Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
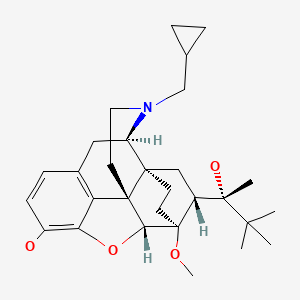
CASRN: 52485-79-7
Drug Levels and Effects
Summary of Use during Lactation
Because of the low levels of buprenorphine in breastmilk, its poor oral bioavailability in infants, and the low drug concentrations found in the serum and urine of breastfed infants, its use is acceptable in nursing mothers. Monitor the infant for drowsiness, respiratory depression, adequate weight gain, and developmental milestones, especially in younger, exclusively breastfed infants. Although unlikely, if the baby shows signs of increased sleepiness (more than usual), difficulty breastfeeding, breathing difficulties, or limpness, a physician should be contacted immediately. Observe infants for withdrawal signs if breastfeeding is stopped abruptly.
Women who received buprenorphine for opiate abuse during pregnancy and are stable should be encouraged to breastfeed their infants postpartum, unless there is another contraindication, such as use of street drugs.[1-12] The long-term outcome of infants breastfed during maternal buprenorphine therapy for opiate abuse has not been well studied.[13] The breastfeeding rate among mothers taking buprenorphine for opiate dependency may be lower than in other mothers, especially with multiple buprenorphine initiation attempts; however, among women taking buprenorphine as part of an abstinence program, the retention rate may be better in nursing mothers than in non-breastfeeding mothers.
Drug Levels
Buprenorphine has poor oral bioavailability and is usually given by the sublingual or parenteral route. Sublingual bioavailability is 30 to 40% in adults and peak levels in blood occur 60 to 90 minutes after a dose. Buprenorphine is metabolized to the slightly active metabolite, norbuprenorphine. Further metabolism is by glucuronidation to active metabolites.
Maternal Levels. A breastfeeding mother taking sublingual buprenorphine maintenance 4 mg daily during pregnancy and lactation had milk samples collected 6 times over the course of a day at 4 weeks postpartum. Milk levels and milk volumes ingested by the infant were measured, but not reported. The authors estimated that the total dose ingested by the infant over 1 day was 3.28 mcg of buprenorphine and 0.33 mcg of norbuprenorphine.[14] Assuming an infant weight of 4 kg, the infant dosage in this study is equivalent to about 1.4% of the maternal weight-adjusted dosage.
Four mothers who were 4 days postpartum and taking 0.4, 2, 4 or 6 mg of oral buprenorphine maintenance once daily during pregnancy and lactation had their milk collected 2, 4, 6 and 12 hours after a dose. Peak milk levels occurred 2 hours after the dose in the mothers taking 2 and 4 mg and 4 hours after the dose in the mother taking 6 mg daily. Peak levels were 0.8, 7.8 and 5.8 mcg/L, respectively. Milk levels of buprenorphine and norbuprenorphine were undetectable (lower limit of the assay not given) in the mother taking buprenorphine 0.4 mg daily. Average milk levels in the mothers taking 2, 4 and 6 mg were 0.4, 3.5, and 4.4 mcg/L of buprenorphine and 0.57, 0.45, and 1.15 mcg/L of norbuprenorphine, respectively.[15,16] Based on the average milk levels reported, an exclusively breastfed infant would receive less than 1% of the maternal weight-adjusted dosage. Dosages were on the low end of the usual dosage range for treatment of opiate withdrawal. Furthermore, the authors reported that the mothers' doses were given orally. The oral route is known to have poor bioavailability. The combination of low dose and oral route may have contributed to the low milk levels.
One woman who was receiving daily sublingual buprenorphine (dosage not stated) for narcotic abstinence had milk levels of 520, 720 and 230 ng/L on days 3, 6 and 9 postpartum (times of samples not stated).[17]
One woman who was 8 days postpartum had been receiving buprenorphine 8 mg sublingually for narcotic abstinence for 7 months. Ten random milk samples were collected over 4 days. The highest milk levels of buprenorphine and norbuprenorphine were 14.7 and 6.3 mcg/L.[18] Using the peak milk level data, the estimated maximum intake of an exclusively breastfed infant would be 2.4% of the maternal weight-adjusted dosage of buprenorphine and norbuprenorphine, but not including the contribution of any glucuronide metabolite.
