This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Perry T, editor. Therapeutics Letter. Vancouver (BC): Therapeutics Initiative; 1994-.
Therapeutics Letter 111 explores deprescribing of proton pump inhibitors. Conclusions: Many patients take PPIs well beyond the recommended course of treatment. This incurs inconvenience, costs and potential for harms. Do not prescribe or renew PPIs without a well-documented indication and therapeutic goal. Write the indication and duration of therapy in the directions, to ensure this appears on the prescription label. Consider deprescribing PPIs after 4 weeks of treatment when symptoms have resolved. Start with reduced dose or a longer interval, switching to on-demand dosing or discontinuation when successful. Patients capable of “chasing” a dose with water to facilitate stomach emptying can consider dose-splitting to save money. Informed patient consent and a strategy to deal with recurrent symptoms enhance success. For more information, consult the high-quality resources shown below.
Keywords:
Adverse Effects, Deprescriptions, Gastroesophageal Reflux, Long Term Adverse Effects, Peptic Ulcer, Proton Pump Inhibitors;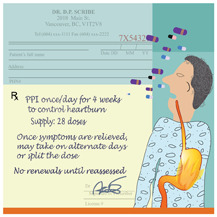
Our previous reviews3–9 of randomized clinical trial (RCT) evidence on PPIs concluded:
- Patients treated effectively do not require chronic acid suppressive medications.4
- Long-term PPIs are appropriate in relapsing severe erosive esophagitis.3
- No PPI demonstrated superiority for GERD or symptoms related to PUD.9
- No long-term RCTs monitored adverse effects of PPIs.9
Understanding serious long-term adverse effects of PPIs thus relies on observational studies showing that PPIs are associated with an increased risk of a variety of serious adverse events. These include enteric infections (notably C. difficile), spontaneous bacterial peritonitis, fractures, hypomagnesemia, acute interstitial nephritis, iron deficiency, vitamin B12 deficiency, gastric polyps and gastric cancer.8 Recently, dementia was added to this list.10 The apparent association with serious pneumonia may not be causative.11 Yet strong acidity in the stomach has long evolutionary roots, and acid may function as an “ecological filter” against harmful ingested microbes.12
An obligation to consider deprescribing?
Studies in the US, Australia, and UK found that 40–65% of hospitalized people taking long-term PPIs, and 40–55% of primary care outpatients, had no documented reason for taking a PPI.13 In BC, 34% of people in residential care did not have a documented indication for their PPI prescription.14
Without evidence of long-term effectiveness, costs and harms create a clinical obligation to consider deprescribing PPIs in many people taking long-term therapy.
A Cochrane review of evidence for PPI deprescribing found six RCTs lasting 6-months (N=1758). Five RCTs compared continued PPI use with on-demand use; one compared continued use with abrupt cessation.15 Unlike the majority of patients who take PPI for mild symptoms or unknown indications, most trial participants had moderately severe reflux esophagitis, for whom deprescribing is less likely to be effective. The trials were small, short in duration, and did not record clinical outcomes most relevant to benefits or harms of deprescribing. Thus, there are no RCT data to inform conclusions about long-term benefits or harms of PPI continuation, reduction, or discontinuation.
Guideline for deprescribing PPIs
A non-industry funded Canadian Deprescribing Network guideline is now available.13 The authors searched for evidence to help clinicians decide when and how to safely taper or stop PPI, using Cochrane methodology and the GRADE framework for guideline development. They define deprescribing of PPIs as:
- dose reduction;
- change to intermittent or on demand use;
- substituting a histamine 2 receptor antagonist (H2RA); or
- complete cessation of PPI.
