Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 25655-41-8
Drug Levels and Effects
Summary of Use during Lactation
The use of povidone-iodine in the mother near term and during breastfeeding increases breastmilk iodine levels and can cause transient hypothyroidism in breastfed infants, especially in geographic areas that are iodine deficient. Maternal exposure to povidone-iodine near term can sometimes interfere with thyroid studies done as a part of newborn screening tests. Although iodine from povidone-iodine is minimally absorbed through intact adult skin, exposure of mothers who are or will be breastfeeding to povidone-iodine should be minimized by using lower concentrations of povidone-iodine, applying it to the smallest possible surface areas of the body, shortening contact time, and avoiding repeated applications. If povidone iodine is removed from the abdomen with alcohol within several minutes after its application for cesarean section delivery, it is absorbed into the bloodstream and excreted in breastmilk, but may not affect neonatal urinary iodine, TSH or FT4 during the perinatal period.[1] Iodine absorption can be extensive with vaginal use; avoid douching with povidone iodine or use of iodine-containing tampons during breastfeeding.
Drug Levels
Maternal Levels. Random samples of breastmilk from day 5 postpartum in 140 women were analyzed for iodine content. Iodine levels in milk samples were 0.095 mg/L in mothers not exposed to any iodine (n = 91). In women who had 10% povidone iodine (10 mg/mL of iodine) topically applied, iodine levels were about 0.14 mg/L in women who had it applied once to 900 square cm of skin for epidural analgesia (n = 39), and about 1.2 mg/L in women who it applied to the entire abdominal wall 3 times before cesarean section (n = 10).[2]
Iodine milk levels were measured in a study of mothers who received 10% povidone-iodine (n = 21) or chlorhexidine (n = 13) topically to the perineum starting immediately before the final stage of labor and daily postpartum to the episiotomy. At 96 hours postpartum, milk iodine levels averaged 1.2 mg/L in mothers who received topical povidone-iodine compared to average milk levels of 0.1 mg/L in the mothers who received chlorhexidine.[3]
A study randomized 80 consecutive term patients into 4 groups who received either povidone-iodine or benzalkonium chloride as a skin disinfectant before delivery and one of these for postpartum vaginal lacerations. Prepartum doses were about 7 mL and postpartum doses were about 0.5 mL. The calculated amount of iodine ingested by the infants in breastmilk during the first 5 days of life correlated well with the amount of povidone-iodine applied to their mothers' skin. Patients who received prepartum povidone-iodine had higher median breastmilk iodide levels on day 5 postpartum than those not exposed (0.93 mg/L pre- and postpartum, 0.76 mg/L prepartum only); those with only postpartum povidone-iodine did not have elevated iodine milk levels (0.62 to 0.64 mg/L).[4]
A nursing mother who was 7.5 months postpartum used povidone-iodine gel containing 50 mg of iodine per 5 gram dose vaginally once daily for 6 days. Three days after discontinuing the gel, total milk iodine levels were 0.55 mg/L which was 3 to 4 times the typical milk iodine levels and over 6 times her serum iodine level. Total iodine levels fell to 0.1 mg/L by day 7 and inexplicably increased to 0.23 mg/L on day 8 after stopping.[5]
A woman began vaginal douching twice daily with povidone-iodine after delivery. On day 22 postpartum, her breastmilk iodine levels were extremely elevated at 5 micromoles/L. After discontinuing douching, her breastmilk iodine levels dropped to normal levels of less than 1 micromole/L by 7 days after discontinuing povidone-iodine douching.[6]
Infant Levels. In a study in Belgium, breastfed infants had urinary iodine levels measured at 5 days of age. Infants whose mothers were not exposed to any iodine (n = 23) had urinary iodine levels of 0.144 mg/L, those whose mothers had 10% povidone-iodine applied to 900 square cm before epidural analgesia (n = 27) had urinary iodine levels of about 0.28 mg/L, and those whose mothers had 10% povidone iodine applied 3 times to their entire abdomen (n = 11) had urinary iodine levels of 1.84 mg/L.[2]
