Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
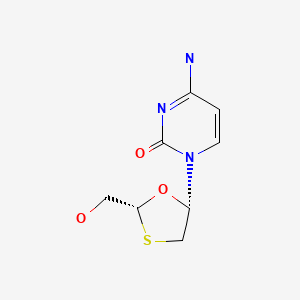
CASRN: 134678-17-4
Drug Levels and Effects
Summary of Use during Lactation
Lamivudine has been well studied in HIV-positive nursing mothers and appears to be well tolerated by their breastfed infants. It has not been studied in HIV-negative nursing mothers being treated for hepatitis B infection, but the low doses used would not be expected to cause any serious adverse effects in breastfed infants. The manufacturer estimates that a breastfed infant's dose would be about 6% of the infant dose for children over 2 years of age. Achieving and maintaining viral suppression with antiretroviral therapy decreases breastfeeding transmission risk to less than 1%, but not zero. Individuals with HIV who are on antiretroviral therapy with a sustained undetectable viral load and who choose to breastfeed should be supported in this decision. If a viral load is not suppressed, banked pasteurized donor milk or formula is recommended.[1,2]
An expert review of available data concluded that there is currently no justification for contraindicating the use of lamivudine for hepatitis B therapy during breastfeeding.[3] Some professional organization guidelines allow breastfeeding during lamivudine therapy, although one guideline cautions against it because of a lack of long-term safety data.[4-6] The lack of long-term safety data with long-term, low-level infant exposure should be discussed with the mother.[4] No differences exist in infection rates between breastfed and formula-fed infants born to hepatitis B-infected women, as long as the infant receives hepatitis B immune globulin and hepatitis B vaccine at birth. Mothers with hepatitis B are encouraged to breastfeed their infants after their infants receive these preventative measures.[7,8]
Drug Levels
Maternal Levels. Milk samples were taken daily before breastfeeding from 2 groups of women receiving lamivudine, one on monotherapy and the other on combination therapy. In the group receiving lamivudine 300 mg twice daily (n = 10), the average milk concentration was 1.2 mg/L (range <0.5 to 6.1 mg/L). In the group receiving 150 mg twice daily plus zidovudine (n = 10), the average milk lamivudine concentration was 0.9 mg/L (range <0.5 to 8.2 mg/L).[9]
Twenty women who were receiving oral lamivudine 150 mg twice daily as part of a combination antiretroviral regimen had their milk analyzed at either 2 or 5 months postpartum. Milk samples were provided at a median of 4 hours (range 1 to 8.5 hours) after the last dose. The median lamivudine concentration in breastmilk was 1.8 mg/L.[10]
Forty women were given postpartum prophylaxis with unstated dosages of lamivudine, nevirapine, and zidovudine (or stavudine if the hemoglobin <8 g/dL). Blood and milk samples were collected once during the first 3 days postpartum and once at 7 days postpartum. The median times after a dose that samples were collected were 5.3 hours (range 0 to 99 hours) for the first sample and 6 hours (range 4.3 to 20 hours) for the 7-day sample. Average breastmilk lamivudine concentrations were calculated only for samples that had detectable (>20 mcg/L) concentrations of lamivudine. The mean breastmilk concentrations were 0.4 (n = 9) and 0.4 mg/L (n = 30), respectively, at the two sampling times, which was 2.9 to 3.3 times the simultaneous maternal serum concentrations.[11]
Forty-seven samples of breastmilk and maternal serum were obtained at 6, 12 and 24 weeks postpartum from mothers taking lamivudine as part of a combination of antiretrovirals. The lamivudine dosage the mothers were taking was not stated in the abstract. The median breastmilk concentrations of lamivudine at a median of 14 hours after the last maternal dose were 510 (17 samples), 387 (17 samples) and 310 mcg/L (13 samples). Median milk concentrations were 2.6 times (interquartile range 1.1 to 3.5 times) the maternal plasma concentrations.[12] In a related study by the same authors, the lamivudine milk to plasma ratio was found to be 2.96 in 49 patients.[13]
