
Thus, if the chronic nature of alcohol dependency has been established by follow-up studies showing that the process of pathological alcohol consumption is spontaneously stable, triggering overmortality, it is inaccurate to consider the prognosis of affected subjects as being unfavourable overall. Spontaneous remissions that can be assimilated to an extinction of the process of pathological alcohol consumption (implementation of continuous abstinence or a return to controlled consumption) are possible without recourse to a therapeutic aid for patients with a generally less severe condition. In the severest of cases, treatment, regardless of type, sometimes improves the spontaneous advance in the long term (>10 years) by reducing the mortality.
Table
Outcome at 5 years of 4,585 adults presenting with DSM-IV criteria of misuse (abuse or dependency), depending on whether they have been treated (according to Dawson, 1996).
Regardless of the severity of the alcohol-related disease, all patients can benefit from a therapeutic approach.
The multi-faceted aetiology of alcohol dependency triggers a wide range of clinical pictures, which, in itself, is responsible for the variation in the responses to the therapeutic strategies uniformly applied to a patient population. Post-treatment follow-up studies tend to highlight factors pertaining to success and failures, taking into account the severity indices of the disease, which are assumed, often incorrectly, to indicate an unfavourable prognosis.
Prospective surveys have revealed a difference in the prognosis of abstinence following treatment administered to men and women. In fact, it appears that the crucial factors for abstinence or failure vary according to gender; men seem to be more aware, for instance, of preserving a married life in order to remain abstinent, whereas women react far more to preoccupations regarding the somatic complications of the alcoholic disease to incite themselves not to drink again. Marital status prior to treatment appears overall as a factor for good prognosis, while the socio-educational level has only a variable impact on prognosis in studies with divided results; a low educational level cannot, therefore, be taken as a predictive factor for failure. Advancing age is a predictive factor for abstinence provided that the duration of active alcohol dependency (prior to withdrawal) without recourse to treatment is prolonged (greater than 10 years). Unemployment is a failure factor, especially if it occurs during the post-withdrawal period. The combination of these sociodemographic factors in a model comprising age, male gender, stable employment, and no prior hospital stay does not, however, forecast treatment success after 6 months.
Cognitive predispositions, such as the sentiment of auto-efficacy, low expectations, the positive effects of alcohol consumption, or self affirmation, are validated, predictive factors in several studies. These mental dimensions are generally reinforced during abstinence by promoting its maintenance.
The presence of concomitant disorders, regardless of any causal relationship with alcohol dependency, often has a pejorative effect on any changes in this parameter after withdrawal. In fact, they disrupt an effective treatment procedure or steer it toward strategies that do not modify, first and foremost, the attitude toward pathological alcohol consumption per se. If the frequently related psychiatric disorders (anxiety and depression) make it difficult to preserve abstinence, they nevertheless seem to have a negative impact on female prognosis more often than in men. The presence of an antisocial personality disorder is a failure factor that is found in most studies; however, the existence of legal complications (penalties), which are often associated in this respect, would promote continued abstinence. The presence of severe alcohol-related disease, such as pancreatitis, cirrhosis, or polyneuritis of the lower limbs, will affect the prognosis to varying degree. The subgroup of patients presenting with severe, alcohol-induced cirrhosis and having benefited from a liver transplant, nevertheless presents particularly high, long-term abstinence levels associated with a rapid and significant improvement in their quality of life. The latter alone can play a motivational role in maintaining abstinence. Lastly, the presence of another form of dependency to a psychoactive substance is a pejorative predictive factor in advance, by reducing treatment compliance. Nicotine dependency, which is very common among alcohol-dependent subjects, cannot be considered as a failure factor because the few studies aimed at comparing the outcome of abstinence in smokers and non-smokers give contradictory results.
The relationships of a subject with his/her family, social or professional environment were reasonably well studied to identify the factors influencing the prognosis. More generally, investment in social activities is a good prognostic factor, which sometimes resists confrontation with other personal factors in the analysis of logistic regression. Conversely, isolation is a factor that promotes premature failure and a high failure rate, delaying the return to a carer. The support of the partner or of one or more members of the family during psychotherapy, administered in conjunction with patient management, is a factor that limits the risk of failure. However, a meta-analysis of the studies assessing the influence of social relations on the prognosis of abstinence concludes a weak, inconstant determinism.
Biological vulnerability to alcohol dependency and to probable genetic determinism would be responsible for the extremely variable effects in terms of the frequency and intensity of wanting to drink in alcohol-dependent populations. The considerable desire to drink before treatment is a poor prognostic factor in patients not treated by substances to curb the appetite.
