NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Evans I, Thornton H, Chalmers I, et al. Testing Treatments: Better Research for Better Healthcare. 2nd edition. London: Pinter & Martin; 2011.

Testing Treatments: Better Research for Better Healthcare. 2nd edition.
Show detailsIn the preceding chapters we have drawn together many examples to illustrate why treatments can – and should – be based on sound research designed to address questions that are important to patients. Whether we are members of the general public, patients, or healthcare professionals, the effects of treatments touch the lives of all of us one way or another. Robust evidence from fair testing of treatments really does matter.
In this chapter we look at how such evidence can shape the practice of healthcare so that decisions about the treatment of individuals can be reached jointly by clinicians and patients. Good decisions should be informed by good evidence, which will tell us about the likely consequences of different treatment options. However, the meaning and value of those consequences will be different for different individuals. So, using the same evidence, one individual may reach a different decision from another. For example, a fully functioning finger may mean a lot more to a professional musician, a good sense of smell to a chef, and good eyesight to a photographer than they would to other people. They may therefore be prepared to make greater efforts or take greater risks to achieve the result that matters to them. The interface between evidence and decisions is complex, so most of this chapter will address some common questions on this issue.
However, before that, we consider ‘shared decision making’ more closely and illustrate what it might look like in practice. Sharing decisions in this way steers a middle course between professional paternalism and abandoning patients to make up their own minds alone. Patients regularly complain about lack of information yet, quite naturally, they have different expectations of the responsibility they want to accept.1, 2
SHARED DECISION-MAKING
‘Shared decision-making has been defined as “the process of involving patients in clinical decisions”. The ethos is one where professionals (should) work to define problems with sufficient clarity and openness so that patients can comprehend the uncertainties that surround most decisions in medicine and therefore appreciate that choices have to be made between competing options. The clinician’s expertise lies in diagnosing and identifying treatment options according to clinical priorities; the patient’s role is to identify and communicate their informed values and personal priorities, as shaped by their social circumstances.’
Adapted from Thornton H. Evidence-based healthcare. What roles for patients? In: Edwards A, Elwyn G, eds. Shared decision-making in health care. Achieving evidence-based patient choice. Second edition. Oxford: Oxford University Press, 2009, p39.
Some patients prefer not to have detailed information about their illness and treatment options and would rather leave things entirely to their professional advisers, but many are keen to learn more. For those who would like more information, there should be ready access to well-written material and to skilled health professionals who can advise how and where they can access it in a format that best suits them.
What constitutes an ‘ideal consultation’ can differ widely from one person to the next. Some people are content to adopt a dependent role while others prefer to lead. A more participatory role in coming to a decision – with the doctor’s encouragement – can be the most rewarding approach and can become the preferred option once a patient experiences how this works. A simple question from a patient can open up the dialogue, as we illustrate below. Importantly, patients can be led to feel involved in their care when they are treated as equal partners, whatever the level of involvement.
WHAT MIGHT THE IDEAS IN THIS BOOK LOOK LIKE FOR YOU?
Although no two consultations are identical, the guiding principles for how to arrive at the best possible decision, as set out in this book, are the same. The goal is that both patient and health professional leave the consultation feeling satisfied that they have worked things through together in the light of the best available relevant evidence. Patients consult their doctors with a wide range of health problems – some short term; some long-term; some life-threatening; others just ‘troublesome’. Their personal circumstances will be infinitely variable, but they will all have questions that need to be addressed so that they can decide what to do.
To illustrate this, we begin with a consultation between patient and doctor concerning a common problem: osteoarthritis (‘wear and tear’ arthritis) of the knees. We then go on to address some fundamental questions about using research evidence to inform practice – questions that patients with a wide variety of conditions might want answered when they consult a health professional, and those that readers of this book might well pose after reading earlier chapters.