The mother of a 7.5 month-old breastfed (extent not stated) infant used povidone-iodine gel containing 50 mg per 5 gram dose vaginally once daily for 6 days. Two days later, she noted the odor of iodine on her infant. The infant's serum and urinary iodine levels were extremely elevated, with a serum total iodine level of 0.13 mg/L and a urinary level of 1.02 mg/L or 6.8 mg/gram of creatinine. Serum thyroxine and thyrotropin (TSH) were normal.[5]
A woman began using povidone-iodine as a vaginal douche twice daily after delivery. Her breastfed infant developed hypothyroidism accompanied by high urine iodine levels of about 4 micromoles/L. The infant's urine iodine levels were about 0.3 micromoles/L by 2 weeks after the mother discontinued douching.[6]
In a study of mothers who received 10% povidone-iodine (n = 21) or chlorhexidine (n = 13) topically to the perineum starting immediately before the final stage of labor and daily postpartum to the episiotomy, urine iodine levels were measured in their infants. In the infants whose mothers received povidone-iodine, urine iodine levels were much higher at 24 and 48 hours postpartum. At 96 hours postpartum, the breastfed infants (n = 13) infants whose mothers received povidone-iodine had urine iodine levels of 8.3 mg/L compared to levels of 0.4 mg/L in those who did not breastfeed (n = 8) and 0.6 mg/L in the infants of mothers who received chlorhexidine (n = 13).[3]
Effects in Breastfed Infants
In a study in Belgium, breastfed infants had thyroid function tests measured at 5 days of age. Both basal and thyrotropin-releasing hormone-stimulated thyrotropin (TSH) levels were higher in infants exposed to the breastmilk from mothers who received topical povidone-iodine during delivery. Serum thyroxine (T4) and liothyronine (T3) levels were normal in all groups.[2]
A woman began bathing almost daily with povidone-iodine (1% iodine) and applying povidone-iodine 1% ointment to her skin daily during pregnancy and for 6 weeks postpartum for furunculosis. At 6 weeks of age, her breastfed (extent not stated) infant had a low serum thyroxine level of 4 ng/L (normal 7 to 20 ng/L), a greatly elevated serum thyrotropin level of 99 units/L (normal 0.8 to 5 units/L). The infant was treated with oral levothyroxine until the age of 7 months at which time thyroid function tests and development were normal.[7]
A woman began using povidone-iodine as a vaginal douche twice daily after delivery. Her breastfed infant developed hypothyroidism (low serum thyroxine and high thyrotropin) over the first 3 weeks of life. After oral levothyroxine supplementation of the infant was begun and maternal povidone-iodine was discontinued, the infant's thyroid function tests normalized within a week.[6]
A group of investigators in Belgium reviewed the results of infant thyrotropin levels on day 5 postpartum in 4745 newborn infants delivered over a 2-year period at their hospital. Infants were divided among those whose mothers had iodine overload (n = 3086) from topical povidone-iodine 10% solution during labor and delivery and those whose mothers had no iodine overload (n = 1659). Mothers had povidone-iodine applied either as a single application to 900 square cm for epidural anesthesia or 3 applications to the entire abdominal wall for cesarean section. Breastfed infants whose mothers had iodine overload had a greater risk for having elevated thyrotropin levels and requiring recall for retesting (3.2% with cesarean section and 2.7% with epidural anesthesia) compared to those who did not (0.1%). Bottle-fed infants were affected much less than breastfed infants.[8] After replacing povidone-iodine with chlorhexidine 0.5% in 70% isopropanol for disinfection for 6 months, 1178 infants that were delivered at this institution had no increased rate of elevations in thyroid function tests and a reduced rate of recalls in breastfed infants.[9]