Six women receiving a median daily dose of 0.29 mg/kg of buprenorphine sublingually for opiate abstinence were studied during the first 5 to 8 days postpartum. Hindmilk samples were obtained 6 to 8 times over a 24-hour period. Breastmilk contained estimated median infant doses of 0.42 mcg/kg of buprenorphine and 0.33 mcg/kg of norbuprenorphine daily, which are equivalent to 0.2% and 0.12% of the maternal weight-adjusted dosage. The range of buprenorphine plus norbuprenorphine was 0.18% to 0.77% of the maternal weight-adjusted dosage. Milk from the nursing mother of a 9-month-old infant receiving 0.32 mg/kg of buprenorphine had concentrations of the drug and metabolite similar to those of the other women.[19]
Seven infants who averaged 1.12 months postpartum (range 0.58 to 1.85 months) and taking buprenorphine sublingually for opiate substitution during pregnancy and lactation collected foremilk and hindmilk samples with each feeding for 24 hours. The average maternal dosage was 9.3 mg daily and the median was 7 mg daily (range 2.4 to 24 mg daily). The average buprenorphine concentration in milk was 3.65 mcg/L and the average norbuprenorphine concentration was 1.94 mcg/L. These corresponded to daily dosages of 0.55 and 0.29 mcg/kg, respectively and weight-adjusted dosages of 0.38% and 0.18% of the maternal dosage, respectively.[20]
One woman taking sublingual buprenorphine in an unstated dosage donated breastmilk samples on 5 occasions over a 30-day period. Buprenorphine concentrations ranged from 2.4 to 4 mcg/L, buprenorphine glucuronide 0.8 to 9.3 mcg/L, norbuprenorphine 3.2 to 4.0 mcg/L, and norbuprenorphine glucuronide 24.9 to 34.5 mcg/L.[21]
Ten women on buprenorphine maintenance therapy with sublingual dosages ranging from 2 to 22 mg once daily. Milk samples were provided 2 to 2.5 hours after the daily dose on days 2, 3, 4, 14, and 30 postpartum. Median buprenorphine milk levels ranged from 1.4 to 4.8 mcg/L, median norbuprenorphine milk levels ranged from 0.1 to 0.2 mcg/L, median buprenorphine glucuronide milk levels ranged from 2.3 to 3.2 mcg/L, and median norbuprenorphine glucuronide milk levels ranged from 0.4 to 1.8 mcg/L. Concentrations in milk were positively correlated to the maternal dose.[22]
Four women receiving buprenorphine and naloxone combination therapy as sublingual filmstrips for opioid use disorder provided milk samples at 2.5 hours after ingestion of the drug. Three participants provided samples on Days 2, 3, 4, 14, and 30; one participant provided samples only until Day 4. Maternal buprenorphine-naloxone doses ranged from 12 mg/3 mg to 20 mg/5 mg. Average buprenorphine concentrations in milk ranged from 2.43 to 8.37 mcg/L. Average buprenorphine glucuronide concentrations in milk ranged from 3.95 mcg/L to undetectable. Average norbuprenorphine concentrations in milk ranged from 2.3 to 4.5 mcg/L. Average norbuprenorphine glucuronide concentrations in milk ranged from 2.68 mcg/L to 11.23 mcg/L.[23]