The intensity of the neuropsychic effects of alcohol consumption and the fantastical investment that patients have in facilitating functions (e.g., disinhibition, anxiolysis, potentiation of sexual desire) are important factors in failure. They could be mediated by the specific sensitivity of the hypothalamo-hypophyseal axis, the opioid system, and dopaminergic salting in the limbic system. Premature alcohol dependency with a marked genetic component (Cloninger type II) appears to present a less favourable prognosis in two prospective studies than environment-associated alcohol dependency (Cloninger type I). Nevertheless the higher frequency of an antisocial personality, dependency on opiates, and indices potentiated by severity constitute three astounding factors that do not allow this subtype to be identified as a failure factor. The presence of genetic polymorphisms could be associated with the severity of the dependency.
Therapeutic interventions have a globally positive effect, although considered as weak in heterogeneous populations of alcohol-dependent subjects. Prospective studies investigating the predictive factors of failure have not been able to identify stable personal, environmental, or biological factors allowing a valid model of “poor responders” to therapeutic strategies identifiable on the basis of certain criteria to be constructed. However, the factors detected on an inconstant basis are often factors highlighting the severity of the disease or a deficiency in factors associated with success, such as the lack of favourable environment or predisposition to change (motivation). Consequently, a therapeutic project from which seriously affected patients can benefit should never be renounced.
Two compounds have nowadays proved their efficacy in promoting post-withdrawal abstinence.
The development of knowledge in the understanding of the neurobiological mechanisms of alcohol dependency has allowed the efficacy of certain molecules acting more specifically on the neuroaminergic systems involved to be demonstrated in both animals and humans. The assessment criteria most often used are: alcohol consumption, the number of subjects remaining abstinent throughout the study, the failure rate or the length of time prior to failure. The results available from randomised trials comparing these compounds against a placebo have been included in the meta-analyses.
Acamprosate, a homotaurine synthesis calcium derivative, is a compound similar to taurine, which is a GABA receptor antagonist. GABA is involved with other neuroamines in the physiopathology of alcohol dependency in the central nervous system, and its role is apparently to modulate and inhibit catecholaminergic routes. Despite the advances made in recent studies, the mechanism of action of acamprosate does not appear to have been completely elucidated. Its activity in reducing alcohol consumption is based on inhibition of neuronal hyperexcitability associated with stimulant amino acids (especially glutamate) on NMDA receptors, or on reducing the functionality of calcium channels. Positive results have been obtained during treatment periods and prolonged follow-up (≥1 year) and in combination with disulfirame. The side effects (moderate and transient) are chiefly gastrointestinal (dose-dependent diarrhea, abdominal pain, and nausea). Recommendation of acamprosate in the treatment of psychological alcohol dependency appears to be justified according to marketing authorisation recommendations. Recent data suggest that the neuroprotection of the compound during the withdrawal period would warrant the initiation of treatment even before consumption had stopped. Lastly, the compilation of results obtained in various studies shows that 4 to 6 patients of 10 treated patients benefit from treatment in terms of promoting abstinence. The characteristics of the subgroup of responding patients have not been identified to date.
Naltrexone, a specific opiate receptor antagonist, reduces the traits of alcohol preference in animals. Initially, two randomised studies versus placebo demonstrated the efficacy of this product in terms of improving the abstinence level after 12 weeks of follow-up and reducing by two the failure rate in subjects who had renewed consumption of at least one glass. In the event of resuming alcohol consumption, the treated patients experienced a reduction in the positive craving effects, which limits the risk of returning to excessive consumption. This diminished alcohol-related euphoria seems to be more marked in alcohol-dependent patients with an initially high desire to drink. Naltrexone also seems to reduce the effect of waiting for positive sensations of alcohol consumption described as a predictive failure factor. A meta-analysis of randomised studies has highlighted a globally positive effect with acceptable heterogeneity for the criterion of reducing the failure rate. The results are less favourable for the criterion of alcohol consumption expressed in days of alcohol intake. The quality of treatment compliance is discussed especially because it seems to condition its efficacy. The paucity of studies confirming the efficacy of the compound on longer periods (≥6 months) has thus far limited the marketing authorisation in France to 3 months and still does not enable the optimal theoretical duration of treatment to be determined. The most frequently reported side effect (5% to 15%, depending on the study) is nausea at the beginning of treatment. This is associated with an inactive metabolite and tends to be more frequent in women, young subjects, and those consuming low quantities of alcohol.
Other compounds are promising. Gamma-hydroxybutyric acid, which possesses similar characteristics to a neurotransmitter, reduces voluntary alcohol intake by various mechanisms and withdrawal symptoms in both rats and humans. Although recent studies suggest its efficacy in promoting abstinence and its tolerance in the treatment of alcohol-dependent subjects, its use as a “street drug” is particularly worrying and curtails its development. Ondansetron is a serotoninergic 5-HT3 receptor antagonist used as an anti-emetic during anti-cancer chemotherapy. Initial studies in the rat indicate its ability to reduce the craving to drink. Two randomised studies conducted in humans highlight short-term (6 weeks) and mid-term (12 weeks) efficacy. The interest of this compound in this particular indication has yet to be seen.
