Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 298-46-4
Drug Levels and Effects
Summary of Use during Lactation
Breastfeeding during carbamazepine monotherapy does not appear to adversely affect infant growth or development, and breastfed infants had higher IQs and enhanced verbal abilities than nonbreastfed infants at 6 years of age in one study.[1] A safety scoring system finds carbamazepine possible to use during breastfeeding.[2] If carbamazepine is required by the mother, it is not a reason to discontinue breastfeeding.
Carbamazepine and its active metabolite have relatively high levels in breastmilk and breastfed infants have serum levels that are sometimes measurable, but usually well below the anticonvulsant therapeutic range. Most infants have had no adverse reactions, but sedation, poor sucking, withdrawal reactions and 3 cases of hepatic dysfunction have been reported. These have all been complicated because of intrauterine exposure and, in some cases, concurrent drug therapy. Monitor the infant for jaundice, drowsiness, adequate weight gain, and developmental milestones, especially in younger, exclusively breastfed infants and when using combinations of anticonvulsant or psychotropic drugs. One author recommends monitoring infant serum carbamazepine levels, liver enzymes, and a complete blood count during therapy.[3]
Drug Levels
In published reports of anticonvulsant use during breastfeeding, most women were taking a combination of anticonvulsants. Some other anticonvulsants (e.g., phenytoin, carbamazepine) stimulate the metabolism of other drugs including anticonvulsants, whereas others (e.g., valproic acid) inhibit the metabolism of other drugs. Therefore, the relationship of the maternal dosage to the concentration in breastmilk can be quite variable, making calculation of the weight-adjusted percentage of maternal dosage less meaningful than for other drugs in this database.
Maternal Levels. Three women taking carbamazepine and phenytoin for epilepsy had carbamazepine and its epoxide metabolite measured in breastmilk. One woman receiving 6 mg/kg daily had carbamazepine milk levels of 1.8, 1.3 and 1.8 mg/L and epoxide metabolite levels of 0.7, 0.5 and 1.1 mg/L on days 2, 3 and 30 postpartum, respectively. A second woman taking carbamazepine 5.8 mg/kg daily had milk carbamazepine levels of 1.5 and 1.8 mg/L and epoxide metabolite levels of 0.7 and 0.9 mg/L at 3 and 5 weeks postpartum, respectively. The third woman taking carbamazepine 7.3 mg/kg daily had a carbamazepine milk level of 1.5 mg/L and epoxide metabolite level of 0.5 mg/L at 3 weeks postpartum.[4,5]
Three carbamazepine breastmilk levels were measured between days 3 and 32 postpartum at unstated times after the dose in an unstated number of women who were taking carbamazepine and other anticonvulsants in unstated dosages. Carbamazepine milk levels averaged 1.9 mg/L (range 0.8 to 3.8 mg/L), while maternal serum levels averaged 4.3 mg/L.[6]
An epileptic woman was taking carbamazepine 1 gram daily and primidone 1 gram daily during pregnancy and postpartum. At 5 weeks postpartum, a milk sample was measured. The milk fat contained 1.4 mg/L while the skimmed portion contained 2.3 mg/L of carbamazepine.[7]
Four mothers taking carbamazepine monotherapy in an average dosage of 10.95 mg/kg daily had average milk levels of 1.78 mg/L at various times during the first month postpartum. Carbamazepine epoxide milk levels measured in 3 of the women averaged 0.39 mg/L.[8]
Sixteen women taking carbamazepine alone or with other anticonvulsants had breastmilk levels measured, 14 during the first week postpartum, 1 at 24 days and 1 at 35 days postpartum. Their average dosage was 13.8 mg/kg daily. Milk carbamazepine levels averaged 2.5 mg/L. Carbamazepine epoxide was measured in the milk of 6 of the women and averaged 1.5 mg/L. In 9 of the women, milk carbamazepine levels were measured on more than 1 occasion; no marked interday differences were found.[9]
