Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 15676-16-1
Drug Levels and Effects
Summary of Use during Lactation
Sulpiride is not approved for marketing in the United States by the U.S. Food and Drug Administration, but is used as a psychotherapeutic agent and galactogogue in other countries. Sulpiride increases serum prolactin, but its clinical value in increasing milk supply is questionable. In a study that enrolled only mothers with documented low milk production a few weeks postpartum, sulpiride was effective in increasing milk volume, but it was only more effective than placebo in avoiding supplementation in those with no initial milk production. Galactogogues should never replace evaluation and counseling on modifiable factors that affect milk production.[1,2] If mothers are provided instruction in good breastfeeding technique and breastfeed frequently, sulpiride is unlikely to provide additional benefit. Whether sulpiride has any benefit as a galactogogue in women who continue to have insufficient milk production after nursing technique and frequency have been optimized has not been studied adequately.
Sulpiride is excreted into breastmilk in rather large amounts, far above the accepted value of 10% of the maternal weight-adjusted dosage in some cases, but blood concentrations in breastfed infants have not been evaluated. Two studies found no adverse effects in breastfed infants whose mothers were treated with sulpiride for 2 to 4 weeks as a galactogogue, although others estimated that the dose in milk was high enough to increase serum prolactin in breastfed infants.[3]
Postpartum mothers are at a relatively high risk for postpartum depression and sulpiride can cause depression as a side effect. Therefore, sulpiride should be avoided in women with a history of major depression and not used for prolonged periods in any mothers during this time of high susceptibility. Tiredness occurred occasionally and cases of headache and leg edema have also been reported in nursing mothers taking sulpiride as a galactogogue.[4,5]
Drug Levels
Maternal Levels. In a study reported only in abstract form, sulpiride was not detected in milk (study details and assay limit not stated) with maternal dosages of up to 200 mg daily.[6]
Twenty women were taking sulpiride 50 mg twice daily by mouth to enhance milk production. A single milk sample from each woman was taken at 2 hours after the morning dose between the 3rd to the 7th day of therapy. The average milk sulpiride concentration was 970 mcg/L (range 260 to 1970 mcg/L).[7] This translates to an average daily maximum infant dosage of 146 mcg/kg (range 39 to 297 mcg/kg) in the infant or 8.7% (range 2 to 18%) of the weight-adjusted maternal dosage.
Single doses of sulpiride of either 3 mg (n = 5) or 10 mg (n = 4) were given to nursing mothers. After 3 mg, peak milk concentrations ranged from 10 to 37 mcg/L and trough concentrations ranged from 9 to 13 mcg/L. After 10 mg, peak milk concentrations ranged from 37 to 293 mcg/L and trough concentrations ranged from 29 to 85 mcg/L. The authors calculated that a 24-hlur dose to the infant would range from 1.2 to 9.9 mcg after a 3 mg maternal dose and from 3.8 to 46.3 mcg after a 10 mg maternal dose.[3]
A woman with dissociative disorder and persistent dysthymic depression was treated during pregnancy with brotizolam 0.25 mg daily, propericiazine 10 mg daily, and zolpidem 5 mg daily. Zolpidem was discontinued at week 28 and sulpiride 100 mg daily was begun at week 33. Milk samples taken at 7.5 and 11.5 hours after the previous dose on day 9 postpartum contained 445.8 and 192.2 mcg/L of sulpiride, respectively.[8]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
In a study of 14 women given sulpiride 50 mg 3 times daily for 4 weeks, no side effects were reported in their breastfed infants.[5]
In a study of 24 nursing mothers who received sulpiride 50 mg 3 times daily for 2 weeks, no side effects were reported in their breastfed infants.[4]
In a study comparing sulpiride to placebo for enhancement of milk production, infant weight gain was greater in the infants of treated women up to day 15, but there was no difference in weight gain between the groups thereafter.[9]
Effects on Lactation and Breastmilk
Sulpiride increases serum prolactin and may cause galactorrhea at a higher rate than other psychotropic drugs.[10-14] The levo- isomer, levosulpiride, which is available abroad, has also caused hyperprolactinemia and galactorrhea.[15]
Several studies have been published on the use of sulpiride in enhancing milk supply.[4,5,7,9,10,16,17] Most of the studies have serious design flaws. Although these studies were all placebo controlled, only 3 studies were blinded and randomized.