Fifty-eight mothers who were taking a combination regimen of lamivudine, nevirapine and zidovudine had their serum and breastmilk analyzed for the presence of these drugs. Mothers took lamivudine 150 mg twice daily starting at 34 to 36 weeks postpartum and continuing until 6 months postpartum. Breastmilk was collected within 24 hours after delivery and at 2, 6, 14 and 24 weeks postpartum at variable times after the previous dose. The median breastmilk lamivudine concentration for 153 samples across all visits was 1214 mcg/L. The authors estimated that a fully breastfed infant would receive a daily dosage of 182 mcg/kg of lamivudine.[14]
Sixty-six mothers who were receiving lamivudine 150 mg twice daily as part of a combination antiretroviral regimen provided a total of 206 milk samples at birth, 1 month, 3 months and/or 6 months postpartum. Milk samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous dose. The median breastmilk lamivudine concentration was 446 mcg/L (range 269 to 683 mcg/L).[15] In a continuation of the same study, 65 breastmilk samples obtained at 1, 3 and 6 months postpartum were analyzed for lamivudine after the same dose. The median concentration was 684 mcg/L (IQR 405 to 868 mcg/L). It is not clear if the latter study included some of the same patients as the first study.[16]
Fifteen women had been taking lamivudine 150 mg twice daily for 53 to 182 days as part of a drug combination that included either abacavir and zidovudine or lopinavir, ritonavir, and zidovudine. Breastmilk samples were collected at just before a dose at a median of 1 month postpartum. Whole breastmilk levels contained a median of 0.14 mg/L of lamivudine, which was a median of 74% of maternal blood levels.[17]
Thirty women were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking zidovudine 300 mg, lamivudine 150 mg, lopinavir 400 mg, and ritonavir 100 mg twice daily by mouth starting at delivery. On the study day, at a median of 14.9 hours after the previous evening's dose, maternal plasma and breastmilk samples were obtained prior to the morning dose and 2, 4 and 6 hours after the dose. One hundred seven of the 121 breastmilk samples contained detectable quantities (10 mcg/L or greater) of lamivudine, with an median breastmilk concentration of 0.94 mg/L over the 6 hours.[18]
Women in Malawi received the option B+ regimen for prevention of mother-to-child transmission of HIV consisting of tenofovir, lamivudine and efavirenz between 6 and 8 pm daily. The lamivudine dose was not stated, but was presumably 300 mg daily. Milk samples collected in the morning from 33 women at month 1 postpartum had a median lamivudine concentration of 537 mcg/L (IQR 369 to 768 mcg/L). Milk samples collected in the morning from 47 women at month 12 postpartum had a median lamivudine concentration of 430 mcg/L (IQR 266 to 531 mcg/L).[19]
Lamivudine was measured in 6 HIV-positive nursing mothers during ongoing therapy with a dosage of 150 mg every 12 hours. A peak breastmilk level of 994 mcg/L (range 958-1274 mcg/L) was reached at 2 to 4 hours after the dose.[20]
Thirty-nine Nigerian and Ugandan women took lamivudine 150 mg twice daily (n = 11) or 300 mg once daily in the morning (n = 10) or previous evening (n = 18) as part of a combination therapy for HIV. Expressed milk samples were taken before the dose and at 0.5, 1, 2, 4, and 8 hours after the morning dose of 150 or 300 mg or samples between 12 to 20 hours after the 300 mg evening dose. The median peak breastmilk concentration from dried breastmilk spots in mothers taking 150 mg twice daily was 908 mcg/L (IQR 772 to 1015 mcg/L) at a median of 6 hours after the dose (IQR 4 to 6 hours). The median peak breastmilk concentration from dried breastmilk spots in mothers taking 300 mg once daily was 663 mcg/L (IQR 445 to 890 mcg/L) at a median of 6 hours after the dose (IQR 4 to 8 hours).[21]
Nine HIV-positive women about to undergo cesarean section received 3 doses of lopinavir 200 mg, ritonavir 150 mg, zidovudine 300 mg, lamivudine 50 mg at 3 hour intervals before the procedure. Breastmilk samples were collected at a mean of 25 hours postpartum. In the 8 women where it was quantified, the average milk concentration of lamivudine was 449 mcg/L (range 143 to 1148 mcg/L).[22]