Six women taking carbamazepine at an average dosage of 733 mg daily (range 600 to 1000 mg daily) had an average breastmilk carbamazepine level of 2.4 mg/L (range 1.2 to 3.4 mg/L) during the first week postpartum. Milk levels averaged 50% (range 32 to 80%) of maternal serum levels.[10]
One mother taking carbamazepine 200 mg twice daily had breastmilk carbamazepine levels of 2.8 and 2.2 mg/L at 2 and 63 days postpartum.[11]
A woman was taking carbamazepine 300 mg twice daily plus fluoxetine and buspirone for bipolar disorder. Her breastmilk carbamazepine levels were unmeasurable (<0.5 mg/L) on day 13 postpartum and 0.5 mg/L on day 21 postpartum.[12]
Breastmilk levels of carbamazepine and its metabolite were measured in one milk sample taken 8 hours after a dose of 200 mg of carbamazepine. The carbamazepine concentration was 2.3 mg/L and the carbamazepine epoxide concentration was 1.5 mg/L.[13]
Seven women taking an average of 520 mg (range 250 to 800 mg daily) of carbamazepine daily had breastmilk levels measured on 1 or more occasions during the first 34 days postpartum, although all but 2 levels were taken during the first 5 days. The average milk levels of carbamazepine and its epoxide metabolite were 3.5 and 1.3 mg/L, respectively. Milk levels of the drug and metabolite were 64% and 79% of simultaneous maternal levels.[14]
Sixty-one women taking carbamazepine had measurements of carbamazepine taken between day 6 and 29 postpartum (median 7 days) for routine monitoring. Sixty had serum and breastmilk analyzed and one had only milk analyzed; 58 also had carbamazepine epoxide measured. Milk carbamazepine levels ranged from 0.5 to 6.7 mg/L (mean 2.1 mg/L); milk carbamazepine epoxide levels ranged 0.3 to 3.7 mg/L (median 0.5 mg/L). Only 7% of the milk carbamazepine levels were in the therapeutic range used for treating epilepsy. Concomitant valproic acid use by mothers increased carbamazepine epoxide levels in maternal serum and milk.[15]
A nursing mother was taking carbamazepine 600 mg twice daily at 8 am and 8 pm in late pregnancy and postpartum. Breastmilk concentrations were measured on one day at 8 am, 11 am and 2 pm. Milk levels were 3.5, 4.4 and 3.1 mg/L, respectively.[16]
Infant Levels. An infant whose mother was taking carbamazepine 6 mg/kg daily during pregnancy and postpartum had carbamazepine serum levels of 1.1, 1.3 and 1.8 mg/L days 2, 3 and 30 of age, respectively. The epoxide metabolite was only detectable on day 2 at a concentration of 0.3 mg/L. Another infant whose mother was taking carbamazepine 5.8 mg/kg daily during pregnancy and postpartum had a carbamazepine serum level of 0.5 mg/L and undetectable epoxide metabolite level at 5 weeks of age. Infant carbamazepine serum levels in these 2 infants averaged 44% of the simultaneous maternal carbamazepine serum levels.[4,5]
Three breastfed infants had steady-state serum carbamazepine levels measured during maternal therapy. The mother's dosages and corresponding infant serum levels are as follows: 10.3 mg/kg daily and 0.5 mg/L at 5 days of age; 22 mg/kg daily and 1 mg/L at 28 days of age; and, 10.6 mg/kg and 4.7 mg/L at 28 days of age. The latter mother was also taking ethosuximide and clonazepam. The epoxide metabolite was not measured.[8]
An infant whose mother was taking carbamazepine 200 mg twice daily had serum carbamazepine levels of 1.8 and 1.1 mg/L at 2 days and 63 days of age. The infant was exclusively breastfed for 9 days and partially breastfed thereafter.[11]
Total and free carbamazepine levels of 0.7 and 0.22 mg/L, respectively, were measured in a breastfed 3-month-old whose mother was taking carbamazepine 200 mg in the morning and 300 mg at bedtime (about 8 mg/kg daily). The serum sample was taken about 14 hours after the last dose. Total and free levels were 15% and 20% of the simultaneous maternal serum total and free levels.[17]
