Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
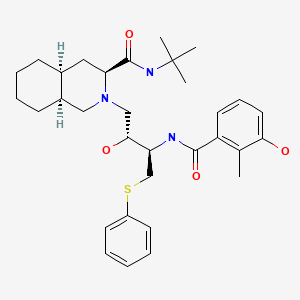
CASRN: 159989-64-7
Drug Levels and Effects
Summary of Use during Lactation
Nelfinavir levels in milk are low and the drug is usually not detectable in the serum of breastfed infants. However, some evidence of nelfinavir-induced adverse reactions in brestfed infants exists. Nelfinavir is not a recommended agent during breastfeeding.[1,2] Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended.[3,4]
Drug Levels
Maternal Levels. Five women were receiving nelfinavir 1250 mg twice daily as part of a highly-active antiretroviral combination regimen. During the first 5 days postpartum milk was collected just before and 2 hours after the dose of nelfinavir. Breastmilk nelfinavir concentrations ranged between 6 and 24% of the maternal serum concentration. The M8 metabolite was not detectable in milk. Further details on the timing, or actual breastmilk concentrations were not provided.[5]
Twenty-six samples of breastmilk and maternal serum were obtained at 6, 12 and 24 weeks postpartum from mothers taking nelfinavir as part of a combination of antiretrovirals. The nelfinavir dosage the mothers were taking was not stated in the abstract. The median breastmilk concentrations of nelfinavir were 49 mcg/L at a median of 14 hours after the last dose at 6 weeks postpartum (10 samples), 51 mcg/L at a median of 14 hours after the last dose at 12 weeks postpartum (7 samples), and 184 mcg/L at a median of 16 hours after the last dose at 24 weeks postpartum (9 samples). Median milk concentrations were 8% (interquartile range 4 to 14%) of maternal plasma concentrations.[6] In a related study by the same authors, the nelfinavir milk to plasma ratio was found to be 0.21 in 29 patients.[7]
Twenty-six breastfeeding Kenyan mothers were receiving oral nelfinavir 1.25 grams twice daily in addition to zidovudine and lamivudine for HIV infection. Blood and breastmilk samples were collected at delivery, and at 2, 6, 14, and 24 weeks postpartum at various times after the previous dose of nelfinavir. The 104 breastmilk samples were analyzed for nelfinavir and its active metabolite, hydroxyl-t-butylamidenelfinavir (M8). Median breastmilk nelfinavir concentrations were 83 mcg/L at birth, 358 mcg/L at 2 weeks, 286 mcg/L at 6 weeks, 233 mcg/L at 14 weeks and 180 mcg/L at 24 weeks postpartum. The M8 metabolite was undetectable (<10 mcg/L) in most samples; the highest concentrations found at any time was 32 mcg/L. Nelfinavir levels in breastmilk tended to drop during the dosing interval but M8 levels were relatively stable.[8]
Infant Levels. The infants of postpartum mothers taking nelfinavir as part of a combination of antiretrovirals had undetectable serum nelfinavir concentrations by HPLC/MS analysis. The nelfinavir dosage the mothers were taking and times of infant plasma sampling were not stated in the abstract. Nelfinavir was not detectable in infant plasma at 6, 12 or 24 weeks of age.[6]
Twenty-six breastfeeding Kenyan mothers were receiving oral nelfinavir 1.25 grams twice daily in addition to zidovudine and lamivudine for HIV infection. Infant blood samples were obtained at various times between 2 and 24 weeks postpartum. Nelfinavir and M8 concentration were undetectable (<10 mcg/L) for 20 of the 28 infant blood samples. The highest concentrations detected were 30 mcg/L for nelfinavir and 32 mcg/L for M8 which are less than the MIC for the HIV virus.[8]
Effects in Breastfed Infants
A study compared the frequency of rash, hepatotoxicity, and hyperbilirubinemia among 464 breastfed infants whose mothers were taking either nelfinavir (n = 206) or nevirapine (n = 258) along with zidovudine and lamivudine for HIV infection during pregnancy and postpartum. Infants were examined during the first, second and sixth weeks postpartum. Moderate rash occurred in 7 (2.7%) of the infant exposed to nevirapine and one (0.5%) infant exposed to nelfinavir. Rash occurred at a median of 2 weeks postpartum. Four infants (1.9%) exposed to nelfinavir developed hepatotoxicity (3 moderate and 1 severe) and none exposed to nevirapine. Twenty-one infants (4.5%) developed high-risk hyperbilirubinemia, all prior to 48 hours of age, but there was no difference in exposure between the two drugs.[9]
Effects on Lactation and Breastmilk
Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen.[10-12] Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients,[13,14] although this has been disputed.[15] The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
References
- 1.