Thus, among the many compounds tested in promoting post-withdrawal abstinence, only two, acamprosate and naltrexone, have nowadays proven their efficacy. A comparison of the efficacy of both these compounds and the benefits of their concomitant administration are currently being assessed.
Psychotherapy has proved beneficial for alcohol-dependent patients.
The psychosocial approach is considered to be the principal therapeutic strategy for alcohol dependency, and numerous psychotherapeutic techniques have been put forward. Few of them can be modelled sufficiently well to suggest an evaluation approach within the scope of randomised trials. Supporting psychotherapies, motivational therapies, behavioural and cognitive therapies, and the movements of former drinkers have been assessed.
The purpose of motivational therapy is to accompany the alcohol-dependent patient in the process of modifying his/her behaviour by incorporating the subject and enabling him/her to go through the various stages of change, as proposed in the Prochaska and DiClemente model. In a randomised study comparing this approach with a series of 20 meetings with groups of former drinkers (e.g., Alcoholics Anonymous) and with 12 sessions of cognitive and behavioural therapies, motivational therapy proved just as effective as the other two strategies in promoting abstinence and was far less costly. Highly resistant patients opposing the care programme had the better prognosis.
Among the many types of cognitive and behavioural therapy (CBT) proposed for alcohol-dependent subjects to modify their approach via procedures emphasising desensitisation and positive reinforcement, the failure prevention model established by Monti is the most widely used. During a cycle of collective sessions, the patient learns to recognise the principal situations in which failure may occur and to overcome these by acquiring, through role-playing, appropriate behavioural responses to prevent a return to alcohol consumption. The individual evaluation of these methods is complicated by the simultaneous use of several techniques within complex protocols. However, it seems that they are more effective in abusers than in alcohol-dependent subjects. Lastly, a recent analysis of 26 studies suggests that efficacy would be better in less severely affected patients involved in a structured treatment programme. These methods present an acceptable cost/benefit ratio.
Marital and family therapies take into account the fact that alcohol dependency often has an adverse effect on marital relations. Involvement of the partner or management of the couple might improve treatment compliance. In terms of families, the inter-relationships between an alcoholic and his/her family are generally complex. The ambivalent and often contradictory feelings of the family can be expressed during family therapy, the efficacy of which in promoting abstinence has been confirmed in two randomised trials.
There are about 10 or so “cured drinkers” associations in France that coexist alongside Alcoholics Anonymous, who introduced this therapeutic model. Attempts at evaluating this therapy have encountered two major methodological obstacles, namely the problem of finding a genuine control group and gauging attendance due to the “anonymous” nature of the meetings. In a large-scale, North American study comparing this type of approach with minimal (motivational) or behavioural therapies, sessions inspired by the Alcoholics Anonymous programme were deemed comparable in terms of efficacy to behavioural psychotherapies in subjects with a low level of opposition and resistance. Until a subgroup of patients more receptive to this type of management is identified, associations must be proposed to every alcohol-dependent subject (routine issuing of contact numbers), despite the lack of precise efficacy-related data.
It has thus been shown that psychotherapies are beneficial to alcohol-dependent patients. Motivational therapies can be applied at an early stage to allow the patient to undertake his/her treatment. Family management can prove useful in cases of dysfunction. Cognitive and behavioural therapies are justified and established during withdrawal.
Combine an aetiological trait with a specific therapeutic strategy to boost efficacy
The crucial aetiological factors of alcohol dependency in a given individual are divided among three groups of factors: cultural and environmental; biological and genetic; and mental and psychopathological. The relative weight of each of these groups of factors varies from one subject to the next and determines the extremely variable type, expression, and advance of the alcohol-related disease. The application of a “standard treatment” to a heterogeneous group of patients with a disease of varying aetiology highlights a global deficit in terms of efficacy for want of reaching the predominant target. The concept of “adapted crossover” tends to link an aetiological trait with a specific strategy to boost efficacy. A few attempts are opening up interesting research channels.
The inconsistency of individual responses to medicinal treatment and the craving to drink suggest the presence of genetic factors that predispose their efficacy through sensitivity to the neurobiological target. It has thus been shown that patients carrying the A1 allele of DRD2 (second gene of the dopamine receptor) were more sensitive to the efficacy of a dopaminergic agonist (bromocriptine) than homozygous patients for the A2 allele, in whom treatment was, on the whole, ineffective. The identification of a variety of responses to naltrexone, according to the subtypes of opiate receptors, would probably modify the efficacy profile of this compound in this indication. Evidence of such agreement paves the way to a choice of strategies.
