Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
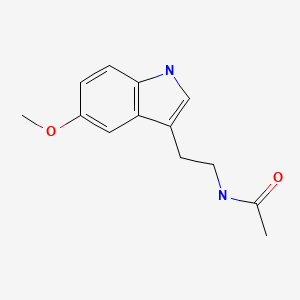
CASRN: 73-31-4
Drug Levels and Effects
Summary of Use during Lactation
Melatonin is the hormone produced by the pineal gland that plays a role in regulating sleep and circadian rhythm as well as a possible role in gut-brain signaling.[1] It is a normal component of breastmilk, with concentrations higher during nighttime (peak around 3 am) than daytime.[2-6] Women who work the night shift have lower milk melatonin concentrations during the midnight to 6:30 am period than on days when they are not working, which becomes larger on subsequent days of working the night shift.[7] Elective cesarean section results in higher daytime colostrum levels than with vaginal delivery.[8] Some authors suggest that mothers should nurse in the dark at night in order to avoid reductions in the melatonin content of breastmilk, which could disturb infant sleep patterns.[9] Differentiating milk pumped during the day from milk pumped during darkness has also been suggested for women pumping milk for their infants.[2,10] Some studies have attributed longer sleep time in breastfed infant than in formula-fed infants to melatonin in breastmilk.[11,12] Another study found higher colostrum melatonin levels at night which appeared to increase the phagocytic activity of colostral cells against bacteria.[13] A survey of 329 mothers found that infants who consumed mistimed expressed breastmilk took longer to get to sleep compared with infants who were directly breastfed, formula fed, fed timed expressed breast milk and fed breast milk/formula combined. Breastfed infants had more awakenings at night compared with infants who consumed mistimed expressed breastmilk.[14]
Exogenous administration of melatonin has no specific use during breastfeeding and no data exist on the safety of maternal use of melatonin during breastfeeding. However, doses higher than those expected in breastmilk after maternal supplementation have been used safely in infants.[15] It is unlikely that short-term use of usual doses of melatonin in the evening by a nursing mother would adversely affect her breastfed infant, although some authors recommend against its use in breastfeeding because of the lack of data and a relatively long half-life in preterm neonates.[16,17]
Dietary supplements do not require extensive pre-marketing approval from the U.S. Food and Drug Administration. Manufacturers are responsible to ensure the safety, but do not need to prove the safety and effectiveness of dietary supplements before they are marketed. Dietary supplements may contain multiple ingredients, and differences are often found between labeled and actual ingredients or their amounts. A manufacturer may contract with an independent organization to verify the quality of a product or its ingredients, but that does not certify the safety or effectiveness of a product. Because of the above issues, clinical testing results on one product may not be applicable to other products. More detailed information about dietary supplements is available elsewhere on the LactMed Web site.
Drug Levels
Melatonin is a normal component of human milk which is synthesized from the amino acid tryptophan.
Maternal Levels. A study of 169 mothers of newborns measured melatonin in milk samples. Milk samples were obtained at 8 am on days 3, 10, 25 and 55 for those with infants born at 24 to 33.9 weeks of gestation or of infants or on day 3 for those with infants born at 34 to 41 weeks of gestation. Median milk melatonin concentrations measured on day 3 were significantly higher in mothers who delivered before 34 weeks of gestation than in those who delivered after 34 of gestation (20 ng/L vs. 8 ng/L). In mothers who delivered between 24 to 33.9 weeks of gestation, median milk melatonin concentrations were stable, between 16 and 20 ng/L, from day 3 to 55.[6]
Ten nursing mothers who were 3 to 5 days postpartum had serum and breastmilk melatonin levels measured between 2 pm and 5 pm and again between 2 am and 4 am. The breastmilk melatonin level averaged 23 ng/L at night, an average of 35% of the maternal serum concentration. Melatonin was undetectable (<10 ng/L) in milk during the daytime. Six of the mothers collected milk after each feeding for 24 hours once within 3 months of delivery. All mothers exhibited a marked circadian rhythm of melatonin excretion into breastmilk with detectable levels first occurring in the evening and dropping to undetectable levels in the morning.[18]