- AIDSinfo. Panel on treatment of pregnant women with HIV infection and prevention of perinatal transmission. Recommendations for use of antiretroviral drugs in transmission in the United States, 2018: Counseling and management of women living with HIV who breastfeed.
- 2.
- World Health Organization. HIV and infant feeding: Update. 2007. http://whqlibdoc
.who .int/publications/2007 /9789241595964_eng.pdf - 3.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. 2021. https://www
.who.int/publications /i/item/9789240031593 [PubMed: 34370423] - 4.
- Department of Health and Human Services. Recommendations for the use of antiretroviral drugs during pregnancy and interventions to reduce perinatal HIV transmission in the United States. Infant feeding for individuals with HIV in the United States. 2023. https:
//clinicalinfohivgov /en/guidelines /perinatal/infant-feeding-individuals-hiv-united-states?view=full - 5.
- Colebunders R, Hodossy B, Burger D, et al. The effect of highly active antiretroviral treatment on viral load and antiretroviral drug levels in breast milk. AIDS 2005;19:1912-5. [PubMed: 16227801]
- 6.
- Corbett A, Kashuba A, Rezk N, et al. Antiretroviral drug concentrations in breast milk and breastfeeding infants. 15th Annual Conference on Retroviruses and Opportunistic Infections (CROI) 2/3/2008 to 2/6/2008; Boston, MA Poster # 648 2008.
- 7.
- Rezk NL, White N, Bridges AS, et al. Studies on antiretroviral drug concentrations in breast milk: Validation of a liquid chromatography-tandem mass spectrometric method for the determination of 7 anti-human immunodeficiency virus medications. Ther Drug Monit 2008;30:611-9. [PMC free article: PMC2901847] [PubMed: 18758393]
- 8.
- Weidle PJ, Zeh C, Martin A, et al. Nelfinavir and its active metabolite, hydroxyl-t-butylamidenelfinavir (M8), are transferred in low quantities to breast milk and do not result in biologically significant concentrations in breast-feeding infants whose mothers are taking nelfinavir. Antimicrob Agents Chemother 2011;55:5168-71. [PMC free article: PMC3195023] [PubMed: 21876052]
- 9.
- Minniear TD, Zeh C, Polle N, et al. Rash, hepatotoxicity and hyperbilirubinemia among Kenyan infants born to HIV-infected women receiving triple-antiretroviral drugs for the prevention of mother-to-child HIV transmission. Pediatr Infect Dis J 2012;31:1155-7. [PubMed: 22772167]
- 10.
- García-Benayas T, Blanco F, Martin-Carbonero L, et al. Gynecomastia in HIV-infected patients receiving antiretroviral therapy. AIDS Res Hum Retroviruses 2003;19:739-41. [PubMed: 14585204]
- 11.
- Pantanowitz L, Evans D, Gross PD, Dezube BJ. HIV-related gynecomastia. Breast J 2003;9:131-2. [PubMed: 12603389]
- 12.
- Evans DL, Pantanowitz L, Dezube BJ, Aboulafia DM. Breast enlargement in 13 men who were seropositive for human immunodeficiency virus. Clin Infect Dis 2002;35:1113-9. [PubMed: 12384846]
- 13.
- Hutchinson J, Murphy M, Harries R, Skinner CJ. Galactorrhoea and hyperprolactinaemia associated with protease-inhibitors. Lancet 2000;356:1003-4. [PubMed: 11041407]
- 14.
- Orlando G, Brunetti L, Vacca M. Ritonavir and saquinavir directly stimulate anterior pituitary prolactin secretion, in vitro. Int J Immunopathol Pharmacol 2002;15:65-8. [PubMed: 12593790]
- 15.
- Montero A, Bottasso OA, Luraghi MR, et al. Galactorrhoea, hyperprolactinaemia, and protease inhibitors. Lancet 2001;357:473-5. [PubMed: 11273087]
Substance Identification
Substance Name
Nelfinavir
CAS Registry Number
159989-64-7
Drug Class
Breast Feeding
Milk, Human
Anti-Infective Agents
Antiviral Agents
Anti-HIV Agents
Anti-Retroviral Agents
HIV Protease Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Saquinavir.[Drugs and Lactation Database (...]Review Saquinavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Indinavir.[Drugs and Lactation Database (...]Review Indinavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Atazanavir.[Drugs and Lactation Database (...]Review Atazanavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Lopinavir.[Drugs and Lactation Database (...]Review Lopinavir.. Drugs and Lactation Database (LactMed®). 2006
- Review Ritonavir.[Drugs and Lactation Database (...]Review Ritonavir.. Drugs and Lactation Database (LactMed®). 2006
- Nelfinavir - Drugs and Lactation Database (LactMed®)Nelfinavir - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