Having found no evidence comparing these approaches, the Canadian guideline recommends deprescribing PPIs in adults who have completed a minimum of 4 weeks of PPI treatment and whose upper GI symptoms are resolved. This recommendation does not apply to people with Barrett esophagus, severe esophagitis, or a documented history of bleeding ulcers. The authors suggest on-demand use or a clinically reasonable tapering schedule:
- Reduce PPI dose by half at 1–2-week intervals until the PPI is discontinued; or
- Increase dosing interval from daily to every 2–3 days. Switching to H2RA or oral antacids during the taper may also be helpful.
The guideline discusses how to monitor patients. In deprescribing experiments, patients were followed at 4 and 12 weeks after stopping a PPI, and again at 6–12 months. Differentiating “rebound hypersecretion” from non-acid symptoms of gastroesophageal reflux is challenging.
Efficacy of on-demand PPI use
AstraZeneca (discoverer of omeprazole) sponsored research showing by 1999 that on-demand use of 10 or 20 mg was more effective than placebo for preventing recurrence of heartburn in 424 patients without demonstrated esophagitis.16 The more potent enantiomer esomeprazole acted similarly in 342 patients randomized to 20 mg vs. placebo on-demand.17 The active group used esomeprazole on about 1 in 3 days, leading to the novel conclusion that on-demand therapy “provides a more individualized approach to management of the patient with GERD, whereby the patient dictates the extent of drug usage according to his or her specific needs.” Repeating similar studies led a recent report to emphasize that on-demand PPIs for non-life-threatening conditions have “obvious potential benefits in terms of cost of treatment and convenience to patients.”18 This is partly because inhibition of acid secretion lasts much longer than the elimination half-life of PPIs.
Dose splitting is an inexpensive way to reduce daily dosage. Product monographs advise against this, because PPIs are subject to gastric acid degradation before reaching their absorptive site in the small bowel. However, “chasing” a dose with water to help empty the stomach ensures absorption of dissolved omeprazole and esomeprazole.19 For non-life-threatening conditions, dose splitting is thus a pharmacologically reasonable option.
The Canadian Association of Gastroenterology (CAG) and Choosing Wisely Canada support deprescribing, recommending that “PPI therapy for gastrointestinal symptoms should not be maintained long term without an attempt to stop/reduce them at least once per year in most patients.”20
Conclusions
- Many patients take PPIs well beyond the recommended course of treatment. This incurs inconvenience, costs and potential for harms.
- Do not prescribe or renew PPIs without a well-documented indication and therapeutic goal. Write the indication and duration of therapy in the directions, to ensure this appears on the prescription label.
- Consider deprescribing PPIs after 4 weeks of treatment when symptoms have resolved. Start with reduced dose or a longer interval, switching to on-demand dosing or discontinuation when successful.
- Patients capable of “chasing” a dose with water to facilitate stomach emptying can consider dose-splitting to save money.
- Informed patient consent and a strategy to deal with recurrent symptoms enhance success. For more information, consult the high-quality resources shown below.
PPI DEPRESCRIBING RESOURCES
- PPI Evidence-Based Deprescribing Guideline
- RXFiles (Saskatchewan) on Deprescribing PPIs
- BC Provincial Academic Detailing Service: Proton Pump Inhibitors in Primary Care
- Alberta College of Family Physicians: Tools for Practice. PPIs: Is Perpetual Prescribing Inevitable?
Footnotes
For a complete list of references and links to PPI deprescribing resources go to: www
.ti.ubc.ca/letter111
References
- 1.
- BC Provincial Academic Detailing Service. Proton Pump Inhibitors in Primary Care. January 2015. https://www2
.gov.bc.ca /assets/gov/health /practitioner-pro/provincial-academic-detailing-service /pad-2015-proton-pump-inhibitors-newsletter .pdf - 2.
- Nexium24H product monograph (OTC esomeprazole). https://www
.nexium24 .ca/sites/default/themes /nexium_ca/pdf/Nexium-Insert-Leaflet-EN.pdf - 3.
- Therapeutics Initiative. Treatment of Gastroesophageal Reflux Disease (GERD). Therapeutics Letter. 1994 (Dec); 3:1–2. https://ti
.ubc.ca/letter3 - 4.
