Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 1211327-92-2
Drug Levels and Effects
Summary of Use during Lactation
After a standard subcutaneous dose of peginterferon beta-1a, the amount of peginterferon beta 1a in milk is miniscule. In addition, because interferon is poorly absorbed orally, it is not likely to reach the bloodstream of the infant. Polyethylene glycol is not excreted into breastmilk.[1] Many women have breastfed while taking conventional interferon beta-1a and a few with peginterferon beta-1a with no adverse infant effects reported. The Multiple Sclerosis Centre of Excellence on Reproduction and Child Health considers interferon beta to be "moderately safe" to use during breastfeeding,[2] and a French consensus group of neurologists concluded that interferon beta can be used during breastfeeding.[3] No special precautions appear to be required during breastfeeding while using peginterferon beta.
Drug Levels
Maternal Levels. Five breastfeeding women with multiple sclerosis who had weaned their infants began receiving peginterferon beta-1a subcutaneous injection at a median of 29.6 weeks postpartum. Patients collected a baseline breastmilk sample prior to treatment initiation and daily breastmilk samples on days 1 to 14 after a 125 mcg dose to measure intact peginterferon beta-1a. The peginterferon beta-1a concentration in breastmilk at baseline was below detectable levels. The highest breastmilk concentration recorded was 126.2 ng/L in one patient on day 6 after the dose. All of the other mothers had peak milk levels below 72 ng/L. Mean breast milk concentrations were 47.1, 40.9, 54.8, 65.7, 42.8, 38.2, and 27.4 ng/L on days 2, 4, 6, 8, 10, 12, and 14, respectively. Most breast milk samples had undetectable concentrations of peginterferon beta-1a (<15 mcg/L) from day 8 to day 14. The geometric mean peak concentration was 48.9 ng/L and the median time to the peak was 4 days. The mean breastmilk concentration across all study days was 35.95 ng/L. The authors estimated that a fully breastfed infant would receive a total of 0.019% of the maternal weight-adjusted dosage over a two-week dosage interval.[4]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Six women had been receiving interferon beta-1a (Avonex, Biogen) 30 mcg intramuscularly once weekly for multiple sclerosis for months to years. None of the mothers noticed any adverse effects in their breastfed infants.[5]
A woman received interferon beta-1b (Betaferon, BayerHealthCare; dosage unspecified) for multiple sclerosis throughout pregnancy. She continued the drug while she exclusively breastfed her infant. At 5 months of age, the infant was monitored regularly by a physician and was developing well with no abnormalities.[6]
One mother received interferon beta-1a for multiple sclerosis during pregnancy and postpartum. All of their infants were exclusively breastfed for 6 months and no noticeable problems were reported in any of them.[7]
In data collected from 4 countries, 17 women received interferon and 41 women received glatiramer during pregnancy and postpartum for treatment of multiple sclerosis. Of these, 63% breastfed (extent not stated) their infants for a mean of 8.8 months. No mention was made of adverse reactions in breastfed infants.[8]
Thirty-nine women with multiple sclerosis who were treated with interferon beta-1a during breastfeeding were followed by the German Multiple Sclerosis and Pregnancy Registry. During breastfeeding, the drug was administered every other day (n = 8), 3 times a week (n = 15), or once a week (n = 12). In addition, one woman receive peginterferon beta-1a every 2 weeks, and in 3 additional women, the frequency was not known. One woman received both interferon beta-1a every other day and glatiramer daily. Most infants were also exposed during pregnancy. Infants were breastfed for an average of 9.2 months (range 1.6 to 28.5 months) during interferon therapy. Infants were followed for 1 year and most developed normally; the percentages of infants with developmental delay, courses of antibiotics and hospitalizations did not differ from the reference German population. No conditions attributable to interferon beta-1a were found.[9]
A single-center study in Germany enrolled 426 women taking beta-interferon or peginterferon-beta during pregnancy who delivered 466 infants. Of these, 158 infants were breastfed, 112 exclusively until month 5 postpartum. In total, 34 of the 158 infants (21.5%) were breastfed while the mother was taking interferon. Seven infants were breastfed up to one week, 11 were breastfed over 1 week and up to 2 months, 10 were breastfed over 2 months and up to 6 months, and 6 were breastfed over 6 months and up to 12 months. In the peginterferon beta-1a group, a higher percentage stopped breastfeeding under interferon exposure within the first month after childbirth compared to the interferon beta-1a group (68.8% vs. 22.2%). Preliminary analyses did not indicate any differences in the development of weight, length, and head circumference between exposed and unexposed subgroups during breastfeeding, but the analysis was not adequately powered to reliably detect or exclude differences.[10]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
Glatiramer, Immune Globulin, Interferon Beta, Methylprednisolone
References
- 1.