Infant Levels. Six nursing infants from 5 to 8 days of age whose mothers were taking a median daily dose of 0.29 mg/kg of buprenorphine sublingually had one urine sample collected between 4 and 20 hours after the previous maternal dose. Buprenorphine was undetectable (<187 ng/L) in 3 infants; the other 3 had urine concentrations of about 468 ng/L. Norbuprenorphine urine concentrations ranged from 414 to 1987 ng/L (median 952 ng/L). A seventh 9-month-old breastfed infant whose mother was taking 20 mg (0.32 mg/kg) of buprenorphine daily had serum and urine collected. Serum concentrations of buprenorphine and norbuprenorphine were 234 ng/L and 745 ng/L, respectively, at 2.25 hours after the previous maternal dose. A urine sample obtained 3.5 hours after the previous maternal dose contained <234 ng/L and 455 ng/L of the drug and metabolite, respectively.[19]
The infant of a mother receiving buprenorphine (dosage not stated) was breastfeeding (extent not stated). A single blood sample from the infant after 14 days of maternal sublingual buprenorphine use contained 0.7 mcg/L of buprenorphine. No buprenorphine metabolites were detected.[21]
Nine infants were breastfed (3 exclusively and 6 partially) by mothers who were taking sublingual buprenorphine in single daily doses ranging from 2 to 22 mg once daily. A blood sample from a heel stick was taken on day 14 postpartum. Doses of the individual mothers and the time since the last dose and time since the last breastfeeding were not stated. Buprenorphine was detectable (>0.1 mcg/L) in the plasma of only 4 of the infants, with the highest reported plasma level of 2.9 mcg/L. Norbuprenorphine (<2 mcg/L) and the glucuronide metabolites of buprenorphine (<0.1 mcg/L) and norbuprenorphine (<0.25) were not detectable in any of the infants.[22]
An exclusively breastfed 2-week-old infant was brought to the emergency department because of somnolence and decreased feeding. He had pinpoint pupils, lethargy and a Glasgow coma score of 5. The infant’s mother was taking buprenorphine 8 mg twice daily for several months and denied any illicit drug use. Sixteen hours after symptom onset, urine levels of norbuprenorphine (13 mcg/L) and norbuprenorphine glucuronide (11 mcg/L) were elevated. Buprenorphine (<2 mcg/L) and buprenorphine glucuronide (<5 mcg/L) urine levels were in a typical range.[24]
Women receiving buprenorphine and naloxone combination in doses ranging from 12 mg/3 mg to 20 mg/5 mg therapy as sublingual filmstrips for opioid use disorder breastfed their infants, one exclusively and three partially. Plasma was obtained from 3 infants via a heel stick on day 14. Buprenorphine, buprenorphine glucuronide, and norbuprenorphine glucuronide were either not detected or detected at concentrations below the limit of quantification in all infant plasma samples at day 14. Two infants had concentrations of norbuprenorphine, 0.9 and 5.4 mcg/L in plasma on day 14.[23]
Effects in Breastfed Infants
Numerous infants have been reported to breastfeed during maternal narcotic abstinence therapy with buprenorphine with no adverse effects, one for 6 months.[14,17,25-27] The amounts of buprenorphine in milk may not be sufficient to prevent neonatal withdrawal, and treatment of infant may be required.[16,28]
Despite breastfeeding and relatively high infant serum drug levels, mild buprenorphine withdrawal occurred in the neonate of a mother taking buprenorphine 4 mg daily (route not specified) during pregnancy and postpartum for heroin dependency.[14] This indicates that an insufficient dosage appeared in milk to prevent neonatal abstinence.
