Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 57-83-0
Drug Levels and Effects
Summary of Use during Lactation
Because of the low reported levels of progesterone in breastmilk, even with the high-dose products, amounts ingested by the infant are small and would not be expected to cause any adverse effects in breastfed infants. The progesterone vaginal ring available in some countries produces maternal blood levels that are lower than those of ovulating women.[1] Most studies indicate that progesterone is not detrimental to milk production or duration of nursing.[2,3] No special precautions appear to be required.
In Russia, a progesterone gel (Progestogel - Besins Healthcare; not available in the US) has been used topically as a one-time application to the breasts to treat postpartum breast engorgement when more conservative measures have failed.[4] A subsequent study failed to detect any decrease in breast hardness 20 minutes after application of progesterone gel in mothers with engorgement.[5] The safety and efficacy of this use have not been well studied and the manufacturer of Progestogel recommends avoiding its use during lactation.
Drug Levels
Maternal Levels. Women who received 6 subdermal implants containing 100 mg each of progesterone between days 30 to 35 postpartum for contraception had milk progesterone levels measured. Milk progesterone levels were 5.7 mcg/L in 6 women at 3 to 4 months postpartum and 6.3 mcg/L in 7 women at 9 to 12 months postpartum. By comparison, 9 women who received a Copper T intrauterine device had negligible progesterone levels. The authors estimated that infants would receive about 5 mcg of progesterone daily through breastmilk.[6,7]
Infant Levels. Women received 6 subdermal implants containing 100 mg each of progesterone between days 30 to 35 postpartum for contraception. A metabolite of progesterone, pregnane-3-glucuronide, was measured in the urine of their infants. At 3 to 4 months (n = 9) and 9 to 12 months (n = 7) postpartum, urine metabolite levels were 6.3 mcg/L and 15.7 mcg/L, respectively. These values were not significantly different from those of infants whose mothers were using a Copper T intrauterine device.[6,7]
Effects in Breastfed Infants
Eighty-four women had 6 subdermal implants containing 100 mg each of progesterone inserted between days 30 to 35 postpartum as a contraceptive. Compared to women who received either a placebo or a Copper T intrauterine device, there were no differences in the growth rates of their infants over the first 6 months postpartum.[8]
One hundred ninety-two mothers who received 6 subdermal implants containing 100 mg each of progesterone inserted on postpartum day 60 as a contraceptive. The weight gain of 60 infants who were exclusively breastfed for 6 months was compared to that of infants whose mothers received either placebo (n = 68 at day 30) or a Copper T (n = 64 at day 30 and n = 49 at day 60) intrauterine device. No differences were found in the average weight gains among the 3 groups of infants at 6 months of age.[9]
Vaginal rings that released progesterone were inserted at about 60 days postpartum in 128 women. The 2 types of rings released progesterone either 7.5 mg daily decreasing to 4.5 mg at 90 days or 15 mg daily decreasing to 7 mg daily at 90 days. Over the first 12 months postpartum, no differences in weight gain were found between the exclusively breastfed infants of mothers who received the progesterone rings and control mothers who received a Copper T intrauterine device for contraception.[10]
One hundred twenty breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone for 90 days, starting during weeks 5 to 7 postpartum. No differences were found in the growth of breastfed infants or in developmental milestones compared to the normal population values.[11]
One hundred eighty-seven breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone, starting at about day 57 postpartum. No differences were found in weight gain during the first 6 months of use compared to infants whose mothers received either a Copper T intrauterine device, an oral progestin-only contraceptive or levonorgestrel implant.[12]
A study comparing 100 women who received vaginal ring that released about 10 mg daily of progesterone to those who received a Copper T intrauterine device between days 29 and 64 postpartum found no differences in weight gain of their breastfed infants over the first year postpartum.[13]
Two hundred eighty-five women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 262 women who received a Copper T intrauterine device beginning between weeks 5 and 9 postpartum. No differences in the weight gain of breastfed infants were seen between the 2 groups during the 14-month observation period.[14]