Twenty-one mothers collected breastmilk samples 5 times in a 24-hour period between day 5 and 10 postpartum. The median melatonin concentration in daytime milk (10 am to 10 pm) was 1.5 mg/L and the median concentration in nighttime milk (10 pm to 10 am) was 7.3 ng/L. No statistically significant difference was found between the breastmilk of mothers with preterm and full-term infants.[2]
Twenty-four healthy mothers and 24 mothers with allergic eczema were studied in a crossover fashion to watch either a humorous video, a non-humorous video, or no video at 2-week intervals. Melatonin was measured in breastmilk 5 times between 10 pm and 6 am. Melatonin levels were higher at all times in the mothers who had watched the humorous video. The melatonin levels in mothers with eczema were generally lower than in normal mothers, but had a greater increase to similar levels in both groups after viewing the humorous video. The highest milk melatonin levels occurred at the 2 am sampling in all phases of the study, with a peak of 20.8 ng/L in healthy mothers and 19.9 ng/L in those with eczema.[19]
In studies in which exogenous oral melatonin was given to women, the resulting serum melatonin was variable, but peak serum concentrations ranged from 1.1 to 2.6 mcg/L for each 1 mg administered.[20-22] This would result in an average increase in breastmilk melatonin concentration from 0.4 to 1 mcg/L for each 1 mg administered to the mother, based on an average milk concentration of 35% of the maternal serum concentration. While the resulting concentrations would be higher than the typical physiologic peak milk concentrations of 0.02 mcg/L,[18,19] it would present a considerably lower dose to the infant than the 10 mg/kg dosages of melatonin that have been safely administered to neonates in clinical studies.[9,15]
One study found that breastmilk melatonin concentration was inversely correlated with breastmilk prolactin concentration and was higher in women experiencing fatigue in the morning.[23]
Five nursing mothers provided breastmilk samples every 2 hours over a 24-hour period. Melatonin was undetectable during the day, but began to rise at about 8 pm, reaching a peak at about 3 am, and then declining.[11]
Thirty women who were 48 to 72 hours postpartum provided 2 colostrum samples, one at noon and one at midnight. Melatonin levels in colostrum averaged about 16 ng/L at noon and 36 ng/L at midnight.[13]
A study in Turkey found that melatonin colostrum levels measured between 1:00 and 3:00 am between 48 and 72 hours postpartum were higher in mothers who delivered vaginally (mean 266 ng/L) than in those delivering by elective cesarean section (mean 205 ng/L) or emergency cesarean section (mean 167 ng/L). All differences between groups were statistically significant.[24]
Melatonin was analyzed in 392 breastmilk samples from 98 healthy nursing mothers at 0 to 30 days postpartum. Milk samples were obtained at 03:00, 09:00, 15:00, and 21:00 in one day. Peak milk levels occurred at 03:00 in both term and preterm milk. At 03:00 preterm colostrum had a higher average concentration than term colostrum 28.67 ng/L and 25.31 ng/L, respectively. Melatonin levels were numerically, but not statistically, higher in transitional and term milk at 03:00. The lowest levels of melatonin in milk occurred at 09:00 and 21:00.[4]
A study compared daytime and nighttime melatonin colostrum and milk levels in mothers who had an elective cesarean section (n=18) to mothers who had a vaginal delivery (n=21). Nighttime melatonin levels were higher in colostrum, transitional and mature milk in both groups, with nighttime melatonin ranging from 10.9 to 17.5 ng/L higher than daytime levels. Colostrum melatonin levels were higher in mothers who had an elective cesarean section (average 30.3 ng/L) than in mothers who had a vaginal delivery (average 14.7 ng/L).[8]
Infant Levels. A study of 8 breastfed and 6 formula-fed infants found different patterns of the melatonin metabolite, 6-sulfatoxymelatonin, in their urine. Breastfed infants had a sinusoidal excretion pattern with a peak at 6 am and a trough at 6 pm. Formula-fed infants had a simple increase in the metabolite that was at baseline between about 8 pm and 4 am with a peak at about noon.[25]
Plasma melatonin levels were measured in 167 infants at birth and 173 infants on day 3 postpartum.