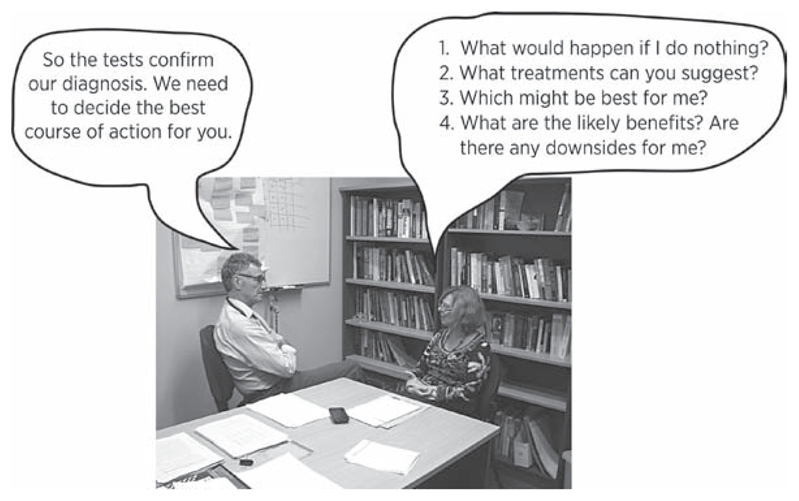
Dialogue between doctor and patient and some questions to ask
SHARED DECISION-MAKING: A CONSULTATION FOR A COMMON CONDITION
Doctor:
Well, you have moderate osteoarthritis of the knees, which is common as people get older. It’s often referred to as ‘wear-and-tear-arthritis’. The usual course is for this condition to fluctuate – get better or worse – but with a slow progression over the years or decades. How is it currently troubling you?
Patient:
Well, if I overdo things, my knees get quite painful and can stay that way for hours and make sleeping difficult. Recently, the pain has got worse, and I was worried I would need a knee replacement.
Doctor:
Knee replacement is certainly an option but we usually reserve that for when simpler measures have failed.
Patient:
So what else can you suggest?
Doctor:
Well, simple analgesics or anti-inflammatory drugs can help manage the pain. Other than drugs, some special exercises to strengthen the muscles around the knee can help maintain function and decrease the pain. Would you like to know more about those?
Patient:
Those drugs upset my stomach, so I’d like to hear more about the exercises.
Doctor:
Fine. I’ll give you a handout that explains some of the exercises, but also get you to see our physiotherapist. Meanwhile, you can safely take paracetamol regularly for the pain and stay active.
Patient:
That’s helpful, but aren’t there more treatment options?
Doctor:
There are further options available for severe osteoarthritis. But at this stage you could well find that you will experience a steady improvement as you build up the muscles with the exercises, sleep better because you have less pain, and can generally do more. You might also consider going swimming, or walking the dog more often, which will not only strengthen the muscles but should also help you ‘feel good’, and help to keep your weight in check into the bargain! I think we can safely leave considering more drastic options until we see how you get on with the exercises and the pain relief. But don’t hesitate to come back to me if you think you’re disappointed with progress.
QUESTIONS ABOUT TRANSLATING RESEARCH EVIDENCE INTO PRACTICE
Question 1. Isn’t anything worth trying when a patient has a life-threatening condition?
It can be tempting to want to try the latest ‘wonder-drug’, or follow the example of some high-profile celebrity who has made claims in the popular press about a treatment regimen that they’ve followed, perhaps involving ‘alternative’ medicine that has been well-marketed but not tested. Mainstream treatments can seem much less glamorous and promising, but most that are being used for life-threatening conditions will have been painstakingly tested to find out how effective and how safe they are. So, seeking out the best evidence at the start can save much time, heartache, and money.
Mainstream medicine, generally speaking, recognizes that there are degrees of uncertainty about the effectiveness and safety of the medicines on offer. It aims to reduce those uncertainties to an acceptable level by testing, and by constantly and systematically reviewing the evidence to improve the treatments on offer. Such improvements depend critically on the help of patients who come to see that this is the only way to make solid progress.