A study comparing progesterone ring (n = 459) to the copper-T IUD (n = 330) in postpartum women found no adverse effects on infant breastfeeding or growth.[15]
Effects on Lactation and Breastmilk
Eighty-four women had 6 subdermal implants containing 100 mg each of progesterone inserted between days 30 to 35 postpartum as a contraceptive. Compared to women who received either a placebo or a Copper T intrauterine device, no difference was found in the breastfeeding rates during the first 9 months postpartum. At 1 year postpartum, more women in the Copper T group were breastfeeding than in the progesterone or placebo groups.[8]
Vaginal rings that released progesterone were inserted at about 60 days postpartum in 246 women. The 3 types of rings released progesterone either 5, 10 or 15 mg daily. Control women received a Copper T intrauterine device. At 6 and 12 months postpartum there was no significant difference in the percentage of infants who were breastfed between the progesterone and Copper T groups.[16]
One hundred twenty breastfeeding women used a vaginal ring that released about 10 mg daily of progesterone, starting during weeks 5 to 7 postpartum. The rate of weaning was greater in the progesterone ring group than in groups of women who received levonorgestrel or norethindrone implants for postpartum contraception.[11]
In a multicenter study, 802 women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 734 women who received a Copper T intrauterine device beginning at day 29 to 63 postpartum. No differences were found in the rate of breastfeeding between the 2 groups over the first year postpartum.[17]
Two hundred eighty-five women who received a vaginal ring that released about 10 mg daily of progesterone were compared to 262 women who received a Copper T intrauterine device beginning between weeks 5 and 9 postpartum. No differences in the breastfeeding rates were seen between the 2 groups during the 14-month observation period.[14]
An observational study followed 192 women who used a vaginal ring that released 10 mg of progesterone daily beginning between days 54 and 64 postpartum. All subjects used the vaginal ring for at least 4 months; 90% were still using it at 6 months and 73% were using it at 9 months postpartum. The duration of breastfeeding and infant growth were similar to reference groups.[18]
A double-blind placebo-controlled trial randomized 46 postpartum women who were abstinent former smokers to oral micronized progesterone 200 mg twice a day or placebo for 4 weeks to assess smoking abstinence rates. Entry into the study occurred only after breastfeeding was well established. No statistical difference was found in the number of days of breastfeeding between the groups.[19]
A study comparing progesterone ring (n = 459) to the copper-T IUD (n = 330) in postpartum women found that lactation amenorrhea lasted longer (405 days) with the progesterone ring than with the IUD (120 days).[15]
A transgender woman took and spironolactone 50 mg twice daily to suppress testosterone, domperidone 10 mg three times daily, increasing to 20 mg four times daily, oral micronized progesterone 200 mg daily and oral estradiol to 8 mg daily and pumped her breasts 6 times daily to induce lactation. After 3 months of treatment, estradiol regimen was changed to a 0.025 mg daily patch and the progesterone dose was lowered to 100 mg daily. Two weeks later, she began exclusively breastfeeding the newborn of her partner. Breastfeeding was exclusive for 6 weeks, during which the infant's growth, development and bowel habits were normal. The patient continued to partially breastfeed the infant for at least 6 months.[20]
A transgender woman was taking spironolactone 100 mg twice daily, progesterone 200 mg daily and estradiol 5 mg daily. She was started on domperidone 10 mg three times daily to increase milk supply. She was able to pump 3 to 5 ounces of milk daily by one month after starting. The dose of domperidone was increased to 30 mg three times daily after 8 weeks because of a decreased milk supply. Her milk supply returned to 3 to 5 ounces of milk daily. By 6 months, her milk supply had decreased to about 5 mL daily, even though her serum prolactin was still elevated.[21]
A transgender woman had been taking estradiol 2 mg twice daily for 14 years. She began taking domperidone 10 mg four times daily and progesterone 100 mg daily 107 days prior to her partner’s due date. At the same time, the estradiol dosage was increased to 4 mg twice daily. At 94 days prior to the due date, the domperidone dosage was increased to 20 mg four times daily, the progesterone dose was increased to 200 mg daily and estrogen was changed to transdermal estradiol 25 mcg daily. Progesterone was discontinued 34 days prior to the due date. She pumped and stored milk beginning at 34 days prior to the due date and by 27 days postpartum, she was breastfeeding the infant twice daily, expressing 150 mL of milk daily and was able to decrease the domperidone dosage to 20 mg three times daily. Lower dosages reduced milk supply.[22]