Infants born before 34 weeks gestational age had significantly lower plasma melatonin concentrations both at birth and on day 3 postpartum compared to infants born after 34 weeks gestational age. More infants born at less than 34 weeks of gestation had deficient plasma levels of 7 ng/L or less compared to infants born at 34 weeks or greater at birth (78% vs 57%) or at 3 days of age (81% vs 34%). Median 24-hour urine concentrations of the melatonin metabolite, 6-sulfatoxy-melatonin were significantly lower in infants born before week 34 of gestation than in those born between after 34 weeks, both on day 1 (230 ng/L vs.533 ng/L) and on Day 3 (197 ng/L vs. 359 ng/L).[6]
Effects in Breastfed Infants
A study on 54 exclusively breastfed infants (n = 54), formula-fed infants (n = 40) and their mothers questioned their mothers regarding infant behavior. Melatonin was measured in the milk of 5 of the mothers. Exclusively breastfed infants had a lower incidence of colic attacks, lower severity of irritability attacks, and a trend for longer nocturnal sleep duration. Melatonin in human milk showed a circadian curve and was unmeasurable in all artificial milks.[11]
An 18-month-old breastfed infant was having bleeding episodes since birth. A platelet aggregation test showed that the infant had reduced platelet aggregation after breastfeeding. When the infant was fasting, platelet aggregation was normal. The infant's mother occasionally took melatonin up to 10 mg daily for sleep. After she stopped melatonin intake for 3 months, the infant's platelet aggregation was normal and the infant had no further bleeding episodes, even after major trauma.[26] The bleeding episodes were possibly caused by melatonin in milk.
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
- Anderson G, Vaillancourt C, Maes M, Reiter RJ. Breastfeeding and the gut-brain axis: Is there a role for melatonin? Biomol Concepts 2017;8:185-95. [PubMed: 28723608]
- 2.
- Katzer D, Pauli L, Mueller A, et al. Melatonin concentrations and antioxidative capacity of human breast milk according to gestational age and the time of day. J Hum Lact 2016;32:NP105-NP110. [PubMed: 27121237]
- 3.
- Molad M, Ashkenazi L, Gover A, et al. Melatonin stability in human milk. Breastfeed Med 2019;14:680-2. [PubMed: 31381362]
- 4.
- Qin Y, Shi W, Zhuang J, et al. Variations in melatonin levels in preterm and term human breast milk during the first month after delivery. Sci Rep 2019;9:17984. [PMC free article: PMC6884443] [PubMed: 31784629]
- 5.
- Italianer MF, Naninck EFG, Roelants JA, et al. Circadian cariation in human milk composition, a systematic review. Nutrients 2020;12:E2328. [PMC free article: PMC7468880] [PubMed: 32759654]
- 6.
- Biran V, Decobert F, Bednarek N, et al. Melatonin levels in preterm and term infants and their mothers. Int J Mol Sci 2019;20:2077. [PMC free article: PMC6540351] [PubMed: 31035572]
- 7.
- Booker LA, Wilson D, Spong J, et al. Maternal circadian disruption from shift work and the impact on the concentration of melatonin in breast milk. Breastfeed Med 2024;19:33-9. [PubMed: 38150529]
- 8.
- Aparici-Gonzalo S, Carrasco-García Á, Gombert M, et al. Melatonin content of human milk: The effect of mode of delivery. Breastfeed Med 2020;15:589-94. [PubMed: 32721174]
- 9.
- Sánchez-Barceló EJ, Mediavilla MD, Reiter RJ. Clinical uses of melatonin in pediatrics. Int J Pediatr 2011;2011:892624. [PMC free article: PMC3133850] [PubMed: 21760817]
- 10.
- Arslanoglu S, Bertino E, Nicocia M, Moro GE. WAPM Working Group on Nutrition: Potential chronobiotic role of human milk in sleep regulation. J Perinat Med 2012;40:1-8. [PubMed: 22848905]
- 11.
- Cohen Engler A, Hadash A, Shehadeh N, Pillar G. Breastfeeding may improve nocturnal sleep and reduce infantile colic: Potential role of breast milk melatonin. Eur J Pediatr 2012;171:729-32. [PubMed: 22205210]
- 12.
- Rudzik AE, Robinson L, Ball HL. Infant sleep duration and melatonin levels in exclusively breastfed and exclusively formula fed infants. Am J Hum Biol 2016;28:294. doi:10.1002/ajhb.22831 [CrossRef]
- 13.