Ten women who had undergone cesarean section delivery of term newborns were given extradural buprenorphine 200 mcg followed by 8.4 mcg/hour with an anesthetic for postoperative pain for 3 days postpartum. A control group of 10 other women were given extradural anesthetic only without buprenorphine. Over 11 days postpartum, newborns of mothers in the buprenorphine group had much lower milk intake and lower weight gain than those in the non-buprenorphine group. The authors suggested that extradural buprenorphine suppressed infant breastfeeding. Infant neurobehavioral assessments were not performed.[29]
Six infants whose mothers were taking buprenorphine during pregnancy and postpartum were breastfed. Four of the infants had signs of opioid abstinence, indicating that the amounts of buprenorphine in breastmilk were inadequate to prevent withdrawal. At 1 month after discharge from the hospital, all infants had normal development and weight gain.[19]
Seven infants who averaged 1.12 months of age (range 0.58 to 1.85 months) were being breastfed by mothers taking buprenorphine for opiate substitution during pregnancy and lactation. Urine screening indicated that 4 mothers had also been using cannabis, 1 was using unprescribed benzodiazepines, and 1 mother was using both cannabis and benzodiazepines. Four of the infants were exclusively breastfed and 3 were mostly breastfed. Infants had no apparent drug-related adverse effects and showed satisfactory developmental progress.[20]
A mother used buprenorphine (dose and indication not stated) during pregnancy. Her infant displayed no signs of neonatal abstinence at birth. The infant was breastfed (extent not stated) until 4 months of age when the mother stopped breastfeeding. Two days later the infant had withdrawal symptoms including frequent yawning, sneezing, pupillary dilation, agitation, sweating, hyperactive Moro reflex, myoclonic jerks, tremors, and insomnia. The infant was given methadone with immediate improvement of her withdrawal symptoms. The infant’s withdrawal symptoms were probably caused by abrupt withdrawal of breastfeeding.[30]
In a study of 7 women taking buprenorphine in a median dose of 7 mg daily (range 2.4 to 24 mg daily) , breastfed infants were followed-up at 3 and 4 weeks of age. Four infants were exclusively breastfed and 3 were partially breastfed. At the follow-up visits, infants were assessed for weight gain, sleeping patterns, skin color, and elimination and hydration patterns. All infants had values within normal limits for these parameters at follow-up.[31]
A cohort of 124 infants exposed during pregnancy to maternal medication for opioid maintenance therapy were followed postpartum in a Norwegian study. Forty-six infants were born to mothers taking buprenorphine. Overall, infants who were breastfed had a lower rate of neonatal abstinence symptoms and a shorter duration of therapy for neonatal abstinence. However, the differences were not statistically significant for the subset of infants whose mothers took buprenorphine.[32]
A study of pregnant women being treated for opiate dependency with buprenorphine at a clinic in Vienna were followed as were their newborn infants. No difference was found between breastfed (n = 31) and nonbreastfed infant (n = 41) in average measures of neonatal abstinence, dosage requirements of morphine, durations of treatment for neonatal abstinence or durations of hospital stays.[30]
A statewide retrospective database study found that infants diagnosed with NAS spent a median of 2 days less in the hospital if they were breastfed than those who were not breastfed.[33]
The results of two multicenter cohort studies were compared. The original study had 86 newborns with neonatal abstinence and the second had 113 infants. All infants had been exposed to methadone or buprenorphine in utero. Infants who were breastfed had a shorter hospitalization by 4.5 to 7.5 days than infants who were not breastfed. Infants who were exposed to buprenorphine had a shorter hospitalization by 4 to 5 days than those exposed to methadone.[34]
A study of 89 pregnant women were treated with buprenorphine for maintenance of opioid abstinence. Fewer of their infants who were exclusively breastfed required morphine for neonatal abstinence symptoms than those who were not exclusively breastfed. Exclusively breastfed infants had an earlier time to peak abstinence symptoms and fewer days in the hospital than the nonexclusively breastfed infants.[35]
A 2-week-old infant was brought to the emergency department for drowsiness and poor feeding. He was lethargic and had pinpoint pupils upon admission, with a Glasgow coma score of 5 and blood glucose of 79 mg/dL. Two doses of naloxone 0.15 mg resulted in infant crying and improved tone. The infant’s mother had been taking buprenorphine 8 mg twice daily for several months for opioid use disorder. She was exclusively breastfeeding and denied illicit drug use. After admission to the hospital, the infant had several episodes of hypoglycemia and required another dose of naloxone for bradycardia, lethargy and pinpoint pupils with some improvement. Breastfeeding was stopped and the infant developed mild withdrawal symptoms that did not require treatment.[36] The infant’s symptoms were probably caused by buprenorphine, but the contribution by breastfeeding cannot be differentiated from prenatal exposure.