Fifty-four breastfed infants whose mothers were taking carbamazepine had serum samples taken between 6 and 10 days postpartum. Maternal serum carbamazepine levels varied from 1.4 to 9.0 mg/L and serum carbamazepine epoxide levels ranged from 0.1 to 5.4 mg/L. Infant serum carbamazepine levels ranged between 0 and 2.6 mg/L. In 31 infants who also had serum carbamazepine epoxide measured, levels ranged from 0.0 to 0.6 mg/L. The infant/maternal serum concentration ratio ranged from 0 to 0.7 and the epoxide ratio ranged from 0 to 3. No correlation between maternal serum and infant serum was found. Maternal co-administration of enzyme-inducers decreased the value of the carbamazepine infant/maternal serum concentration ratio.[18]
An exclusively breastfed newborn infant was receiving milk from a mother receiving carbamazepine 600 mg every 12 hours with breastmilk carbamazepine levels ranging from 3.1 to 4.4 mg/L during a dosage interval. The infant's serum carbamazepine level measured at the time of the mother's morning dose was 1.3 mg/L. The baby had symptoms of gastroesophageal reflux until breastfeeding was discontinued.[16]
In a multicenter study of nursing mother-infant pairs, 11 infants had blood samples taken at about the same time as maternal blood samples. All of the infants had blood levels of carbamazepine below the lower limit of quantification (0.7 mg/L) and only one had a blood level of carbamazepine 10,11-epoxide greater than the lower limit of quantification (0.1 mg/L). The authors estimated the average infant carbamazepine serum concentration to be 0.35 mg/L, assuming unquantifiable serum concentrations to be 50% of the lower limit of quantification. Median infant blood levels of carbamazepine were 5.7% (range 3.7 to 8.4%) and median carbamazepine epoxide infant blood levels were 5.4% (range 0.9 to 9.6%) of their mothers’ blood levels.[19]
Sixty-three infants whose mothers were taking carbamazepine had serum measurements of carbamazepine taken between day 6 and 29 postpartum (median 7 days) for routine monitoring. Forty-nine infants had paired maternal serum levels. Fifty-eight also had carbamazepine epoxide measured. Infant serum carbamazepine levels ranged from 0.5 to 2.6 mg/L (median 0.5 mg/L); carbamazepine epoxide levels ranged 0.3 to 0.6 mg/L (median 0.3 mg/L). No significant correlations were noted between infant serum and maternal serum carbamazepine levels, daily maternal dosage or weight-adjusted dosage. Infant serum levels were below the lower limit of the therapeutic range for epilepsy (4 mg/L), and 65% of infants had values less than the lower limit of quantification (1 mg/L). Ninety-one percent of infant serum carbamazepine epoxide levels were less than the lower limit of quantification (0.5 mg/L).[15]
Effects in Breastfed Infants
No adverse effects were noted by the mothers in 3 breastfed infants during maternal carbamazepine and phenytoin therapy.[5]
An epileptic woman taking carbamazepine 1 gram and primidone 1 gram daily during pregnancy and postpartum breastfed her infant for 5 weeks and noted no difference in activity in the infant before and after nursing.[7]
A probable case of drug-induced drowsiness occurred in a newborn whose mother was taking primidone, carbamazepine and phenytoin (dosages not stated). At day 30, breastfeeding was discontinued because of the drowsiness that occurred after each feeding and poor weight gain. The same group of researchers found that 15 partially breastfed infants whose mothers were taking various anticonvulsants, including carbamazepine, gained weight at a slower rate during the first 5 days postpartum than did 75 infants of epileptic mothers who bottle fed or control mothers taking no medications.[20]
A 10-week-old breastfed infant whose mother was taking clemastine, phenytoin and carbamazepine was drowsy, refused to feed, was irritable, and had high-pitched crying.[21] These side effects were possibly caused by clemastine in breastmilk, but carbamazepine could also have contributed.