- Honorio-Franca AC, Hara CCP, Ormonde JV, et al. Human colostrum melatonin exhibits a day-night variation and modulates the activity of colostral phagocytes. J Appl Biomed 2013;11:153-62. doi:10.2478/v10136-012-0039-2 [CrossRef]
- 14.
- Booker LA, Spong J, Deacon-Crouch M, Skinner TC. Preliminary exploration into the impact of mistimed expressed breast milk feeding on infant sleep outcomes, compared to other feeding patterns. Breastfeed Med 2022;17:853-8. [PubMed: 36137055]
- 15.
- Gitto E, Aversa S, Reiter RJ, et al. Update on the use of melatonin in pediatrics. J Pineal Res 2011;50:21-8. [PubMed: 21029156]
- 16.
- Andersen LP, Gogenur I, Rosenberg J, Reiter RJ. The safety of melatonin in humans. Clin Drug Investig 2016;36:169-75. [PubMed: 26692007]
- 17.
- Vine T, Brown GM, Frey BN. Melatonin use during pregnancy and lactation: A scoping review of human studies. Braz J Psychiatry 2022;44:342-8. [PMC free article: PMC9169489] [PubMed: 34730672]
- 18.
- Illnerová H, Buresova M, Presl J. Melatonin rhythm in human milk. J Clin Endocrinol Metab 1993;77:838-41. [PubMed: 8370707]
- 19.
- Kimata H. Laughter elevates the levels of breast-milk melatonin. J Psychosom Res 2007;62:699-702. [PubMed: 17540228]
- 20.
- DeMuro RL, Nafziger AN, Blask DE, et al. The absolute bioavailability of oral melatonin. J Clin Pharmacol 2000;40:781-4. [PubMed: 10883420]
- 21.
- Fourtillan JB, Brisson AM, Gobin P, et al. Bioavailability of melatonin in humans after day-time administration of D(7) melatonin. Biopharm Drug Dispos 2000;21:15-22. [PubMed: 11038434]
- 22.
- Markantonis SL, Tsakalozou E, Paraskeva A, et al. Melatonin pharmacokinetics in premenopausal and postmenopausal healthy female volunteers. J Clin Pharmacol 2008;48:240-5. [PubMed: 18071190]
- 23.
- Groër M, Davis M, Casey K, et al. Neuroendocrine and immune relationships in postpartum fatigue. MCN Am J Matern Child Nurs 2005;30:133-8. [PubMed: 15775810]
- 24.
- Namlı Kalem M, Kalem Z, Yuce T, et al. Comparison of melatonin levels in the colostrum between vaginal delivery and cesarean delivery. Am J Perinatol 2018;35:481-5. [PubMed: 29166676]
- 25.
- Cubero J, Valero V, Sanchez J, et al. The circadian rhythm of tryptophan in breast milk affects the rhythms of 6-sulfatoxymelatonin and sleep in newborn. Neuro Endocrinol Lett 2005;26:657-61. [PubMed: 16380706]
- 26.
- Iavarone S, Massoud M, Di Felice G, et al. Antiplatelet effect of melatonin through breastfeeding: A pediatric case report. Children (Basel) 2023;10:1839. [PMC free article: PMC10741506] [PubMed: 38136041]
Substance Identification
Substance Name
Melatonin
CAS Registry Number
73-31-4
Drug Class
Breast Feeding
Milk, Human
Complementary Therapies
Central Nervous System Depressants
Antioxidants
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Marine Oils.[Drugs and Lactation Database (...]Review Marine Oils.. Drugs and Lactation Database (LactMed®). 2006
- Review Beta-Carotene.[Drugs and Lactation Database (...]Review Beta-Carotene.. Drugs and Lactation Database (LactMed®). 2006
- Review Glucosamine.[Drugs and Lactation Database (...]Review Glucosamine.. Drugs and Lactation Database (LactMed®). 2006
- Review Chondroitin.[Drugs and Lactation Database (...]Review Chondroitin.. Drugs and Lactation Database (LactMed®). 2006
- Review Coenzyme Q10.[Drugs and Lactation Database (...]Review Coenzyme Q10.. Drugs and Lactation Database (LactMed®). 2006
- Melatonin - Drugs and Lactation Database (LactMed®)Melatonin - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