Understandably, patients with life-threatening conditions can be desperate to try anything, including untested ‘treatments’. But it is far better for them to consider enrolling in a suitable clinical trial in which a new treatment is being compared with the current best treatment. Such a comparison will not only reveal what extra benefits the new treatment might bring, but also what harms it might cause. Life-threatening conditions can need powerful treatments – and there is no treatment that does not have some side-effects. This makes it all the more important that a new treatment is tested thoroughly and fairly so that the findings can be recorded in a systematic way to see whether it is really likely to help patients.
Question 2. Although patients might want to know if a treatment ‘works’, suppose they don’t want all the details?
It is important to strike a balance between information overload and depriving people of enough information to help them make an adequately informed choice. It is equally important to remember that a person may well need some information initially and more later on as they weigh the pros and cons needed to reach a decision. During a consultation, both doctor and patient should feel satisfied that the patient has the amount of information needed to go ahead and select, with the doctor, what the current best course of action is. But it doesn’t stop there. If, after spending more time thinking about things, the patient has more questions and wants more details, the doctor should help the patient find out what they might want to know, and help clarify anything that is unclear.
Some choices involve difficult trade-offs; it may come down to choosing the lesser of two evils. For example, in Chapter 4 we discussed aortic aneurysm – the enlargement of the main artery from the heart – which may develop fatal leaks. Major surgery can correct the problem, but one or two patients per 100 will die from the operation itself. So there is a trade-off between the early mortality of the operation against the later risk of fatal rupture. Long term, an operation is the better bet, but some patients may reasonably choose not to opt for surgery, or at least delay it until after an important event such as their daughter’s wedding. So rather than diving blind into an ‘only hope’ solution, it is better to weigh up the risks and their possible timing.
Question 3. Statistics are confusing – should patients really have to look at the numbers?
The way that numbers are presented can be very daunting – or even downright misleading. But if you really do want to compare one treatment with another, or to find out more about how the condition you have affects others like you, numbers always come into it somewhere. But some ways of presenting numbers are more helpful than others.
The best way to make the numbers mean something for lay people (and doctors too!) is to use frequencies. That means using whole numbers. So, saying 15 people out of a hundred is generally preferable to saying 15%. Then it is often helpful to give the numbers not only in words but also in graphic form of some kind – for example, coloured bar charts; pie charts; pin men/ smiley and sad faces in boxes, etc; and also in tables. Presenting ‘numbers’ with these ‘decision aids’ means that as many people as possible can grasp what the data mean.
Here is one way of explaining the effect of blood pressure drugs on the risk of heart disease and stroke in patients with high blood pressure over a period of ten years, using a bar chart.3

What will happen to 100 people like you in the next 10 years?
Out of 100 people with high blood pressure not taking any treatment, in the next ten years, 13 would be expected to get heart disease or have a stroke. If all 100 people took blood pressure drug A, only 11 of them would get heart disease or have a stroke – and two of them would avoid getting heart disease or having a stroke. If all 100 had taken blood pressure drug B, then ten would get heart disease or have a stroke and three would avoid getting heart disease or having a stroke. That’s straightforward. Yet these simple numbers are often reported in terms only intelligible to statisticians.
Now let’s look at how the numbers work out using a table rather than a bar chart. In this example we will concentrate on the better treatment – drug B:
Let’s put the numbers into natural frequencies (simple counts) first, then work it through.
| NO TREATMENT | WITH DRUG B | |
|---|---|---|
| Heart disease or stroke (over 10 years) | 13 out of 100 people | 10 out of 100 people |
| No heart disease or stroke | 87 out of 100 people | 90 out of 100 people |
| TOTAL | 100 | 100 |
With no treatment, the risk of heart disease or stroke is 13% (or 13 out of 100), whereas with drug B the risk is 10% (or 10 out of 100) – a difference of 3% (or 3 out of 100). Since drug B prevents 3 of the 13 instances of heart disease or stroke that would have occurred, that is a relative risk reduction of 3/13 or about 23%. So we can say there was a 3% absolute risk reduction with treatment, or a 23% relative risk reduction. These are two different ways of expressing the same thing.