Poor sucking, vomiting and lack of weight gain was reported in a partially breastfed 4-week-old whose mother was taking carbamazepine monotherapy in a dose of 11 mg/kg daily.[8]
Weak sucking occurred in 1 of 15 breastfed infants whose mothers were on carbamazepine monotherapy, but a causal relationship could not be confirmed.[9]
A breastfed infant whose mother was taking primidone 375 mg, phenobarbital 90 mg, and carbamazepine 800 mg daily did well despite a saliva phenobarbital level of 3.4 mg/L. At 7 months of age, after the mother abruptly stop nursing, the infant had a number of "startle reactions" and infantile seizures occurred which were confirmed by an abnormal electroencephalogram. Continued phenobarbital administration to the infant for 15 months controlled the seizures and no more occurred up to 5 years of age.[22]
A 3-week-old infant whose mother was taking carbamazepine monotherapy 600 mg daily during pregnancy and postpartum had persistent jaundice from birth. Cholestasis and elevated hepatic transaminases were found. Jaundice slowly resolved after discontinuation of breastfeeding on day 17 of life, but transaminase values increased to a peak 6.5 weeks after discontinuation of breastfeeding. Cholestatic hepatitis was possibly caused by carbamazepine exposure in utero and in breastmilk.[23]
An infant was born to a mother who was taking carbamazepine monotherapy 400 mg daily during pregnancy and postpartum. The infant was exclusively breastfed for 9 days, then partially breastfed. Jaundice was present at birth and serum gamma-glutamyltransferase (GGT) levels were elevated and remained elevated for at least 25 days, even after bilirubin levels decreased. The infant had a rare form of ABO incompatibility, but this was not thought to fully explain the elevated GGT levels. At 2, 4 and 6 months of age, the infant was developing normally. Serum carbamazepine levels were 1.8 and 1.1 mg/L at 2 days and 63 days of age. The transient hepatic dysfunction was possibly caused by carbamazepine exposure in utero and in breastmilk.[11]
In a telephone follow-up study, mothers reported no side effects among 6 infants exposed to carbamazepine (ages and dosages not stated) in breastmilk.[24]
One author reported a mother who was taking clonazepam 6 mg daily and carbamazepine 1400 mg daily. The infant had serum clonazepam levels of about 40% of the mother's serum level. Her infant was described as "somewhat lazy at the breast and tired." Carbamazepine levels were not reported.[25]
Possible drug-induced seizure-like activity and cyanosis occurred in a breastfed 3-week-old whose mother was taking fluoxetine, carbamazepine and buspirone during pregnancy and postpartum.[12]
A breastfed 3-month-old whose mother was taking carbamazepine 200 mg in the morning and 300 mg at bedtime had normal liver function tests.[17]
A fullterm infant whose mother was taking carbamazepine 400 mg daily during pregnancy and postpartum developed asphyxia at birth and required mechanical ventilation. Transient jaundice and liver enzyme elevation were attributed to asphyxia. The mother began breastfeeding on day 8 postpartum. At 3 to 7 weeks of age, cholestasis, jaundice and elevation of hepatic transaminases occurred. The late hepatic abnormalities were considered to be probably caused by carbamazepine in breastmilk.[26]
Two infants were breastfed during maternal therapy with carbamazepine 600 and 1200 mg daily and levetiracetam. The infants appeared to remain healthy throughout the 6- to 8-week study period.[27]
In a long-term study on infants exposed to anticonvulsants during breastfeeding, no difference in average intelligence quotient at 3 years of age was found between infants who were breastfed (n = 26) a median of 6 months and those not breastfed (n = 32) when their mothers were taking carbamazepine.[25] Breastfeeding during carbamazepine monotherapy does not appear to adversely affect infant growth or development, and breastfed infants had slightly higher IQs and enhanced verbal abilities than nonbreastfed infants at 6 years of age in one study.[28] Combination therapy with sedating anticonvulsants or psychotropics may result in infant sedation or withdrawal reactions.
A prospective cohort study in Norway followed infants of mothers who took antiepileptic drugs during pregnancy and lactation and compared them to infants of mothers with untreated epilepsy and infants with fathers who took antiepileptics as control groups. Of the 223 mothers studied, 48 were taking carbamazepine monotherapy. Infants were assessed at 6, 18 and 36 months of age. Continuous breastfeeding in children of women using antiepileptic drugs was associated with no greater impaired development than those with no breastfeeding or breastfeeding for less than 6 months.[29,30]
An exclusively breastfed infant, whose mother took carbamazepine 1200 mg daily during late pregnancy and postpartum, had poor weight gain, poor sucking, and vomiting beginning at birth with normal neurological and laboratory tests. Because gastroesophageal reflux was suspected, ranitidine and food thickeners were tried, but were unsuccessful. High milk and plasma carbamazepine levels were found. Partial formula feeding did not resolve the problem, but cessation of breastfeeding resolved the symptoms rapidly. The adverse effect was probably caused by carbamazepine.[16]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date. One woman on long-term carbamazepine therapy had slight galactorrhea 3.5 years after delivery, although her serum prolactin was normal.[9] The prolactin level in a mother with established lactation may not affect her ability to breastfeed.
