Clinic Exam: Interview, Physical Exam, ECG, Original Cohort Exam 29: Protocol
Clinic Exam: Interview, Physical Exam, ECG, Original Cohort Exam 29: Protocol
Framingham Phenotypic Identifier: e_exam_ex29_0_0210s
Table of Contents
- Section I General Information
- Section II Informed Consent & Tracking Procedures
- Section III Clinical Measurements & Procedures
- Section IV Tech-Administered Questionnaires
- Section V Physician-Administered Medical History
- Section VI Offsite Examination
- Section VII Appendix
Section I. General Information
1. Exam Components -- clinic and offsite
Cohort Exam 29 Clinic Components
- Section I: Informed Consent & Tracking Procedures
- Informed Consent
- Waiver of Informed Consent
- HIPAA-Release of Health Information for Research Purpose
- FHS Follow-up by Proxy
- Tracking Information Form (Salmon Sheet)
- Section II: Clinical Measurements & Procedures
- Anthropometrics
- Height
- Weight
- Blood Pressure
- Observed Physical Performance
- Handgrip
- Chair Stands
- Balance
- Timed Walk
- Anthropometrics
- Section III: Tech-Administered Questionnaires
- Healthcare Preferences
- Cognitive Function: The Mini-Mental Status Examination
- Sociodemographics and Subjective Health
- Activities of Daily Living Self Reported Performance:
- Rosow-Breslau
- NAGI Scale
- KATZ-Activities of Daily Living
- Compensatory Strategies for Walking in the Home
- IADL'S (Instrumental Activities of Daily Living)
- CES-D (Center for Epidemiological Studies Depression Scale)
- Berkman Social Network Questionnaire
- Leisure Time Cognitive & Physical Activities
- Other
- Use of Nursing and Community Services
- Falls and Fractures
- Procedure Sheet & Exit Interview
- Walking in the Home
- Section IV: Physician-Administered Medical History
- Medical History
- Resting Blood Pressure (2)
- Referral Tracking
- Section V: Exam Completeness
- Procedures Sheet
- Exit Interview
- Adverse Events
Cohort Exam 29 Offsite Components
- Section I: Informed Consent & Tracking Procedures
- Informed Consent
- Waiver of Informed Consent
- HIPAA-Release of Health Information for Research Purpose
- FHS Follow-up by Proxy
- Tracking Information Form (Salmon Sheet)
- Section II: Clinical Measurements & Procedures
- Anthropometrics
- Weight
- Observed Physical Performance
- Handgrip
- Chair Stands
- Balance
- Timed Walk
- Anthropometrics
- Section III: Tech-Administered Questionnaires
- Healthcare Preferences
- Cognitive Function: The Mini-Mental Status Examination
- Sociodemographics and Subjective Health
- Activities of Daily Living Self Reported Performance:
- Rosow-Breslau
- NAGI Scale
- KATZ-Activities of Daily Living
- Compensatory Strategies for Walking in the Home
- IADL'S (Instrumental Activities of Daily Living)
- CES-D (Center for Epidemiological Studies Depression Scale)
- Berkman Social Network Questionnaire
- Leisure Time Cognitive & Physical Activities
- Other
- Use of Nursing and Community Services
- Falls and Fractures
- Proxy Form
- Section IV: Technician-Administered Medical History
- Medical History
- Resting Blood Pressure
- Section V: Exam Completeness
- Exit Interview
- MD Chart Review
- Referral Tracking & Adverse Events
- Participant Letter
- MD Letter to Personal Physician
2. Equipment for Exam Procedures & Equipment Calibration Times
Equipment for Exam 29 Procedures
- Clinic:
- Detecto Scale
Worcester Scale Co., Inc.
██████████
Worcester, MA
██████████
██████████ - Detecto Scale
Halliday Medical
Walpole, MA 02081
██████████
██████████
- Detecto Scale
- Offsite:
- SECA Portable Scale Model #841
MSI: Measurement Specialties Inc.
Fairfield, NJ 07007
- SECA Portable Scale Model #841
- Clinic:
- Weight to calibrate scale: 50 lbs.
- Worcester Scale Co., Inc. (See address above)
- Marquette Mac5000 (electrocardiogram cart)
- Marquette Electronics
██████████
Jupiter, FL 33468-9100 - ██████████
██████████
██████████ - ██████████
██████████
- Marquette Electronics
- Acquisition Module for Mac5000
- Cam-14 (See address above)
- Marquette Mac5000 – Offsite Visits
- Portable standard mercury column sphygmomanometer:
- Baumanometer 300 model
W.A. Baum Co., Inc.
██████████
Copaigue, NY 11726-3292
██████████
- Baumanometer 300 model
- Aneroid Sphygmomanometer – gauge type (offsite)
- P/N 5090 – 03 Tycos
Samuel Perkins, Inc.
Quincy, MA 02169 - Repairs and Calibration
Welch Allyn
Arden, NC 28704
██████████
- P/N 5090 – 03 Tycos
- Litman stethoscope tubing and earpieces with bell: Classic II
- Bauman latex free blood pressure cuffs in four sizes: regular adult, large adult, pediatric, thigh (clinic only).
- JAMAR dynamometer
- Model #5030J1
Sales Address:
Lafayette Instrument Co.
██████████
Lafayette, IN 47903
██████████ - Calibration Address:
Sammons Preston
██████████
Chicago, IL 60622
██████████
- Model #5030J1
- Stopwatch -Water Resistant/Shock Resistant VCAT: 1045
- Used as of 1-31-2007
Fisher Scientific
Atlanta, GA
██████████
- Used as of 1-31-2007
- Heart Square, by Heartware Inc.
- purchased from: Nova Heart
- Adjusted stool, 18"
- United Chair
██████████
██████████
Leeds, AL 35094
- United Chair
- Pocket Talker II
- Williams Sound Corp.
██████████
Eden Prairie, MN 55344
██████████
- Williams Sound Corp.
- SECA Stadiometer
- Halliday Medical
██████████
Walpole, MA 02081
██████████
- Halliday Medical
Equipment Calibration Time Table
| Activity | Daily | Weekly | Monthly | Yearly |
|---|---|---|---|---|
| Scale (Onsite) | ||||
| Zero Reading | X | |||
| 50# Weight | X | |||
| Professionally Calibrated | X | |||
| Digital Scale (Offsite) | ||||
| 50# Weight | X | |||
| Stadiometer (Onsite) | ||||
| Check w/ measuring tape | X | |||
| Tape Measure (Onsite & Offsite) | ||||
| Use purple tape measure | X | |||
| Mercury Manometer (Onsite) | ||||
| Zero Reading | X | |||
| Check Inflation System | X | |||
| Aneroid-Gauge Type (Offsite) | ||||
| Check Inflation System | X | |||
| Hand Grip (Onsite) | ||||
| Zero Reading | X | |||
| Professional Calibration | X | |||
| Hand Grip (Offsite) | ||||
| Zero Reading | X | |||
| Professional Calibration | X | |||
| Digital Timer (Onsite & Offsite) | ||||
| Professional Calibration | X | |||
| Scale | ||||
| Detecto Scale (Clinic) | ||||
| Zero Reading | X | |||
| 50 lb. Weight | X | |||
| Professionally Calibrated | X | |||
| Seca Scale (Offsite) | ||||
| Zero Reading | X | |||
| 50 lb. Weight | X | |||
| Sphygmomanometer | ||||
| Mercury Manometer | ||||
| Zero Reading | X | |||
| Check Inflation System | X | |||
| Aneroid-Gauge Type | ||||
| Check Inflation System | X | |||
| Stadiometer (Check level) | X | |||
| Dynamometer (Professional Calibrated) | X |
3. Guidelines for Coding Accuracy
To insure maximum accuracy and legibility for persons performing data entry, please adhere to the following guidelines:
- Use a red or blue pen or any other pen which will stand out from the page (pencil or black ball-point pens are unacceptable).
- Make sure all numerals are unmistakably clear.
- If measurements are not taken, please enter 9s in blanks if the coding option is available and document the reason. If the coding option of 9 is not available, leave blank and write any comments on why the questions were not asked. Your comments are helpful at any point of the exam where data is not recorded in the standard manner.
- If you make an error, please cross it out entirely, write the correct information in the margin, and initial the change. Do not superimpose numerals one on top of the other.
- Make sure both sides of the examination form are completed.
Section II. Informed Consent & Tracking Procedures
1. Informed Consent
An informed consent is administered to each participant by a trained interviewer prior to the collection of any research examination study data. The "consent form" is a two-part document. The firstpart is a narrative description of the studies goals, the content of the exam, the risks and benefits of participating, the confidentiality policies, the right to withdraw from the study, and what compensation is provided in the unlikely event that results in the need for medical care. The second part is the participants authorization page, which the participant signs. This documents the participant's consent agreeing to (1) participate in an interview and clinical examination, (2) be contacted by study personnel in the future, (3) obtain medical records concerning information relevant to the study, (4) release their clinically relevant study data to their medical care provider, and (5) use of previously frozen blood samples for research. The documents core content complies with guidelines from the National Heart, Lung, and Blood Institute and is approved by BU Medical Center IRB.
A. Overview
Informed consent is the first data collection form administered during the FHS exam. Only updated versions of the informed consent form, approved by the BUMC IRB will be used. All study subjects will be provided with:
- A description of what data collection procedures will be followed and what is involved in each procedure;
- The benefits and risks of participating in a research study which includes genetic analysis;
- A description of what procedures are in place to protect confidentiality;
- Information on the right to withdraw from the study, to not participate in a procedure or to decline to answer a question(s) without penalty;
- An opportunity to document their preference for the use and disposition of their study data and genetic materials; and
- A record of and a mechanism for contacting the project director/principal investigator and the study coordinator.
B. Administration
As the FHS staff person obtaining informed consent for cohort exam 29, one must provide ample time for the participant to read the consent and answer any questions the participant may have. During the consent process the consenter must " ... minimize the possibility of coercion or undue influence ... "(46.116 Code of Federal Regulations). One does this by allowing the participant to make their decision to participate on their own, without rushing them during the consent process. Participants must be given "... sufficient opportunity to consider whether or not to participate..." and if the participant refuses the exam their wishes must be honored (46.116 Code of Federal Regulations).
Once the participant has agreed to participate in the current exam cycle, their consent must be documented. This is done by using "...a written consent form approved by the IRB and [the consent must be] signed and dated by the subject..." (50.2 7 Code of Federal Regulations). Note: Be sure to use the current version of the approved consent if have any question of what consent should be used please ask either ██████████ or the BU/FHS liaison.
Listed below is important information that must also be documented during the consent process.
Completing the Physician Checkbox
A participant should check yes in the following situations:
- If the participant has a doctor and would like us to send results to their doctor;
- If the participant does not have a doctor, but will be getting one within the next 4-6 weeks and would like us to send results to their new physician.
A participant should check no in the following situations:
- If the participant does not want their research exam results sent to their personal physician
- If the participant does not have a doctor and will not be getting one within 4-6 weeks
Visual Impaired Participants
For participants that are visually impaired, the consent form should be read to the participant. A witness must be present during the consent process. The witness must attest that the information in the consent form was accurately explained to and apparently understood by the participant. Therefore, the subject can either sign ("make their mark") and date the consent form if they can or verbally agree to participate. The consenter signs the form as the person obtaining the consent and the witness will write on the consent form "consent witnessed by" and she/he also will sign and date the form.
If the participant refuses to have the consent form read to them (i.e., asks you to stop), a detailed summary of the exam contents must be provided to the participant. After the participant is informed of what is contained in the consent and they have indicated their agreement to participate, have them sign ("make their mark") and date the consent form if they can, to indicate their willingness to participate or allow them to verbally agree. The consenter must also document on the consent the way he/she communicated this information and also have the witness sign and date.
Photocopying Consents
A photocopy of the participant's signed consent must be given to the participant. According to the Code of Federal Regulation 21CFR 50.27 Documentation of Informed Consent "(a)...informed consent shall be documented by the use of a written consent form approved by the IRB and signed and dated by the subject...at the time of the consent. A copy shall be given to the person signing the form."
For offsite visits, the consent will need to be copied and mailed to the participant after the visit.
2. Waiver of Informed Consent


3. HIPAA - Release of Health Information for Research Purposes
RESEARCH SUBJECT'S AUTHORIZATION
FOR RELEASE OF HEALTH INFORMATION FOR RESEARCH PURPOSES
Name of Research Study: The Framingham Heart Study
██████████ Framingham, MA
01702-5827
IRB Number: 1910G
Subject's Name: ____________________ Birth Date: ____________________
We want to use your private health information in this research study. This will include both information we collect about you as part of this study as well as health information about you that is stored in your medical records. The law requires us to get your authorization (permission) before we can use your information or share it with others for research purposes. You can choose to sign or not to sign this authorization. If you choose not to sign this authorization, you will still be able to take part in the research study.
Section A:
I authorize the use or sharing of my health information as described below:
Who will be asked to give us your health information:
- Hospitals and physicians you have identified as providing medical care for a reported health problem
Who will be able to use your health information for research:
- The researchers and research staff conducting the Framingham Heart Study.
Section B: Description of Information:
(1) The researchers need to collect information about you and your health. This will include information collected during the study as well as information from your existing medical records so we can review the health problem(s) you have reported to us. The information disclosed under this authorization will not be redisclosed to anyone but the researchers conducting this study except as required by law.
(2) I authorize __________________________________________________ (List name of hospital/physician or clinic) to release to the Framingham Heart Study the following information from my medical records. Disclose the following information for the dates ranging from _______________ to _______________.
Specific description of information we will collect may include:
| •Face Sheet | •CT Scan (Head/Heart) |
| •Discharge Summary | •MRI/MRA (Head/Neck) |
| •ER Report | •Lab Reports- Cardiac Enzymes |
| •Admission Notes | •Consults (Cardiology & Neurology) |
| • Progress Notes | •Cardiac Catheterization |
| •Operative Report | •Exercise Tolerance Test |
| •Pathology report | •Nursing Home Notes |
| •Chest X-Rays | •Notes near time of death |
| •EKGs (All) | •Other: (for example: Echocardiogram, Arteriography, Venous Ultrasound, V/Q Scan, PA gram, etc.) |
Section C: General
- Expiration:
This authorization expires at the end of the study.