Eleven mothers taking lamivudine 300 mg once daily provided milk samples at a median of 12.8 hours after a dose. The median drug concentration in milk was 1313 mcg/L, which resulted in an estimated infant dosage of 200 mcg/kg daily and a relative infant dose of 4.92% of the maternal weight-adjusted dosage.[23]
Infant Levels. Twenty nursing mothers were receiving oral lamivudine 150 mg twice daily as part of a combination antiretroviral regimen. Their infants had serum concentrations determined at either 2 or 5 months postpartum. Serum samples were provided at a median of 4 hours (range 1 to 8.5 hours) after the last dose. The median infant serum lamivudine concentration was 28 mcg/L (range <14 to 53 mcg/L). The average value was 5% of the IC50 for HIV.[10]
The infants of postpartum mothers taking nevirapine as part of a combination of antiretrovirals had undetectable serum nevirapine concentrations by HPLC/MS analysis. The lamivudine dosage the mothers were taking and times of infant plasma sampling were not stated in the abstract. Infant serum concentrations were measured at 6 (17 samples), 12 (17 samples), and 24 (13 samples) weeks of age at an average of 14 hours after the last maternal dose. Median infant serum lamivudine concentrations were 13, 10, and 5 mcg/L, respectively, which was 6% of the maternal serum concentration.[12]
Fifty-eight infants whose mothers were taking a combination regimen of lamivudine, nevirapine and zidovudine had their serum analyzed for the presence of these drugs. Mothers took lamivudine 150 mg twice daily starting at 34 to 36 weeks postpartum and continuing until 6 months postpartum and were instructed to exclusively breastfeed for 5.5 months. Serum samples were collected within 24 hours after delivery and at 2, 6, 14 and 24 weeks postpartum. The median infant dried blood spot lamivudine concentrations were 67 mcg/L at delivery, 32 mcg/L at week 2, 24 mcg/L at week 6, 20 mcg/L at week 14 and not measurable (<16 mcg/L) at week 24 postpartum.[14]
Breastfed infants of 66 mothers who were receiving lamivudine 150 mg twice daily as part of a combination antiretroviral regimen had a total of 64 blood samples analyzed at 1 month, 3 months and/or 6 months postpartum. Samples were collected at a median of 4.5 hours (range 3.5 to 6 hours) after the previous maternal dose and a median of 30 minutes (range 20 to 60 minutes) after the previous nursing. The median infants' lamivudine plasma concentration was 18 mcg/L (range 7 to 35 mcg/L), which was a median of 2% (range 0 to 4%) of the maternal serum concentration.[15] In a continuation of the same study, 17 breastfed infants (extent not stated) donated 22 blood samples between 1 and 6 months for lamivudine analysis. Their mothers were taking lamivudine 150 mg twice daily as part of combination antiretroviral regimens. The median concentration was 29.2 mcg/L (IQR 12.2 to 58.7 mcg/L). It is not clear if the latter study included some of the same patients as the first study.[16]
Twenty-four infants were breastfed either partially or exclusively by their mothers who had been taking lamivudine 150 mg twice daily for 53 to 182 days as part of a drug combination that included either abacavir and zidovudine or lopinavir, ritonavir, and zidovudine. Infant blood was collected at a median of 1 month postpartum at 11 to 18 hours after the last dose and a median of 1 hour (range 6 minutes to 35 hours) after the last breastfeeding. All of the infant plasma samples had undetectable (<7 mcg/L) plasma levels of lamivudine.[17]
Thirty nursing mothers were studied at 6, 12 or 24 weeks postpartum (10 at each time). Each mother was taking lamivudine 150 mg twice daily by mouth starting at delivery. Infant plasma samples were obtained before their mother's first dose and at 2, 4 and 6 hours after the mother's dose. Infants were allowed to breastfeed ad libitum during the study period. Lamivudine was detectable (10 mcg/L or greater) in 107 of the 115 infant plasma samples, at a median concentration of 180 mcg/L.[18]
