Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 42408-82-2
Drug Levels and Effects
Summary of Use during Lactation
Maternal use of oral opioids during breastfeeding can cause infant drowsiness, which may progress to rare but severe central nervous system depression. Limited data indicate that butorphanol is excreted into breastmilk in small amounts. Butorphanol is poorly orally absorbed, so it is unlikely to adversely affect the breastfed infant. Monitor the infant for drowsiness, adequate weight gain, and developmental milestones, especially in younger, exclusively breastfed infants. If butorphanol is required by the mother of a newborn, it is not a reason to discontinue breastfeeding; however, once
the mother's milk comes in, it is best to provide pain control with a nonnarcotic analgesic and limit maternal intake to 2 to 3 days with close infant monitoring. If the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness, a physician should be contacted immediately. Labor pain medication may delay the onset of lactation. Because there is no published experience with repeated, high, intravenous or intranasal doses of butorphanol during breastfeeding, other agents may be preferred in these situations, especially while nursing a newborn or preterm infant
Drug Levels
In adults, the oral bioavailability of butorphanol is 17% while the intranasal bioavailability is 70%. Butorphanol is metabolized to inactive metabolites. Intranasal and parenteral doses of 25 to 30 mcg/kg have been used in infants as young as 6 months for postoperative analgesia.
Maternal Levels. Twelve lactating women were given a single butorphanol dose at 2 to 4 days postpartum. Six of these women were given a 2 mg single intramuscular dose and 6 others were given a single 8 mg oral dose. Milk was sampled 3 times after the dose. The reported average milk levels were 1.5, 0.7 and 0.3 mcg/L at 2, 4 and 8 hours, respectively, after the 2 mg intramuscular dose. The average milk levels after the 8 mg oral dose were 3.6, 1.8 and 1.1 mcg/L at 3, 5 and 8 hours, respectively. The half-life of elimination from milk was about 2 hours.[1] Using the data from this study, doses of butorphanol 2 mg intramuscularly or 8 mg orally will result in average milk levels of 0.7 and 2 mcg/L, respectively, over 8 hours after the dose. Using these calculated average milk levels, an exclusively breastfed infant would receive 0.035 mcg/kg from a 2 mg intramuscular maternal dose of butorphanol, and 0.1 mcg/kg from an 8 mg oral maternal dose of butorphanol, from milk ingested up through 8 hours after the dose. These amounts represent 0.11% and 0.08% of the maternal weight-adjusted dosages, respectively.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Relevant published information was not found as of the revision date.
Effects on Lactation and Breastmilk
Narcotics and narcotic agonist-antagonists can increase serum prolactin.[2,3] However, the prolactin level in a mother with established lactation may not affect her ability to breastfeed.
A study compared women who received butorphanol or nalbuphine during labor (n = 26) to those who received no analgesia (n = 22). The time to effective breastfeeding was longer (46.5 minutes) in the analgesia group than in the no analgesia group (35.4 minutes).[4]
A national survey of women and their infants from late pregnancy through 12 months postpartum compared the time of lactogenesis II in mothers who did and did not receive pain medication during labor. Categories of medication were spinal or epidural only, spinal or epidural plus another medication, and other pain medication only. Women who received medications from any of the categories had about twice the risk of having delayed lactogenesis II (>72 hours) compared to women who received no labor pain medication.[5]
Alternate Drugs to Consider
Acetaminophen, Hydromorphone, Ibuprofen, Morphine, Nalbuphine
References
- 1.
- Pittman KA, Smyth RD, Losada M, et al. Human perinatal distribution of butorphanol. Am J Obstet Gynecol 1980;138:797-800. [PubMed: 7446613]
- 2.
- Tolis G, Dent R, Guyda H. Opiates, prolactin, and the dopamine receptor. J Clin Endocrinol Metab 1978;47:200-3. [PubMed: 263291]
- 3.
- Saarialho-Kere U. Psychomotor, respiratory and neuroendocrinological effects of nalbuphine and haloperidol, alone and in combination, in healthy subjects. Br J Clin Pharmacol 1988;26:79-87. [PMC free article: PMC1386503] [PubMed: 3060191]
- 4.
- Crowell MK, Hill PD, Humenick SS. Relationship between obstetric analgesia and time of effective breast feeding. J Nurse Midwifery 1994;39:150-6. [PubMed: 7931694]
- 5.
- Lind JN, Perrine CG, Li R. Relationship between use of labor pain medications and delayed onset of lactation. J Hum Lact 2014;30:167-73. [PMC free article: PMC4684175] [PubMed: 24451212]
Substance Identification
Substance Name
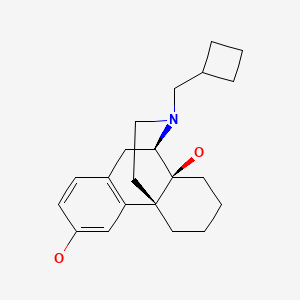
Butorphanol
CAS Registry Number
42408-82-2
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Nalbuphine.[Drugs and Lactation Database (...]Review Nalbuphine.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydromorphone.[Drugs and Lactation Database (...]Review Hydromorphone.. Drugs and Lactation Database (LactMed®). 2006
- Review Tramadol.[Drugs and Lactation Database (...]Review Tramadol.. Drugs and Lactation Database (LactMed®). 2006
- Review Oxcarbazepine.[Drugs and Lactation Database (...]Review Oxcarbazepine.. Drugs and Lactation Database (LactMed®). 2006
- Review Fentanyl.[Drugs and Lactation Database (...]Review Fentanyl.. Drugs and Lactation Database (LactMed®). 2006
- Butorphanol - Drugs and Lactation Database (LactMed®)Butorphanol - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