- Right To Revoke:
You may revoke (take back) this authorization at any time. To do this, you must ask the Framingham Heart Study for the names of the Privacy Officers at the institutions where we got your health information. You must then notify those Privacy Officers in writing that you want to take back your Authorization. If you do, we will still be permitted to see the information that we obtained before you revoked your authoriiation but we will only use your information the way the Informed Consent Form says.
- Your Access to the Information:
You have the right to see your Framingham Heart Study record only after the research study has been completed.
I have read this information, and I will receive a signed copy of this form.
__________________________________________________
Signature of research subject or personal representative
_______________
Date
Printed name of personal representative: __________________________________________________
Relationship to research subject: __________________________________________________
Please describe the personal representative's authority to act on behalf of the subject:
_________________________________________________________________
HIPAA: Research Subject's Authorization for Release of Health Information for Research Purposes
The HIPAA Privacy Rule, in effect April 14, 2003, protects the privacy of subject's health information which is used in human research. For researchers to gain access to health information that is stored at any HIPPA "covered entity" investigators must provide the covered entity with written assurances covering how the health information will be used and protected.
The Framingham Heart Study is not a "covered entity". However hospitals, nursing homes and physician offices from which the FHS collect medical records are covered by HIPAA rules. Therefore, in order for the FHS to retrieve medical records, participants must sign the HIPAA medical release form. If the participant chooses not to sign the form they will be able to participate in the exam but the FHS will not be able to obtain any outside medical records.
The following explanation of the form is to be given during the intake process:
We want to use your private health information in this research study. This will include both information we collect about you as part of this study as well as health information about you that is stored in your medical records. The law requires us to get your authorization (permission) before we can use your information or share it with others for research purposes. You can choose to sign or not sign this authorization. If you choose not to sign this authorization, you will still be able to take part in the research study.
The participant must also be given adequate time to read the release form. If they agree to sign the form, they must also be given a copy of it with their signature. For offsite exams, a photocopy will be mailed with the Informed Consent to the participant.
For cognitively impaired participants: If the participant is cognitively impaired and have had their consent form waived, have the participants' POA sign the IIlPPA form and ask for copies of the POA documentation to go along with it. The POA documentation is necessary for medical records to obtain records from covered entities.
4. FHS Follow-up by Proxy

Follow-Up by Proxy
One of the most important goals of the Framingham Heart Study (FHS) is to keep track of any major changes in your health through the end of the study. This information is important for answering scientific questions about heart disease and other health conditions. You are the best source of information regarding your health, but there may come a time when you are not able to provide details of your health. We are asking you to provide us with the name . of a person that can answer questions about your health if you cannot. This person will be considered your "proxy'' for the Framingham Heart Study.
What is a proxy?
A proxy is someone who can "stand in" for you and tell us about your health when you cannot because of a serious illness.
Why is a proxy needed?
For over 50 years you have been providing important information about your health to FHS. This information should not be lost, even if you are unable to provide it.
What does a proxy do?
We will ask your proxy to answer questions about your health, just like the questions you have been asked each exam cycle on your medical history update.
Whom should I name as my proxy?
You should select someone who knows you well·enough to provide health information about you. For example, your proxy can be your power of attorney, your legal health care proxy, or your legal next-of-kin (including your spouse, son, daughter, brother, sister, etc.).
Am I allowed to change my proxy?
Yes, you may change your proxy at any time by either calling FHS or by indicating your wishes at your FHS examination.
Will you give my proxy information about me?
No, all of your information is strictly confidential and will not be provided to your proxy.
What would you like me to do now?
Using the attached form please indicate whom you have chosen to be your proxy. Please indicate his/her name, contact information, relationship to you, and then sign the form.
You will be given a copy of this form for your own records and one to give to your proxy. This material should be kept by your proxy so he/she understands your wishes as a participant in the Framingham Heart Study.
If you have any questions, call ██████████ Cohort Participant Coordinator, ██████████ or ██████████
Thank you for your continued dedication to the Framingham Heart Study!
FHS Follow-up by Proxy
During each exam cycle the cognitively intact participant will be asked to designate a health care proxy for the Framingham Heart Study. They are asked to provide a proxy in the event that they are unable to provide the details of their health. The participant should select someone who knows them well enough to provide health information about them.
Ask the participant to read the letter entitled "Follow-up by Proxy" and complete the designation form. Examples of proxies are: Power of Attorney, Legal Health Care Proxy, and/or legal next-of-kin (spouse, son or daughter, brother or sister, or their doctor). If they have a Power of Attorney (POA) and have paperwork, a photocopy of this is necessary for the Medical Records Department to obtain records in the event the participant becomes cognitively impaired and the proxy signs a medical release form.
Two photocopies of the proxy packet must be given to the participant, one for them to keep, the other to give to their "proxy".
Section III. Clinical Measurements & Procedures
1. Anthropometrics
Update Sociodemographic Data and Family History
Personal and family information is found on the Personal and Family History Data Sheet (salmon colored sheets). A copy is made in which to write updated information on during intake. The information can be obtained from the participant, the proxy or the chart at the facility where they reside.
Updated information regarding the participant's current address, physician and two contacts should be written on the photocopied sheet provided.
On the inside of the form is the family demographic information. This covers the participant's spouse, children, parents and siblings. Updated information regarding their vital status (living or dead) and health status should be documented.
Weight Measurement
Clinic
- Ask participant to wear FHS gown for measurement if he/she brought a heavy gown from home ask them to remove it. The participant should remove slippers or shoes.
- Prior to asking participant to step onto the scale lift the counter poise and position it at zero.
- Ask the participant to step onto the scale, facing measurement beam.
- Instruct the participant to stand in the middle of the scale platform with head erect and eyes looking straight ahead. Weight should be equally distributed on both feet and the participant should not touch or support him/herself
- With the participant standing still in the proper position lift the counterweight (larger weight) and slide it to the right until the beam approaches balance.
- Adjust the top poise until the beam is evenly balanced.
- Have the participant step off the scale. The technician should stand directly in front of the scale and read the weight with eyes level to the point of measurement.
- Record the weight to the nearest pound; round up if ≥ 0.5, round down if < 0.5.
- Calibrate the scale daily
- Protocol modification- if deviations from protocol record it as a protocol modification. Example: Left Shoes On.
Offsite
- The participant should remove slippers or shoes.
- Prior to asking participant to step on the scale turn scale on and check to make sure it reads 0.0. The scale should be on a flat, hard surface.
- Ask the participant to step onto the scale.
- Instruct the participant to stand in the middle of the scale platform with head erect and eyes looking straight ahead. Weight should be equally distributed on both feet and the participant should not touch or support himself/herself.
- Read the digital display while participant is on the scale.
- Have the participant step off the scale.
- Record the weight to the nearest pound; round up if ≥ 0.5, round down if < 0.5.
- If participant is unable to stand for weight measurement at a nursing home record the last weight in nursing home chart and the date the weight was obtained. If the participant is unable to stand on a scale during a home visit, record the weight measurement as 999.
- Calibrate the scale monthly
Standing Height Measurement
(clinic only)
Clinic
- Participant should be barefoot or wearing thin socks so positioning of the body can be seen. Ask participant to stand erect with his/her back to vertical mounted stadiometer.
- Heels should be together and against the vertical ruler, both feet flat on the floor, with weight distributed evenly across both feet. Check to make sure both feet are back against the wall.
- Participant faces straight ahead with his/her head positioned in the Frankfort horizontal plane (see next page). The lower margin of the bony orbit (the socket containing the eye) should be on the same horizontal plane as the most forward point in the supratragal notch (the notch just above the anterior cartilaginous projections of the external ear).
- Ask participant to let arms hang freely by the sides of the trunk, palms facing the thighs. Ask participant to inhale deeply and maintain a fully erect position.
- Bring the level down snugly (but not tightly) on top of participant's head.
- Record measurement to the nearest 1/4 inch, rounding down.
Note: Measurement is not taken during offsite visits.
2. Blood Pressure & Maximum Inflation
Technician's Seated Blood Pressure
A. Equipment:
- One standard Littman stethoscope tubing and earpieces with bell: Classic II 3M
- One standard mercury column sphygmomanometer: Baumanometer (clinic)
- Aneroid sphygmomanometer (off-site)
- BP cuffs in four sizes (all Latex free)
- Thigh adult cuff
- Large adult cuff
- Regular adult cuff
- Pediatric cuff
B. Blood Pressure Cuff Placement:
- Bare participant’s left arm to the point of the shoulder.
- Determine correct cuff size using guidelines inside the cuff.
- Palpate the brachial artery.
- With participant seated, place the appropriate cuff around the upper left arm. The midpoint of the length of the bladder should lie over the brachial artery. Each cuff has an artery marker. The mid-height of the cuff should be at heart level.
- Place the lower edge of the cuff, with its tubing connections, about one inch (1") above the natural crease across the inner aspect of the elbow.
- Wrap the cuff snugly about the arm, with the palm of the participant’s hand turned upward.
- If the subject has had a left-sided mastectomy, the right arm may be used for blood pressure measurement. If right arm is used, note it on the form.
C. Determination of Maximal Inflation Level
For each participant, determine the maximal inflation level, or the pressure to which the cuff is to be inflated for blood pressure measurement. This assures that the cuff pressure at the start of the reading exceeds the systolic blood pressure and thus allows the first Kortokoff sound to be heard.
- Attach the cuff tubing to the sphygmomanometer.
- Palpate the radial pulse.
- Inflate the cuff rapidly until the radial pulse is no longer felt (palpated systolic pressure) by inflating rapidly to 70 mmHg, then inflating by 10mmHg increments.
- Deflate the cuff quickly and completely.
- The maximal inflation level is 30 mmHg above the palpated systolic pressure.
D. Guidelines for Accurate Blood Pressure Readings:
- The participant should be in a seated position for at least 5 minutes before the blood pressure is measured.
- All readings are made to the nearest even digit.
- Any reading which appears to fall exactly between marking on the mercury column should be read to the next higher marking (i.e. 2, 4, 6, 8, or 0).
- All readings are made to the top of the meniscus, the rounded surface of the mercury column.
- When the pressure is released quickly from a high level, a vacuum is formed above the mercury and the meniscus is distorted. Allow a few moments for it to reappear before reading the manometer.
For offsite Blood Pressures: Check that the needle is at the zero mark at the start and the end of the measurement. Place the manometer in direct line of sight with the eye on a line perpendicular to the center of the face of the gauge.
E. Blood Pressure Readings:
- Following any previous inflation, wait at least 30 seconds after the cuff has completely deflated.
- By closing the thumb valve and squeezing the bulb, inflate the cuff at a rapid but smooth continuous rate to the maximal inflation level (30 mmHg above palpated systolic pressure).
- The examiner’s eyes should be level with the mid-range of the manometer scale and focused at the level to which the pressure will be raised.
- Open the thumb valve slightly. Allow the cuff to deflate, maintaining a constant rate of deflation at approximately 2 mmHg per second.
- Using the bell of the stethoscope, listen throughout the entire range of deflation, from the maximum pressure past the systolic reading (the pressure where the FIRST regular sound is heard), until 10 mmHg BELOW the level of the diastolic reading (that is, 10 mmHg below the level at which the LAST regular sound is heard).
- Deflate the cuff fully by opening the thumb valve.
- Remove the stethoscope. Neatly enter systolic and diastolic readings in the spaces provided on the form.
Elevated Blood Pressure
If, during a home visit the blood pressure is:
- > 200/110 a call is made to a FHS physician who will notify the participant’s personal physician. The chart will be marked “expedite” so that the letter to the personal physician is sent out ASAP.
- > 180/100 the chart is expedited
-The Referral sheet is completed to note that contact was made to an FHS MD during the exam.
-If a phone contact was made by an FHS MD to the participant’s personal physician, the FHS MD is to complete a “Record of Telephone Encounter” form.
If, during a nursing home visit the blood pressure is:
- > 140/90 inform the nurse caring for the participant or the charge nurse
- > 180/100 inform the nurse caring for the participant or the charge nurse. The chart will be marked “expedite” so that the letter to the personal physician is sent out ASAP.
3. ECG
ECG Lead Placement
- V1: The first intercostal space is palpated just below the clavicle. Count down and identify the 4th intercostal space just below the fourth rib. Point V1 is just to the right of the sternum in the fourth intercostal space. Make a small line with a marking pencil here to show where the ECG lead should be placed.
- V2: Should be at the same level as Point V1 and immediately to the left of the sternum. Make a small line with a marking pencil to show where the ECG lead should be placed.
- To locate the horizontal reference level for electrodes (Point E), starting from V2, locate the
fifth intercostal space. Move your finger in the 5th intercostal space laterally to where the
midclavicular (center of the chest where you feel a bend in the clavicle) line intersects the fifth
intercostal space. Make a horizontal line at this point.
Mark the exact transverse (horizontal) level at this spot with the midsternal line. It should be about one inch (1”) below V1 and V2 placements.
- V6: Move the participant’s elbow laterally away from the body. Mark the midaxillary line in the exact vertical center plane of the thorax down to the intersection of the horizontal plane marked by the location of E. This is the exact location of V6. (NOTE: It is a common mistake to locate the midaxillary line too far anteriorly, toward the V5 location).
- V4: Place the # arm of the Heart Square firmly across the lower sternum at the level of Point E (as
you face the participant, the writing on the Heart Square will appear upside down and backwards). Adjust the
E and V6 arms of the Heart Square so they are both perpendicular to the long axis of the
thoracic spine at the level of the E position. The E arm should be exactly horizontal. If the
participant is lying flat, the V6 arm should be exactly vertical.
Slide the V6 arm so the 0 point (the arrow labeled V6) is at the marked location for V6. Double check that the E arm is still in the correct spot.
V4: On the V6 arm (the slide), find the number corresponding to the E measurement. Following the corresponding 45 degree line to the surface (e.g. 16) and mark the location following the inside of the square. Place electrodes on TOP of the breast.