Blood samples were taken from 25 breastfed infants of mothers who were receiving option B+ regimen for prevention of mother-to-child transmission of HIV consisting of tenofovir, lamivudine and efavirenz between 6 and 8 pm daily. The lamivudine dose was not stated, but was presumably 300 mg daily. The median morning infant plasma concentration of lamivudine at 6 months of age was 2.5 mcg/L (IQR 2.5 to 7.6 mcg/L). The median morning infant plasma concentration of lamivudine at 12 months of age was 0 mcg/L.[19]
Lamivudine 150 mg twice daily was given to 6 HIV-positive nursing mothers. Two of their breastfed infants had detectable lamivudine serum levels of 13.2 and 15.6 mcg/L.[20]
Thirty-nine Nigerian and Ugandan women took lamivudine 300 mg once daily in the morning (n = 10) or previous evening (n = 18) or 150 mg twice daily (n = 11) as part of a combination therapy for HIV. Their exclusively breastfed infants were fed on demand and had blood samples taken at 2 and 8 hours after the dose. Lamivudine was detectable (>16.6 mcg/L) in the dried blood spots of 36% (14 of 39) of infants, at a median of 17.7 mcg/L (IQR 16.3 to 22.7 mcg/L). Of these, detectable levels were found in 7 of 10 (70%) infants whose mothers had 300 mg once daily in the morning, in 4 of 18 (22%) of those whose mothers had taken their dose the previous evening, and in 3 of 11 (27%) infants whose mothers were given the drug twice daily.[21]
Four infants were breastfed by mothers taking lamivudine 300 mg once daily, although the extent of breastfeeding was not sated. Infant serum concentrations taken between 11 and 18 hours after maternal drug intake at 1 month of age ranged from 4 to 91 mcg/L.[23]
Effects in Breastfed Infants
A study assigned pregnant women to zidovudine alone or highly active antiretroviral therapy (HAART: zidovudine, lamivudine and nevirapine) to prevent maternal-to-child transmission of HIV infection. After delivery, all infants received one month of zidovudine prophylaxis; some infants were breastfed and others were formula fed. A higher percentage of infants in the HAART-exposed group had neutropenia than those in the unexposed group at 1 month of age (15.9% and 3.7%, respectively). Hematologic toxicity was transient and asymptomatic. From 2 to 6 months postpartum, no differences in hematologic toxicity were seen between breastfed and formula-fed infants. No statistical difference in hepatic toxicity was seen between the breastfed and formula-fed infants.[24]
Twenty-four infants who were breastfed by HIV-positive mothers developed HIV infection by 6 months of age. Six of these infants had a mutation that might have been selected for by subtherapeutic levels of lamivudine in breastmilk.[25]
An HIV-positive mother took a combination tablet containing dolutegravir 50 mg, abacavir sulfate 600 mg and lamivudine 300 mg (Triumeq) once daily. Her infant was exclusively breastfed for about 30 weeks and partially breastfed for about 20 weeks more. No obvious side effects were noted.[26]
One mother took lamivudine for 33 days, 25 before birth and eight days postpartum for chronic hepatitis B infection. Her infant was breastfed (extent not stated). At three months of age, the infant died with the death attributed to sudden infant death syndrome. The death was unlikely to be related to lamivudine.[27]
Effects on Lactation and Breastmilk
Gynecomastia has been reported among men receiving highly active antiretroviral therapy. Gynecomastia is unilateral initially, but progresses to bilateral in about half of cases. No alterations in serum prolactin were noted and spontaneous resolution usually occurred within one year, even with continuation of the regimen.[28-30] Some case reports and in vitro studies have suggested that protease inhibitors might cause hyperprolactinemia and galactorrhea in some male patients,[31,32] although this has been disputed.[33] The relevance of these findings to nursing mothers is not known. The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
Alternate Drugs to Consider
(Hepatitis B) Interferon Alfa, Tenofovir
References
- 1.