In a study of mothers in Spain who received 10% povidone-iodine (n = 21) or chlorhexidine (n = 13) topically to the perineum starting immediately before the final stage of labor and daily postpartum to the episiotomy, no differences in thyrotropin, thyroxine or free thyroxine was found among their breastfed infants at day 5 to 7 postpartum.[3]
A breastfed infant whose mother was using povidone-iodine as a douche during pregnancy and during the first few weeks after delivery had symptoms of sinus tachycardia and increased concentrations of blood total and free thyroxine at 10 days of age and elevated thyrotropin at 1 month of age. The povidone-iodine was discontinued and the infant's total thyroxine normalized by 1 month of age, free thyroxine normalized by 1.5 months of age and the thyrotropin level normalized by 2.5 months of age. No other explanation for the thyroid function abnormalities could be found except maternal povidone-iodine use, but blood and milk iodine levels were not measured. Povidone-iodine was the probable cause of the adverse reaction in the infant.[10]
A study in Japan randomized 80 consecutive term patients into 4 groups who received either povidone-iodine or benzalkonium chloride as a skin disinfectant before delivery and one of these for postpartum vaginal lacerations. Prepartum doses were about 7 mL and postpartum doses were about 0.5 mL of solution. Infant thyrotropin levels were elevated in the infants whose mothers received topical povidone-iodine pre- and postpartum compared to infants whose mothers received no povidone-iodine. After discontinuing the use of peripartum povidone-iodine, the rate of recall of infants for abnormal thyroid function tests dropped from 4.47% to 0.74%.[4]
In Switzerland, a girl born at 29 weeks of gestation with adequate size for gestational age showed negative TSH screening on day 5. Her mother had developed an abscess of the abdominal wall 1 week after her cesarian section and was treated with povidone-iodine tampons. The baby's TSH was elevated to 23 milliunits/L on day 23, and 288 milliunits/L on day 29. Free thyroxine (T4) levels were decreased to 2.8 ng/L and free liothyronine (T3) with 1.52 ng/L, without signs or symptoms of hypothyroidism. Iodine contents of maternal milk and of infant urine were 4.4 mg/L and 3.9 mg/L, respectively. Treatment with levothyroxine was started, breastfeeding was discontinued and disinfection with povidone-iodine was stopped. The infant's thyroid function tests normalized after 6 days.[11] The infant's abnormal thyroid function tests were probably caused by maternal iodine use.
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
References
- 1.
- Fuse Y, Ogawa H, Tsukahara Y, et al. Iodine metabolism and thyroid function during the perinatal period: Maternal-neonatal correlation and effects of topical povidone-iodine skin disinfectants. Biol Trace Elem Res. 2022;201:2685–700. [PubMed: 35931927]
- 2.
- Chanoine JP, Bourdoux P, Pardou A, et al. Iodinated skin disinfectants in mothers at delivery and impairment of thyroid function in their breastfed infants. In, Medeiros-Neto G, Gaitan E, eds Frontiers in thyroidology, vol 2 New York: Plenum Press 1986:1055-60.
- 3.
- Arena Ansotegui J, Emparanza Knorr JI. An Esp Pediatr. 1989;30:23–6. San Millan, Vege, MJ, et al[Iodine overload in newborn infants caused by the use of PVP-iodine for perineal preparation of the mother in vaginal delivery] [PubMed: 2648916]
- 4.
- Koga Y, Sano H, Kikukawa Y, et al. Affect on neonatal thyroid function of povidone-iodine used on mothers during perinatal period. J Obstet Gynaecol (Tokyo 1995) 1995;21:581-5.
- 5.
- Postellon DC, Aronow R. Iodine in mother's milk. JAMA. 1982;247:463. [Letter]
- 6.
- Delange F, Chanoine JP, Abrassart C, et al. Topical iodine, breastfeeding, and neonatal hypothyroidism. Arch Dis Child. 1988;63:106–7. [Letter]
- 7.
- Danziger Y, Pertzelan A, Mimouni M. Transient congenital hypothyroidism after topical iodine in pregnancy and lactation. Arch Dis Child. 1987;62:295–6. [PMC free article: PMC1778303] [PubMed: 3566323]
- 8.