Effects on Lactation and Breastmilk
Buprenorphine can increase serum prolactin.[37] However, the prolactin level in a mother with established lactation may not affect her ability to breastfeed.
In a multicenter prospective study of 246 pregnant women receiving either methadone or buprenorphine for opiate dependency, 153 women were receiving high-dose buprenorphine. Twenty-two percent of women receiving buprenorphine breastfed their infants, which was the same percentage as those receiving methadone.[38]
A retrospective chart review of 276 opiate-dependent mothers who delivered in a Baby Friendly Hospital found that mothers taking buprenorphine or methadone for opiate dependency were unlikely to breastfeed their infants. Only 45% of the 20 mothers on buprenorphine maintenance initiated breastfeeding. Of all women in the study, 60% discontinued breastfeeding before discharge from the hospital.[39]
A retrospective case series reported on 85 opioid-dependent women maintained on buprenorphine during pregnancy and postpartum during the period of December 2007 to August 2012. Of these women, 65 were breastfeeding on discharge from the hospital and 66% of these were breastfeeding at their 6- to 8-week follow-up appointment (extent of nursing not stated).[40]
A retrospective cohort study in Australia compared breastfeeding rates on discharge of drug-using mothers who were taking either buprenorphine, other opiates or nonopioids (e.g., benzodiazepines, amphetamines, cocaine, alcohol, inhalants, cannabinoids, psychotropics). Breastfeeding rates at discharge from the hospital were as follows: buprenorphine 27%, other opiates 31%, and nonopioids 51%.[41]
A small retrospective study found that only 3 of 10 pregnant women treated with buprenorphine plus naloxone for opioid dependence were breastfeeding their infants at the time of hospital discharge.[42]
A retrospective cohort study of 150 women enrolled in a substance abuse treatment program found that women taking methadone had a higher prevalence of breastfeeding than women taking buprenorphine plus naloxone. However, this difference appeared to be related to the greater intention to breastfeed before delivery in the methadone group.[43]
A retrospective cohort study of 228 women enrolled in a perinatal substance abuse treatment program found that women taking buprenorphine had a higher prevalence of breastfeeding than women taking methadone. The intention to breastfeed before delivery was similar in both groups.[44]
A systematic review of studies on the effect of breastfeeding on the outcomes of infants whose mothers were taking methadone during pregnancy and postpartum concluded that the association between newborn feeding method and neonatal abstinence syndrome among newborns exposed to buprenorphine in breastmilk was unclear.[45]
A retrospective chart review of 64 mothers given buprenorphine postpartum for opioid use disorder found that mothers who breastfed their infants were more likely to attend a follow-up appointment within 10 to 14 weeks postpartum.[46]
A small retrospective study of 19 mothers with for opiate use disorder found that mothers who were taking buprenorphine were more likely to breastfeed their infants than mothers taking methadone (70% vs 29%).[47]
A retrospective cohort study from three medical centers studied women who were begun on buprenorphine for opioid use disorder. Women who had undergone more than one attempt at initiating sublingual buprenorphine had a much higher rate of not breastfeeding their infants than those who had a single successful attempt at buprenorphine initiation at both maternal discharge (24% vs 79%) and infant discharge (24% vs 55%).[48]
Alternate Drugs to Consider
(Analgesia) Acetaminophen, Butorphanol, Fentanyl, Hydromorphone, Ibuprofen, Morphine; (Opiate Dependency) Methadone, Naltrexone
References
- 1.
- Kocherlakota P. Neonatal abstinence syndrome. Pediatrics 2014;134:e547-61. [PubMed: 25070299]
- 2.
- Sutter MB, Leeman L, Hsi A. Neonatal opioid withdrawal syndrome. Obstet Gynecol Clin North Am 2014;41:317-34. [PubMed: 24845493]
- 3.
- Mozurkewich EL, Rayburn WF. Buprenorphine and methadone for opioid addiction during pregnancy. Obstet Gynecol Clin North Am 2014;41:241-53. [PubMed: 24845488]
- 4.