- World Health Organization. Consolidated guidelines on HIV prevention, testing, treatment, service delivery and monitoring: recommendations for a public health approach. 2021. https://www
.who.int/publications /i/item/9789240031593 [PubMed: 34370423] - 2.
- Department of Health and Human Services. Recommendations for the use of antiretroviral drugs during pregnancy and interventions to reduce perinatal HIV transmission in the United States. Infant feeding for individuals with HIV in the United States. 2023. https:
//clinicalinfohivgov /en/guidelines /perinatal/infant-feeding-individuals-hiv-united-states?view=full - 3.
- Ehrhardt S, Xie C, Guo N, et al. Breastfeeding while taking lamivudine or tenofovir disoproxil fumarate: A review of the evidence. Clin Infect Dis 2015;60:275-8. [PubMed: 25313254]
- 4.
- Terrault NA, Bzowej NH, Chang KM, et al. AASLD guidelines for treatment of chronic hepatitis B. Hepatology 2016;63:261-83. [PMC free article: PMC5987259] [PubMed: 26566064]
- 5.
- EASL 2017 Clinical practice guidelines on the management of hepatitis B virus infection. J Hepatol 2017;67:370-98. [PubMed: 28427875]
- 6.
- Sarin SK, Kumar M, Lau GK, et al. Asian-Pacific clinical practice guidelines on the management of hepatitis B: A 2015 update. Hepatol Int 2016;10:1-98. [PMC free article: PMC4722087] [PubMed: 26563120]
- 7.
- Visvanathan K, Dusheiko G, Giles M, et al. Managing HBV in pregnancy. Prevention, prophylaxis, treatment and follow-up: Position paper produced by Australian, UK and New Zealand key opinion leaders. Gut 2016;65:340-50. [PubMed: 26475631]
- 8.
- Dionne-Odom J, Tita AT, Silverman NS. #38: Hepatitis B in pregnancy screening, treatment, and prevention of vertical transmission. Am J Obstet Gynecol 2016;214:6-14. [PubMed: 26454123]
- 9.
- Moodley J, Moodley D, Pillay K, et al. Pharmacokinetics and antiretroviral activity of lamivudine alone or when coadministered with zidovudine in human immunodeficiency virus type 1-infected pregnant women and their offspring. J Infect Dis 1998;178:1327-33. [PubMed: 9780252]
- 10.
- Shapiro RL, Holland DT, Capparelli E, et al. Antiretroviral concentrations in breast-feeding infants of women in Botswana receiving antiretroviral treatment. J Infect Dis 2005;192:720-7. [PubMed: 16088821]
- 11.
- Giuliano M, Guidotti G, Andreotti M, et al. Triple antiretroviral prophylaxis administered during pregnancy and after delivery significantly reduces breast milk viral load study within the Drug Resource Enhancement Against AIDS and Malnutrition Program. J Acquir Immune Defic Syndr 2007;44:286-91. [PubMed: 17146372]
- 12.
- Corbett A, Kashuba A, Rezk N, et al. Antiretroviral drug concentrations in breast milk and breastfeeding infants. 15th Annual Conference on Retroviruses and Opportunistic Infections (CROI) 2/3/2008 to 2/6/2008; Boston, MA Poster # 648 2008.
- 13.
