Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
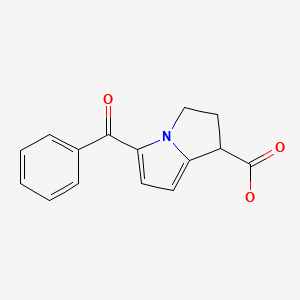
CASRN: 74103-06-3
Drug Levels and Effects
Summary of Use during Lactation
Milk levels of ketorolac are low with the usual oral dosage, but milk levels have not been measured after higher injectable dosages or with the nasal spray. Ketorolac injection is used for a short time (typically 24 hours) after cesarean section in some hospital protocols with no evidence of harm to breastfed infants. However, the ketorolac dose an infant receives in colostrum is very low because of the small volume of colostrum produced. Some evidence suggests that IV ketorolac as part of a multimodal post-cesarean section analgesia reduces percentage of mothers who fail exclusive breastfeeding compared to patient-controlled IV morphine-based analgesia. Ketorolac has strong antiplatelet activity and can cause gastrointestinal bleeding. The manufacturer indicates that ketorolac is contraindicated during breastfeeding, so an alternate drug is preferred after the first 24 to 72 hours when larger volumes of milk are produced, especially while nursing a newborn or preterm infant.
Maternal use of ketorolac eye drops would not be expected to cause any adverse effects in breastfed infants. To substantially diminish the amount of drug that reaches the breastmilk after using eye drops, place pressure over the tear duct by the corner of the eye for 1 minute or more, then remove the excess solution with an absorbent tissue.
Drug Levels
Maternal Levels. Ten women who were 2 to 6 days postpartum and were taking ketorolac 10 mg orally four times daily had their milk ketorolac levels measured at various times during 2 days of drug administration. Milk levels were undetectable (<5 mcg/L) in 4 of the patients at all collection times. In the other 6 patients, ketorolac was detectable 2 hours after the first dose of the day in concentrations from 5.2 to 7.3 mcg/L on day 1 and from 5.9 to 7.9 mcg/L on day 2. Ketorolac was not detectable in milk in any patient at 10 hours after the last dose.[1] The paper erroneously states that the breastfed infant would receive an estimated 3.16 to 7.9 mg daily based on a calculation error. The correct calculation yields an estimated maximum daily intake of 7.9 mcg or 0.18% of the maternal weight-adjusted dosage.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
A randomized, double-blind study compared standard care of mothers receiving a cesarean section delivery (n = 60) to those receiving standard care plus multimodal pain management that included a single dose of 60 mg of intramuscular ketorolac given at the time of fascial closure (n = 60). No significant differences in abnormal neonatal growth, difficulty feeding, neonatal sedation, or respiratory depression rates between the two groups were seen during the first month postpartum.[2]
Effects on Lactation and Breastmilk
A randomized, double-blind study compared standard care of mothers receiving a cesarean section delivery (n = 60) to those receiving standard care plus multimodal pain management that included a single dose of 60 mg of intramuscular ketorolac given at the time of fascial closure (n = 60). No significant differences in breastfeeding rates (78% and 79%, respectively) were seen during the first month postpartum.[2]
In a study comparing standard of care to enhanced recovery after cesarean section deliveries, a fixed dose of ketorolac 15 mg every 6 hours intravenously for 24 hours postpartum was part of the enhanced recovery protocol whereas as needed ketorolac 15 mg intravenously was part of the standard protocol. Patients in the enhanced recovery protocol (n = 58) had a greater frequency of exclusive breastfeeding (67%) than those in the standard protocol (48%; n = 60).[3]
A retrospective study evaluated 1349 women who had undergone a cesarean section and were given ketorolac within 15 minutes of the end of surgery. The results indicated that there was no difference in pain control in the first 6 hours after surgery nor in the percentage of women who were breastfeeding at discharge.[4]
A prospective cohort study of postcesarean pain control compared (1) morphine PCA and scheduled ibuprofen for the first 12 hours followed by continued scheduled ibuprofen with hydrocodone-acetaminophen as needed to a multimodal pain management regimen consisting of (2) acetaminophen 1000 mg orally every 8 hours, ketorolac 30 mg IV once initially, then 15 mg IV every 8 hours for 24 hours, then ibuprofen 600 mg orally every 8 hours for the remainder of the postoperative course with opioids given only as needed. Of women who planned to exclusively breastfeed on admission, fewer women used formula prior to discharge in the multimodal group compared to the traditional group (9% vs. 12%).[5]
Alternate Drugs to Consider
(Systemic) Acetaminophen, Flurbiprofen, Ibuprofen, Indomethacin, Naproxen, Piroxicam
References
- 1.
- Wischnik A, Manth SM, Lloyd J, et al. The excretion of ketorolac tromethamine into breast milk after multiple oral dosing. Eur J Clin Pharmacol. 1989;36:521–4. [PubMed: 2787750]
- 2.
- Hadley EE, Monsivais L, Pacheco L, et al. Multimodal pain management for cesarean delivery: A double-blinded, placebo-controlled, randomized clinical trial. Am J Perinatol. 2019;36:1097–105. [PubMed: 30822800]
- 3.
- Teigen NC, Sahasrabudhe N, Doulaveris G, et al. Enhanced recovery after surgery at cesarean delivery to reduce postoperative length of stay: A randomized controlled trial. Am J Obstet Gynecol. 2020;222:372.e1–372.e10. [PubMed: 31669738]
- 4.
- Yurashevich M, Pedro C, Fuller M, et al. Intra-operative ketorolac 15 mg versus 30 mg for analgesia following cesarean delivery: A retrospective study. Int J Obstet Anesth. 2020;44:116–21. [PubMed: 32947103]
- 5.
- Macias DA, Adhikari EH, Eddins M, et al. A comparison of acute pain management strategies after cesarean delivery. Am J Obstet Gynecol. 2021;226:407.e1–407.e7. [PubMed: 34534504]
Substance Identification
Substance Name
Ketorolac
CAS Registry Number
74103-06-3
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Bromfenac.[Drugs and Lactation Database (...]Review Bromfenac.. Drugs and Lactation Database (LactMed®). 2006
- Review Azelastine.[Drugs and Lactation Database (...]Review Azelastine.. Drugs and Lactation Database (LactMed®). 2006
- Review Epinastine.[Drugs and Lactation Database (...]Review Epinastine.. Drugs and Lactation Database (LactMed®). 2006
- Review Diclofenac.[Drugs and Lactation Database (...]Review Diclofenac.. Drugs and Lactation Database (LactMed®). 2006
- Review Brimonidine.[Drugs and Lactation Database (...]Review Brimonidine.. Drugs and Lactation Database (LactMed®). 2006
- Ketorolac - Drugs and Lactation Database (LactMed®)Ketorolac - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