Recommendations
The expert summary of the published data covers a very wide field, including the various contexts of alcohol usage, changes in consumption habits, and the social, economic, and health-related consequences of excessive alcohol consumption. Several trends can be identified, based on current knowledge.
In France, global alcohol consumption has fallen by almost 40% in 40 years, and the consumption of wine has also decreased by 40%, but over a period of 20 years. Wine consumption, nevertheless, largely predominants because 65% of people over the age of 65 drink wine on a daily basis. Consumption habits are very different in young people. They drink beer and spirits more so than wine and tend to do so on weekends, in a celebratory context. They frequently mix their drinks and become inebriated. Studies show that, the earlier alcohol consumption begins, the greater the risk of regular consumption. In a working environment, alcohol consumption, which is often associated with certain habits that develop only at a very slow pace, is still responsible for 10% to 20% of accidents. These accidents are, however, less frequent that alcohol-induced road-traffic accidents, which cause approximately 1,900 deaths each year. Alcohol is also involved in domestic accidents and acts of violence. Excessive alcohol consumption has a high social cost: the loss of income due to disease or premature death is four times higher than health costs.
Over 2 million people in France are estimated to have symptoms of dependency, and almost 40% of these present with another mental disorder. Sensation-seeking, the early onset of consumption, and resistance to the subjective effects of alcohol are three factors for predicting abuse and dependency. Although the genetic component of dependency cannot be contested, the interaction between genetic disposition and familial and social environmental factors is nevertheless crucial in the development of a dependency syndrome. Research into predisposing genetic factors is a long and arduous task with this complex, multi-faceted disease. Significant comorbidity between dependency and other psychiatric disorders could also reflect the same genetic component. Animal models have proved interesting for promoting the understanding of neurobiological mechanisms underlying the phenomena of dependency, tolerance, and sensitisation, and for investigating the impact of various stimuli, especially stress, on the consumption level.
The management of patients presenting with an alcohol-related problem is still limited today because fewer than 20% of these people seek medical advice over an average period of 10 years from the onset of the initial symptoms. The treatments have, however, elicited a certain, albeit modest, response. Thanks to advances in medical research, it will probably be possible in the future to adapt treatment to the profile of each individual patient to optimise efficacy.
The intervention of public authorities bears testimony to the increasing interest attached to the health and social aspects of excessive alcohol consumption. Within the scope of the public health code, three circulars (1970, 1975, 1983) outline the specialist mechanisms for preventing and treating alcohol-related diseases, thus clearly demonstrating that this falls within the State remit. The drink code (training, accessibility of drinks, protection of minors, regulation of alcohol-promoting advertising) has been modified and completed on several occasions since its introduction in 1915 and is nowadays an integral part of the public health code. The Évin Law in itself has conveyed an important public health message. As part of the process to harmonise European legislation, France opted for an authorised blood alcohol limit of 0.5 gram per litre in the blood for drivers of road vehicles. A blood alcohol level of 0.5 g/l to 0.8 g/l contravenes the law, and a level equal to or greater than 0.8 g/l constitutes a criminal offence. Despite these measures, drunk driving nevertheless remains a major cause of road-traffic accidents. In recent years, several campaigns have been launched at the initiative of the Road Safety authorities to encourage drivers to assess their blood alcohol levels and, more recently, to promote the “ideal driver” (one who doesn't drink).
Several campaigns to prevent excessive alcohol consumption have been devised by the Comité français d'éducation pour la santé (French health education committee) “Un verre ça va, trois verres bonjour les dégâts” (one glass is fine, three glasses is asking for trouble). Some of these are directed at young adolescents (“Tu t'es vu quand t'as bu?” (Have you seen yourself when you've had a drink?)), whereas others have been developed in conjunction with CNAMTS (“Et vous avec l'alcool, vous en êtes où?” (Where does alcohol get you?)) and the MILDT (“Drogues, savoir plus risquer moins” (Drugs: more knowledge, less risk)). In 2001, the national programme strategy was streamlined according to the results of the collective expert report on the effects of alcohol consumption on health (published in 2001), the aim being to provide the general public with scientifically validated information. A new campaign (“L'alcool, pas besoin d'être ivre pour en mourir” (Alcohol - you don't have to be drunk to die from it)) is scheduled and is intended, among other things, to make people understand that inebriation/drunkenness is not the only form of excessive consumption.
Further to the analysis and summary of published data relating to this second collective expert report on alcohol, the experts put forward recommendations for public health strategies to consolidate the existing prevention and management approach. The experts also propose research in several directions to promote the knowledge and understanding of risks, especially in young people, of the impact of concealed advertising, the mechanisms underlying excessive consumption, and the phenomenon of resistance to alcohol in particular, and lastly, of evaluating essential screening tools.