Alternate Drugs to Consider
(Seizure Disorder) Divalproex, Gabapentin, Lamotrigine, Oxcarbazepine, Phenytoin, Valproic Acid
References
- 1.
- Meador KJ, Baker GA, Browning N, et al. Breastfeeding in children of women taking antiepileptic drugs: Cognitive outcomes at age 6 years. JAMA Pediatr. 2014;168:729–36. [PMC free article: PMC4122685] [PubMed: 24934501]
- 2.
- Uguz F. A new safety scoring system for the use of psychotropic drugs during lactation. Am J Ther. 2021;28:e118–e26. [PubMed: 30601177]
- 3.
- Stowe ZN. The use of mood stabilizers during breastfeeding. J Clin Psychiatry. 2007;68 Suppl 9:22–8. [PubMed: 17764381]
- 4.
- Pynnönen S, Sillanpaa M. Carbamazepine and mother's milk. Lancet 1975;306:563. PMID: 51396. [PubMed: 51396]
- 5.
- Pynnönen S, Kanto J, Sillanpaa M, et al. Carbamazepine: Placental transport, tissue concentrations in foetus and newborn, and level in milk. Acta Pharmacol Toxicol (Copenh). 1977;41:244–53. [PubMed: 578653]
- 6.
- Kaneko S, Sato T, Suzuki K. The levels of anticonvulsants in breast milk. Br J Clin Pharmacol 1979;7:624-7. Letter. PMID: 465285. [PMC free article: PMC1429673] [PubMed: 465285]
- 7.
- Niebyl JR, Blake DA, Freeman JM, et al. Carbamazepine levels in pregnancy and lactation. Obstet Gynecol. 1979;53:139–40. [PubMed: 760015]
- 8.
- Kuhnz W, Jager-Roman E, Rating D, et al. Carbamazepine and carbamazepine 10,11-epoxide during pregnancy and postnatal period in epileptic mothers and their nursed infants and their effects on neonatal behavior. Pediatr Pharmacol (New York). 1983;3:199–208. [PubMed: 6677873]
- 9.
- Froescher W, Eichelbaum M, Niesen M, et al. Carbamazepine levels in breast milk. Ther Drug Monit. 1984;6:266–71. [PubMed: 6390794]
- 10.
- Meyer FP, Quednow B, Potrafki A, et al. Zentralbl Gynakol. 1988;110:1195–205. [The perinatal pharmacokinetics of anticonvulsant drugs] [PubMed: 3239295]
- 11.
- Merlob P, Mor N, Litwin A. Transient hepatic dysfunction in an infant of an epileptic mother treated with carbamazepine during pregnancy and breast feeding. Ann Pharmacother. 1992;26:1563–5. [PubMed: 1362364]
- 12.
- Brent NB, Wisner KL. Fluoxetine and carbamazepine concentrations in a nursing mother/infant pair. Clin Pediatr (Phila). 1998;37:41–4. [PubMed: 9475699]
- 13.
- Lopes BR, Barreiro JC, Baraldi PT, et al. Quantification of carbamazepine and its active metabolite by direct injection of human milk serum using liquid chromatography tandem ion trap mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci. 2012;889-890:17–23. [PubMed: 22366281]
- 14.
- Shimoyama R, Ohkubo T, Sugawara K. Monitoring of carbamazepine and carbamazepine 10,11-epoxide in breast milk and plasma by high-performance liquid chromatography. Ann Clin Biochem. 2000;37(Pt 2):210–5. [PubMed: 10735366]
- 15.
- Kacirova I, Grundmann M, Brozmanova H. Therapeutic monitoring of carbamazepine and its active metabolite during the 1st postnatal month: Influence of drug interactions. Biomed Pharmacother. 2021;137:111412. [PubMed: 33761618] [CrossRef]
- 16.
- Antonucci R, Cuzzolin L, Manconi A, et al. Maternal carbamazepine therapy and unusual adverse effects in a breastfed infant. Breastfeed Med. 2018;13:155–7. [PubMed: 29431474]
- 17.
- Wisner KL, Perel JM. Serum levels of valproate and carbamazepine in breastfeeding mother-infant pairs. J Clin Psychopharmacol. 1998;18:167–9. [PubMed: 9555601]
- 18.
