Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 92623-85-3
Drug Levels and Effects
Summary of Use during Lactation
Amounts of milnacipran in breastmilk are low and would not be expected to cause any adverse effects in breastfed infants. However, until more data become available, milnacipran should be used with caution during breastfeeding, especially while nursing a newborn or preterm infant.
Drug Levels
Maternal Levels. Eight lactating women who were at least 12 weeks postpartum and weaning their infants received a single oral dose of milnacipran 50 mg. The average peak milk level of milnacipran was 262 mcg/L at an average of 4 hours and the average milk level was 122 mcg/L. The average relative infant dosage was estimated to be 2.8% of the weight-adjusted maternal dosage or 5% using the peak milk levels. Milnacipran was eliminated from milk with an average half-life of 7.5 hours.[1,2]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
Effects on Lactation and Breastmilk
Galactorrhea is reported by the manufacturer to be a side effect of milnacipran.[2] One woman who was being treated for depression took an intentional overdose of 950 mg of milnacipran orally. From day 5 to day 15 after the overdose, the patient noted a flow of milk from her left breast. The galactorrhea resolved without treatment.[3]
In a study of cases of hyperprolactinemia and its symptoms (e.g., gynecomastia) reported to a French pharmacovigilance center, milnacipran was not found to have an increased risk of causing hyperprolactinemia compared to other drugs.[4]
An observational study looked at outcomes of 2859 women who took an antidepressant during the 2 years prior to pregnancy. Compared to women who did not take an antidepressant during pregnancy, mothers who took an antidepressant during all 3 trimesters of pregnancy were 37% less likely to be breastfeeding upon hospital discharge. Mothers who took an antidepressant only during the third trimester were 75% less likely to be breastfeeding at discharge. Those who took an antidepressant only during the first and second trimesters did not have a reduced likelihood of breastfeeding at discharge.[5] The antidepressants used by the mothers were not specified.
A retrospective cohort study of hospital electronic medical records from 2001 to 2008 compared women who had been dispensed an antidepressant during late gestation (n = 575) to those who had a psychiatric illness but did not receive an antidepressant (n = 1552) and mothers who did not have a psychiatric diagnosis (n = 30,535). Women who received an antidepressant were 37% less likely to be breastfeeding at discharge than women without a psychiatric diagnosis, but no less likely to be breastfeeding than untreated mothers with a psychiatric diagnosis.[6] None of the mothers were taking milnacipran.
In a study of 80,882 Norwegian mother-infant pairs from 1999 to 2008, new postpartum antidepressant use was reported by 392 women and 201 reported that they continued antidepressants from pregnancy. Compared with the unexposed comparison group, late pregnancy antidepressant use was associated with a 7% reduced likelihood of breastfeeding initiation, but with no effect on breastfeeding duration or exclusivity. Compared with the unexposed comparison group, new or restarted antidepressant use was associated with a 63% reduced likelihood of predominant, and a 51% reduced likelihood of any breastfeeding at 6 months, as well as a 2.6-fold increased risk of abrupt breastfeeding discontinuation. Specific antidepressants were not mentioned.[7]
Alternate Drugs to Consider
(Fibromyalgia) Duloxetine, Pregabalin
References
- 1.
- Forest Pharmaceuticals. An open-label, single-dose pharmacokinetic study in healthy, lactating women. Study MLN-PK-22 2012.
- 2.
- Allergan, Inc. Savella Package Insert. August 18, 2023.
- 3.
- de Haro L, Hayek-Lanthois M, Rodor F, Valli M. [Amenorrhea and galactorrhea after acute overdose with milnacipran]. Therapie 2001;56:799-800. [PubMed: 11878113]
- 4.
- Trenque T, Herlem E, Auriche P, Drame M. Serotonin reuptake inhibitors and hyperprolactinaemia: A case/non-case study in the French pharmacovigilance database. Drug Saf 2011;34:1161-6. [PubMed: 22077504]
- 5.
- Venkatesh KK, Castro VM, Perlis RH, Kaimal AJ. Impact of antidepressant treatment during pregnancy on obstetric outcomes among women previously treated for depression: An observational cohort study. J Perinatol 2017;37:1003-9. [PMC free article: PMC10034861] [PubMed: 28682318]
- 6.
- Leggett C, Costi L, Morrison JL, et al. Antidepressant use in late gestation and breastfeeding rates at discharge from hospital. J Hum Lact 2017;33:701-9. [PubMed: 28984528]
- 7.
- Grzeskowiak LE, Saha MR, Nordeng H, et al. Perinatal antidepressant use and breastfeeding outcomes: Findings from the Norwegian Mother, Father and Child Cohort Study. Acta Obstet Gynecol Scand 2022;101:344-54. [PMC free article: PMC9564556] [PubMed: 35170756]
Substance Identification
Substance Name
Milnacipran
CAS Registry Number
92623-85-3
Drug Class
Breast Feeding
Milk, Human
Antidepressive Agents
Serotonin and Noradrenaline Reuptake Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Levomilnacipran.[Drugs and Lactation Database (...]Review Levomilnacipran.. Drugs and Lactation Database (LactMed®). 2006
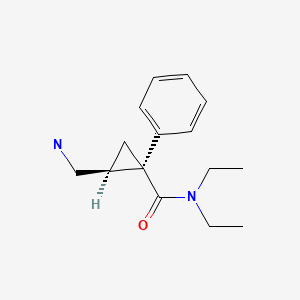
- Biochemical profile of midalcipran (F 2207), 1-phenyl-1-diethyl-aminocarbonyl-2-aminomethyl-cyclopropane (Z) hydrochloride, a potential fourth generation antidepressant drug.[Neuropharmacology. 1985]Biochemical profile of midalcipran (F 2207), 1-phenyl-1-diethyl-aminocarbonyl-2-aminomethyl-cyclopropane (Z) hydrochloride, a potential fourth generation antidepressant drug.Moret C, Charveron M, Finberg JP, Couzinier JP, Briley M. Neuropharmacology. 1985 Dec; 24(12):1211-9.
- Review Netarsudil.[Drugs and Lactation Database (...]Review Netarsudil.. Drugs and Lactation Database (LactMed®). 2006
- Review Berotralstat.[Drugs and Lactation Database (...]Review Berotralstat.. Drugs and Lactation Database (LactMed®). 2006
- Review Pregabalin.[Drugs and Lactation Database (...]Review Pregabalin.. Drugs and Lactation Database (LactMed®). 2006
- Milnacipran - Drugs and Lactation Database (LactMed®)Milnacipran - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