The participant may now lower the left arm in a more comfortable position.
- V3: Exactly halfway between V2 and V4.
- V5: Exactly halfway between V4 and V6.
- Before electrodes are placed on the participant, ask if he/she is known to be allergic to alcohol wipes. If yes, prepare the
areas of electrode placement by rubbing with water and drying with a washcloth. If allergies are denied, prepare the
areas by wiping with an alcohol wipe and drying with a washcloth.
NOTE: Place the electrodes on the participant and hook up the leads before entering the data in the ECG machine. This will allow ample time for the participant to relax and the machine interference to smooth out.
- Attach limb leads in the following order: right leg (RL), left leg (LL), right arm (RA), left arm (LA) parallel to the limb with tabs facing toward the heart. This will avoid lead reversal.
- The body of the electrode is placed centrally at the pencil mark with the tab extending downward. Precordial electrodes are attached in the following order: V1, V2, V3, V4, V5, V6. Recheck all leads for proper placement.
- Ask the participant to lie still and relax. In the computer, enter the participants Name, ID, Age, Height (clinic only), Weight, and Gender. Enter the Exam Cycle, Location (1=clinic 2=offsite), and your Tech ID.
- The ECG is printed and reviewed for errors. If ECG needs to be run at 5 mmHg because of high voltage (if the standard 10 mmHg is beyond the lines of the ECG paper), highlight (yellow or orange highlighter) the 5 mmHg on the bottom of the printed ECG. On the top margin of the tracing write “ 1/2 STANDARD” using a bold magic marker.
- Leads are checked again for proper placement and disconnected. Electrodes are carefully removed.
ECG CODING FOR FRAMINGHAM HEART STUDY EXAMINATIONS
- General Comments:
Although the computerized ECGs which are recorded in clinic include measurements of rate, intervals and axis, it is important that the examining MD carefully examine the ECG and record these features on the coding forms. Your measurements (not those made by the computer) form the basis of the official ECG interpretation.
An important rule to remember: Please ask for help when you are unsure about interpretation of ECGs or our methods of coding. Be sure to always look at the old ECG for interim changes.
- Heart Rate:
Each exam room is equipped with a rate stick with which heart rate can be measured. (The computer does a good job with this measurement).
- Intervals:
PR, QRS and QT intervals are measured in hundredths of a second based upon examination of the ECG recording. (Lead II should be used when possible for these measurements). A QRS of 0.08 seconds is coded as 08.
- QRS Angle"
This refers to frontal plane axis in degrees. Each exam room is equipped with a hexaxial device for measuring QRS axis. (The computer does a good job with this measurement).
- Conduction Abnormality:
- IV Block
This refers to right and left bundle branch block. Note that the code 1 is used for incomplete BBB and 2 is for complete BBB. For complete BBB the QRS interval should be .12 sec or greater. When the QRS is prolonged, but the pattern is not that of right or left BBB, the indeterminate IV block is coded as follows: 1 =QRS .12 or greater, 2=QRS of .11 or .10. Remember that the measurements of QRS duration are those made by the examining physician and not by the computer. An RSR' pattern in the absence of QRS prolongation should be coded as normal. When an RSR' pattern occurs with a QRS duration of .09 sec or greater it represents incomplete RBBB.
- Hemi block
1=left anterior. This is present when the QRS axis is -30 or less and small q wave is present in lead I.
2=left posterior. QRS axis is >90 and small q is present in AVF, in absence of evidence of right ventricular hypertrophy.
- Fascicular block
1=bifascicular. A) If complete RBBB + (1st degree AV block or a hemiblock) are present. B) Complete LBBB.
2=trifascicular. If RBBB + hemiblock + 1st degree AV block. Or LBBB + 1st degree AV block.
- AV Block
1st degree when QRS duration is .20 seconds or greater (measured in lead Il).
2nd degree when some P waves are not conducted. This comes in tow forms a) Mobitz I. When progressive PR prolongation precedes the dropped P wave and b) Mobitz Il when QRS complexes are dropped without prior PR prolongation. AV dissociation occurs when P waves are QRS complexes march out independent of each other.
- WPW
A short PR intervals is present (typically .12 seconds or less) and a slurred upstroke of the QRS is present (so called delta wave). When these features are both fulfilled, WPW= 1. When the PR is .12 or less and a delta wave is possibly present, or when a delta wave is present but the PR is marginally short .13 to .14 seconds, WPW=2.
- Atrial Enlargement:
- Right Atrial Abnormality
The P wave is inferior leads is peaked with a height of 2.5 mm.
- Morris P wave
The terminal portion of the V wave in lead VI is inverted and measures at least Imm by Imm (at normal standardization). This reflects left atrial enlargement.
- Right Atrial Abnormality
- Myocardial Infarction
This is determined on the basis of the appearance of wide (.04 seconds) or deep (1/4 the height or the R wave) q waves. All tracings should be compared to the prior exam ECG which is always provided. The appearance of new, but small q waves should also be regarded as suggestive of MI. Loss of R waves in leads where they were previously present (see prior exam's ECG) should also raise suspicion of MI. A posterior MI is present when R > S in V1, R is .04 seconds in duration, and an upright T wave is recorded in that lead. When criteria are largely, but incompletely fulfilled be sure to code this item as maybe!
- Maximum I Wave Amplitude <-5mm
This refers to giant inverted T waves at least 5mm deep. This condition is occasionally seen in hypertrophic cardiomyopathy.
- Left Ventricular Hypertrophy
Be sure to carefully code each of the voltage criteria individually. Definite LVH is present when increased voltage is present together with a strain pattern (downsloping ST). Possible LVH is present when voltage criteria are fulfilled but only mild ST-T abnormalities (flattening) are noted. For cohort Exam 21, we have a separate code for LVH by voltage only. When complete BBB is present, LVH should be coded as unknown (9).
- Right Ventricular Hypertrophy
Definite RVH is present when increased R wave voltage is present in V1 and increase S wave voltage is present in V5 in the absence of RBBB. The sum of RV1 + SV5 should be at least 10.5mm.
- Arrhythmias
The presence of rhythm disturbances should be made on the basis of examination of the ½ speed rhythm strip which accompanies each ECG. This represents a simultaneous 3 lead recording of the entire 12-lead ECG.
- IV Block


4. Observed Physical Performance
A. Overview:
An objective performance measure of physical functioning is an assessment instrument in which an individual is asked to perform a specific task and is evaluated in an objective, standardized manner using predetermined criteria, which may include counting of repetitions or timing of the activity as appropriate. Two theoretical models of the pathway from disease to disability have been developed. The first comes from the World Health Organization and goes from disease to impairment to disability, to handicapped. The second, which is being used more now by geriatricians and aging researchers, progresses from disease, to impairment, to functional limitations, to disability.
Definitions
Impairment: Dysfunctional and structural abnormalities in specific body systems, such as the musculoskeletal system or the cardiovascular system.
Functional limitations: Restrictions in basic physical and mental actions, including things such as ambulation reaching, and grasping.
Disability: Difficulty doing activities of daily life, including not only personal care, but household management, jobs, and hobbies.
B. Methods:
During all tests, participant safety is paramount. Participants who do not feel safe or who are unable to perform a test should not be pressed. All procedures should be clearly demonstrated to the participant prior to performing any test and the participant should be queried to ensure that they understand the instructions. If it is obvious that the participant has not understood the directions, reread the standard instructions. You will be demonstrating each maneuver. Someone who may not completely understand the verbal instructions may still be able to petform the test following the demonstration.
C. Equipment:
- Data sheets
- Pen
- Stopwatch
- 1 Armless straight back chair measuring approximately 18" high from floor to top of seat.
- JAMAR Dynamometer
- Straight back chair with arm rests
- Measured 4 meter walking course
D. A note on encouragement:
If a participant expresses doubt as to whether he or she can perform the task, ask the participant whether they would like to try. If they say yes, proceed with the task but if they say no, honor the participant's choice to decline the testing.
E. Introductory script:
We are going to try to do different physical activities together. I will ask you to stand in different positions for me. I will ask you to walk for me and then I will ask you to stand up from a chair.
I will first explain what I would like you to do, then I will demonstrate it for you, and then I will ask you to try it for me.
F. Performance Measures:
- Hand Grip Strength Test
- Stands
- Repeated Chair Stands
- Measured Walks
JAMAR Hand Grip Strength Test:
- Introductory script: This instrument will measure your grip strength. The instrument is a little heavy, so be careful. When I tell you, I want you to squeeze the instrument as hard as you can. Do not expect the handle to move very much.
- Participant is seated in chair with arms, forearm resting on chair arm, elbow at about a 90 degree angle.
- Participant should hold JAMAR in upright position, wrist in neutral position, JAMAR facing the technician.
- Make sure that red peak-hold needle is set to zero.
- Tell participant to squeeze as hard as s/he can, and squeeze until you tell s/he to stop. Hold squeeze for a 3 to 5-1000 second count.
- Take back JAMAR, hold at eye level at about a foot from your eyes and record reading on the kilogram scale. If directly in the middle of the scale then the reading is the odd number between the two even hash marks; otherwise record as the closest hash mark.
- Repeat steps until three measurements are recorded with the right hand.
- Repeat steps for three trials with the left hand.
Stands:
The tests of balance provide an assessment of the participant's ability to hold three basic standing positions with the eyes open. These positions are side-by-side, semi-tandem, and full tandem stand (or heel-to-toe) and are performed in this order. Participants taking this test must be able to stand unassisted without using a cane or a walker. Don't assume that a participant who arrives for testing using a cane or walker can't stand unassisted. Ask them if they can stand without the device and are willing to try the test. If they say yes, you can assist them to assume the correct position for the testing.
The participant will hold each standing position for ten seconds.
Side by Side: Feet together
Semi-Tandem: Heel of one foot lines up with the big toe of the other foot
Tandem: Heel of one foot touching the toes of the other foot
While performing stands, the participant should be wearing comfortable shoes, with low heels. No bare feet or slippers. The participant must be able to stand unaided. You may assist participant with getting up from a chair.
- Side by Side stand:
First, I would like you to stand with your feet together, side by side, for ten seconds. Please watch first while I demonstrate. You may use your arms, bend your knees, or move your body to maintain your balance, but try not to move your feet. Try to hold this position until I say "stop".
Are you ready? Begin.
You may help the participant into the position. Allow them to hold onto your arms to obtain their balance. If they are holding on, say, When you are ready, let go of my arms. Begin timing the ten seconds when he or she lets go.
When the subject steps out of position, grasps your arm, or when the ten seconds have elapsed, stop timing and say, stop. If the participant steps out of position, the stopwatch is stopped when their foot is replanted on the floor. Record results on data sheet.
If the participant is unable to hold the side by side position for ten seconds, skip the next two stands.
- Semi-tandem stand:
Next, I would like you to stand with the heel of one foot touching the big toe of the other foot for ten seconds. You may put either foot in front, whichever is more comfortable for you. Please watch while I demonstrate. You may use your arms, bend your knees or move your body to maintain your balance, but try not to move your feet. Try to hold this position until I say "stop".
Are you ready? Begin.
If the participant is unable to hold the semi-tandem stand for ten seconds, skip the tandem stand.
- Tandem:
Next, I want you to try to stand with the heel of one foot in front of and touching the toes of the other foot for ten seconds. You may put either foot in front, whichever is more comfortable for you. Please watch while I demonstrate. You may use your arms, bend your knees or move your body to maintain your balance but try not to move your feet. Try to hold this position until I say "stop".
Are you ready? Begin.
The following questions should be answered for each stand:
Was this test completed? (Held for 10 seconds)
- Coding
- 0 = No
- 1 = Yes
- 8 = N/A
- 9 = Unknown
- If test was not attempted or completed, why not?
- Coding
- 1 = Physical limitation
- 2 = Refused
- 3 = Other (write in)
- 9 = Unknown
- Number of seconds held if less than 10 seconds.
c. Repeated Chair Stands:
The participant will attempt to stand up once from his chair without using his or her arms. This is not timed. If he or she is able to do this, then proceed to the timed five consecutive chair stands.
If participant feels it is unsafe, skip the chair stands
Do you think it is safe to try to stand up from a chair without using your arms?
The next tests measure the strength in your legs. First, I will ask you to fold your arms across your chest and sit so that your feet are flat on the floor. Then I will ask you to stand up without using your arms.
Please watch while I demonstrate.
Please fold your arms across your chest and begin when I say, "Ready, stand."
Stand in front of the participant before he or she begins. Be prepared to supply physical support if the participant's safety requires it, but do not stand so close as to impede the task.
If he or she cannot get up from his chair the first time without using their arms, ask him to try standing up using his arms. Score this and skip the repeated stands.
Do you think it is safe to try and stand up from a chair five times without using your arms?
If participant does not feel that it would be safe, abort the five chair stands and record on data sheet.
I will ask you to stand up straight, as quickly as you can, five times without stopping in between. After you stand up each time, sit down and then stand up again. Keep your arms folded across your chest. I will be timing you.
When you have finished the last stand, please sit down and hold out your left arm, with the palm facing up, so that I can take your pulse.
Please watch while I demonstrate.
Please fold your arms across your chest and begin when I say, "Ready, stand".
Start timing on the word "Stand".
Count aloud after the participant reaches the top of each stand.
If the participant appears to be fatigued before completing all five stands, ask if they can continue. Only if they say "no" should the examiner stop timing and stop the procedure.
If the participant did not use his or her hands during the initial chair stand, but begins to use them during the repeated stands, then stop.
If, after one minute has elapsed, the participant has not completed all five stands, then stop.
Stop timing when the participant has straightened up completely for the fifth time.
Have the subject sit down immediately after the fifth stand so that you can take the thirty second pulse on the left wrist.
Answer the following questions:
| Was this test completed? Coding 0= No 1= Yes 8= Not attempted 9= Unknown | If not attempted or completed, why not? Coding 1 = Physical limitations 2 = Test not completed 3 =Refused 4 = Other __________ 5 = Test stopped in 60 seconds 9=Unknown |
If it is an off site visit, the height of the chair used is measured and recorded.
The time to complete five stands in seconds is recorded.