- Kacirova I, Grundmann M, Brozmanova H. Therapeutic monitoring of carbamazepine concentrations in breastfeeding mothers, maternal milk and nursed infants. Ther Drug Monit. 2011;33:503. Abstract.
- 19.
- Birnbaum AK, Meador KJ, Karanam A, et al. Antiepileptic drug exposure in infants of breastfeeding mothers with epilepsy. JAMA Neurol. 2020;77:441–50. [PMC free article: PMC6990802] [PubMed: 31886825]
- 20.
- Kaneko S, Suzuki K, Sato T, et al. The problems of antiepileptic medication in the neonatal period: Is breast-feeding advisable? In, Janz D, Dam M, Richens A et al. Epilepsy, pregnancy and the child New York Raven Press 1982:343-8.
- 21.
- Kok TH, Taitz LS, Bennett MJ, et al. Drowsiness due to clemastine transmitted in breast milk. Lancet 1982;319:914-5. Letter. PMID: 6122135. [PubMed: 6122135]
- 22.
- Knott C, Reynolds F, Clayden G. Infantile spasms on weaning from breast milk containing anticonvulsants. Lancet 1987;330:272-3. Letter. PMID: 2886736. [PubMed: 2886736]
- 23.
- Frey B, Schubiger G, Musy JP. Transient cholestatic hepatitis in a neonate associated with carbamazepine exposure during pregnancy and breast-feeding. Eur J Pediatr. 1990;150:136–8. [PubMed: 2279511]
- 24.
- Ito S, Blajchman A, Stephenson M, et al. Prospective follow-up of adverse reactions in breast-fed infants exposed to maternal medication. Am J Obstet Gynecol. 1993;168:1393–9. [PubMed: 8498418]
- 25.
- Schaefer C, Peters P, Miller RK, et al. Drugs during pregnancy and lactation. Treatment options and risk assessment, 3rd ed. Boston: Academic Press. 2015:733. doi: 10.1016/B978-0-12-408078-2.00001-9. [CrossRef]
- 26.
- Frey B, Braegger CP, Ghelfi D. Neonatal cholestatic hepatitis from carbamazepine exposure during pregnancy and breast feeding. Ann Pharmacother. 2002;36:644–7. [PubMed: 11918515]
- 27.
- Johannessen SI, Helde G, Brodtkorb E. Levetiracetam concentrations in serum and in breast milk at birth and during lactation. Epilepsia. 2005;46:775–7. [PubMed: 15857447]
- 28.
- Meador KJ, Baker GA, Browning N, et al. Effects of breastfeeding in children of women taking antiepileptic drugs. Neurology. 2010;75:1954–60. [PMC free article: PMC3014232] [PubMed: 21106960]
- 29.
- Veiby G, Engelsen BA, Gilhus NE. Early child development and exposure to antiepileptic drugs prenatally and through breastfeeding: A prospective cohort study on children of women with epilepsy. JAMA Neurol. 2013;70:1367–74. [PubMed: 24061295]
- 30.
- Vajda F. Epilepsy: Effects of exposure to antiepileptic drugs during development. Nat Rev Neurol 2014;10:11-2. Editorial. PMID: 24323050. [PubMed: 24323050]
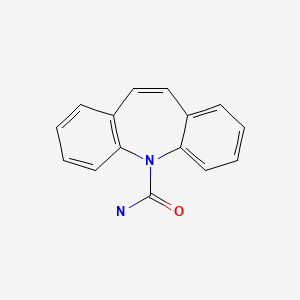
Substance Identification
Substance Name
Carbamazepine
CAS Registry Number
298-46-4
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Oxcarbazepine.[Drugs and Lactation Database (...]Review Oxcarbazepine.. Drugs and Lactation Database (LactMed®). 2006
- Review Imipramine.[Drugs and Lactation Database (...]Review Imipramine.. Drugs and Lactation Database (LactMed®). 2006
- Review Clomipramine.[Drugs and Lactation Database (...]Review Clomipramine.. Drugs and Lactation Database (LactMed®). 2006
- Review Valproic Acid.[Drugs and Lactation Database (...]Review Valproic Acid.. Drugs and Lactation Database (LactMed®). 2006
- Review Desipramine.[Drugs and Lactation Database (...]Review Desipramine.. Drugs and Lactation Database (LactMed®). 2006
- Carbamazepine - Drugs and Lactation Database (LactMed®)Carbamazepine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