- Therapeutics Initiative. Review and Update. Therapeutics Letter. 1995 (Sep); 9:1–2. https://ti
.ubc.ca/letter9 - 5.
- Therapeutics Initiative. New Drugs. Therapeutics Letter. 1996 (Mar–Apr); 13:1–2. https://ti
.ubc.ca/letter13 - 6.
- Therapeutics Initiative. Review and Update. Therapeutics Letter. 1996 (Nov–Dec); 16:1–2. https://ti
.ubc.ca/letter16 - 7.
- Therapeutics Initiative. New Drugs IV. Therapeutics Letter. 1998 (Sep–Oct); 26:1–2. https://ti
.ubc.ca/letter26 - 8.
- Therapeutics Initiative. Do Single Stereoisomer Drugs Provide Value? Therapeutics Letter. 2002 (Jun–Sep); 45:1–2. https://ti
.ubc.ca/letter45 - 9.
- Therapeutics Initiative. Comparative Effectiveness of Proton Pump Inhibitors. Therapeutics Letter. 2016 (Mar–Apr); 99:1–2. https://ti
.ubc.ca/letter99 - 10.
- Gomm W, von Holt K, Thom F et al. Association of Proton Pump Inhibitors With Risk of Dementia: A Pharmacoepidemiological Claims Data Analysis. JAMA Neurol. 2016;73(4):410–6. DOI: 10.1001/jamaneurol.2015.4791 [PubMed: 26882076] [CrossRef]
- 11.
- Filion KB, Chateau D, Targownik LE et al. Proton pump inhibitors and the risk of hospitalization for community-acquired pneumonia: replicated cohort studies with meta-analysis. Gut 2014; 63(4):552–558. DOI: 10.1136/gutjnl-2013-304738 [PMC free article: PMC3963530] [PubMed: 23856153] [CrossRef]
- 12.
- Beasley DE, Koltz AM, Lambert JE et al. The Evolution of Stomach Acidity and Its Relevance to the Human Microbiome. PLoS ONE 2015;10(7):e0134116. DOI: 10.1371/journal.pone.0134116 [PMC free article: PMC4519257] [PubMed: 26222383] [CrossRef]
- 13.
- Farrell B, Pottie K, Thompson W et al. Deprescribing Proton Pump Inhibitors: Evidence-based clinical practice guideline Can Fam Physician 2017; 63: 354–64. http://www
.cfp.ca/content/63/5/354 [PMC free article: PMC5429051] [PubMed: 28500192] - 14.
- Chan A, Liang L, Tung A et al. Is there a reason for the PPI? An assessment of PPI prescribing in residential care patients in a large Canadian hospital system. (In Press) Can J Hosp Pharm 2018. [PMC free article: PMC6209499] [PubMed: 30401995]
- 15.
- Boghossian TA, Rashid FJ, Thompson W et al. Deprescribing versus continuation of chronic proton pump inhibitor use in adults. Cochrane Database of Systematic Reviews 2017, Issue 3. Art. No.: CD011969. DOI: 10.1002/14651858.CD011969.pub2 [PMC free article: PMC6464703] [PubMed: 28301676] [CrossRef]
- 16.
- Lind T, Havelund T, Lundell L et al. On demand therapy with omeprazole for the long-term management of patients with heartburn without oesophagitis – a placebo-controlled randomized trial. Aliment Pharmacol Ther 1999;13(7):907–14. DOI: 10.1046/j.1365-2036.1999.00564.x [PubMed: 10383525] [CrossRef]
- 17.
- Talley NJ, Lauritsen K, Tunturi-Hihnala H et al. Esomepreazole 20 mg maintains symptom control in endoscopy-negative gastro-esophageal reflux disease: a controlled trial of ‘on-demand’ therapy for 6 months. Aliment Pharmacol Ther 2001;15(3):347–54. 10.1046/j.1365-2036.2001.00943.x [PubMed: 11207509] [CrossRef]
- 18.