If less than five stands are completed, enter the number of stands completed.
Measured Walks:
The participant will first observe while the examiner demonstrates how to walk the measured course at a normal pace. The participant will then be asked to walk the measured 4 meter course at a normal walking pace while being observed and timed. Next, he or she will repeat this usual pace while being timed. The examiner will then demonstrate the rapid pace walk and the participant will be asked to walk the course at a rapid pace while being timed.
A cane or walker may be used during the walk, but if people with such devices can walk short distances without them, they should be encouraged to do so. Many people with assistive devices use them only when they walk outdoors or for long distances indoors. Doing the test without the device provides a much more accurate assessment of the functional limitation of the participant. Ask the participant if she ever walks at home without the device. Then ask the participant if s/he thinks he/she can walk a short distance for the test. Participants who normally use assistive devices should be watched particularly closely during the test to prevent falling.
The walking course should be unobstructed and include at least an extra one-half meter on each end. You will need a measuring tape to measure the distance of the walking course and masking tape to mark the starting and finish lines.
- Walk #1:
Now I am going to obsen1e how you normally walk, if you use a cane or other walking aid and would be more comfortable with it, you may use it.
This is our walking course. I want you to walk to the other end of the course at your usual speed, just as if you were walking down the street. Walk all the way past the other end of the tape before you stop. Do you think this would be safe?
If participant says that it would not be safe indicate this on the data sheet and abort walks.
Please watch while I demonstrate. When I want you to start, I will say "Ready, begin."
Have the participant line up his or her toes behind the line on the floor. Start timing when you say, "begin" and stop timing when the participant breaks the plane of the line at the end of the course. Record the time on data sheet.
- Walk #2:
Now I want you to repeat the walk. Remember to walk at your usual pace, and all the way past the other end of the course.
Ready? Begin.
Observed Performance Scoring
If a participant has an actual measured time of 9.99, make a note on the exam stating that the figure represents an actual time as opposed to unknown, and flag the variable so that when it gets cleaned, whoever is cleaning can make a point of changing the person's time back from missing. Otherwise, round the time up to ten seconds and code that the participant was able to hold their position for 10 seconds.
Section IV. Tech-Administered Questionnaires
1. Healthcare Preferences
End of Life Preference Questionnaire
A. Rationale and Background:
Americans today enjoy a longer lifespan, many living well into their 80s and 90s. For many, however, an unfortunate consequence ofliving well into old age is a life accompanied by chronic and debilitating illnesses. Advances in medical technology have left many frail elderly patients vulnerable to a prolonged death commonly characterized by extended hospitalizations and costly invasive medical procedures. A key element to improving care at the end oflife is the principle of patient autonomy including patients' rights to participate in decisions about the medical care. However, many patients near the end of life are not cognizant and are unable to participate in these important decisions. Therefore, advance care planning is a necessary component to achieve quality of care at the end of life.
The questionnaire should be introduced to the participant by using the following text:
People have many ideas about health and health care. Understanding these ideas is crucial to improving care. We are interested in learning what you believe to be the most important considerations at this point in your life. There are no right or wrong answers. We are simply interested in your opinions. We understand that this is a sensitive topic. Your participation is voluntary and you may choose to stop answering questions at any time.
Would you like to proceed? (0=No, 1=Yes, 9=Not done due to cognitive status)
This question will be used to assess the feasibility of collecting information about advance care planning in community-dwelling elders and the acceptability of this questionnaire to original cohort participants.
B. Definition of Terms:
Health Care Proxy - is a legal document that designates a trusted relative or friend to make health care decisions for you if, because of an illness or accident, you're incapable of making or communicating them yourself
Living Will - A living will is a document in which you specify in advance medical treatment that you would or would not want in the event that you became unable to express your wishes. Massachusetts is one of only three states that recognizes health care proxies but does not recognize living wills. Living wills are still potentially useful because they guide Agents (for example your health care proxy, family members) and physicians about the types of choices a person would make.
Health Care Preferences - Are a statement of what an individual values in their life and their preferences concerning future health states such as being permanently comatose, ventilated or tube fed. Some patients want to "fight to the end" while others believe if they decline treatment they are "giving up"; yet others want to focus on their "quality of life" or "live life until they die". Depending on an individual's preferences their medical care can be focused on extending life as much or on minimizing suffering and promoting comfort until death.
Power of Attorney - is a legal document that designates a trusted relative or friend to make legal and financial decisions for you if, because of an illness or accident, you' re incapable of making or communicating them yourself. Sometimes, a Power of Attorney also gives the designee the right to make health care decisions.
If the participant requests further information encourage the participant to contact their physician or other health care provider.
C. Procedure:
- Read the introduction to the participant including the statement that this is a sensitive topic, their participation is voluntary, and they may choose to stop answering questions at any time.
- Ask if they want to proceed.
- Always read the introduction to each set of questions.
- Remember that we are asking a participant about their beliefs and preferences. There are no right or wrong answers. We want to know their thoughts.
- These questions must be answered by the participant, not a proxy.
D. Methods:
There are 16 items included in the Health Care Preferences Questionnaire.
- Read the introduction to each set of questions.
- Read each question as it is written on the form and then read the available responses.
- Code 9 = Refused or Do not know is used when:
- The question was asked, but the participant chooses not to answer. For example, response was I would rather not say or Go on to the next question.
- The question was asked, but the participant does not know, does not remember or does not understand the statement.
- Circle the response on the form.
- When the participant asks about the meaning of any item or tries to qualify a statement, simply repeat the statement. If the participant still asks about the meaning or says he/she does not understand, check 9 = refused or don't know. Do not try to interpret the statement for the participant.
- If a participant becomes visibly upset by the questions do not continue and document which question they found upsetting and inform Dr. Murabito.
- If a participant wants further information refer them to their physician.
E. Interviewer Feedback:
At the end of each questionnaire, the interviewer will be asked to answer the following questions for each participant:
- Did the participant choose to stop before completing all 16 questions? If so, why did they stop and at what question.
- Did the participant seem upset or bothered by any of the questions that were asked? If yes, which question.
- Where there any questions that the participant had particular difficulty understanding? If yes, which question(s).
Important Differences Between Health Care Proxies and Living Wills
Committees and MINS - Advance Directives 08/01/2000
Advance Directives, such as Health Care Proxies and Living Wills, allow people to retain control over medical decisions. Massachusetts law allows people to make their own Health Care Proxies, but does not officially recognize Living Wills. A Health Care Proxy designates another person to make medical decisions should you be unable to do so, and a Living Will allows you to list medical treatments that you would or would not want if you became terminally ill and unable to make your own decisions.
Massachusetts is one of only three states that recognizes Health Care Proxies but does not recognize Living Wills. Living Wills are still potentially useful because they guide Agents and physicians about the types of choices a person would make. More information about advance directives can be found at:
What is a Living Will?
A living will is a document in which you specify in advance medical treatment that you would or wou.ld not want in the event that you become unable to express your wishes. Massachusetts is one of only three states that recognizes health care proxies but does not recognize living wills. Living Wills are still potentially useful because they guide Agents and physicians about the types of choices a person would make.
MASSACHUSETTS HEALTH CARE PROXY
What does the Health Care Proxy Law allow?
The Health Care Proxy is a simple legal document that allows you to name someone you know and trust to make health care decisions for you if, for any reason and at any time, you become unable to make or communicate those decisions. It is an important document, however, because it concerns not only the choices you make about your health care, but also the relationships you have with your physician, family, and others who may be involved with your care. Read this and follow the instructions to ensure that your wishes are honored.
Under the Health Care Proxy Law (Massachusetts General Laws, Chapter 201D), any competent adult 18 years of age or over may...appoint a Health Care Agent. You (known as the "Principal") can appoint any adult EXCEPT the administrator, operator, or employee of a health care facility such as a hospital or nursing home where you are a patient or resident UNLESS that person is also related to you by blood, marriage, or adoption.
What can my Agent do?
Your Agent will make decisions about your health care only when you are, for some reason, unable to do that yourself. This means that your Agent can act for you if you are temporarily unconscious, in a coma, or have some other condition in which you cannot make or communicate health care decisions. Acting with your authority, your Agent can make any health care decision that you could, if you were able.
Your Agent will make health care decisions for you according to your wishes or according to his/her assessment of your wishes, including your religious or moral beliefs. It is very important that you talk with your Agent so that he or she knows what is important to you. If your Agent does not know what your wishes would be in a particular situation, your Agent will decide based on what he or she thinks would be in your best interests...if you still object to any decision made by your Agent, your own decisions will be honored unless a Court determines that you lack capacity to make health care decisions.
Your Agent's decisions will have the same authority as yours would, if you were able, and will be honored over those of any other person, except for any limitation you yourself made, or except for a Court Order specifically overriding the Proxy.
Who should have the original and copies?
After you have filled in the form, remove this information page and make at least four photocopies of the form. Keep the original yourself where it can be found easily (bot in your safe deposit box). Give copies to your doctor and/or health plan to put into your medical record. Give copies to your Agent. You can give additional copies to family members, your clergy and/or lawyer, and other people who may be involved in your health care decision making.
How can I revoke or cancel the document?
Your Health Care Proxy is revoked when any of the following four things happens:
- You sign another Health Care Proxy later on.
- You legally separate from or divorce your spouse who is named in the Proxy as your Agent.
- You notify your Agent, your doctor, or other health care provider, orally or in writing, that you want to revoke your Health Care Proxy.
- You do anything else that clearly shows you want to revoke the Proxy, for example, tearing up or destroying the Proxy, crossing it out, telling other people, etc.
For More Information on Choice in Death and Dying:
http://www.abcd-caring.org Americans for Better Care of Dying
http://www.careguide.net Everything families need to understand, plan, and manage care for their elderly loved ones
http://www.choices.org (Choice In Dying web site, which has general information as well as information about Massachusetts).
http://www.partnershipforcaring.org Partnership for caring: America's voices for the dying.
The following information on Advance Directives was printed from the Partnership for Caring website.
http://www.partnershipforcaring.org Partnership for caring: America's voices for the dying.
Very Willing
Somewhat Willing
Somewhat Unwilling
Very Unwilling
Rather Die
2. Mini-Mental State Exam (MMSE)
A. Background and Rationale:
Cognitive function may decline as a result of certain risk factors (e.g. hypertension, elevated cholesterol, cardiac arrhythmias). This in turn could adversely impact the physical functioning and quality oflife of older adults. Dementia is a major illness and cause of disability among the elderly. Cerebrovascular disease or multi infarct dementia is the second leading cause of dementing illness among Caucasians, preceded only by Alzheimer's Disease.
The Mini-Mental State Exam (MMSE) is a widely used test of cognitive function among the elderly; it includes tests of orientation, attention, memory, language and visual-spatial skills.
B. Definitions:
- Alert Level: In general participant scoring below education-adjusted cut-off scores* on the MMSE may be
cognitively impaired.
MMSE-EDUCATION ADJUSTED CUT-OFF SCORES
- Subjects whose education levels are 7th grade or lower, a score on the MMSE of 22 or below
- Subjects whose education attainment level is 8th grade or some high school (but not a graduate of), a score on the MMSE of 24 or below
- Subjects whose education attainment level is high school graduate, a score on the MMSE of 25 or below
- Subjects whose education attainment level is some college or higher, a score on the MMSE of 26 or below.
*Note: The Education Adjusted Cut-off Scores are calculated by data management.
- Mini-Mental State Exam Scoring:
The official total score for the MMSE (i.e. the scores used for statistical analyses) are computer generated. Examiners record individual test item scores on the MMSE test form. The one exception is “WORLD” where examiners record the response of subjects in the exact order that it is given by the subject.
For referral purposes, any participant with a drop of 3 points in score since their last exam should be referred to neurology group. A preliminary score can be calculated by Bernadette Shaw to determine if the participant should be referred. A referral form should be completed and given to the Neuro Project Coordinator, ██████████ after the exam. Referral forms can be found in the appendices.
If a participant is referred they may also qualify for a consent form Waiver.
- Consent Form Waiver:
Guidelines dated 3/10/01 verified 3/25/04:
Any subject with MMSE at or above 26 may be presumed competent unless listed otherwise at last evaluation
Any subject with MM:SE below 13 requires use of a Waiver unless seen by a neurologist and declared not demented
MMSEs between 25 and 13 would trigger a decision process. The participants in this category will sign a consent but they may qualify for a waiver. The neurology team will review each case and decide which category to be in (Consent or Waiver).
***Refer to Waiver of lnformed Consent Section of manual for full protocol.***
C. Methods:
- The MMSE asks questions to ascertain cognitive status. Responses are scored:
- 0=incorrect
- 1=correct
- 6=item administered, participant does not answer
- 9=test item not administered/unknown
- If a response is ambiguous, the interviewer records the response in the margin so a decision can be made on its appropriateness. Please refer all questionable responses to the neuropsychologists (i.e. ██████████)
- When a participant is incapacitated by blindness, has a functional disability, is illiterate, or is otherwise unable to respond to a question, the interviewer should specify the problem and questions involved (see "Factors Potentially Affecting Mental Status Testing" later in the section).
D. Expanded Scoring Instructions for Mini-Mental Exam:
Important note: The single exception to scoring 6 for no response is if a participant is in a coma (this circumstance would be encountered in a nursing home visit) In this instance, administer the first item (to establish no response -- give a 0 to the first item if there is no response). (This exception is made to conform with the stroke protocol.)
9 = When test item was not administered (refused or inability because of physical limitations) or subject's response is uninterpretable (response could be correct, but tester is unable to discern the response).
Important note: Sometimes a participant might produce a response that is not a word (i.e. a neologism) but has been responding with intelligible responses on previous items (right or wrong). In this case the items should be scored 0. The key to differentiating a 0 or a 9 is consistency within test. If a person has a speech abnormality, such as aphasia or dysarthria, across all items, most (or many) responses will be unintelligible. If a person is, for example, demented, he/she may produce a flow of intelligible responses with occasional unintelligible responses. A "9" must represent situations in which the EXAMINER is not sure whether (1) the participant responded correctly (because of slurred speech, severe stuttering, etc.), or (2) if the participant has some other factor that prevents test item administration (such as an inability to administer copy this figure test item to a right-handed person who has right-handed paralysis, or to someone who has a visual impairment or inability to hear).