- Clowse ME, Förger F, Hwang C, et al. Minimal to no transfer of certolizumab pegol into breast milk: Results from CRADLE, a prospective, postmarketing, multicentre, pharmacokinetic study. Ann Rheum Dis 2017;76:1890-6. [PMC free article: PMC5705850] [PubMed: 28814432]
- 2.
- Bove R, Alwan S, Friedman JM, et al. Management of multiple sclerosis during pregnancy and the reproductive years: A systematic review. Obstet Gynecol 2014;124:1157-68. [PubMed: 25415167]
- 3.
- Bodiguel E, Bensa C, Brassat D, et al. Multiple sclerosis and pregnancy. Rev Neurol (Paris) 2014;170:247-65. [PubMed: 24684929]
- 4.
- Houtchens M, Mahlanza T, Ciplea AI, et al. Peginterferon beta-1a concentrations in breast milk of lactating multiple sclerosis patients. Mult Scler Relat Disord 2022;60:103700. [PubMed: 35263702]
- 5.
- Hale TW, Siddiqui AA, Baker TE. Transfer of interferon beta-1a into human breastmilk. Breastfeed Med 2012;7:123-5. [PubMed: 21988602]
- 6.
- Rockhoff M, Hellwig K. Family planning and interferon (beta)-1b - A case report of successful hormonal stimulation, pregnancy and breast-feeding under interferon (beta)-1b. Aktuelle Neurologie 2012;39 (Suppl 1):S49-S51. doi:10.1055/s-0032-1304879 [CrossRef]
- 7.
- Hellwig K, Gold R. Glatiramer acetate and interferon-beta throughout gestation and postpartum in women with multiple sclerosis. J Neurol 2011;258:502-3. [PubMed: 20878174]
- 8.
- Fragoso YD, Boggild M, Macias-Islas MA, et al. The effects of long-term exposure to disease-modifying drugs during pregnancy in multiple sclerosis. Clin Neurol Neurosurg 2013;115:154-9. [PubMed: 22633835]
- 9.
- Ciplea AI, Langer-Gould A, Stahl A, et al. Safety of potential breast milk exposure to IFN-beta or glatiramer acetate: One-year infant outcomes. Neurol Neuroimmunol Neuroinflamm 2020;7:e757. [PMC free article: PMC7251509] [PubMed: 32434802]
- 10.
- Klehmet J, Begus-Nahrmann Y, Taipale K, et al. Impact of interferon beta exposure on birth outcome and child development - Results from the post-authorisation safety study PRIMA. Mult Scler Relat Disord 2023;77:104844. [PubMed: 37393802]
Substance Identification
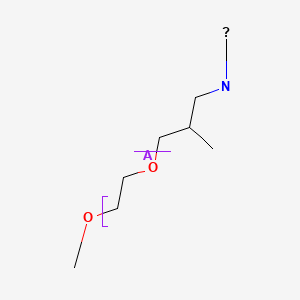
Substance Name
Peginterferon Beta
CAS Registry Number
1211327-92-2
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Peginterferon Alfa.[Drugs and Lactation Database (...]Review Peginterferon Alfa.. Drugs and Lactation Database (LactMed®). 2006
- Review Interferon Beta.[Drugs and Lactation Database (...]Review Interferon Beta.. Drugs and Lactation Database (LactMed®). 2006
- Review Polyethylene Glycol.[Drugs and Lactation Database (...]Review Polyethylene Glycol.. Drugs and Lactation Database (LactMed®). 2006
- An update on Peginterferon beta-1a Management in Multiple Sclerosis: results from an interdisciplinary Board of German and Austrian Neurologists and dermatologists.[BMC Neurol. 2019]An update on Peginterferon beta-1a Management in Multiple Sclerosis: results from an interdisciplinary Board of German and Austrian Neurologists and dermatologists.Kolb-Mäurer A, Sunderkötter C, Kukowski B, Meuth SG, members of an expert meeting. BMC Neurol. 2019 Jun 15; 19(1):130. Epub 2019 Jun 15.
- Real-world propensity score comparison of treatment effectiveness of peginterferon beta-1a vs. subcutaneous interferon beta-1a, glatiramer acetate, and teriflunomide in patients with relapsing-remitting multiple sclerosis.[Mult Scler Relat Disord. 2021]Real-world propensity score comparison of treatment effectiveness of peginterferon beta-1a vs. subcutaneous interferon beta-1a, glatiramer acetate, and teriflunomide in patients with relapsing-remitting multiple sclerosis.Reder AT, Arndt N, Roman C, Geremakis C, Mendoza JP, Su R, Makin C, Avila RL, Vignos MC. Mult Scler Relat Disord. 2021 Jun; 51:102935. Epub 2021 Apr 8.
- Peginterferon Beta - Drugs and Lactation Database (LactMed®)Peginterferon Beta - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