To regulate, inform, and form
to reconstruct a consistent framework comprising regulation, information, and prevention
For more than a decade, legislators have wanted to regulate advertising for alcohol. In France, the Évin Law of 10 January 1991 laid the basis for prohibiting direct or indirect publicity and the sponsorship of alcoholic drinks by manufacturers. However, this prohibition principle has been flouted on numerous occasions since then, partly voiding this particular law. In its current format, the law authorises advertising only via certain media and under certain conditions. The content of the advertising messages is restrictive in theory and must be reduced to informative messages. The expert group, however, considers that the use of graphics, pictures, and photographs is emphasising the product, taking it beyond the boundaries of information. Moreover, the alcohol industry employs marketing strategies, such as promotions or distribution of free samples at student gatherings, attempting to promote alcohol consumption by depicting actors in films or magazines. The expert group recommends stricter application of the law to prohibit such practices and possibly the creation of a watchdog commission.
to inform via targeted health campaigns
As regards prevention through general public communication campaigns, research on the impact of messages has shown that health messages are perceived and accepted much more readily when they are issued from a source that is appreciated by the spectator. The campaigns that are best received by young people are those that involve people whom they feel close to and can identify with (DJs, athletes, leaders, singers and actors, etc.). The best remembered advertisements are those with the most popular band sounds, especially those that play well-known music and songs. The group of experts recommends that the public authorities take these various aspects into account when designing campaigns intended for the general public.
Educational approaches to prevent the consumption of psychoactive substances including alcohol by young people must not be limited to information about the products and their effects. Targeted information on the short-term consequences of switching from experimental to regular consumption should be given, as well as information on the risks of abusive consumption. This information must provide accurate data relating to the prevalence of alcohol abuse to correct the exaggerated perceptions that young people often have about peer group consumption, and to highlight the differences between male/female consumption. According to the expert group, the educational/preventive strategy should also take into account the differences between boys and girls, in terms of usage context and consumption level, and should be based on promoting the physical and mental health of young people by improving their individual skills (with regard to stress, anxiety, inhibitions associated with social relations, and violence) using programmes that include the entire family.
Individual and collective preventive measures must follow within the framework of occupational medicine: staff should be informed of the risks associated with alcohol by involving approved organisations, forming link groups within the company by involving different players (representatives from the following sectors: staffing, trade unions, hygiene committee, safety and conditions of work, human resources directorate, and medico-social department) and, in small companies by appointing someone to assist with alcohol-related problems. Numerous experiments to boost awareness can help to change the way people think (alcohol-free day, action in company restaurants, alcohol-free drinks parties, etc.) within establishments. The expert group recommends that such actions be extended and perpetuated so as to ensure their long-term success. The group encourages the setting up of a charter to reflect internal regulations and the code of practice regarding alcohol consumption in the workplace, which has already been implemented in some large companies.
to promote the initial and continuous training of all professionals involved in health education, prevention, and in the management of people experiencing alcohol-related problems
All professionals involved in prevention—general practitioners, work doctors, school doctors and nurses, social workers, educationalists as well as magistrates, the police, and driving school instructors—should receive relationship training, enabling them to deal with people who are likely to have an alcohol-related problem. The expert group recommends setting up a continuous training system, culminating in the awarding of a diploma.
General practitioners come into contact with 75% of the French population during the course of one year and should therefore be experienced in identifying people with an alcohol-related problem or alcohol abuse or dependency. Surveys show that GPs are often reticent to broach the subject of alcohol consumption. They require training in this matter. As part of a medical study reform procedure, the expert group recommends that transversal modules be introduced, specialising in training in alcohol-related subjects, along with the creation of a university addictology subsidiary.
Patients usually seek medical advice for two reasons on average, leaving little time for discussions focusing on screening and prevention. So that patients can attend consultations focusing solely on screening and prevention, the general practitioner must receive official recognition in this domain together with financial compensation. The expert group wants the public authorities to find a swift, technical solution to the matter of financial remuneration (introduction in the nomenclature of a key letter, “prevention”, another means of remuneration).
Screen and prevent
to define a coherent framework for road safety intervention
Of all the persons breathalysed at the side of the road after an accident, over 6% of drivers have a blood alcohol level exceeding 0.5 g/l. In the event of a fatal accident, a blood alcohol level greater than 0.5 g/l is recorded in 30% of cases. The expert group recommends that French drivers be constantly informed of the effects of alcohol on driving and of the legal implications of having excess alcohol in the blood when behind the wheel. The alcohol consumption of passengers and pedestrians is not curbed by the law except in the case of public drunkenness resulting in death/injuries.