- Bagley SM, Wachman EM, Holland E, Brogly SB. Review of the assessment and management of neonatal abstinence syndrome. Addict Sci Clin Pract 2014;9:19. [PMC free article: PMC4166410] [PubMed: 25199822]
- 5.
- Lefevere J, Allegaert K. Question: is breastfeeding useful in the management of neonatal abstinence syndrome? Arch Dis Child 2015;100:414-5. [PubMed: 25784740]
- 6.
- Reece-Stremtan S, Marinelli KA. ABM clinical protocol #21: Guidelines for breastfeeding and substance use or substance use disorder, revised 2015. Breastfeed Med 2015;10:135-41. [PMC free article: PMC4378642] [PubMed: 25836677]
- 7.
- Cleveland LM. Breastfeeding recommendations for women who receive medication-assisted treatment for opioid use disorders: AWHONN Practice Brief Number 4. Nurs Womens Health 2016;20:432-4. [PubMed: 27520608]
- 8.
- McQueen K, Murphy-Oikonen J. Neonatal abstinence syndrome. N Engl J Med 2016;375:2468-79. [PubMed: 28002715]
- 9.
- Holmes AP, Schmidlin HN, Kurzum EN. Breastfeeding considerations for mothers of infants with neonatal abstinence syndrome. Pharmacotherapy 2017;37:861-9. [PubMed: 28488805]
- 10.
- Committee Opinion No. 711: Opioid use and opioid use disorder in pregnancy. Obstet Gynecol 2017;130:e81-e94. [PubMed: 28742676]
- 11.
- Bogen DL, Whalen BL. Breastmilk feeding for mothers and infants with opioid exposure: What is best? Semin Fetal Neonatal Med 2019;24:95-104. [PubMed: 30922811]
- 12.
- Harris M, Schiff DM, Saia K, et al. Academy of Breastfeeding Medicine Clinical Protocol #21: Breastfeeding in the setting of substance use and substance use disorder (Revised 2023). Breastfeed Med 2023;18:715-33. [PMC free article: PMC10775244] [PubMed: 37856658]
- 13.
- Wachman EM, Schiff DM, Silverstein M. Neonatal abstinence syndrome: Advances in diagnosis and treatment. JAMA 2018;319:1362-74. [PubMed: 29614184]
- 14.
- Marquet P, Chevrel J, Lavignasse P, et al. Buprenorphine withdrawal syndrome in a newborn. Clin Pharmacol Ther 1997;62:569-71. [PubMed: 9390114]
- 15.
- Jernite M, Diemunsch P, Kintz P. Buprenorphine excretion in breast milk. Anesthesiology 1999;91 (3A):A1095.
- 16.
- Jernite M, Diemunsch P, Kintz P, et al. [Passage of buprenorphine into mother's milk]. Ann Fr Anesth Reanim 1999;18 (Suppl 1):109S.
- 17.
- Johnson RE, Jones HE, Jasinski DR, et al. Buprenorphine treatment of pregnant opioid-dependent women: Maternal and neonatal outcomes. Drug Alcohol Depend 2001;63:97-103. [PubMed: 11297835]
- 18.
- Grimm D, Pauly E, Poschl J, et al. Buprenorphine and norbuprenorphine concentrations in human breast milk samples determined by liquid chromatography-tandem mass spectrometry. Ther Drug Monit 2005;27:526-30. [PubMed: 16044112]
- 19.
- Lindemalm S, Nydert P, Svensson JO, et al. Transfer of buprenorphine into breast milk and calculation of infant drug dose. J Hum Lact 2009;25:199-205. [PubMed: 19136395]
- 20.
- Ilett KF, Hackett LP, Gower S, et al. Estimated dose exposure of the neonate to buprenorphine and its metabolite norbuprenorphine via breastmilk during maternal buprenorphine substitution treatment. Breastfeed Med 2012;7:269-74. [PubMed: 22011128]
- 21.