Scoring for Administered Individual Items: (applies only if a test item is administered)
Score 0 for the following reasons:
- Incorrect response
- I don’t know
- Unintelligible response in context of other intelligible responses (see scoring of 9 as well).
- Participants attempted to respond but responds incorrectly (i.e. they are demonstrating that they heard the question and are making an attempt to respond to it).
E. Questions: Scripts and Procedures for Each Question:
Introductory Script: I'm going to start by asking questions that require concentration and memory. Some questions are more difficult than others and some will be asked more than one time.
Read each question on the form.
Record the response on the form.
- What is the date today? (3 = correct score for month (1 pt), day (1 pt) and year (1 pt))
- Ask for the date. Then ask specifically for parts omitted (e.g. Can you also tell me what month, year it is?)
- If participant supplies part or all of the date (e.g. month and day, or month, day, and year), record as appropriate and do not ask those questions again.
- What is the season?
Since distinctions between seasons can be difficult during certain months, one week leeway is allowed on either side of the actual date.
Month Correct Response January Winter February Winter March Winter or Spring April Spring May Spring June Spring or Summer July Summer August Summer September Summer or Fall October Fall November Fall December Fall or Winter - What day of the week is it?
- What town, county, and state are we in?
- Ask the participant what town, county, and state we are in.
- For offsite visits, refer to the section of the manual titled “New England Counties” for a complete list of counties.
- If a participant has Never lived in Framingham, MA. They can give the name of the town, county, and state they live in. The examiner can look up their answer for correctness and score it appropriately.
- What is the name of this place?
- Ask the participant where they are. Any appropriate answer is okay. On q home visits, the examiner can ask, what is the address of this place?
- What floor of the building are we on?
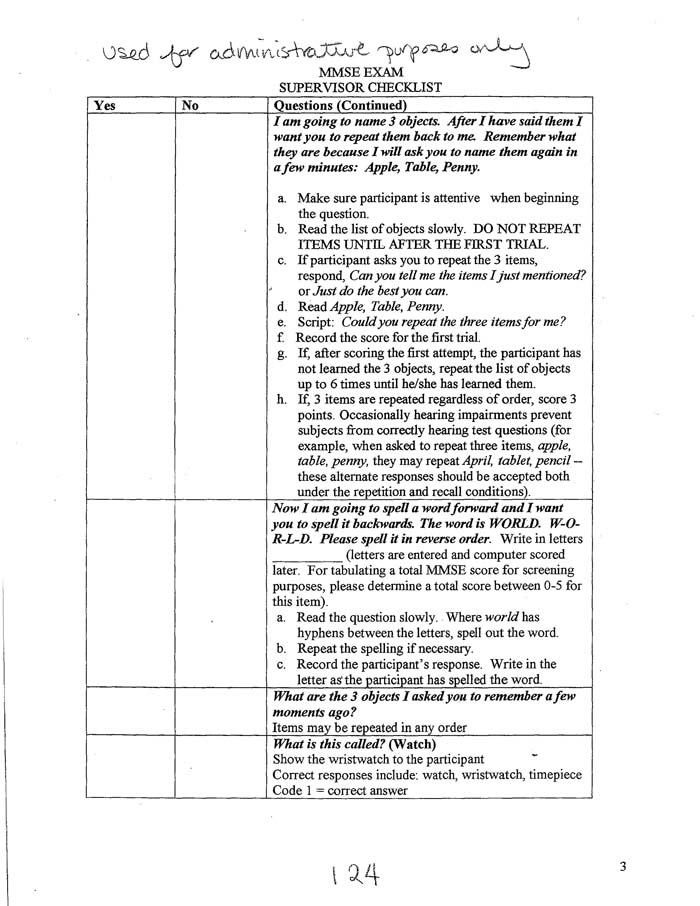
- I am going to name 3 objects. After I have said them I want you to repeat them back to me. Remember what they are
because I will ask you to name them again in a few minutes: Apple, Table, Penny.
- Make sure participant is attentive when beginning the question.
- Read the list of objects slowly. DO NOT REPEAT ITEMS UNTIL AFTER THE FIRST TRIAL.
- If participant asks you to repeat the 3 items, respond, Can you tell me the items I just mentioned? or Just do the best you can.
- Read Apple, Table, Penny.
- Script: Could you repeat the three items for me?
- Record the score for the first trial.
- If, after scoring the first attempt, the participant has not learned the 3 objects, repeat the list of objects up to 6 times until he/she has learned them.
- If, 3 items are repeated regardless of order, score 3 points. Occasionally hearing impairments prevent subjects from correctly hearing test questions (for example, when asked to repeat three items, apple, table, penny, they may repeat April, tablet, pencil -- these alternate responses should be accepted both under the repetition and recall conditions).
- Now I am going to spell a word forward and I want you to spell it backwards. The word is WORLD. W-O-R-L-D. Please
spell it in reverse order. Write in letters __________ (letters are entered and computer scored later). For
tabulating a total MMSE score for screening purposes, please determine a total score between 0-5 for this item).
- Read the question slowly. Where world has hyphens between the letters, spell out the word.
- Repeat the spelling if necessary.
- Record the participant’s response. Write in the letter as the participant has spelled the word.
- What are the 3 objects I asked you to remember a few moments ago?
- Items may be repeated in any order.
- What is this called? (Watch)
- Show the wristwatch to the participant
- Correct responses include: watch, wristwatch, timepiece
- Code 1 = correct answer
- What is this called? (Pencil)
- Show the pencil to the participant. NOTE: the pencil should be a standard sharpened wooden pencil with eraser.
- Correct responses include: Pencil, number 2 pencil
- Code 1 = correct for correct answer.
- Please repeat the following: No ifs, ands or buts.
- Enunciate clearly — include the “S” at the end of ifs, ands, or buts, (if you think the participant heard you but repeated it incorrectly, make a note of what was missed and score 0).
- Allow only one attempt.
- Code 1 = correct when the participant correctly repeated the phrase.
- Code 0 = incorrect when the participant did not repeat the phrase exactly.
Occasionally hearing impairments prevent participants from correctly hearing test questions. In the case of repeating no ifs, ands, or buts, some judgment must be made on the part of the examiner as to whether the participant could hear the “s” or not.
- Please read the following and do what it says.
- Hand participant the “Please Close Your Eyes” card.
- The participant may read the sentence out loud. The task to be coded is the participant’s ability to follow instructions by closing his/her eyes. It is not necessary for the sentence to be read out loud if the participant performs the function properly.
- Code 1 = correct when the participant closes his/her eyes.
- Code 0 = incorrect when the participant did not close his/her eyes.
- Please write a sentence.
- Script: Write any complete sentence on this piece of paper for me.
- Repeat the instructions to participant if necessary.
- Code 1 = correct if the participant wrote a complete sentence as directed.
- Written commands, such as sit down, where the subject is implied, are considered correct responses.
- Spelling and/or punctuation errors are not counted as errors.
- Code 0 = incorrect when the participant did not write a complete sentence as directed.
- Code 1 = if the participant is cognitively able to dictate a sentence but is physically unable
to write it. In this case the examiner should write the dictated sentence and make a note that it
was dictated.
Code 6 = Low vision
- Please copy this drawing.
- Script: Here is a drawing. Please copy the drawing on the same piece of paper.
- If the participant asks if the figures should be drawn separately or together the examiner should respond, Draw the figures as you see them.
- To be correct, each pentagon must have 5 sides, 5 sides that point outward. The two figures must be overlapping.
- The overlap figures must have 4 sides.
- Code “0” = incorrect when the participant’s figure did not match.
- Take this piece of paper in your right hand, fold it in half with both hands, and put it in your lap.
(If participant is unable to use right hand because of physical disability, you can alter instructions to read "Take this piece of paper in your left hand, fold it in half with your left hand, and put it in your lap". The goal is to see whether the subject is able to follow a 3-step command, so this variation to the directions to accommodate subject's physical limitations is allowable.)
- Read the full statement BEFORE handing the paper to the participant.
- DO NOT direct the paper to participant’s right side. Hold the paper in front and have the participant reach out to take it. Observe which hand is used.
- DO NOT repeat instructions or coach participant. Only repeat if the examiner felt it was not heard or if instructions were not given clearly (just repeat the directions in full as they were the first time).
- Score: 1 for each correctly performed act (code 6 if low vision).
F. Factors Potentially Affecting Mental Status Testing
The examiner’s impression for Cohort Cycle 28 will include the following:
| NO | YES | MAYBE | UNKNOWN | |
|---|---|---|---|---|
| 0 | 1 | 2 | 9 | Illiteracy or low education |
| 0 | 1 | 2 | 9 | Not fluent in English |
| 0 | 1 | 2 | 9 | Poor eyesight |
| 0 | 1 | 2 | 9 | Poor hearing |
| 0 | 1 | 2 | 9 | Paralysis |
| 0 | 1 | 2 | 9 | Depression/Possible Depression |
| 0 | 1 | 2 | 9 | Aphasia |
| 0 | 1 | 2 | 9 | Coma |
| 0 | 1 | 2 | 9 | Parkinsonism or neurological |
| 0 | 1 | 2 | 9 | Impairment |
| 0 | 1 | 2 | 9 | Other |
PLEASE CLOSE YOUR EYES
Sociodemographics and Subjective Health
This is a self-reported form. If not self-reported the Proxy Section of the exam form must be completed.
A. Socio-demographics
- Where do you live?
- Coding
- 0 = Private residence
- 1 = Nursing home
- 2 = Other institution, such as an assisted living facility or retirement community
- 9 = Unknown
- Does anyone live with you? (NOTE: Code nursing home resident as NO to these questions.)
- Coding
- 0 = No
- 1 = Yes
- 9 = Unknown
NOTE: If the answer to the above question was 0 or 9 you may skip the following section. If the answer was yes, the examiner needs to determine who lives in the same household. It is important to ask whether others live in the same household for < 3 months per year or > 3 months per year. The list is:
- Spouse
- Significant Other
- Children
- Friends
- Relatives
- Pets
- Coding
- 0 = No
- 1 = Yes, less than 3 months per year
- 2 = Yes, more than 3 months per year
- 9 = Unknown
- Are you Currently working at a paying job or doing unpaid volunteer or community work?
- Coding
- 0 = No
- 1 = Yes,
- 9 = Unknown
- During the past 6 months (180 days) how many days were you so sick that you were unable to carry out your usual
activities?
- Coding
- 999 = Unknown
B. Subjective Health
The following two questions MAY NOT be answered by a proxy.
- In general, how is your health now?
- Coding
- 1 = Excellent
- 2 = Good
- 3 = Fair
- 4 = Poor
- 9 = Unknown
- Compare your health to most people your own age:
- Coding
- 1 = Better
- 2 = About the same
- 3 = Worse than most people your own age
- 9 = Unknown
4. Activities of Daily Living Self Reported Performance:
Rosow-Breslau Questions
A. Rationale & Background
Respondents' self-assessments of health may raise questions about the validity of such judgments. However, we are not interested in the literal details of people's medical condition as much as in the behavioral consequences, their physical capacity for role fulfillment and social participation. We are primarily concerned with the functional health which old people report, i.e., the degree to which they claim they can manage adequately or are restricted in their activities because of their physical condition or capacity. Breslau, M, Rosow, I: A Guttman Health Scale for the Aged 556-559
B. Methods
The method of assessing physical functioning is self-report. The questions assess the degree of difficulty that a person has performing a specific activity. This form has several important purposes:
- These data will enable us to assess the level of independence and function in the study population.
- It is hypothesized that impairments of physical function may be a risk factor for cardiovascular end points and progression of disease.
- It will measure loss of physical functioning as a consequence of cardiovascular disease.
C. Procedures
Questions:
- Coding
- 0 = No, unable to do
- 1 = Yes, independent
- 2 = Does not do
- 9 = Unknown
- Are you able to do heavy work around the house, like shovel snow or wash windows, walls, or floors without help? (Scrub floors, wash windows, rake leaves, and mow lawn). (Note: Code 2 if person does not do this activity).
- Are you able to walk half a mile without help? (Walk one half mile or 4-6 blocks without stopping for more than 5 minutes). (Note: Code 2 if person does not do this activity).
Questions 3 & 4 should be asked exactly how they are listed on the exam form.
b. Nagi Questionnaire
Tech-Administered
- Method
Show and explain the answer key before administering the questionnaire. The participant is to choose one of the following answers for each activity:
- No Difficulty
- A Little Difficulty
- Some Difficulty
- A Lot of Difficulty
- Unable to Do
- Don't Do on MD Orders
Unable to Assess Difficulty Because Not Done as Part of Daily Activities
- Procedure
- Start with, For each activity, tell me whether you have No Difficulty, A little Difficulty, Some Difficulty, A Lot of Difficulty, if you are Unable to do it, if you Do not do it on MD Orders or Institutional Orders, or if you are Unable to Assess Difficulty Because the activity is not done as part of your daily activities.
- Read each activity separately, and go through the level of difficulty for each one until the participant understands the response choices.
Notes:
"Institutional Orders" is any facility that assists a person with their daily activities, (ex. Nursing homes, assisted living facilities, etc.)
Do not ask these questions if the participant is cognitively impaired; proxy may answer these questions.
No Difficulty
A Little Difficulty
Some Difficulty
A Lot of Difficulty
Unable to Do
Don't Do on MD Orders or Institutional Orders
Unable to Assess Difficulty Because Not Done as Part of Daily Activities
KATZ: Activities of Daily Living
- Background and Rationale:
This section is designed to assess the following spectrum of physical functioning. This section assesses:
- General level of physical functioning and mobility
- Ability to carry out instrumental activities of daily living
- Ability to carry out activities of daily living
- Framingham Disability Index
- Activities of Daily Living (Title on top of form):
Part 1:
Ask the participant, During the course of a normal day, can you do the following activities independently or do you need human assistance or the use of a device?