- Rezk NL, White N, Bridges AS, et al. Studies on antiretroviral drug concentrations in breast milk: Validation of a liquid chromatography-tandem mass spectrometric method for the determination of 7 anti-human immunodeficiency virus medications. Ther Drug Monit 2008;30:611-9. [PMC free article: PMC2901847] [PubMed: 18758393]
- 14.
- Mirochnick M, Thomas T, Capparelli E, et al. Antiretroviral concentrations in breast-feeding infants of mothers receiving highly active antiretroviral therapy. Antimicrob Agents Chemother 2009;53:1170-6. [PMC free article: PMC2650559] [PubMed: 19114673]
- 15.
- Palombi L, Pirillo MF, Andreotti M, et al. Antiretroviral prophylaxis for breastfeeding transmission in Malawi: drug concentrations, virological efficacy and safety. Antivir Ther 2012;17:1511-9. [PubMed: 22910456]
- 16.
- Pirillo MF, Scarcella P, Andreotti M, et al. Hepatitis B virus mother-to-child transmission among HIV-infected women receiving lamivudine-containing antiretroviral regimens during pregnancy and breastfeeding. J Viral Hepat 2015;22:289-96. [PubMed: 25174900]
- 17.
- Shapiro RL, Rossi S, Ogwu A, et al. Therapeutic levels of lopinavir in late pregnancy and abacavir passage into breast milk, in the Mma Bana Study, Botswana. Antivir Ther 2013;18:585-90. [PMC free article: PMC5502724] [PubMed: 23183881]
- 18.
- Corbett AH, Kayira D, White NR, et al. Antiretroviral pharmacokinetics in mothers and breastfeeding infants from 6 to 24 weeks post-partum: Results of the BAN Study. Antivir Ther 2014;19:587-95. [PMC free article: PMC4110187] [PubMed: 24464632]
- 19.
- Palombi L, Pirillo MF, Marchei E, et al. Concentrations of tenofovir, lamivudine and efavirenz in mothers and children enrolled under the Option B-Plus approach in Malawi. J Antimicrob Chemother 2016;71:1027-30. [PubMed: 26679247]
- 20.
- Waitt C, Diliiy Penchala S, Olagunju A, et al. Development, validation and clinical application of a method for the simultaneous quantification of lamivudine, emtricitabine and tenofovir in dried blood and dried breast milk spots using LC–MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci 2017;1060:300-7. [PMC free article: PMC5588985] [PubMed: 28651173]
- 21.
- Waitt C, Olagunju A, Nakalema S, et al. Plasma and breast milk pharmacokinetics of emtricitabine, tenofovir and lamivudine using dried blood and breast milk spots in nursing African mother-infant pairs. J Antimicrob Chemother 2018;73:1013-9. [PMC free article: PMC5890695] [PubMed: 29309634]
- 22.
- Ramírez-Ramírez A, Sanchez-Serrano E, Loaiza-Flores G, et al. Simultaneous quantification of four antiretroviral drugs in breast milk samples from HIV-positive women by an ultra-high performance liquid chromatography tandem mass spectrometry (UPLC-MS/MS) method. PLoS One 2018;13:e0191236. [PMC free article: PMC5774716] [PubMed: 29351333]
- 23.
- Aebi-Popp K, Kahlert CR, Crisinel PA, et al. Transfer of antiretroviral drugs into breastmilk: A prospective study from the Swiss Mother and Child HIV Cohort Study. J Antimicrob Chemother 2022;77:3436-42. [PMC free article: PMC9704434] [PubMed: 36177836]
- 24.
- Bae WH, Wester C, Smeaton LM, et al. Hematologic and hepatic toxicities associated with antenatal and postnatal exposure to maternal highly active antiretroviral therapy among infants. AIDS 2008;22:1633-40. [PMC free article: PMC2664540] [PubMed: 18670224]
- 25.
- Inzaule SC, Weidle PJ, Yang C, et al. Prevalence and dynamics of the K65R drug resistance mutation in HIV-1-infected infants exposed to maternal therapy with lamivudine, zidovudine and either nevirapine or nelfinavir in breast milk. J Antimicrob Chemother 2016;71:1619-26. [PubMed: 26953333]
- 26.