In one study, 28 women were randomized to sulpiride 50 mg (n = 14) or placebo (n = 14) 3 times daily for 4 weeks. Women were within 4 months postpartum and had identified themselves as having insufficient milk. The two groups were fairly well matched at the initiation of the trial, except that mothers in the placebo group had been supplementing for longer than women in the sulpiride group, 33 and 22 days, respectively. Mothers in both groups fed their infants an average of 5.3 times daily. Mothers were given no instruction on breastfeeding technique. Serum prolactin rose in sulpiride-treated patients to about 400 mcg/L and fell slightly in placebo-treated patients. However, neither milk yields at the beginning of the study nor increases in yield showed any relationship to increases in serum prolactin. Infant weight gain was greater in the treated patients at the end of the study (1081 vs 795 grams); however, most of the infants in both groups were given supplementary feedings, so it is impossible to tell if the weight gain in the sulpiride group was caused by increased milk production or by the supplementation.[5]
A study of 66 primiparous mothers with normal infants who expressed a desire to breastfeed, received sulpiride 100 mg 3 times daily for the first 4 days postpartum, then 50 mg 3 times daily for the next 86 days. Mothers who received sulpiride maintained elevated baseline serum prolactin levels of 117 to 119 mcg/L throughout the 90-day study period. Mothers taking placebo had a normal drop in serum prolactin from 113 mcg/L on day 1 to 20 mcg/L on day 90; however, on days 4, 15 and 30, their 30-minute postsuckling prolactin levels reached about the same levels as the sulpiride-treated mothers because they had very small increases in prolactin after nursing. At days 60 and 90, women taking placebo had much lower baseline and postsuckling prolactin levels than treated women. Infant weight gain was greater in the infants of treated women up to day 15, but there was no difference between the groups thereafter.[9] This study suffered from a high 38% dropout rate, which makes intent-to-treat analysis unfeasible.
A randomized, double-blind trial studied 60 women who were 25 to 40 days postpartum, 40 with insufficient lactation averaging 293 mL daily and 20 with no milk production at the start of the study. No mention was made of any lactation education given to the subjects before or during the study or the frequency of nursing during the study. Subjects were given l-sulpiride, d-sulpiride or d,l-sulpiride 50 mg twice daily or placebo for 15 days. Milk production increased in all drug groups. All women with insufficient lactation, including those receiving placebo, could avoid supplementation after 6 days of therapy. Women with no milk production at the start who received a drug were able to stop supplementation after 10 to 15 days; those in the placebo group were not able to breastfeed at the end of the study. The authors state that the increased milk production declined progressively after drug discontinuation, but did not provide any data.[10]
Alternate Drugs to Consider
(Galactogogue) Domperidone, Metoclopramide
References
- 1.
- Brodribb W. ABM Clinical Protocol #9: Use of galactogogues in initiating or augmenting maternal milk production, second revision 2018. Breastfeed Med 2018;13:307-14. [PubMed: 29902083]
- 2.
- Breastfeeding challenges: ACOG Committee Opinion, Number 820. Obstet Gynecol 2021;137:e42-e53. [PubMed: 33481531]
- 3.
- Moreland TA, Donnet ML, McEwen J, et al. Sulpiride excretion in lactating mothers. Eur J Clin Pharmacol 1989;36 (Suppl):A153. doi:10.1007/BF02411402 [CrossRef]
- 4.
- Ylikorkala O, Kauppila A, Kivinen S, et al. Treatment of inadequate lactation with oral sulpiride and buccal oxytocin. Obstet Gynecol 1984;63:57-60. [PubMed: 6361642]
- 5.
- Ylikorkala O, Kauppila A, Kivinen S, et al. Sulpiride improves inadequate lactation. Br Med J (Clin Res Ed) 1982;285:249-51. [PMC free article: PMC1499674] [PubMed: 6807435]
- 6.