The answers will be coded by the examiner as:
- 0 = No help needed, independent
- 1 = Uses device, independent
- 2 = Human assistance needed, minimally dependent
- 3 = Dependent
- 4 = Does not do during a normal day
- 9 = Unknown
NOTE: With a nursing home visit, the participant's chart may be used to verify or to obtain accurate information on ADL's. If information is obtained from the nursing home chart or staff then proxy information on screen must be completed.
The activities include:
- Dressing
- Undressing and redressing
- Picking out clothes, dress oneself including buttoning, fastening, etc.
- Devices such as: velcro, elastic laces.
- Bathing
- Including getting in and out of tub or shower
- Getting water, soap, towel and other necessary items and wash oneself
- Devices such as: bath chair, long handled sponge, hand held shower, safety bars.
- Eating
- Able to eat from a dish and drink from a cup
- Devices such as: rocking knife, spork, long straw, plate guard.
- Transferring
- Getting in and out of a chair
- Arising from a sitting position to a standing position and back
- Devices such as: sliding board, grab bars, special seat.
- Toileting activities
- Using the bathroom facilities and handling clothing
- Devices such as: special toilet seat, commode.
- Bladder continence
- Ask if person has "accidents" (code =5 if use special product)
- Devices such as: external catheter, drainage bags, ileal appliance, protective device.
- Bowel continence
- Ask if person has "accidents" (code=5 if use special products)
- Devices such as: suppositories, bedpan, regular enemas.
- Walking on a level surface about 50 yards
- Devices such as: cane, crutches, or walker.
- Walking up and down one flight of stairs
- Devices such as: handrail, cane.
No Help Needed
Uses Device
Human Assistance needed
Dependent
Do no do during a normal day
Compensatory Strategies for Walking in the Home
Do not administer to Nursing home residents
- Method
Tech administered-
Coding procedure as follows:
- 0 = No
- 1 = Yes
- 8 = Refused
- 88 = n/a, reside in assisted living
- 9 = Don't Know
- Procedure
- Read each question to the participant and record answer using the appropriate code.
- Questions:
- Is there a step to go into your (entry way step)?
- In you home, are the bedrooms, bathrooms, and kitchen all on the same floor?
- When you walk, do you use a cane at home?
- When you walk, do you use a walker at home?
- Do you use a wheel chair at home?
- When you walk, do you reach out for or hold on to the furniture or walls at home?
- When you walk, do you hold on to another person at home?
- When you walk in the dark, do you hold on to furniture or walls?
- When you walk in the dark, do you hold on to another person?
IADL'S-Instrumental Activities of Daily Living
Tech-Administered
- Background and Rationale:
The Lawton IADL's is used to assess the ability to carry out instrumental activities of daily living.
- Instrumental Activities of Daily Living are coded by the examiner as:
- 01 = Completely Unable
- 02 = With Some Help
- 03 = Without Help
The Participant uses the prompt card when asking these questions. The participant will choose one answer from the prompt card that best describes their ability to cany out the activities.
- The IADL questions are NOT administered to nursing home residents.
Questions:
| 1) | Can you use the phone: |
| 2) | Can you get to places out of walking distance: |
| 3) | Can you go shopping for groceries: |
| 4) | Can you prepare your own meals: |
| 5) | Can you do your own housework: |
| 6) | Can you do your own handyman work: |
| 7) | Can you do your own laundry: |
| 8a) | Do you take medicines or use any medications: |
| 8b) | Do you take your own medicines: |
| 8c) | If you had to take medicine, could you do it: |
| 9) | Can you manage your own money: |
Completely Unable
With Some Help
Without Help
CES-D Scale
A. Rationale and Background:
The Center for Epidemiologic Studies Depression Scale (CES-D) was developed for use in epidemiologic research of depressive symptomatology in the general population. It was designed as a screening instrument to elicit symptoms associated with depression. It is intended to document the presence and severity of depressive symptoms but is not intended to make clinical diagnosis. It assesses the current state of the subject by focusing on symptomatology in the past week.
Note: The depression questions used in the NHANES 1 survey were the 20-item set of the CES-D developed and validated by the Center for Epidemiologic Studies, National Institute of Mental Health (NIMH).
The scale is given at each exam. The scale is not given if the patient is: sedated, aphasic, non-English speaking, or uncooperative.
B. Procedure:
- Each question is read to the participant who responds with one of four answers.
- Response alternatives should be printed on paper which is placed in front of the participant for reference.
- Each category of response should be explained to the participant prior to administering the scale.
- If the participant is unable to read the response sheets, the interviewer should read each response as well as the question referring to their feelings in the past week.
- Be sure the participant understands that the questions refer to his/her feelings only during the past week.
C. CES-D Scoring:
Each item has a range of four response options which indicated how often the survey examinee had felt that way during the past week:
| Code | Response Option |
|---|---|
| 0 | Rarely or none of the time (less than 1 day) |
| 1 | Some or a little of the time (1-2 days) |
| 2 | Occasionally or a moderate amount of the time (3-4 days) |
| 3 | Most or all of the time (5-7 days) |
Questionnaire items 4, 8, 12, and 16 were worded in a positive (i.e., nondepressed) direction. The other 16 scale items were worded in a negative direction to elicit depressive symptomatology directly. To score the CES-D, the sense of the fours positive questionnaire items was reversed by subtracting their coded value (indicating the response option selected) from 3. Then the coded values for all 20 items were summed into a total score. The range of possible scores was 0-60. The final score is calculated by the computer.
D. Methods:
The CES-D Questionnaire consists of 20 questions. Since it is a scale for depression, it must be completed using responses by the participant, not a proxy.
SCRIPT: The questions below ask about your feelings. For each of the following statements, please say if you felt that way during the past week.
- Hand the response sheet to the participant and explain the response options. The following definitions should be given:
- Code
- Rarely or none of the time (< one full day)
- Some or a little of the time (1 to 2 days in the past week)
- Occasionally or moderate amount of time (3 to 4 days in the past week, or about 1/2 the time)
- Most of the time (5 to 7 days in the past week)
If participant answers YES to a given statement, repeat the above responses to get a correct answer.
- Read each item as it is written on the form, prefacing each question with the statement During the past week,
then continuing with the response categories. For example:
SCRIPT: During the past week I was bothered by things that usually don't bother me. Did you feel that way rarely or none of the time, some or a little of the time, occasionally or moderate amount of time, or most or all of the time?
- Discontinue reading the responses when the participant provides a response before you are finished. On the next item, however, again begin to read the entire set of responses.
- Code 9 = Refused or Do not know is used when:
- The question was asked, but the participant chooses not to answer. For example, response was I would rather not say, or Go on to the next question.
- The question was asked, but the participant does not know, does not remember, or does not understand the statement.
** If "unknown" is used more than 4 times on the questionnaire it is no longer considered valid for research. Do your best to have the participant give you an answer listed on the response key.**
- Circle the response on the form.
- When the participant asks about the meaning of any item or tries to qualify a statement, simply repeat the statement. For
example:
Participant: What do you mean by bothered?
Interviewer: I was bothered by things that usually don't bother me. Did you feel that way rarely or none of the time, some or a little of the time, occasionally or moderate amount of time, or most or all of the time during the past week?
- When the participant still asks about the meaning or says he/she does not understand, check 9 = refused or do not know. Do not try to interpret the statement for the participant.
Rarely or none of the time (Less than 1 day)
Some or a little of the time (1-2 days)
Occasionally or moderate amount of time (3-4 days)
Most or all of the time (5-7 days)
Berkman Social Network Questionnaire
A. Background & Rationale
The intent of the Berkman Social Network Questionnaire (BSNQ) is to determine the participant's social support systems both from friends and relatives. Printed response sheets in large font should be given to the participant to help them better understand and answer the questions.
B. Procedures
Before administering the BSNQ, read the following statement, The next questions ask about your social support. Please tell me the response that most closely describes your current situation.
The first four (4) questions should be answered with the following responses:
- None
- 1 or 2
- 3 to 5
- 6 to 9
- 10 or more
- Unknown*
* Unknown can be used only when participant is unable to answer, refuses, or if the question was not asked. The participant is not told this is an option for an answer.
- How many close friends do you have; people that you feel at ease with and can talk to about private
matters?
The response should be based on whom the participant can talk to, in person and telephone contact.
- How many of these close friends do you see at least once a month?
This question refers only to friends the participant has been in physical contact with, or spoken to in person. Talking on the phone should not be included in the scoring. This separates how often the participant talks to people versus physically meeting with them.
- How many relatives do you have; people that you feel at ease with and can talk to about private
matters?
The response should be based on relatives whom the participant can talk to, in person and telephone contact
- How many of these relatives do you see at least once a month?
This question refers only to relatives the participant has been in physical contact with, or spoken to in person. Talking on the phone should not be included in the scoring. This separates how often the participant talks to people versus physically meeting with them.
- Do you participate in any groups such as a senior center, social or work group, religious connected group, self-help
group, or charity, public service or community group?
This can include volunteer work or groups where the participant physically works or joins others. Again, it does not include telephone contact.
- Coding
- 0 = No
- 1 = Yes
- 9 = Unknown
- About how often do you go to religious meetings or services?
The answer should reflect how often the participant goes to meetings or services. Watching services on television should not be scored as having gone to meetings or services. The intent of this question is how often the person joins others in this particular activity.
- Coding
- 1 - 9
- See Exam Form
Question 7 asks about insurance coverage.
| 7. | Do you have health insurance other than Medicare or Medicaid? The intent of questions 8-12 is for friends and family, not mental health specialists. They should be answered with the following responses:
|
* Unknown can be used only when participant is unable to answer, refuses, or if the question was not asked. The participant is not told this is an option for an answer.
The remaining questions should be asked exactly as they are printed on the page. The technician should not try to explain them.
None
1 or 2
3 to 5
6 to 9
10 or more
None of the time
A little of the time
Some of the time
Most of the time
All of the time
Leisure Time Cognitive & Physical Activities
- Background and Rationale
The intent of the Leisure Time Cognitive and Physical Activities questionnaire is to determine whether increased participation in leisure activities lowers the risk of dementia or participation in leisure activities declines during the preclinical phase of dementia. Response sheets, using large print should be given to the participant to help them better understand and answer the questions.
- Procedures
- Show and explain the answer key before administering the questionnaire. The participant is to choose
one of the following answers for each activity:
- Never
- Daily (7 days/week)
- Several Days Per Week (2-6 days/week)
- Once Weekly (1 day/week)
- Monthly (once a month)
- Occasionally (less than once a month)
- Ask each question individually. Start with, During the past year, how often have you participated in the following leisure time activities?
- These questions can be answered by the participants' proxy. For nursing home visits this information can also be taken from the up-to- date Minimum Data Sheets.
- This questionnaire can be asked of all participants regardless of their cognitive status.
- Show and explain the answer key before administering the questionnaire. The participant is to choose
one of the following answers for each activity:
Note:
"Group exercises" is considered done as a group, not exercise done alone.
"Crossword Puzzles" Include word searches
"Reading books/Newspapers" If the participant is legally blind but listens to books on tape, this is considered as a book on tape reader. It involves the same process once it migrates to the brain: attention, memory, and sequence.
Never
Daily (7 days per week)
Several Days Per Week (2-6 days)
Once Weekly (1 day per week)
Monthly (Once a month)
Occasionally (less than once a month)
9. Other
Use of Nursing and Community Services
These questions are meant to gather information on use of nursing and community services in the interim.
Question 1: Have you been admitted to a nursing home (or skilled facility) since your last exam or medical history update?
Question 2: Since your last exam, have you been visited by a nursing service, or used home, community, or outpatient programs?
If a participant moved into a nursing home prior to the two year interim, then the first question 1 is 0 = No. If the first question is No because the participant has been living in a nursing home for more than 2 years, the rest of Nursing and Community Services should be coded as 0 = No.
Falls and Fractures
- Falls
Ask the participant, Since your last exam have you accidentally fallen and hit the floor or ground?
- Coding
- 0 = No
- 1 = Yes
- 2 = Maybe
- 9 = Unknown
If yes, ask How many times did you fall in the past year?
NOTE: Falls during sports activities are not coded.
- Fractures
Ask the participant, Since your last exam or medical history update have you broken any bones?
- Coding
- 0 = No
- 1 = Yes
- 2 = Maybe
- 9 = Unknown
List the location of each fracture individually (3 spaces available)
Procedure Sheet & Exit Interview
(Clinic & Offsite)
On the back of the Numerical Data Sheet there is a Procedure Sheet and Exit Interview.
- Procedure Sheet
Prior to the exit interview staff should check the participant chart to see what procedures were completed. The staff should then fill in the procedure sheet using the corresponding codes.
- Exit Interview
Once the procedures are reviewed an exit inteIView is to be completed with the participant. During the exit interview:
- Check the referral tracking sheet (complete with your ID number and any adverse events in clinic) and review with the participant any referral recommendations.
- Make sure the participant leaves the clinic area with all of their belongings; and
- Ask for feedback from the participant on how they felt about their examination.
- Enter one of the following codes:
- 0=No Feedback
- 1=Positive Feedback
- 2=Negative Feedback
- 3=Other
- Write in any comments that are made.
- Enter one of the following codes:
- Proxy Information
Whenever someone else is providing information about a participant that is collected on the forms, this person is considered a "proxy". When an offsite visit is to a nursing home frequently a nurse familiar with the participant will be the proxy. Sometimes during offsite exams there will be more than one proxy. For example a Home Health Aid may answer all of the questions relating to ADL' s, and the daughter may answer all of the medical questions. In cases like these, record information for both proxies on the numerical data sheet.
Important: The proxy that is designated by the participant as their FHS proxy does not have to be the same person as the one listed on the numerical data sheet.
Section V. Physician-Administered Medical History
Medical History
The forms from the participant's last examination are provided in a folder behind the current medical history form. The medical history taken from the participant is an update from the Heart Study' s last contact with the participant (based on the date of the last Health History Update or last examination). The examiner should also refer to the Summary of Findings form in the participant's chart to verify whether a medical encounter is new or has already been identified. This form records the outcome of all Endpoint reviews and therefore documents all cardiovascular disease events adjudicated by the study.