- Swortwood MJ, Scheidweiler KB, Barnes AJ, et al. Simultaneous quantification of buprenorphine, naloxone and phase I and II metabolites in plasma and breastmilk by liquid chromatography-tandem mass spectrometry. J Chromatogr A 2016;1446:70-7. [PubMed: 27083254]
- 22.
- Jansson LM, Spencer N, McConnell K, et al. Maternal buprenorphine maintenance and lactation. J Hum Lact 2016;32:675-81. [PubMed: 27563013]
- 23.
- Jansson LM, McConnell K, Velez M, et al. Buprenorphine-naloxone maintenance and lactation. J Hum Lact 2024;40:113-9. [PubMed: 38018534]
- 24.
- Dorey A, Owen K, Chenoweth J, et al. Possible buprenorphine toxicity in a breastfeeding neonate. Clin Toxicol 2019;57:889-90. doi:10.1080/15563650.2019.1636569 [CrossRef]
- 25.
- Schindler SD, Eder H, Ortner R, et al. Neonatal outcome following buprenorphine maintenance during conception and throughout pregnancy. Addiction 2003;98:103-10. [PubMed: 12492761]
- 26.
- Kayemba-Kay's S, Laclyde JP. Buprenorphine withdrawal syndrome in newborns: A report of 13 cases. Addiction 2003;98:1599-604. [PubMed: 14616186]
- 27.
- Johnson RE, Jones HE, Fischer G. Use of buprenorphine in pregnancy: patient management and effects on the neonate. Drug Alcohol Depend 2003;70 (2 Suppl):S87-S101. [PubMed: 12738353]
- 28.
- Loustauneau A, Auriacombe M, Daulouede JP, Tignol J. [Is buprenorphine a potential alternative to methadone for treating pregnant drug users? Inventory of clinical data in the literature]. Ann Med Interne (Paris) 2002;153 (7 Suppl):2S31-6. [PubMed: 12518080]
- 29.
- Hirose M, Hosokawa T, Tanaka Y. Extradural buprenorphine suppresses breast feeding after cesarean section. Br J Anaesth 1997;79:120-1. [PubMed: 9301399]
- 30.
- Elladki H, Thill P. Buprenorphine withdrawal in an infant after cessation of breastfeeding: A case report and review of the literature. Pharmacotherapy 2011;31:435e. doi:10.1592/phco.31.10.311e [CrossRef]
- 31.
- Gower S, Bartu A, Ilett KF, et al. The wellbeing of infants exposed to buprenorphine via breast milk at 4 weeks of age. J Hum Lact 2014;30:217-23. [PubMed: 24399105]
- 32.
- Welle-Strand GK, Skurtveit S, Jansson LM, et al. Breastfeeding reduces the need for withdrawal treatment in opioid-exposed infants. Acta Paediatr 2013;102:1060-6. [PubMed: 23909865]
- 33.
- Metz VE, Comer SD, Pribasnig A, et al. Observational study in an outpatient clinic specializing in treating opioid-dependent pregnant women: Neonatal abstinence syndrome in infants exposed to methadone-, buprenorphine- and slow-release oral morphine. Heroin Addict Relat Clin Probl 2015;17:5-15. https://www
.heroinaddictionrelatedclinicalproblems .org/harcp-archives .php?year=2015 - 34.
- Short VL, Gannon M, Abatemarco DJ. The association between breastfeeding and length of hospital stay among infants diagnosed with neonatal abstinence syndrome: A population-based study of in-hospital births. Breastfeed Med 2016;11:343-9. [PubMed: 27529500]
- 35.
- Wachman EM, Hayes MJ, Sherva R, et al. Association of maternal and infant variants in PNOC and COMT genes with neonatal abstinence syndrome severity. Am J Addict 2017;26:42-9. [PMC free article: PMC5206487] [PubMed: 27983768]
- 36.
- Wong J, Saver B, Scanlan JM, et al. Does maternal buprenorphine dose affect severity or incidence of neonatal abstinence syndrome. J Addict Med 2018;12:435-41. [PubMed: 29905586]
- 37.