- Badroui MH, Hefnawi F, Hegab M, et al. The effect of a nonhormonal drug used as a contraceptive method and lactation stimulant after delivery. Fertil Steril 1978;30:742. [Abstract].
- 7.
- Aono T, Shioji T, Aki T, et al. Augmentation of puerperal lactation by oral administration of sulpiride. J Clin Endocrinol Metab 1979;48:478-82. [PubMed: 429499]
- 8.
- Saito J, Tachibana Y, Wada YS, et al. Transfer of brotizolam, periciazine, and sulpiride in cord blood and breast milk, and alprazolam in breast milk: A case report. J Pharm Health Care Sci 2022;8:10. [PMC free article: PMC8973510] [PubMed: 35361275]
- 9.
- Barguño JM, del Pozo E, Cruz M, et al. Failure of maintained hyperprolactinemia to improve lactational performance in late puerperium. J Clin Endocrinol Metab 1988;66:876-9. [PubMed: 3346364]
- 10.
- Polatti F. Sulpiride isomers and milk secretion in puerperium. Clin Exp Obstet Gynecol 1982;9:144-7. [PubMed: 6762263]
- 11.
- McMurdo ME, Howie PW, Lewis M, et al. Prolactin response to low dose sulpiride. Br J Clin Pharmacol 1987;24:133-7. [PMC free article: PMC1387741] [PubMed: 3620290]
- 12.
- Hanew K, Utsumi A, Sugawara A, et al. Simultaneous administration of TRH and sulpiride caused additive but not synergistic PRL rsesponses in normal subjects. Endocrinol Jpn 1992;39:465-8. [PubMed: 1478187]
- 13.
- Kropp S, Ziegenbein M, Grohmann R, et al. Galactorrhea due to psychotropic drugs. Pharmacopsychiatry 2004;37 (Suppl 1):S84-8. [PubMed: 15052519]
- 14.
- Lu ML, Shen WW, Chen CH. Time course of the changes in antipsychotic-induced hyperprolactinemia following the switch to aripiprazole. Prog Neuropsychopharmacol Biol Psychiatry 2008;32:1978-81. [PubMed: 18848860]
- 15.
- Mahto SK, Agarwal N, Gupta K, et al. A rare side effect of levosulpiride: Galactorrhea. Indian J Pharmacol 2021;53:76-7. [PMC free article: PMC8216124] [PubMed: 33976003]
- 16.
- Polatti F, Brambilla A, Mandelli B, et al. Can pharmacologic hyperprolactinemia and breast-suction induce lactation in women with normal menstrual cycles? Clin Exp Obstet Gynecol 1984;11:123-5. [PubMed: 6499184]
- 17.
- Aono T, Aki T, Koike K, et al. Effect of sulpiride on poor puerperal lactation. Am J Obstet Gynecol 1982;143:927-32. [PubMed: 7102768]
Substance Identification
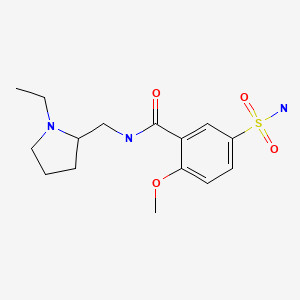
Substance Name
Sulpiride
CAS Registry Number
15676-16-1
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Metoclopramide.[Drugs and Lactation Database (...]Review Metoclopramide.. Drugs and Lactation Database (LactMed®). 2006
- Review Domperidone.[Drugs and Lactation Database (...]Review Domperidone.. Drugs and Lactation Database (LactMed®). 2006
- Review Fenugreek.[Drugs and Lactation Database (...]Review Fenugreek.. Drugs and Lactation Database (LactMed®). 2006
- Review Marine Oils.[Drugs and Lactation Database (...]Review Marine Oils.. Drugs and Lactation Database (LactMed®). 2006
- Review Alcohol.[Drugs and Lactation Database (...]Review Alcohol.. Drugs and Lactation Database (LactMed®). 2006
- Sulpiride - Drugs and Lactation Database (LactMed®)Sulpiride - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