Various approaches can reduce alcohol-related road risks for young people. These include planning the evening ahead, before any alcohol is consumed, and appointing someone to drive home. The driver should ideally abstain from drinking alcohol. This type of behaviour should be emphasised, and the actions of associations working in this domain highlighted. It is also interesting to encourage establishments (nightclubs and bars, etc.) to train bar staff to assume more responsibility in their work. It would also be important for the public authorities to consider the cost (and tax implications) of non-alcoholic drinks in order to make them more attractively priced for consumers and distributors. Within the scope of departmental action plans relating to road safety (PDASR), the group of experts recommends promoting various practices to reduce road-related risks for young people, particularly with regard to organisation of group transport. Driving schools could be involved more extensively in disseminating information on the risks associated with driving under the influence of alcohol.
to encourage the development of self-assessment methods to determine alcohol abuse
Given the medical, psychological, social, and familial consequences of alcohol abuse, it is extremely important to screen and assess the relevance of the risks involved and of the damage sustained by consumers. The expert group recommends that every alcohol consumer be given an opportunity to assess his/her consumption level, the risks involved, and the potential damage that this may cause. To this end, self-questionnaires could be distributed in the doctor's clinic, in the clinic at work, and in various public places (social security centres, post offices and stations, etc.).
Pregnant women with a alcohol-related problem rarely ask spontaneously for assistance from the doctors who are monitoring their condition. Healthcare professionals, therefore, play a crucial role in identifying pregnant women who consume alcohol. The group of experts recommends that alcohol consumption be routinely mentioned at antenatal examinations and that questionnaires (declared consumption, AUDIT, and DETA) be used (until questionnaires relating specifically to pregnant women are produced). Laboratory markers (GGT – gamma-glutamyltransferase, MCV – mean corpuscular volume) should be used to direct the conversation to alcohol consumption.
Furthermore, blood alcohol levels should be routinely tested for every person attending the accident and emergency department due to an accident sustained at work, in the home, or when relaxing.
to introduce specific assistance and evaluation programmes for populations that are particularly predisposed to alcohol abuse or dependency
Among the people diagnosed with mental disorders (22.5% of life-prevalence in the population), almost 30% are dependent on a psychoactive substance. The knowledge of mental disorders, particularly mood swings, anxiety, schizophrenia, and personality disorders in adults and behavioural problems in youngsters must lead to a thorough investigation of the consumption of psychoactive substances, especially alcohol. The expert group advocates the systematic screening of alcohol consumption in patients suffering from mental disorders or in polyconsumers. Patients receiving opiate replacement therapy must be screened in particular for alcohol consumption.
The prevalence of dependency is, on average, higher in children of alcohol-dependent parents. The expert group recommends that the children of parents receiving specialist treatment for an alcohol-related problem and children exposed to alcohol during the intra-uterine period be monitored very closely.
Certain temperamental traits, such as sensation-seeking or impulsiveness, can be factors that trigger initial alcohol consumption, especially in young subjects. The expert group recommends that professionals coming into contact with young people (school doctors, work doctors and social workers, etc.) pay particular attention to persons presenting with these vulnerability factors, and especially young people who are repeatedly inebriated. Girls do not become drunk as often, but the link between repeated inebriation and regular alcohol consumption is higher in girls than in boys.
Studies have shown that the risk of dependency is higher after a few years of alcohol consumption in subjects initially presenting with good resistance to the mental and psychomotor effects of alcohol. The expert group wishes to point out to healthcare professionals that some people who are less susceptible (resistance) to the subjective effects of alcohol will be particularly vulnerable to alcohol abuse and dependency. This insensitivity may be detected through self-evaluation questionnaires.
Patient management
to define an intervention strategy depending on the severity of the disease
Before taking charge of a patient, it is essential that the severity and grade of the condition be established as well as his/her incentive to stop alcohol consumption. It is, in fact, pointless to institute treatment if the patient has not decided to help himself/herself. In terms of the evaluation, the carer, taking into account all of the relevant medical and social parameters, can propose an intervention strategy in keeping with the disease profile.
In the case of patients presenting with severe dependency and concomitant psychiatric disorders and other somatic and social diseases, the expert group recommends setting up a network of specialists. Outpatient or residential withdrawal must be proposed for such patients. During the post-withdrawal period, the medication and/or psychotherapy administered must be aimed at maintaining abstinence. The form of psychotherapy can be chosen through discussion or left to the patient (psychodynamic approach, cognitive-behavioural, systemic, etc.). In the extreme cases of patients who are dangerous to themselves and to others, the group recommends specific measures (guardianship) and hospitalisation in a psychiatric ward (SHRT: specialist hospitalisation at the request of a third-party).
In cases of dependent patients with no severe, psychiatric concomitant disease, the group of experts recommends treatment by an alcohologist in conjunction with the treating general practitioner for outpatient withdrawal in an attempt to stop the patient from consuming alcohol or to reduce his/her intake. Motivational psychotherapy can be undertaken by the general practitioner in the form of counselling during sessions held at varying intervals.