The health status page may have incomplete data on medical encounters. Be sure to clarify any missing information and record it under medical encounters on the first page of the medical history form.
Medical History Form
1st Examiner Prefix
- (0=MD, 1=Tech, for OFFSITE visit)
Hospitalization in interim
- A hospitalization is considered an overnight stay.
- If the participant was in the Emergency Room (E.R.) and then admitted, the event would be considered only for hospitalization and not as E.R visit.
E.R. visit in interim
- An emergency room visit is when the person is both admitted to and discharged from the emergency room the same day.
Day surgery in interim
- Day surgery is a surgical procedure performed on an out-patient basis either in an ambulatory surgery department of a hospital or in a physician's office.
- The person is in and out the same day.
Major illness with visit to the doctor in interim
- Illness with visit to physician is defined as a visit outside of a regular check-up. It can be further clarified by defining it as a visit to the doctor for a specific reason.
- It is imperative that the reason for the visit be documented.
Check-up in interim by doctor
- A check-up is considered to be a routine visit.
Details of all hospitalizations, ER visits, day surgery, and physician visits must be provided as follows:
- Medical Encounter
Write the details about the medical event. If the participant cannot provide a "medical condition", symptoms leading to the medical encounter should be listed (for example, chest pain, shortness of breath).
- Month/Year
Record the date of the medical encounter. People often cannot recall the exact month or even the year. Trying to couple the event with a season or holiday sometimes helps.
- Site of the hospital or office
The hospital and the city and state are most important.
- Doctor
Record the name of the physician seen. If the participant sees a physician's assistant or a nurse practitioner in the physician's office, obtain both names.
Note: If FHS needs outside hospital records, please obtain details: mo/yr, hospital site.
Medical History - Prescription and Non-Prescription Medication
On home visits, the participant is asked to show the medical technician his/her medication bottles including over-the counter preparations. In the case of a nursing home visit, the technician should record the medications from the participant's medication orders in their nursing home chart.
Copy the name of the medication, the strength including units, and the total number of doses per day/week/month. Include pills, skin patches, eye drops, creams, salves, injections. Include herbal, alternative, and soy-based preparations.
Print the medication name, strength, number per day/week/month, and if taken PRN.
***List ONLY medications taken regularly in the past month/ongoing medications***
Medical History
The physician or off-site medical technician will obtain an interim medical history using the standardized exam 29 form. The questions should be asked exactly as written on the form and the participant's response recorded according to the response choices provided on the form. In addition a comment area is provided on the form to record a narrative account of cardiovascular symptoms including chest pain, shortness of breath, syncope, exertional leg discomfort and cerebrovascular symptoms. It is critical that a narrative be provided to clarify the symptoms for investigators adjudicating events in Endpoint Review.
It is also critical to record all health care visits (physician, ER, hospital) the participant has had for the symptom. Outside medical records will be obtained to verify the participant's account of their medical condition.
Additional instructions for obtaining the medical history and properly coding the participant's responses are as follows.
Alcohol Consumption (screen MD06)
Code number of alcoholic beverages as EITHER weekly OR monthly as appropriate.
Chest pain (screen MD09)
When the participant states that they have not experienced any chest discomfort, clarify further using the terms chest pain, chest tightness, chest pressure.
If the participant states that they never used Nitroglycerin as a way to relieve-the discomfort be sure to code as 8= not tried, rather than 0= no relief.
Cerebrovascular, Neurological and Venous Diseases (screen MD11)
It is important to stress that these CVA symptoms are sudden, not a gradual progression of a symptom.
- Sudden Muscular Weakness
Since (date of last FHS exam) until today, have you experienced any sudden muscular weakness? For example, face drooping or weakness, parlicularly on one side of your body.
- Sudden Speech Difficulty
Since (date of last FHS exam) until today, have you experienced any sudden difficulty with your speech such as understanding spoken words or trouble speaking?
- Sudden Visual Defect
Since (date of last FHS exam) until today, have you experienced any sudden visual defect?
- Sudden Double Vision
Since (date of last FHS exam) until today, have you experienced any double vision?
- Sudden Loss of Vision in One Eye
Since (date of last FHS exam) until today, have you experienced any sudden loss of vision in one eye, like a shade coming down over your eye?
- Sudden Numbness, Tingling
Since (date of last FHS exam) until today, have you experienced any numbness or tingling on one side of your face or one side of your body?
If the participant answers yes, ask is numbness and tingling positional?
CVD Procedures (MD14)
The participant is queried regarding CVD procedures since the last Heart Study contact.
If the participant has had more than one procedure of a particular type code only the first procedure and list all other procedures in the comment section.
Clarify the procedure list for the participant as follows:
Heart valvular surgery
Have you had surgery on your heart valves?
Exercise tolerance test
Have you had an exercise stress test or a treadmill test of your heart?
Coronary Arteriogram
This test is an invasive test done in the hospital. An x-ray is taken of your arteries after you receive an injection of a dye that outlines the blood vessels of your heart.
Coronary artery angioplasty/stent/PCI
Angioplasty is a procedure in which a balloon is used to open a narrowed or blocked artery in your heart. (This is also known as Percutaneous Coronary Intervention (PCI)).
A stent is a wire mesh tube that is placed in the artery to hold it open. The stent is usually placed in the artery during angioplasty.
Coronary bypass surgery
Have you had bypass surgery also known as CABG (coronary artery bypass grafting)?
During bypass surgery the diseased section of your coronary arteries are bypassed with a healthy artery or a vein in order to increase blood flow to your heart muscle.
Permanent pacemaker insertion
Have you had a pacemaker inserted? A pacemaker is used to replace the function of the natural pacemaker in your heart when your heart is beating too slowly. Permanent pacemakers are surgically placed into the chest through a small incision.
Carotid artery surgery
The carotid artery is located in your neck and carries blood and oxygen to your brain. Carotid artery surgery is a surgical procedure to restore adequate blood flow to your brain. A stent is inserted into the carotid artery to open a narrowed or blocked area of the artery to help maintain an adequate blood flow to the brain.
Thoracic aorta surgery
Have you had surgery on your aorta- the large blood vessel coming from your heart? This surgery is done to repair the aorta for example when there is an aneurysm (a weaknening or bulge in the wall of the aorta).
Abdominal aorta surgery
Have you had surgery on the large blood vessel in your abdomen (belly) called the aorta?
This surgery would be done to repair a problem such as an aneurysm (weakening or bulge in the wall of the artery) or blockage in the aorta.
Femoral or lower extremity surgery
Have you had any surgery to improve the circulation in your legs such as bypass surgery or angioplasty?
Lower extremity amputation
Have you had an amputation of part of your leg or foot?
Other cardiovascular procedures (write in)
Have you had any other tests or procedures on your heart or blood vessels?
For Offsite visits a technician will complete the physician medical history portion of the exam. The form will then be reviewed and completed by a physician. ALL physicians will be asked to share in this responsibility during their assigned clinic time. The physician chart review includes the following:
| 1. | Review the physician exam form and complete all physician opinions regarding endpoints (AP, MI, CI, CHF, stroke, syncope, and IC) based upon the coded and written narratives the technician obtained at the time of the visit. |
| 2. | Code the ECG. The MD ECG reading should be added to the letter to the personal physician. |
| 3. | Complete the "clinical diagnostic impression" |
| 3. | Review the letter to the personal physician making any deletions/additions/changes in medical terminology that are required. |
| 4. | Return the chart the SAME day to the technician or the clinic tech at the board in clinic. |
NOTE: The area entitled "Examiner's Opinion" at the bottom of every page is not to be completed by the medical technician but by the physician reviewing the chart in clinic.
Physician-Administered Blood Pressure
A. Equipment:
- One standard Litman stethoscope tubing and earpieces with bell: Classic II 3M
- One standard mercury column sphygmomanometer: Baumanometer (clinic)
- Aneroid sphygmomanometer (off-site)
- BP cuffs in four sizes (All Latex Free)
- Thigh adult cuff
- Large adult cuff
- Regular adult cuff
- Pediatric cuff
B. Blood Pressure Cuff Placement:
- Bare participant's left arm to above the point of the shoulder.
- Determine correct cuff size using guidelines inside the cuff.
- Palpate the brachial artery.
- With participant seated, place the appropriate cuff around the upper left arm. The midpoint of the length of the bladder should lie over the brachial artery. Each cuff has an artery marker. The mid-height of the cuff should be at heart level.
- Place the lower edge of the cuff, with its tubing connections, about one inch (1") above the natural crease across the inner aspect of the elbow.
- Wrap the cuff snugly about the arm, with the palm of the participant's hand turned upward.
- If the subject has had a left-sided mastectomy, the right arm may be used for blood pressure measurement. If right arm is used, note it on the form.
C. Determination of Maximal Inflation Level
For each participant, determine the maximal inflation level, or the pressure to which the cuff is to be inflated for blood pressure measurement. This assures that the cuff pressure at the start of the reading exceeds the systolic blood pressure and thus allows the first Kortokoff sound to be heard.
- Attach the cuff tubing to the sphygmomanometer.
- Palpate the radial pulse.
- Inflate the cuff rapidly until the radial pulse is no longer felt (palpated systolic pressure) by inflating rapidly to 70 mmHg, then inflating by 10mmHg increments.
- Deflate the cuff quickly and completely.
- The maximal inflation level is 30 mmHg above the palpated systolic pressure.
D. Guidelines for Accurate Blood Pressure Readings:
- The participant should be in a seated position for at least 5 minutes before the blood pressure is measured.
- All readings are made to the nearest even digit.
- Any reading which appears to fall exactly between marking on the mercury column should be read to the next higher marking (i.e. 2, 4, 6, 8, or 0).
- All readings are made to the top of the meniscus, the rounded surface of the mercury column.
- When the pressure is released quickly from a high level, a vacuum is formed above the mercury and the meniscus is distorted. Allow a few moments for it to reappear before reading the manometer.
For offsite Blood Pressures: Check that the needle is at the zero mark at the start and the end of the measurement. Place the manometer in direct line of sight with the eye on a line perpendicular to the center of the face of the gauge.
E. Blood Pressure Readings:
- Following any previous inflation, wait at least 30 seconds after the cuff has completely deflated.
- By closing the thumb valve and squeezing the bulb, inflate the cuff at a rapid but smooth continuous rate to the maximal inflation level (30 mrnHg above palpated systolic pressure).
- The examiner's eyes should be level with the mid-range of the manometer scale and focused at the level to which the pressure will be raised.
- Open the thumb valve slightly. Allow the cuff to deflate, maintaining a constant rate of deflation at approximately 2 mmHg per second.
- Using the bell of the stethoscope, listen throughout the entire range of deflation, from the maximum pressure past the systolic reading (the pressure where the FIRST regular sound is heard), until 10 mmHg BELOW the level of the diastolic reading (that is, 10 mmHg below the level at which the LAST regular sound is heard).
- Deflate the cuff fully by opening the thumb valve.
- Remove the stethoscope. Neatly enter systolic and diastolic readings in the spaces provided on the form.
ECG CODING FOR FRAMINGHAM HEART STUDY EXAMINATIONS
A. General Comments:
Although the computerized ECGs which are recorded in clinic include measurements of rate, intervals and axis, it is important that the examining l\ID carefully examine the ECG and record these features on the coding forms. Your measurements (not those made by the computer) form the basis of the official ECG interpretation.
An important rule to remember: Please ask for help when you are unsure about interpretation of ECGs or our methods of coding. Be sure to always look at the old ECG for interim changes.
B. Heart Rate:
Each exam room is equipped with a rate stick with which heart rate can be measured. (The computer does a good job with this measurement).
C. Intervals:
PR, QRS and QT intervals are measured in hundredths of a second based upon examination of the ECG recording. (Lead II should be used when possible for these measurements). A QRS of 0.08 seconds is coded as 08.
D. QRS Angle"
This refers to frontal plane axis in degrees. Each exam room is equipped with a hexaxial device for measuring QRS axis. (The computer does a good job with this measurement).
E. Conduction Abnormality:
- IV Block
This refers to right and left bundle branch block. Note that the code 1 is used for incomplete BBB and 2 is for complete BBB. For complete BBB the QRS interval should be .12 sec or greater. When the QRS is prolonged, but the pattern is not that of right or left BBB, the indeterminate IV block is coded as follows: 1 =QRS .12 or greater, 2=QRS of .11 or .10. Remember that the measurements of QRS duration are those made by the examining physician and not by the computer. An RSR' pattern in the absence of QRS prolongation should be coded as normal. When an RSR' pattern occurs with a QRS duration of .09 sec or greater it represents incomplete RBBB.
- Hemi block
1=left anterior. This is present when the QRS axis is -30 or less and small q wave is present in lead I.
2=left posterior. QRS axis is >90 and small q is present in AVF, in absence of evidence of right ventricular hypertrophy.
- Fascicular block
1=bifascicular. A) If complete RBBB + (1st degree AV block or a hemiblock) are present. B) Complete LBBB.
2=trifascicular. If RBBB + hemiblock + 1st degree AV block. Or LBBB + 1st degree AV block.
- AV Block
1st degree when QRS duration is .20 seconds or greater (measured in lead II).
2nd degree when some P waves are not conducted. This comes in tow forms a) Mobitz I. When progressive PR prolongation precedes the dropped P wave and b) Mobitz II when QRS complexes are dropped without prior PR prolongation. AV dissociation occurs when P waves are QRS complexes march out independent of each other.
- WPW
A short PR intervals is present (typically .12 seconds or less) and a slurred upstroke of the QRS is present (so called delta wave). When these features are both fulfilled, WPW=1. When the PR is .12 or less and a delta wave is possibly present, or when a delta wave is present but the PR is marginally short .13 to .14 seconds, WPW=2.
- Atrial Enlargement:
- Right Atrial Abnormality
The P wave is inferior leads is peaked with a height of 2.5 mm.
- Morris P wave
The terminal portion of the V wave in lead VI is inverted and measures at least 1mm by 1mm (at normal standardization). This reflects left atrial enlargement.