- Chanoine JP, Boulvain M, Bourdoux P, et al. Increased recall rate at screening for congenital hypothyroidism in breast fed infants born to iodine overloaded mothers. Arch Dis Child. 1988;63:1207–10. [PMC free article: PMC1779012] [PubMed: 3196047]
- 9.
- Chanoine JP, Pardou A, Bourdoux P, et al. Withdrawal of iodinated disinfectants at delivery decreases the recall rate at neonatal screening for congenital hypothyroidism. Arch Dis Child. 1988;63:1297–8. [Letter] [PMC free article: PMC1779024] [PubMed: 3196066]
- 10.
- Rakover Y, Adar H. Harefuah. 1989;116:527–9. [Thyroid function disturbances in an infant following maternal topical use of Polydine] [PubMed: 2792927]
- 11.
- Casteels K, Punt S, Bramswig J. Transient neonatal hypothyroidism during breastfeeding after post-natal maternal topical iodine treatment. Eur J Pediatr. 2000;159:716–7. [PubMed: 11014479]
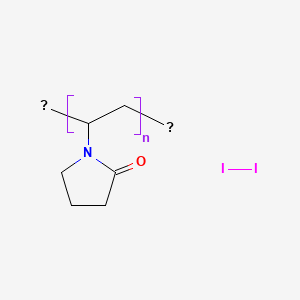
Substance Identification
Substance Name
Povidone-Iodine
CAS Registry Number
25655-41-8
Drug Class
Breast Feeding
Milk, Human
Anti-Infective Agents, Local
Antibacterial Agents
Iodophors
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Iodine.[Drugs and Lactation Database (...]Review Iodine.. Drugs and Lactation Database (LactMed®). 2006
- Iodine Metabolism and Thyroid Function During the Perinatal Period: Maternal-Neonatal Correlation and Effects of Topical Povidone-Iodine Skin Disinfectants.[Biol Trace Elem Res. 2023]Iodine Metabolism and Thyroid Function During the Perinatal Period: Maternal-Neonatal Correlation and Effects of Topical Povidone-Iodine Skin Disinfectants.Fuse Y, Ogawa H, Tsukahara Y, Fuse Y, Ito Y, Shishiba Y, Irie M. Biol Trace Elem Res. 2023 Jun; 201(6):2685-2700. Epub 2022 Aug 6.
- [Relevance of an iodine allergy to commercial polyvidone-iodine preparations].[Z Hautkr. 1983][Relevance of an iodine allergy to commercial polyvidone-iodine preparations].Kunze J, Kaiser HJ, Petres J. Z Hautkr. 1983 Feb 15; 58(4):255-61.
- The effect of type of delivery and povidone-iodine application at delivery on cord dried-blood-specimen thyrotropin level and the rate of hyperthyrotropinemia in mature and normal-birth-weight neonates residing in an iodine-replete area: report of Tehran Province, 1998-2005.[Thyroid. 2007]The effect of type of delivery and povidone-iodine application at delivery on cord dried-blood-specimen thyrotropin level and the rate of hyperthyrotropinemia in mature and normal-birth-weight neonates residing in an iodine-replete area: report of Tehran Province, 1998-2005.Ordookhani A, Pearce EN, Mirmiran P, Azizi F, Braverman LE. Thyroid. 2007 Nov; 17(11):1097-102.
- Review [Iodine overload in newborn infants caused by the use of PVP-iodine for perineal preparation of the mother in vaginal delivery].[An Esp Pediatr. 1989]Review [Iodine overload in newborn infants caused by the use of PVP-iodine for perineal preparation of the mother in vaginal delivery].Arena Ansotegui J, Emparanza Knörr JI, San Millán Vege MJ, Garrido Chércoles A, Eguileor Gurtubai I. An Esp Pediatr. 1989 Jan; 30(1):23-6.
- Povidone-Iodine - Drugs and Lactation Database (LactMed®)Povidone-Iodine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