Numerous studies have confirmed the medical and economic benefit of short-term interventions involving brief, standardised counselling sessions with the principal physician for those individuals whose alcohol consumption exposes them to significant risk. This approach can prevent injury but can also have a curative effect on injuries/damage already sustained.
to facilitate access to care
Alcohol dependency is a treatable condition. Studies show that therapeutic interventions have an overall positive effect, even if the latter is considered to be weak in certain alcohol-dependent populations. Therapy should, therefore, always be proposed, even for severely affected patients, who may benefit from such an approach. The expert group recommends that the results of patient treatment studies be circulated to doctors in order to emphasise the work of the carers and to promote the image of proven efficacy in the treatment of alcohol dependency. First and foremost, however, any doctor taking charge of a patient must inform him/her of the nature of his/her condition.
Given the fact that, at the present time, only 20% of alcohol-dependent people are treated, the expert group considers that priority should be given to providing these patients with access to care via a 100% management approach. The group also draws attention to the marked correlation between disorders associated with alcohol consumption and the risk of contamination with the AIDS virus and hepatitis B and C. Finally, the expert group recommends that specific management networks should be set up for adolescents, young people, and pregnant women.
The expert group recommends that an appropriate management strategy be implemented for any inebriated patient attending the accident/emergency unit (the majority of whom are alcohol-dependent). This involves at least equipping the accident/emergency wards with an ethyl meter and a room where subjects can sober up. Blood alcohol levels must be measured on discharge; otherwise the hospital will be liable if the patient is still under the influence of alcohol. If not all the emergency departments can be equipped, the facilities available to these crisis patients must be improved.
to motivate care institutions to develop an area of therapeutic excellence in addition to their mission to get to the root of the problem
The multifactorial aetiology of alcohol dependence generates a wide range of clinical pictures. This fact, in itself, causes considerable variation in terms of patient response to the therapeutic strategies usually applied. To date, prospective studies have not highlighted stable personal, environmental, or biological factors to individualise treatments or boost their efficacy. The expert group therefore recommends the development of clinical trials in order to link an aetiological trait with a therapeutic strategy. Given the number of people potentially affected, this recommendation should become a clinical research priority in France.
Psychotherapy before or after withdrawal has proved useful in alcohol-dependent patients. Motivational treatments must be applied at an early stage, enabling patients to undergo treatment. Family management may prove useful in the event of dysfunction. Cognitive and behavioural therapies are justified and highlighted during withdrawal. There is, however, a distinct lack of establishments offering these psychotherapeutic options in France. According to the expert group, centres of excellence should be developed for various types of specialist care strategies where patients could receive the form of psychotherapy best suited to his/her profile.
To develop research
to develop research into risks and driving
American, Canadian, and Australian studies have demonstrated the preventive efficacy of lowering the legal blood alcohol level for a few years for newly qualified drivers. The recommendations vary from one country to the next: maximum legal limit of 0 or 0.2 g/l of blood, applicable for 1 to 3 years for newly qualified drivers. The group of experts recommends that these recent experiments be taken into account. They also suggest that a study be carried out to assess the potential impact in France of lowering the maximum legal blood alcohol levels for the first few years after passing a driving test. A legal level of 0 or 0.2 g/l is more prohibitive than a slight drop because it suggests a link between alcohol abstinence and driving.
When they have been drinking, most drivers are more afraid of being arrested than of having an accident. However, numerous factors (sex, sociocultural origin, the experience of the driver, his/her lifestyle and alcohol consumption habits, etc.) affect behaviour. The expert group recommends investigating, via an interdisciplinary approach, the various perceptions that French and European drivers have of the alcohol risk associated with driving. These studies should promote understanding of why and how repressive action may be effective.
Longitudinal studies have highlighted the link between precocious premature onset of alcohol consumption and alcohol-related accidents. The data are, however, still inconclusive with regard to risk factors and protective factors concerning the attitudes and behaviour of young drivers. The expert group recommends studying the context of alcohol consumption in young people and researching the correlation between age of onset of consumption with subsequent driving problems.
Driving under the influence of alcohol, traditionally considered as an accident precursor, is now considered a sign of alcohol dependency. In fact, an illegal blood alcohol level is very often indicative of an alcohol-related problem. Access to care via motivation or a legal obligation appears to engage patients in a voluntary cure procedure. These studies are, nevertheless, limited or foreign. According to the expert group, a study should be carried out to assess the efficacy of identifying patients among people charged for repeated offences in France and of their medical and psychological treatment.
to produce a summary of all the studies relating to the social uses of alcohol
Social science research into alcohol consumption is extensive, fragmented but unrelated. Furthermore, France lags behind somewhat in terms of the history and anthropology of the social uses of alcohol. These deficits result in an underevaluation of all the social factors associated with alcohol consumption. The expert group recommends promoting research aimed at summarising dormant historical, geographical, and ethnological data focusing on “social drinking” in France and at identifying the shortfalls in terms of scientific design before considering limited studies.
