Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 33643-46-8
Drug Levels and Effects
Summary of Use during Lactation
Esketamine is the more potent S-isomer of the racemic drug, ketamine. Esketamine nasal spray used as an antidepressant has not been studied during breastfeeding. Minimal data indicate that single doses of intravenous esketamine or ketamine use during cesarean section delivery may not affect the breastfed infant or lactation. Until more data are available, repeated doses esketamine nasal spray should probably be avoided during breastfeeding. If esketamine is used, monitor the infant for sedation, poor feeding and poor weight gain.
Drug Levels
Maternal Levels. Relevant published information was not found as of the revision date.
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Four mothers who received epidural analgesia with lidocaine and bupivacaine for cesarean section also received general anesthesia with ketamine and midazolam (dosages not specified). Their infants were either breastfed or received their mother's breastmilk by bottle. No adverse effects were reported in the infants.[1]
Effects on Lactation and Breastmilk
A pregnant woman sustained 28% body surface area burns near term. She underwent an emergency cesarean section on her due date under ketamine anesthesia. Although the infant required vigorous resuscitation, the infant began breastfeeding immediately. The infant had transient jaundice that resolved in a few days.[2]
A study compared women undergoing cesarean section who received either placebo or S-ketamine (esketamine) 0.5 mg/kg intramuscularly, followed by a continuous infusion of 2 mcg/kg/minute for 12 hours. This low dose was used to enhance analgesia and reduce residual pain rather than to provide anesthesia. All women received intraspinal bupivacaine 8 to10 mg and sufentanil 5 mcg for analgesia, as well as midazolam 0.02 mg/kg intravenously before the S-ketamine or placebo injection. Postoperatively, patients received patient-controlled intravenous morphine for 24 hours, followed by acetaminophen, oral ketorolac and a single dose of ondansetron 8 mg intravenously as needed. Of the 56 patients enrolled in the study (28 in each group), 13 in each group were contacted at 3 years postpartum. Patients who received placebo reported breastfeeding for an average of 10.5 months and those who received S-ketamine reported breastfeeding for an average of 8 months; however, the difference was not statistically significant.[3]
A randomized, double-blind study compared the effects of intravenous propofol 0.25 mg/kg, ketamine 0.25 mg/kg, ketamine 25 mg plus propofol 25 mg, and saline placebo for pain control in mothers post-cesarean section. A single dose was given immediately after clamping of the umbilical cord. The time to the first breastfeeding was 58 minutes in those who received placebo, 31.9 minutes with ketamine and 25.8 minutes with propofol plus ketamine. The time was significantly shorter than the other groups with the combination.[4]
A study of women with gestational diabetes undergoing elective cesarean section randomized them to postoperative patient-controlled analgesia with either intravenous esketamine 0.5 mg/kg, sufentanil 150 mcg and ondansetron 4 mg (n = 70) or sufentanil and ondansetron alone in the same doses (n = 70). There was no difference between the groups in the time to first lactation, with most beginning at 24 to 48 hours after delivery.[5]
References
- 1.
- Ortega D, Viviand X, Lorec AM, et al. Excretion of lidocaine and bupivacaine in breast milk following epidural anesthesia for cesarean delivery. Acta Anaesthesiol Scand 1999;43:394-7. [PubMed: 10225071]
- 2.
- Mokube JA, Verla VS, Mbome VN, Bitang AT. Burns in pregnancy: A case report from Buea Regional Hospital, Cameroon. Pan Afr Med J 2009;3:21. [PMC free article: PMC2984292] [PubMed: 21532730]
- 3.
- Suppa E, Valente A, Catarci S, et al. A study of low-dose S-ketamine infusion as "preventive" pain treatment for cesarean section with spinal anesthesia: Benefits and side effects. Minerva Anestesiol 2012;78:774-81. [PubMed: 22374377]
- 4.
- Jaafarpour M, Vasigh A, Khajavikhan J, Khani A. Effect of ketofol on pain and complication after Caesarean delivery under spinal anaesthesia: A randomized double-blind clinical trial. J Clin Diagn Res 2017;11:UC04-UC07. [PMC free article: PMC5427408] [PubMed: 28511482]
- 5.
- Han T, Chen Q, Huang J, et al. Low-dose esketamine with sufentanil for postcesarean analgesia in women with gestational diabetes mellitus: A prospective, randomized, double-blind study. Front Endocrinol (Lausanne) 2023;14:1202734. [PMC free article: PMC10454896] [PubMed: 37635978]
Substance Identification
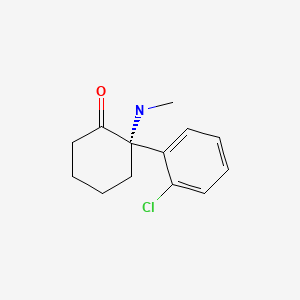
Substance Name
Esketamine
CAS Registry Number
33643-46-8
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- Review Ketamine.[Drugs and Lactation Database (...]Review Ketamine.. Drugs and Lactation Database (LactMed®). 2006
- Efficacy and Safety of Flexibly Dosed Esketamine Nasal Spray Combined With a Newly Initiated Oral Antidepressant in Treatment-Resistant Depression: A Randomized Double-Blind Active-Controlled Study.[Am J Psychiatry. 2019]Efficacy and Safety of Flexibly Dosed Esketamine Nasal Spray Combined With a Newly Initiated Oral Antidepressant in Treatment-Resistant Depression: A Randomized Double-Blind Active-Controlled Study.Popova V, Daly EJ, Trivedi M, Cooper K, Lane R, Lim P, Mazzucco C, Hough D, Thase ME, Shelton RC, et al. Am J Psychiatry. 2019 Jun 1; 176(6):428-438. Epub 2019 May 21.
- Effect of Esketamine Nasal Spray on Olfactory Function and Nasal Tolerability in Patients with Treatment-Resistant Depression: Results from Four Multicenter, Randomized, Double-Blind, Placebo-Controlled, Phase III Studies.[CNS Drugs. 2021]Effect of Esketamine Nasal Spray on Olfactory Function and Nasal Tolerability in Patients with Treatment-Resistant Depression: Results from Four Multicenter, Randomized, Double-Blind, Placebo-Controlled, Phase III Studies.Doty RL, Popova V, Wylie C, Fedgchin M, Daly E, Janik A, Ochs-Ross R, Lane R, Lim P, Cooper K, et al. CNS Drugs. 2021 Jul; 35(7):781-794. Epub 2021 Jul 7.
- Effects of Mu-Opiate Receptor Gene Polymorphism rs1799971 (A118G) on the Antidepressant and Dissociation Responses in Esketamine Nasal Spray Clinical Trials.[Int J Neuropsychopharmacol. 2020]Effects of Mu-Opiate Receptor Gene Polymorphism rs1799971 (A118G) on the Antidepressant and Dissociation Responses in Esketamine Nasal Spray Clinical Trials.Saad Z, Hibar D, Fedgchin M, Popova V, Furey ML, Singh JB, Kolb H, Drevets WC, Chen G. Int J Neuropsychopharmacol. 2020 Dec 3; 23(9):549-558.
- Review Long-term safety of ketamine and esketamine in treatment of depression.[Expert Opin Drug Saf. 2022]Review Long-term safety of ketamine and esketamine in treatment of depression.Nikayin S, Murphy E, Krystal JH, Wilkinson ST. Expert Opin Drug Saf. 2022 Jun; 21(6):777-787. Epub 2022 Apr 19.
- Esketamine - Drugs and Lactation Database (LactMed®)Esketamine - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