A transgender woman was taking sublingual estradiol 4 mg twice daily, spironolactone 100 mg twice daily and progesterone 200 mg at bedtime for gender-affirming therapy. In order to prepare for the birth of the infant being carried by her partner, sublingual estradiol was increased to 6 mg twice daily and progesterone was increased to 400 mg at bedtime. Domperidone 10 mg twice daily was also started to increase serum prolactin levels and later increased to 20 mg 4 times daily. Before the delivery date, progesterone was stopped, spironolactone was decreased to 100 mg daily and estradiol was changed to 25 mcg per day transdermally. At day 59 postpartum, estradiol was changed to 2 mg per day sublingually and spironolactone was increased to 100 mg twice daily. The patient was able to produce up to 240 mL of milk daily containing typical macronutrient and oligosaccharide levels.[23]
A transgender woman who wished to breastfeed was given estradiol transdermal patch 150 mcg daily and progesterone 100 mg daily by mouth. Later estradiol spray 100 mcg and domperidone 10 mg 4 times daily were added. Domperidone dosage was then doubled to 20 mg 4 times daily and progesterone was doubled to 100 mg twice daily. After further adjustment of estradiol and progesterone dosages, 7 mL of milk was produced with pumping, but 2 weeks after the infant’s birth, lactation induction was discontinued at the patient’s request.[24]
A 50-year-old transgender woman wished to breastfeed her grandchild was taking baseline treatment with estradiol 0.3 mg transdermal patch every 72 hours and micronized progesterone 200 mg oral once daily. To initiate lactation, her estradiol dose was increased to a 0.4 mg transdermal patch every 72 hours and nipple stimulation was initiated. Later the patient’s progesterone was increased to 300 mg daily and metoclopramide oral 10 mg three times daily was initiated. She lactated for a total of two weeks and nursed the four-month-old infant on multiple occasions. Her peak milk production was 30 mL from her larger right breast, and 8 mL from her smaller left breast.[25]
Alternate Drugs to Consider
(Contraception) Etonogestrel, Intrauterine Copper Contraceptive, Levonorgestrel Implant, Intrauterine Levonorgestrel, Medroxyprogesterone Acetate
References
- 1.
- RamaRao S, Clark H, Merkatz R, et al. Progesterone vaginal ring: Introducing a contraceptive to meet the needs of breastfeeding women. Contraception 2013;88:591-8. [PubMed: 23769015]
- 2.
- Carr SL, Gaffield ME, Dragoman MV, Phillips S. Safety of the progesterone-releasing vaginal ring (PVR) among lactating women: A systematic review. Contraception 2016;94:253-61. [PubMed: 25869631]
- 3.
- Phillips SJ, Tepper NK, Kapp N, et al. Progestogen-only contraceptive use among breastfeeding women: A systematic review. Contraception 2016;94:226-52. [PubMed: 26410174]
- 4.
- Pustotina O. Management of mastitis and breast engorgement in breastfeeding women. J Matern Fetal Neonatal Med 2016;29:3121-5. [PubMed: 26513602]
- 5.
- Alekseev NP. Progesterone-containing gel does not eliminate postpartum breast engorgement? Breastfeed Med 2017;12:122-3. [PubMed: 28170298]
- 6.
- Croxatto HB, Díaz S. The place of progesterone in human contraception. J Steroid Biochem 1987;27:991-4. [PubMed: 3320572]
- 7.
- Croxatto HB, Díaz S, Peralta O, et al. Subdermal progesterone implants for fertility regulation in nursing women. In, Zatuchni GI, Goldsmith A, Shelton JD, Sciara JJ, eds Long-acting contraceptive delivery systems Philadelphia Harper & Row 1984.
- 8.
- Croxatto HB, Díaz S, Peralta O, et al. Fertility regulation in nursing women. II. Comparative performance of progesterone implants versus placebo and copper T. Am J Obstet Gynecol 1982;144:201-8. [PubMed: 7114130]
- 9.
- Díaz S, Peralta O, Juez G, et al. Fertility regulation in nursing women. VI. Contraceptive effectiveness of a subdermal progesterone implant. Contraception 1984;30:311-25. [PubMed: 6509984]
- 10.
- Díaz S, Jackanicz TM, Herreros C, et al. Fertility regulation in nursing women: VIII. Progesterone plasma levels and contraceptive efficacy of a progesterone-releasing vaginal ring. Contraception 1985;32:603-22. [PubMed: 3912105]
- 11.
- Shaaban MM. Contraception with progestogens and progesterone during lactation. J Steroid Biochem Mol Biol 1991;40:705-10. [PubMed: 1835650]
- 12.
- Díaz S, Zepeda A, Maturana X, et al. Fertility regulation in nursing women IX. Contraceptive performance, duration of lactation, infant gowth, and bleeding patterns during use of progesterone vaginal rings, progestin-only pills, Norplant® implants, and Copper T 380-A intrauterine devices. Contraception 1997;56:223-32. [PubMed: 9408703]
- 13.