Consumption habits have changed in young people according to the way in which people celebrate (several celebrations in succession; travelling by car; consumption of several psychoactive substances; loud, musical atmosphere, etc.), which differ considerably from those described in the 19th century. The expert group recommends investigating what really lies behind this reworking of the contemporary youthful celebration scene in order to convey prevention messages in keeping with the new drinking habits.
to investigate the impact of clandestine advertising
Although alcoholic beverages cannot be advertised in many countries, advertisements nevertheless draw attention to the traditional venues associated with excess drinking (bars and discotheques) when publicising soft drinks (alcohol-free beers, alcohol-free aperitifs and mineral waters, etc.) and also portray famous actors renowned for their overindulgence. The expert group recommends that the impact of this form of advertising, which highlights inebriation instead of portraying alcohol, be investigated, particularly in the promotion of alcohol-free drinks.
In young people's programmes, the action often takes place in cafés, pubs, and cafeterias. Similarly, in children's fiction, we frequently read about sorcerers conjuring up magical cocktails to make people more powerful or more intelligent. The expert group recommends an investigation as to how forms of clandestine publicity can be incorporated in television series and video games, which are extremely popular with young people.
to validate questionnaires for screening and diagnostic purposes in various populations
A certain number of questionnaires are available to healthcare professionals to enable them to broach the subject of alcohol consumption and its potential impact. AUDIT, for instance, seems to be relevant for identifying subjects presenting with a risky alcohol consumption. DETA (four questions) appears to be more suitable for detecting abuse and dependency. The latter was used in France within the scope of the Baromètre health survey to estimate the prevalence of alcohol dependency.
Apart from these general evaluation and screening questionnaires, specific questionnaires should be adapted for certain populations, such as pregnant women and adolescents. These questionnaires, such as T-AC (Tolerance, annoy, cut-down, eye opener) and TWEAK used to screen risk-related, alcohol-induced behaviour in pregnant women, have not been translated or, a fortiori, validated in France. The expert group recommends investigating the validation and circulation of such tools among care-givers in France.
The abuse and dependency criteria could differ in adolescents and young adults from those observed in adults, which are defined by DSM-IV. According to the expert group, the suitability of existing tools for assessing adolescents and young adults should be investigated.
to study the mechanisms underlying increased consumption in animal models
Research in laboratory animals is aimed at understanding the vulnerability factors and mechanisms underlying increased alcohol consumption, with or without dependency.
Numerous strains of rats and mice were selected on various phenotypes in relation to alcohol consumption (voluntary consumption, sleeping time and tolerance, etc.). These phenotypes are influenced by a large number of genes. The genetic approaches must be adapted to this multigenic characteristic. Reference can be made in particular to research on QTL quantitative trait loci or methods for screening genes that are differentially expressed between animal strains contrasting for the trait(s) investigated.
Based on current knowledge, it is not possible to make a distinct correlation between alcohol dependency and one or more genetic mutations among the systems studied. The mechanisms traditionally considered as being involved in alcohol-induced vulnerability involve the dopaminergic, serotoninergic, and opioidergic systems. The expert group recommends investigating in particular the process of rapid adaptation of the central nervous system to the effects of alcohol. Clinical studies have shown that the rapidity of this process can predict the onset of dependency.
to study the interactions between the various factors
Certain environmental factors are likely to play a crucial role, particularly when they manifest at an early stage during the development of the individual, during the fœtal and neonatal periods. Among these factors, particular emphasis is paid to the adverse environmental effects generally referred to as “stress”, early alcohol consumption and the influence of other psychoactive substances (nicotine, tetrahydrocannabinol—or cannabis, 3,4-methylene-dioxymethamphetamine—or ecstasy, etc.).
The relationship between emotional reactivity (temperament) and alcohol consumption can be investigated in animals in order to detect the psychobiological parameters likely to influence vulnerability, be it spontaneous or induced.
The expert group recommends that the various factors (genetic, environmental, behavioural reactivity) involved in vulnerability be analysed in interaction in order to consider the multi-faceted aetiology. A co-ordinated approach to the various factors warrants the setting up of research networks between laboratories possessing complementary expertise. The expert group suggests that long-term, research-promoting structures be created involving several disciplines such as biomedical sciences and human and social sciences in the clinical and experimental research field.
Footnotes
- 1
Telephone survey conducted after random selection of subscribers.
- 2
Survey conducted by means of an anonymous questionnaire on a typical population of schoolchildren.
- 3
"Health and consumption" survey conducted by means of an anonymous questionnaire completed during a "Journée d'Appel de Préparation à la Défense" (defence preparation seminar).
- 4
If the number of victims 12 years of age and under are arbitrarily removed.