- Right Atrial Abnormality
- Myocardial Infarction
This is determined on the basis of the appearance of wide (.04 seconds) or deep (1/4 the height or the R wave) q waves. All tracings should be compared to the prior exam ECG which is always provided. The appearance of new, but small q waves should also be regarded as suggestive of MI. Loss ofR waves in leads where they were previously present (see prior exam's ECG) should also raise suspicion of MI. A posterior MI is present when R > S in VI, R is . 04 seconds in duration, and an upright T wave is recorded in that lead. When criteria are largely, but incompletely fulfilled be sure to code this item as maybe!
- Maximum I Wave Amplitude <-5mm
This refers to giant inverted T waves at least 5mm deep. This condition is occasionally seen in hypertrophic cardiomyopathy.
- Left Ventricular Hypertrophy
Be sure to carefully code each of the voltage criteria individually. Definite LVH is present when increased voltage is present together with a strain pattern (downsloping ST). Possible LVH is present when voltage criteria are fulfilled but only mild ST-T abnormalities (flattening) are noted. For cohort Exam 21, we have a separate code for LVH by voltage only. When complete BBB is present, LVH should be coded as unknown (9).
- Right Ventricular Hypertrophy
Definite RVH is present when increased R wave voltage is present in VI and increase S wave voltage is present in V5 in the absence of RBBB. The sum of RV1 + SV5 should be at least 10.5mm.
- Arrhythmias
The presence of rhythm disturbances should be made on the basis of examination of the ½ speed rhythm strip which accompanies each ECG. This represents a simultaneous 3 lead recording of the entire 12-lead ECG.
Referral Tracking
- Was further medical evaluation recommended for this participant?
This question is to be answered by the physician completing the chart.
In addition to the physician writing in their physician ID number on the form, he/she will code this question using the following codes:
- Coding
- 0= No
- 1= Yes
- 9= Unknown
If No, go to the next section.
If Yes, the MD is to code the reason for further evaluation:
- Blood Pressure result __/__
- Phone call > 200/110
- Expedite ≥180/100
- Elevated > 140/90
Write in abnormality or identified medical problem
- ECG abnormality ______________
- Clinical Physician ______________
- Other ______________
- Was there an adverse event in clinic/offsite exam that does not require further medical evaluation?
- This questions is to be completed by a staff member completing the exit interview.
- In addition to the staff member writing in their technician ID number on the form, he/she will code this question
using the following codes:
- Coding
- 0= No
- 1= Yes
- 9= Unknown
- If Yes, write in any comments and photocopy this form and give to ██████████
- Was a FHS physician contacted during the examination due to adverse exam findings?
- This question is to be completed at off site exams only by the staff member completing interview.
- In addition to the staff member writing in their technician ID number on the form, he/she will code this question
using the following codes:
- Coding
- 0= No
- 1= Yes
- 9= Unknown
- If Yes, write in any comments regarding the telephone encounter.
- Method used to inform participants of need for further medical evaluation:
- This information is to be coded by the physician completed the chart.
- Circle ALL that apply
- 1= Face-to-face in clinic
- 2= Phone call
- 3= Result letter
- 4= Other
- This information is to be coded by the physician completed the chart.
- Method used to inform participant's personal physician of need for further medical evaluation:
- This information is to be coded by the physician completed the chart.
- Circle ALL that apply
- 1= Phone call
- 2= Results letter mailed
- 3= Results letter FAX' d
- 4= Other
- Date referral made: __--__--____ Use 4 digits for year
- ID number of person completing this referral: __________
Notes documenting conversation with participant or participant's personal
physician: __________________________________________________
_______________________________________________________
_______________________________________________________ - This information is to be coded by the physician completed the chart.
Section VI. Offsite Examination
Protocol for Scheduling Offsite Visits
Before making a call, check the roster.
- On the main screen, check the comment line and Consent Status and C.S. Date.
- Check the Referral screen (F14 or shift F4) for additional comments.
- Check the Booking screen (F12 or shift F2) for scheduled exams, exam history, and the participant's age.
If an appointment is already scheduled for the near future or the participant was seen within the past two months, wait a reasonable amount of time to try to schedule the off site visit: we do not want to call our participants or their contacts too frequently, and the original members can get confused if they get several calls from the Framingham Heart Study.
There is a minimum of one year required between exams when starting a new cycle for the Original Cohort. A signed consent is good for two years or until the next cycle begins. Each exam cycle the participants must sign a new consent form. This exam cycle we will no longer be using consent by substituted judgment, some of these participants will now fall under the Waiver of Informed Consent.
When an appointment has been scheduled, the schedule is e-mailed to the offsite email list and a hard copy is given to ██████████ with the appropriate letter (with the nursing home or home visit form letters attached). Kathy will send the appointment letter with the medical information form attached for Home Visits.
- Home Visits
You may call the participant directly to schedule an off site appointment if:
- There is no notation of cognitive impairment (*COG IMP* on the comment line or the F4/F14 screen),
- The Consent Status is less than 3,
- If the participant has not had the regular exam within the past year; and
- There are no comments regarding severe hearing loss or speech difficulties.
If the participants' consent status is 3 or greater or if you have ANY question of their cognitive status, call the participants "FHS Proxy" first following the Waiver of informed Consent protocol, if they have not designated a proxy, call a family member, preferably a Heart Study member. If you called the participant directly and any "red flags" were raised, call their proxy (if there is not a proxy call a family member) before scheduling. Given the ages of the Original Cohort, it is better to call someone in the next generation, preferably one of the children in the Offspring study. All Heart Study members are listed in the Family screen (F18 or shift F8), but check the F14 or F4 screen to see if they have a FHS proxy, if they don't check the comments and contact names to determine the best person to call. Whenever possible, call someone who lives near the participant.
If you cannot reach any contacts, (telephones disconnected, etc.), check the participant's chart (the Salmon Sheet) and/or any recent medical records in the chart to see who was listed as the responsible party or next of kin. If the contact person denies any problems (which often happens) and says the participant can sign any necessary form ask the contact if they would be willing to answer any unanswered questions after the exam.
When doing Home Visits where the Waiver of Informed Consent is used and you're not certain whether the participant can accurately answer questions, request that a family member or caretaker very familiar with the participant be present at the exam.
- Nursing Home Visits
If there is no cognitive impairment noted in the roster, first call the nursing home to schedule the appointment. Identify yourself by name as a staff member of the Framingham Heart Study and ask to speak to the person in charge of the care of the participant. Once you have the nurse in charge of the participant on the line, identify yourself again as noted above, let them know why you are calling, and ask the nurse what the best time to visit the participant would be (some participants have other commitments during the day) and once the best time is determined, schedule an appointment. As a courtesy, call their proxy, if one is not listed contact a relative we have listed, starting with the spouse (unless there are instructions to the contrary on the roster) to inform her/him that we will be going to the nursing home; sometimes a relative wants to be present at the exam.
If the participant has a cognitive impairment follow the procedure for the Waiver of Informed Consent.
If the nursing home staff member tells you the participant has died since our last visit or health update, complete a Death Information Form which goes to the Participant Coordinator. If the nursing home can't or won't provide the information we need and the death occurred several months ago, call the proxy (if available) or a family member for information.
If you're told the participant is too ill for a visit and/or has had serious medical events since our last update, you may call a family member and ask them about the participants' condition and whether they feel we can visit, if they also say no, ask if you can complete a health update with them (using the Medical History Update form).
2. Preparation for an Off-site Examination
- Supplies
The following supplies should be brought with you on an offsite visit:
- 1 Portable EKG machine
- 1 Portable EKG acquisition module
- 1-2 Packs of EKG electrodes
- 1 Heart square
- Alcohol wipes
- Gauze
- Adhesive remover pads
- 3 Blood pressure cuffs; large adult, adult and pediatric (Latex Free)
- 1 Pocket Aneroid Sphygmomanometer
- 1 Litman Classic II Stethoscope
- 1 Pencil
- 1 Wristwatch
- 1 Portable scale
- Response sheets for participant
- 1 JAMAR dynamometer
- 1 Stopwatch
- 1 Tape measure
- 1 Pocket Talker (very helpful for hearing impaired participants)
- Masking tape or tape of equal visibility
- Participant's chart containing last exam, including the MMSE and paperwork for
- Exam 29
- Preparation
On the day of the scheduled Heart Study visit it is best to call the participant or nursing home to confirm the appointment. Instruct the participant that he/she should wear a top that easily opens in the front to facilitate the ECG and remind them to have any available medications they take. With their confirmation letter, a form is included that helps to summarize their medical history since their last exam. Ask them to have this form ready.
When calling a nursing home inform the nurse that access to their patient's chart is necessary. Most nursing homes are accommodating and have the chart set aside for the visit.
3. Proposed Sequence of Exam (offsite)
- Offsite Technician Completes:
- Informed Consent (Use of Waiver if applicable)
- Sociodemographic and family history (Salmon Sheet)
- HIPAA Medical Release Form
- Healthcare proxy form
- Medical History Update
- 2 Blood Pressures
- MMSE
- Numerical Data: Weight, Marital Status
- ECG
- End of Life Preference Questions & Questionnaire's (CES-D, ADL's, Nagi, R-B, etc)
- Observed Performance
- Nursing Home Chart Review-Update any incomplete information (offsite NH exam only)
- Proxy Interview (if needed)
- Chart Completion
- MD Completes:
- Medical History-First Opinions
- MD Letter
- Referral Tracking
- Patient Letter
4. Visiting the Cognitively Impaired
The physical component of the exam requires the cooperation of the participant. The following are some suggestions to be able to effectively communicate with those with dementia.
Effective Communication Suggestions:
- Be patient
- Do not try to reason
- Keep information simple
- Use given names
- Use eye contact
- Give one direction at a time
- Give clear instructions instead of asking questions
- Keep communication in the present
- Use sensitive touch when possible
- Give frequent acknowledgment and encouragement
- Ignore misinformation and simply acknowledge the communication
5. Nursing Home Chart Review Protocol
When visiting a participant in a Nursing Home, most of the necessary information may be obtained through the review of the participants Nursing Home chart. When calling to confirm the off site visit to the Nursing Home, inform the nurse taking care of the participant that you will need to look through his or her chart. Most nurses will ensure that the chart will be available upon your arrival.
- Updating Sociodemographic Data and Family History
Upon opening the nursing home chart, one should see a face sheet. This sheet contains all the personal demographic data on their patient, including their next of kin. If these name(s) vary from the most recent ones on the Personal and Family History they should be documented, along with their addresses and phone numbers.
At the bottom of the face sheet it often lists the admission diagnosis of the patient. This is extremely important, especially if this is their first Nursing Home off site visit.
- Medications
Most charts contain an up-to-date list of the patient's medications. Some facilities keep the medications in a separate chart. If the patient's medications are not listed in their chart, ask for the medication book. Many times the medication sheets for months prior may also still be in the chart, make sure you use the most recent medication list (the dates will be at the bottom of the form).
- Interim Medical History
The two sections that are most helpful in locating medical history information are "Consults" and "Medical History". Some nursing homes keep copies of all hospitalization records in a clear sleeve. The "Physician's Notes" and "Nurses Notes" sections are also helpful.
NOTE: Since all facilities have their own chart organization system it is best to thoroughly examine the whole chart. Some facilities thin their charts more :frequently and if only the last month's information is present, then ask to see the whole interim period. This will ensure that nothing is missed.
- Activities of Daily Living
To update a participant's activities of daily living the best reference is the MDI or minimum data sheet. This is a computer sheet, usually at the :front of the chart, and it is updated about every 4 to 6 months. Thls sheet lists activities of daily living, hospitalizations etc. Always refer back to notes and daily documented information to corroborate data, but this gives a nice head start. To truly confirm the current level of functioning of the patient consult with his or her nurse and list nurse as the Proxy.
- Weight
If you are unable to obtain the participants weight using the FHS protocol you can use their nursing home chart records. Weight is typically done weekly at NH facilities. If you can't find a list of their current weight you can reference their physical exam report. Check to see if the NH keeps a seperate weight book first before using the physical, we want to use the most recent measurement. Record the weight on file and the date it was obtained.
Off-Site Visit Chart Completion
After returning to the Heart Study the following procedure is used to ensure that the chart is processed in an efficient manner.
A. ECG Physician Review
The full size tracing of the ECG and the ECG from the participant's previous exam should be presented to a FHS physician within 24 hours of the visit or within 24 hours of the tech returning to the FHS. This is done for comparison and reading. Should there be any marked ECG changes; the FHS physician should inform the participant's personal physician immediately.
After a contact is made with the PCP, the physician should complete a phone encounter sheet or the referral tracking form to document his/her actions.
The field visit tech will complete the chart the day of the visit or the next day if the visit occurred late in the day or was out of the Metrowest area.
Field visit charts will be processed within 1-2 days of the visit and the tracking sheet will be returned to the off-site tech for confirmation of completion.
B. Chart Review Protocol
- Review all forms to ensure that all areas are completed. This includes the participant's letter and the physician summary sheet. On the summary sheet, document the medical findings that are new since the last exam and any other significant medical conditions carried over from previous exams.
- If the participant had a stroke or has shown marked cognitive changes in the interim, a referral is made to the Stroke and/or Dementia study. After completing the referral forms, attach to the front of the chart.
- A Routing Sheet is used to ensure that the doctor, the Study Coordinator, the Offsite Technician and Data technician review the chart.
- When preparing the chart for the MD to review in clinic, the following documents should be clipped together and put in the
front of the chart:
- ECG - current and from last exam
- Medical History Update
- Summary Sheet to MD
- Letter to Participant
- Referral Tracking Form
- Photocopied Summary of Findings from previous letter
- The chart should be left for the MD to review in clinic that morning. A participant label should be put on the float sheet and the person working the float position should inform the MD that they have a chart to review.
- It is the responsibility of the MD to review the chart in clinic that morning. The chart should not be brought upstairs.
- Once the chart is reviewed by the MD the off site technician should again review the chart for completeness and put the chart in order.
- The chart should then be given to the Cohort Participant Coordinator. The CPC will update the roster and give the chart to the data technician to type the MD letter.
- Once the data technician is finished with the chart he/she should return the routing sheet to the offsite technician. Once this is returned this will indicate the chart is completed.