The relative risk reduction is always a high number – and sometimes a lot higher – and therefore is more attention grabbing. So if you see a headline saying ‘23% of strokes avoided’ it tells you nothing – because it does not state the specific group of people affected, the timespan, or, most importantly, the risk of stroke without any treatment. It is most likely to be the relative risk reduction (but you need to check).
The numbers are sometimes very different. Consider the way a newspaper reported a study of prostate cancer screening. ‘Could cut deaths by 20%’ sounds large. The results could also have been expressed as one death prevented per 1,410 people screened (or a minuscule 0.07%, that is, seven premature deaths prevented per ten thousand men screened). The 20% is the relative risk reduction, the 0.07% the absolute risk reduction. The latter is much smaller, because of the low rate of death from prostate cancer – and unlikely to have grabbed the headlines. The bottom line is that if a headline claim sounds overly optimistic it probably is!4
DON’T BE FOOLED BY EYE-CATCHING STATISTICS
‘Let’s say the risk of having a heart attack in your fifties is 50 per cent higher if you have a high cholesterol. That sounds pretty bad. Let’s say the extra risk of having a heart attack if you have a high cholesterol is only 2 per cent. That sounds OK to me. But they’re the same (hypothetical figures). Let’s try this. Out of a hundred men in their fifties with normal cholesterol, four will be expected to have a heart attack; whereas out of a hundred men with high cholesterol, six will be expected to have a heart attack. That’s two extra heart attacks per hundred.’
Goldacre B. Bad Science. London: Fourth Estate 2008, pp239–40.
So numbers do matter, and presented well can help people make decisions. Patients should not hesitate to ask their doctor to explain results in a way that they can readily understand – with visual materials for clarity as necessary. If decisions about treatments are to be shared, both doctors and patients need to be clear about what the numbers actually mean.
Question 4. How can someone know that the research evidence applies to them?
All decisions rely on previous experience of some kind – individual or collective. Fair tests of treatments such as randomized trials are simply well organized versions of that experience designed to minimize biases. Well organized or not, there will always be some uncertainty about how well previous experience can shape our advice for the next person. So if the patients who had been studied in the fair tests had a similar condition, at a similar stage or severity, to the individual in question, the most reasonable assumption is that the individual would get a similar response, unless there was a good reason to think they or their condition were substantially different.
Of course, even if the evidence is applicable, a patient might reasonably ask: ‘people are all different so surely they may respond differently?’ The ‘fair test’ of a treatment will only tell us what works on average, but rarely guarantees it will work equally well in everyone; and it cannot usually predict who will suffer unwanted side-effects. Research evidence can be used to guide what treatment is likely to be best, and then tried in an individual. With some skin rashes, for example, evidence-based treatment could be applied to one area of the body, using another area as a control (see Chapter 6, p74). By comparing responses in the two areas, both doctor and patient can tell whether it works, or whether there is an adverse effect. Indeed it’s common to try a ‘test patch’ when first using some skin treatments, such as acne treatments on the face.
Mostly, however, we don’t have the convenience of such a straightforward comparison. For some chronic and non-life-threatening problems, such as pain or itch, it is possible to try repeated periods on and off a drug in the same patient. This approach is also called an n-of-1 trial, meaning that the number (n) of participants in the trial is one – a single patient. With such tests in individual patients, the principles for a fair comparison that we outlined in Chapter 6 still apply, including an unbiased or blinded assessment of outcome, etc. Ideally, then, we would use placebo controls of skin treatments or pills, but this is often difficult to organize.