- Bayerdorffer E, Bigard MA, Weiss W et al. Randomized, multicenter study: on-demand versus continuous maintenance treatment with esomeprazole in patients with non-erosive gastroesophageal reflux disease. BMC Gastroenterology 2016;16:48. DOI: 10.1186/s12876-016-0448-x [PMC free article: PMC4831110] [PubMed: 27080034] [CrossRef]
- 19.
- Andersson T, Hassan-Alin M, Hasselgren G et al. Pharmacokinetic studies with esomeprazole, the (S)-isomer of omeprazole. Clin Pharmacokinet 2001;40(6):411–26. DOI: 10.2165/00003088-200140060-00003 [PubMed: 11475467] [CrossRef]
- 20.
- Canadian Association of Gastroenterology, Choosing Wisely Canada. Gastroenterology–Five Things Physicians and Patients Should Question. Last updated: June 2017. https:
//choosingwiselycanada .org/gastroenterology/
- The draft of this Therapeutics Letter was submitted for review to 130 experts and primary care physicians in order to correct any inaccuracies and to ensure that the information is concise and relevant to clinicians.
- The Therapeutics Initiative is funded by the BC Ministry of Health through a grant to the University of BC. The Therapeutics Initiative provides evidence-based advice about drug therapy, and is not responsible for formulating or adjudicating provincial drug policies.
- Deprescribing proton pump inhibitors.[Aust J Gen Pract. 2022]Deprescribing proton pump inhibitors.Turner JP, Thompson W, Reeve E, Bell JS. Aust J Gen Pract. 2022 Nov; 51(11):845-848.
- The Use and Misuse of Proton Pump Inhibitors: An Opportunity for Deprescribing.[J Am Med Dir Assoc. 2021]The Use and Misuse of Proton Pump Inhibitors: An Opportunity for Deprescribing.Dharmarajan TS. J Am Med Dir Assoc. 2021 Jan; 22(1):15-22. Epub 2020 Dec 13.
- Review Deprescribing versus continuation of chronic proton pump inhibitor use in adults.[Cochrane Database Syst Rev. 2017]Review Deprescribing versus continuation of chronic proton pump inhibitor use in adults.Boghossian TA, Rashid FJ, Thompson W, Welch V, Moayyedi P, Rojas-Fernandez C, Pottie K, Farrell B. Cochrane Database Syst Rev. 2017 Mar 16; 3(3):CD011969. Epub 2017 Mar 16.
- Review Problems Associated with Deprescribing of Proton Pump Inhibitors.[Int J Mol Sci. 2019]Review Problems Associated with Deprescribing of Proton Pump Inhibitors.Helgadottir H, Bjornsson ES. Int J Mol Sci. 2019 Nov 2; 20(21). Epub 2019 Nov 2.
- Deprescribing proton pump inhibitors: A study in hospitalized patients in Slovenia.[Int J Clin Pharmacol Ther. 2023]Deprescribing proton pump inhibitors: A study in hospitalized patients in Slovenia.Ravbar N, Kerec Kos M, Jošt M, Čebron Lipovec N, Knez L. Int J Clin Pharmacol Ther. 2023 Jul; 61(7):306-314.
- Deprescribing Proton Pump Inhibitors - Therapeutics LetterDeprescribing Proton Pump Inhibitors - Therapeutics Letter
- Does SPRINT change our approach to blood pressure targets? - Therapeutics LetterDoes SPRINT change our approach to blood pressure targets? - Therapeutics Letter
- Herbal Medicines - Therapeutics LetterHerbal Medicines - Therapeutics Letter
- Selective COX-2 inhibitors: Are they safer NSAIDs? - Therapeutics LetterSelective COX-2 inhibitors: Are they safer NSAIDs? - Therapeutics Letter
Your browsing activity is empty.
Activity recording is turned off.
See more...