- Chen JH, Wu SC, Shao WQ, et al. The comparative trial of TCu 380A IUD and progesterone-releasing vaginal ring used by lactating women. Contraception 1998;57:371-9. [PubMed: 9693396]
- 14.
- Massai R, Miranda P, Valdés P, et al. Preregistration study on the safety and contraceptive efficacy of a progesterone-releasing vaginal ring in Chilean nursing women. Contraception 1999;60:9-14. [PubMed: 10549447]
- 15.
- Roy M, Hazra A, Merkatz R, et al. Progesterone vaginal ring as a new contraceptive option for lactating mothers: Evidence from a multicenter non-randomized comparative clinical trial in India. Contraception 2020;102:159-67. [PMC free article: PMC7483628] [PubMed: 32360666]
- 16.
- Croxatto HB, Díaz S. Progesterone vaginal rings for contraception during breastfeeding. In, Runnebaum R, Rabe T, Kiesel L, eds Advances in gynecological and obstetric research series Vol 2 Female contraception and male fertility regulation New Jersey Parthenon 1987;2:135-42.
- 17.
- Sivin I, Díaz S, Croxatto HB, et al. Contraceptives for lactating women: A comparative trial of a progesterone-releasing vaginal ring and the copper T 380A IUD. Contraception 1997;55:225-32. [PubMed: 9179454]
- 18.
- Massai R, Quinteros E, Reyes MV, et al. Extended use of a progesterone-releasing vaginal ring in nursing women: A phase II clinical trial. Contraception 2005;72:352-7. [PubMed: 16246661]
- 19.
- Allen SS, Allen AM, Lunos S, Tosun N. Progesterone and postpartum smoking relapse: A pilot double-blind placebo-controlled randomized trial. Nicotine Tob Res 2016;18:2145-53. [PMC free article: PMC5055745] [PubMed: 27613934]
- 20.
- Reisman T, Goldstein Z. Case report: Induced lactation in a transgender woman. Transgend Health 2018;3:24-6. [PMC free article: PMC5779241] [PubMed: 29372185]
- 21.
- Wamboldt R, Shuster S, Sidhu BS. Lactation induction in a transgender woman wanting to breastfeed: Case report. J Clin Endocrinol Metab 2021;106:e2047-e2052. [PubMed: 33513241]
- 22.
- Weimer AK. Lactation induction in a transgender woman: Macronutrient analysis and patient perspectives. J Hum Lact 2023;39:488-94. [PubMed: 37138506]
- 23.
- Delgado D, Stellwagen L, McCune S, et al. Experience of induced lactation in a transgender woman: Analysis of human milk and a suggested protocol. Breastfeed Med 2023;18:888-93. [PubMed: 37910800]
- 24.
- van Amesfoort JE, Van Mello NM, van Genugten R. Lactation induction in a transgender woman: Case report and recommendations for clinical practice. Int Breastfeed J 2024;19:18. [PMC free article: PMC10926588] [PubMed: 38462609]
- 25.
- Trahair ED, Kokosa S, Weinhold A, et al. Novel lactation induction protocol for a transgender woman wishing to breastfeed: A case report. Breastfeed Med 2024. [PubMed: 38535753]
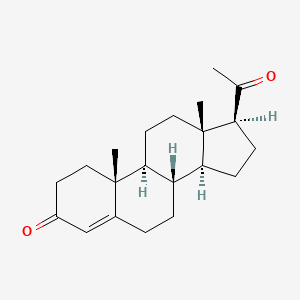
Substance Identification
Substance Name
Progesterone
CAS Registry Number
57-83-0
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Medroxyprogesterone Acetate.[Drugs and Lactation Database (...]Review Medroxyprogesterone Acetate.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydrocortisone.[Drugs and Lactation Database (...]Review Hydrocortisone.. Drugs and Lactation Database (LactMed®). 2006
- Review Norethindrone.[Drugs and Lactation Database (...]Review Norethindrone.. Drugs and Lactation Database (LactMed®). 2006
- Review Methylprednisolone.[Drugs and Lactation Database (...]Review Methylprednisolone.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydrocortisone, Topical.[Drugs and Lactation Database (...]Review Hydrocortisone, Topical.. Drugs and Lactation Database (LactMed®). 2006
- Progesterone - Drugs and Lactation Database (LactMed®)Progesterone - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