For many conditions, however, we cannot ‘try it and see’: the outcome is too remote or too uncertain. For example, it is impossible to know whether aspirin will prevent a patient’s stroke until it is too late. This is a problem in most cases of preventive medicine, and also with treatments for many acute conditions, such as meningitis, pneumonia or snake bite, where we don’t have the opportunity to test it in each individual patient and see. So we then have to rely on whether and how to apply the evidence from the experience of studying others.
In practice, if we are happy the evidence applies, it is then important to ask how the severity of the condition in the patient (or the predicted level of risk in those who are still well) compares with that of the people in the studies. In general, patients with more severe illness have more to gain from treatment. So if severity is equal to or greater than those in studies that showed a treatment to be beneficial, we can generally be confident about the applicability of the evidence. If their illness is less severe (or if still well, they are at relatively low predicted risk) the key issue is whether a smaller benefit than that seen in the studies might still be considered worthwhile.
Question 5. Won’t genetic testing – and ‘personalized medicine’ – mean doctors can work out the specific treatment needed in every individual and make all this unnecessary?
Although the idea of being able to work out the specific treatment needed in every individual is undoubtedly attractive, and may be possible for a few conditions, it seems very unlikely that this approach will become the main way of treating people. As we explained when discussing genetic tests in Chapter 4 (p43–44) most diseases depend not only on complex interactions involving several genes, but also on the even more complex interactions between genes and environmental factors.
The results of genetic analyses have been important in informing decisions in families and individuals with inherited disorders, such as Huntington’s disease, thalassaemias (inherited blood disorders), and some other (mostly rare) diseases. This genetic information has been a great boon in counselling families with these conditions. However, as far as the more common diseases to which we are all subject are concerned, genetic analysis adds little to information already available from family history and clinical examination. Although this situation is likely to change, our limited current knowledge means that we need to be careful not to overinterpret risks for common diseases predicted on the basis of genetic analysis.
We should declare that none of the authors have had their genetic profiles done, nor are we considering doing so. So it shouldn’t surprise you that we would generally advise against genetic testing unless someone has (i) a family history that suggests a specific known genetic disorder, or (ii) one of the few currently known conditions in which a gene or genes clearly predicts who will respond to a treatment.
Question 6. If someone has a condition that is being studied in an ongoing clinical trial, how do they find out about this if their doctor doesn’t know about it? (See also Additional Resources)
Fewer than one in 100 people seeing a doctor will be enrolled in a clinical trial. The proportion varies widely by condition and setting. Even within cancer centres – where trials are widely accepted and used – the range is enormous: most children with cancer are enrolled in trials, but fewer than one in ten adults are. Most trial enrolment depends on the centre a patient is attending: if the centre is not involved in the trial then they won’t be able to enrol patients. So patients might need to look for a centre that is involved in clinical trials. There are a few community-based trials where patients can enrol directly; for example, these often occur in research designed to find out how to help people with mental health problems, such as depression or anxiety. More recently, some other trials have enrolled people directly through the internet. For example, a recent study to assess the effects of stretching before exercise enrolled all participants in this way: they never attended a clinic, but received all their instructions and follow-up over the internet.
If their doctors seem reluctant to enrol patients in trials, patients should find out why. It may be that the patient is not really eligible, for example. However, it may be simply that the doctor is put off by the extra work imposed by the burdensome regulatory demands (see Chapter 9). Patients who believe that they are likely to be eligible for participation in ongoing trials should persist. If a suitable trial is known to exist and a patient makes it clear that they are keen to be enrolled, doctors should support this.
Question 7. What’s the best way of telling if the evidence (on the web or elsewhere) is reliable? What should people look out for?
Unfortunately there is no completely reliable simple marker for reliable information. If you are not going to look at the original research yourself, you are putting your trust in someone else’s assessment. So it is important to assess the likely competence of that person (or organization) and to note whether there is a conflict of interest (or an axe to grind). If not, then ask yourself whether you trust them to have found and assessed the best research: is it described and referenced?