- Saarialho-Kere U, Mattila MJ, Paloheimo M, Seppala T. Psychomotor, respiratory and neuroendocrinological effects of buprenorphine and amitriptyline in healthy volunteers. Eur J Clin Pharmacol 1987;33:139-46. [PubMed: 3691607]
- 38.
- Lejeune C, Aubisson S, Simmat-Durand L, et al. [Withdrawal syndromes of newborns of pregnant drug abusers maintained under methadone or high-dose buprenorphine: 246 cases]. Ann Med Interne (Paris) 2001;152 (Suppl 7):21-7. [PubMed: 11965095]
- 39.
- Wachman EM, Byun J, Philipp BL. Breastfeeding rates among mothers of infants with neonatal abstinence syndrome. Breastfeed Med 2010;5:159-64. [PubMed: 20658895]
- 40.
- O'Connor AB, Collett A, Alto WA, O'Brien LM. Breastfeeding rates and the relationship between breastfeeding and neonatal abstinence syndrome in women maintained on buprenorphine during pregnancy. J Midwifery Womens Health 2013;58:383-8. [PubMed: 23931660]
- 41.
- Patel P, Abdel-Latif ME, Hazelton B, et al. Perinatal outcomes of Australian buprenorphine-exposed mothers and their newborn infants. J Paediatr Child Health 2013;49:746-53. [PubMed: 23745982]
- 42.
- Debelak K, Morrone WR, O'Grady KE, Jones HE. Buprenorphine + naloxone in the treatment of opioid dependence during pregnancy-initial patient care and outcome data. Am J Addict 2013;22:252-4. [PubMed: 23617867]
- 43.
- Gawronski KM, Prasad MR, Backes CR, et al. Neonatal outcomes following in utero exposure to buprenorphine/naloxone or methadone. SAGE Open Med 2014;2:2050312114530282. [PMC free article: PMC4607220] [PubMed: 26770721]
- 44.
- Yonke N, Maston R, Weitzen S, Leeman L. Breastfeeding intention compared with breastfeeding postpartum among women receiving medication-assisted treatment. J Hum Lact 2019;35:71-9. [PubMed: 29723483]
- 45.
- McQueen K, Taylor C, Murphy-Oikonen J. Systematic review of newborn feeding method and outcomes related to neonatal abstinence syndrome. J Obstet Gynecol Neonatal Nurs 2019;48:398-407. [PubMed: 31034790]
- 46.
- Ray-Griffith S, Tharp E, Coker JL, et al. Buprenorphine medication for opioid use disorder: A study of factors associated with postpartum treatment retention. Am J Addict 2021;30:43-8. [PMC free article: PMC7772251] [PubMed: 32673447]
- 47.
- Skiba B, Feldman A. Factors associated with breastfeeding among mothers being treated with opiates. J Invest Med 2022;70:1191. doi:10.1136/jim-2022-ERM.275 [CrossRef]
- 48.
- Kelly JC, Ayala NK, Holroyd L, et al. Number of buprenorphine induction attempts impacts maternal and neonatal outcomes: A multicenter cohort study. Am J Obstet Gynecol MFM 2023;5:100998. doi:10.1016/j.ajogmf.2023.100998 [PubMed: 38236700] [CrossRef]
Substance Identification
Substance Name
Buprenorphine
CAS Registry Number
52485-79-7
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Methadone.[Drugs and Lactation Database (...]Review Methadone.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydromorphone.[Drugs and Lactation Database (...]Review Hydromorphone.. Drugs and Lactation Database (LactMed®). 2006
- Review Dihydrocodeine.[Drugs and Lactation Database (...]Review Dihydrocodeine.. Drugs and Lactation Database (LactMed®). 2006
- Review Oxymorphone.[Drugs and Lactation Database (...]Review Oxymorphone.. Drugs and Lactation Database (LactMed®). 2006
- Review Hydrocodone.[Drugs and Lactation Database (...]Review Hydrocodone.. Drugs and Lactation Database (LactMed®). 2006
- Buprenorphine - Drugs and Lactation Database (LactMed®)Buprenorphine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