- Kobbe R, Schalkwijk S, Dunay G, et al. Dolutegravir in breast milk and maternal and infant plasma during breastfeeding. AIDS 2016;30:2731-3. [PubMed: 27782968]
- 27.
- Greenup AJ, Tan PK, Nguyen V, et al. Efficacy and safety of tenofovir disoproxil fumarate in pregnancy to prevent perinatal transmission of hepatitis B virus. J Hepatol 2014;61:502-7. [PubMed: 24801414]
- 28.
- García-Benayas T, Blanco F, Martin-Carbonero L, et al. Gynecomastia in HIV-infected patients receiving antiretroviral therapy. AIDS Res Hum Retroviruses 2003;19:739-41. [PubMed: 14585204]
- 29.
- Pantanowitz L, Evans D, Gross PD, Dezube BJ. HIV-related gynecomastia. Breast J 2003;9:131-2. [PubMed: 12603389]
- 30.
- Evans DL, Pantanowitz L, Dezube BJ, Aboulafia DM. Breast enlargement in 13 men who were seropositive for human immunodeficiency virus. Clin Infect Dis 2002;35:1113-9. [PubMed: 12384846]
- 31.
- Hutchinson J, Murphy M, Harries R, Skinner CJ. Galactorrhoea and hyperprolactinaemia associated with protease-inhibitors. Lancet 2000;356:1003-4. [PubMed: 11041407]
- 32.
- Orlando G, Brunetti L, Vacca M. Ritonavir and saquinavir directly stimulate anterior pituitary prolactin secretion, in vitro. Int J Immunopathol Pharmacol 2002;15:65-8. [PubMed: 12593790]
- 33.
- Montero A, Bottasso OA, Luraghi MR, et al. Galactorrhoea, hyperprolactinaemia, and protease inhibitors. Lancet 2001;357:473-5. [PubMed: 11273087]
Substance Identification
Substance Name
Lamivudine
CAS Registry Number
134678-17-4
Drug Class
Breast Feeding
Milk, Human
Anti-Infective Agents
Antiviral Agents
Anti-HIV Agents
Anti-Retroviral Agents
Reverse Transcriptase Inhibitors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Emtricitabine.[Drugs and Lactation Database (...]Review Emtricitabine.. Drugs and Lactation Database (LactMed®). 2006
- Review Tenofovir.[Drugs and Lactation Database (...]Review Tenofovir.. Drugs and Lactation Database (LactMed®). 2006
- Review Zidovudine.[Drugs and Lactation Database (...]Review Zidovudine.. Drugs and Lactation Database (LactMed®). 2006
- Review Nevirapine.[Drugs and Lactation Database (...]Review Nevirapine.. Drugs and Lactation Database (LactMed®). 2006
- Toxicology and Carcinogenesis Studies of Mixtures of 3'-Azido-3'-Deoxythymidine (AZT), Lamivudine (3TC), and Nevirapine (NVP) (CAS Nos. 30516-87-1, 134678-17-4, 129618-40-2) in Genetically Modified C3B6.129F1-Trp53(tm1Brd) N12 Haploinsufficient Mice (in utero and postnatal gavage studies).[Natl Toxicol Program Genet Mod...]Toxicology and Carcinogenesis Studies of Mixtures of 3'-Azido-3'-Deoxythymidine (AZT), Lamivudine (3TC), and Nevirapine (NVP) (CAS Nos. 30516-87-1, 134678-17-4, 129618-40-2) in Genetically Modified C3B6.129F1-Trp53(tm1Brd) N12 Haploinsufficient Mice (in utero and postnatal gavage studies).National Toxicology Program. Natl Toxicol Program Genet Modif Model Rep. 2013 Oct; (16):1-236.
- Lamivudine - Drugs and Lactation Database (LactMed®)Lamivudine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