For example, suppose someone wanted to know whether beta-carotene (related to Vitamin A) increases or decreases the risk of cancer. A Google search for ‘beta-carotene cancer’ brings over 800,000 results. Looking at the first ten there are four primary research studies and six that are reviews or opinions. Of those six, there are three that have advertisements for vitamins or alternative medicines on the same page: a worrying sign.
One of these poorer websites says:
‘Question: Does beta-carotene prevent cancer? Answer: Studies have shown that beta-carotene can help reduce the risk of cancer. Beta-carotene can be found in yellow, red, and deep green vegetables. It is also found in fruits. It is a common belief that taking a beta-carotene supplement will have the same effect as eating fruits and vegetables that contain it. However, this is not the case. Studies found an increased lung cancer risk among study participants.’
In addition to the advertisements, ‘studies’ are mentioned but with no description of them or references to published studies – that is a warning sign. It is impossible to tell whether or not the writer has searched for and appraised the ‘studies’ or merely stumbled on ones where he or she liked the conclusions.
Contrast this with the Wikipedia entry (also in the first ten):
‘A review of all randomized controlled trials in the scientific literature by the Cochrane Collaboration published in JAMA in 2007 found that β-carotene increased mortality by something between 1 and 8% (Relative Risk 1.05, 95% confidence interval 1.01–1.08).[15] However, this meta-analysis included two large studies of smokers, so it is not clear that the results apply to the general population.[16]’
This entry states the type of evidence (randomized trials), and gives the references (the numbers in the square brackets). So, the fact that there are no advertisements, and there are specific details about the evidence, is reassuring.
Question 8. Are there reliable sources of information that can be recommended? (See also Additional Resources)
There is no single information source for all diseases and treatments. To apply the principles in this book, readers may want to develop some skills themselves. For example, in addition to Chapters 6–8 in this book, the book Smart Health Choices5 gives some tips on how to find good information, and what to check for.
Of the websites available, few are largely based on systematic reviews. Some that are include the Cochrane Database of Systematic Reviews (www.cochrane.org/cochrane-reviews), which has lay summaries, and the IQWIG website (in German, but also translated into English at www.informedhealthonline.org). In addition, there are many websites that generally provide good information but are not always based on systematic reviews of the best available evidence – for example, NHS Choices (www.nhs.uk) and PubMed Health (www.pubmed.gov/health) both provide high-quality information.
Of course, there is also a lot to be wary of. In particular, watch out for conflicts of interest, such as sites that might financially benefit from people believing the information or others that try to sell something. This can be hard to detect, however – for example, as we mentioned in Chapter 11, some patient groups have undeclared funding from pharmaceutical companies and that can taint the information provided.
Question 9. How should people avoid being ‘labelled’ with an ‘illness’ and getting unnecessary treatments?
Medicine has made amazing advances: vaccines and antibiotics for preventing and treating infections; joint replacements; cataract surgery; and treatment of childhood cancers, to name but a few. But that success encourages medicine to extend its reach to areas of less benefit. To a person with a hammer, the whole world looks like a nail; and to a doctor (or a drug company!) with a new treatment everything looks like an illness. For example, as better treatments for diabetes and high blood pressure have become available, the temptation is for doctors to suggest their use to patients with only slightly abnormal results. This dramatically increases the number of people labelled as diabetic or hypertensive, ‘medicalizing’ many people who once would have been classed as normal.
In addition to any adverse effects of (sometimes unnecessary) treatment, this ‘labelling’ has both psychological and social consequences, which can affect a person’s sense of well being, as well as creating problems with employment or insurance. So it is important for patients and the public to recognize this chain of events; to pause and consider the likely balance of harms and benefits before too hastily agreeing to a treatment. As we discussed in Chapter 4, screening commonly causes these problems of labelling through overdiagnosis, and potential overtreatment.
