Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 15078-28-1
Drug Levels and Effects
Summary of Use during Lactation
Breastmilk levels of nitroprusside sodium have not been measured after exogenous administration. Because of its short half-life of 2 minutes, it is unlikely to appear in breastmilk. However, its toxic metabolite, thiocyanate, is excreted into milk and can be directly toxic to the infant as well as inhibiting iodide transport into breastmilk. Cyanide is another toxic metabolite of nitroprusside that may enter breastmilk. An alternate drug is therefore preferred, during breastfeeding. If use of nitroprusside sodium is unavoidable, the mother should refrain from breastfeeding.
Drug Levels
Nitroprusside is converted with a half-life of about 2 minutes to cyanide and then to thiocyanate in the body. Both of these metabolites have longer half-lives: 7.3 hours for cyanide and an estimated 3 days to 2 weeks for thiocyanate.[1]
Maternal Levels. An older study found that thiocyanate passed into human breastmilk in concentrations from 27% to 50% of maternal serum levels.[2] A later study found milk levels to range from 16% to 42% of maternal plasma levels.[3] A 2004 study found values ranging from 42% to 82%,[1] while a more recent study reported fractional excretion of thiocyanate that ranged between 1.4-14.4%.[4]
Infant Levels. Relevant published information was not found as of the revision date.
Effects in Breastfed Infants
Several studies have found that breastmilk iodine levels are inversely related to the mothers' blood thiocyanate levels, probably through inhibition of the Na/I symporter by thiocyanate.[5-8] However, a recent study failed to demonstrate such a correlation. The authors felt that the effect of thiocyanate on iodine transport may be less pronounced than previously reported.[4] These low breastmilk iodine levels might pose a risk of hypothyroidism to breastfed infants whose mothers have low iodine intake.[4-8]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
Enalapril, Hydralazine, Hydrochlorothiazide, Methyldopa, Propranolol
References
- 1.
- Dorea JG. Maternal thiocyanate and thyroid status during breast-feeding. J Am Coll Nutr. 2004;23:97–101. [PubMed: 15047674]
- 2.
- Funderburk CF, Van Middlesworth L. Effect of lactation and perchlorate on thiocyanate metabolism. Am J Physiol. 1967;213:1371–7. [PubMed: 4294711]
- 3.
- Meberg A, Sande H, Foss OP, et al. Smoking during pregnancy--effects on the fetus and on thiocyanate levels in mother and baby. Acta Paediatr Scand. 1979;68:547–52. [PubMed: 463536]
- 4.
- Dasgupta PK, Kirk AB, Dyke JV, et al. Intake of iodine and perchlorate and excretion in human milk. Environ Sci Technol. 2008;42:8115–21. [PubMed: 19031911]
- 5.
- Vanderpas J, Rivera MT, Berquist H, et al. Thiocyanate overload decreases iodine supply in iodine-deficient breast-fed infants. Horm Res. 2007;68 Suppl. 3:53–4.
- 6.
- Leung AM, Braverman LE, He X, et al. Environmental perchlorate and thiocyanate exposures and infant serum thyroid function. Thyroid. 2012;22:938–43. [PMC free article: PMC3429284] [PubMed: 22827469]
- 7.
- Laurberg P, Nohr SB, Pedersen KM, et al. Iodine nutrition in breast-fed infants is impaired by maternal smoking. J Clin Endocrinol Metab. 2004;89:181–7. [PubMed: 14715847]
- 8.
- Kirk AB, Dyke JV, Martin CF, et al. Temporal patterns in perchlorate, thiocyanate, and iodide excretion in human milk. Environ Health Perspect. 2007;115:182–6. [PMC free article: PMC1817678] [PubMed: 17384762]
Substance Identification
Substance Name
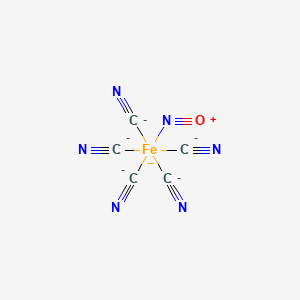
Nitroprusside
CAS Registry Number
15078-28-1
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Sodium nitroprusside-induced cyanide intoxication and prevention with sodium thiosulfate prophylaxis.[Am J Crit Care. 1992]Review Sodium nitroprusside-induced cyanide intoxication and prevention with sodium thiosulfate prophylaxis.Hall VA, Guest JM. Am J Crit Care. 1992 Sep; 1(2):19-25; quiz 26-7.
- Review Sodium Iodide I 123.[Drugs and Lactation Database (...]Review Sodium Iodide I 123.. Drugs and Lactation Database (LactMed®). 2006
- Review Clinical pharmacokinetics of nitroprusside, cyanide, thiosulphate and thiocyanate.[Clin Pharmacokinet. 1984]Review Clinical pharmacokinetics of nitroprusside, cyanide, thiosulphate and thiocyanate.Schulz V. Clin Pharmacokinet. 1984 May-Jun; 9(3):239-51.
- Monitoring cyanide and thiocyanate concentrations during infusion of sodium nitroprusside in children.[Pediatr Cardiol. 1991]Monitoring cyanide and thiocyanate concentrations during infusion of sodium nitroprusside in children.Linakis JG, Lacouture PG, Woolf A. Pediatr Cardiol. 1991 Oct; 12(4):214-8.
- Some aspects of sodium nitroprusside reaction with human erythrocytes.[Clin Chem. 1977]Some aspects of sodium nitroprusside reaction with human erythrocytes.Spiegel HE, Kucera V. Clin Chem. 1977 Dec; 23(12):2329-31.
- Nitroprusside - Drugs and Lactation Database (LactMed®)Nitroprusside - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