The first defence is to be wary of labels and proposed further investigations. The seemingly flippant remark that a normal person is someone who has not been investigated enough has a very serious side to it. So it is always wise to ask whether the illness is considered high or low risk. And, as we suggested earlier, also to ask what would happen if nothing immediate was done: how might the condition be monitored, and what would be the signal for action? Some doctors are relieved that patients don’t want immediate treatment or tests. But other doctors fall into the labelling trap – label = disease = mandatory treatment – not realizing that the patient may be quite happy to wait and see if the problem gets better or worse by itself.
WHO HAS DIABETES?
So how do we decide who has diabetes? When I was in medical school, our numerical rule was this: if you had a fasting blood sugar over 140, then you had diabetes. But in 1997 the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus redefined the disorder. Now if you have a fasting blood sugar over 126, you have diabetes. So everyone who has a blood sugar between 126 and 140 used to be normal but now has diabetes. That little change turned over 1.6 million people into patients.
Is that a problem? Maybe, maybe not. Because we changed the rules, we now treat more patients for diabetes. That may mean we have lowered the chance of diabetic complications for some of these new patients. But because these patients have milder diabetes (relatively low blood sugars between 126 and 140), they are at relatively low risk of these complications to begin with.
Welch HG, Schwartz LM, Woloshin S. Overdiagnosed: making people sick in the pursuit of health. Boston: Beacon Press, 2011: p17–18.
WHERE DO WE GO FROM HERE?
The issues discussed above – about individual concerns and values, about understanding statistics and how they apply to individuals, and about the concerns of extending effective treatments to increasingly milder degrees of disease – all speak to a need for better communication between patient and doctor, and between the health sector and the citizens it serves. So we will finish this chapter with the Salzburg Statement on shared decision making, which sets out an agenda for different groups to improve how we work together.6, 7
Salzburg statement on shared decision making
We call on clinicians to:
- Recognize that they have an ethical imperative to share important decisions with patients
- Stimulate a two way flow of information and encourage patients to ask questions, explain their circumstances, and express their personal preferences
- Provide accurate information about options and the uncertainties, benefits, and harms of treatment in line with best practice for risk communication
- Tailor information to individual patient needs and allow them sufficient time to consider their options
- Acknowledge that most decisions do not have to be taken immediately, and give patients and their families the resources and help to reach decisions
We call on clinicians, researchers, editors, journalists, and others to:
- Ensure that the information they provide is clear, evidence based, and up to date and that conflicts of interest are declared
We call on patients to:
- Speak up about their concerns, questions, and what’s important to them
- Recognize that they have a right to be equal participants in their care
- Seek and use high quality health information
We call on policy makers to:
- Adopt policies that encourage shared decision making, including its measurement, as a stimulus for improvement
- Amend informed consent laws to support the development of skills and tools for shared decision making
Why
- Much of the care patients receive is based on the ability and readiness of individual clinicians to provide it, rather than on widely agreed standards of best practice or patients’ preferences for treatment
- Clinicians are often slow to recognize the extent to which patients wish to be involved in understanding their health problems, in knowing the options available to them, and in making decisions that take account of their personal preferences
- Many patients and their families find it difficult to take an active part in healthcare decisions. Some lack the confidence to question health professionals. Many have only a limited understanding about health and its determinants and do not know where to find information that is clear, trustworthy, and easy to understand
- So what makes for better healthcare? - Testing TreatmentsSo what makes for better healthcare? - Testing Treatments
- CLN6 CLN6 transmembrane ER protein [Homo sapiens]CLN6 CLN6 transmembrane ER protein [Homo sapiens]Gene ID:54982Gene
- Gene Links for GEO Profiles (Select 117435885) (1)Gene
- Related DataSets for GEO Profiles (Select 117435886) (1)GEO DataSets
- Long-term adult survivors of glioblastoma: primary tumorsLong-term adult survivors of glioblastoma: primary tumorsAccession: GDS5205GEO DataSets
Your browsing activity is empty.
Activity recording is turned off.
See more...