NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Center for Substance Abuse Treatment. A Guide to Substance Abuse Services for Primary Care Clinicians. Rockville (MD): Substance Abuse and Mental Health Services Administration (US); 1997. (Treatment Improvement Protocol (TIP) Series, No. 24.)
A Guide to Substance Abuse Services for Primary Care Clinicians.
Show details
Unlike brief intervention, in-depth substance abuse assessment requires specialized skills and consumes a substantial amount of time -- anywhere from 90 minutes to 2 hours. As a result, many primary care clinicians will refer patients suspected of having a substance abuse problem to specialists for both assessment and treatment, although clinicians in underserved areas or with expertise in substance abuse may assume partial or total responsibility for this function. However, even clinicians who will not perform substance abuse assessments should have a basic understanding of their elements and objectives so that they can
- Initiate appropriate referrals
- Participate effectively as a member of the treatment team, if required
- Better fulfill the gatekeepers' monitoring responsibility with respect to patient progress
- Carry out needed case management functions as appropriate
Throughout this chapter, assessment will refer to in-depth assessment as distinct from the postscreening brief assessment discussed in Chapter 3.
Assessment Parameters
Substance abuse assessment is the further investigation of patients (1) whose positive screening results indicate that substance abuse is likely and (2) whose responses to the questions in a brief assessment (see Chapter 3) suggest that compulsion to use, impaired control, presence of other psychosocial problems, or absence of social support will render brief intervention ineffective (College of Family Physicians of Canada, 1994). Information gained through an assessment will clarify the type and extent of the problem and will help determine the appropriate treatment response. Assessment
- Examines problems related to use (e.g., medical, behavioral, social, and financial)
- Provides data for a formal diagnosis of a possible problem
- Establishes the severity of an identified problem (i.e., mild, moderate, intermediate, or severe stage)
- Helps to determine appropriate level of care
- Guides treatment planning (e.g., whether specialized care is needed, components of an appropriate referral, and eligibility for services)
- Defines a baseline of the patient's status to which future conditions can be compared (National Institute on Alcohol Abuse and Alcoholism, 1995a)
If one thinks of screening as triage, then assessment is acquiring the information needed to direct a patient to appropriate treatment. At a minimum, patients must be assessed for
- Acute intoxication and/or withdrawal potential
- Biomedical conditions and complications
- Emotional/behavioral conditions (e.g., psychiatric conditions, psychological or emotional/behavioral complications of known or unknown origin, poor impulse control, changes in mental status, or transient neuropsychiatric complications)
- Treatment acceptance or resistance
- Relapse potential or continued use potential
- Recovery/living environment (American Society of Addiction Medicine, 1996, p. 6)
Assessing along these dimensions helps the assessor confirm that a substance abuse problem exists and recommend an appropriate level of care (see Chapter 5 for a discussion of substance abuse treatment systems and processes). Through a combination of clinical interview, personal history-taking, and self-reports, supplemented by laboratory testing and collateral reports as appropriate, the assessment process identifies patients' health problems, interest in and readiness for treatment, and feasible treatment options. It also provides information on a patient's familial, educational, social, and vocational supports and deficits. Like screening, assessment may be a recurring event if clinical evidence indicates the need.
Who Should Assess?
Professional position is less important than specific training for performing accurate assessments. Where possible, the Consensus Panel recommends referring patients to an experienced substance abuse specialist for intensive assessment. If referral is not possible, the Panel believes that physicians, physician assistants, and advanced practice nurses (nurse practitioners and clinical nurse specialists) with experience in empathic motivational interviewing may perform intensive assessments after receiving training in
- The signs and symptoms of substance abuse
- The biopsychosocial effects of alcohol and other drugs and likely progression of the disease
- Common comorbid conditions and medical consequences of abuse
- The terms used in the classification system of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) (American Psychiatric Association, 1994a), their interpretation, and their relationship to the findings that emerged during the assessment history
- The appropriate use, scoring, and interpretation of standardized assessment instruments
Understanding the Impact Of Culture and Gender
Clinicians performing in-depth assessments should also understand how patients' gender and cultural background bear on the characteristics and severity of the disease (Spector, 1996). For example, more males than females abuse alcohol and drugs, and older women are more likely than older men to abuse prescription drugs. Culture and gender also may influence patients' recognition of their problems (e.g., local cultural norms may condone or accept male drunkenness) and their reaction to the assessment process and recommended treatment interventions (e.g., substantial stigma may be associated with substance abuse treatment, especially for women and older patients of either sex). Assessors also should be aware of the influence of their own gender and cultural background on their response to patients with suspected substance abuse problems and on their interpretation of the information provided through the assessment process. While an understanding of "typical" patterns is useful in anticipating problem areas, experienced assessors resist the temptation to stereotype patients and subsume them within broad categories based on language, ethnicity, age, education, and appearance. An oft-repeated anecdote illustrating the dangers of stereotyping concerns a well-dressed, middle-aged woman and her disheveled teenage son seen in an emergency room following a car accident. The young man was screened for substance abuse; the mother was not. Several hours after admission, the woman went into alcohol withdrawal.
When referring patients for assessment, primary care clinicians should consider whether a particular patient will relate more readily to a male or female assessor of similar cultural background or if a patient who speaks English as a second language will respond more easily to questions posed in his native tongue (Spector, 1996).
Knowledge of Comorbid Mental Disorders
The relationship between mental disorders and substance use disorders is variable and complicated. The Substance Abuse and Mental Health Services Administration (SAMHSA) reports that, in the general population, 4.7 to 13.7 percent of individuals between the ages of 15 and 54 may have both a mental disorder and a substance abuse or dependence problem (Substance Abuse and Mental Health Services Administration, 1995). Intoxication with a drug can produce psychiatric symptoms that subside with abstinence, but for those with a mental illness, substance use may mask, exacerbate, or be used to ameliorate psychiatric symptoms; precipitate psychological decompensation; or increase the frequency with which individuals require hospitalization. Because substance abuse disorders often manifest symptoms similar to those of mental health disorders, misdiagnosis may occur.
Inadvertent bias may affect the assessment process when performed by addiction specialists who do not recognize or accept the role of mental disorders in prompting or sustaining substance use or who have no experience with dually diagnosed patients. Conversely, some mental health practitioners dismiss substance abuse as merely symptomatic of underlying mental health disorders and do not acknowledge it as a problem requiring specific attention. While screening results, per se, do little to illuminate comorbid mental health disorders, information gleaned through a patient's history or inability to respond to brief intervention may suggest a mental health problem. If possible, primary care clinicians should refer patients to assessors who understand and are trained in mental health as well as substance abuse assessment and who are willing and able to expand the assessment process as needed to identify the multiple dimensions that may be contributing to a patient's problems (Institute of Medicine, 1990).
Whether referring for or conducting intensive assessments themselves, primary care clinicians also should be alert to the possibility of conflict of interest when assessors are linked to a program or practice providing substance abuse services. There may be financial incentives (e.g., fee-for-service arrangements) or ideological pressure to interpret assessment results in such a way as to steer patients to a particular program or treatment provider (Institute of Medicine, 1990). Aside from insisting on an independent assessment source, which may be impractical, clinicians have few options for ensuring objective assessments (Institute of Medicine, 1990). However, primary care providers who understand the purposes of assessment and are familiar with its components will be in a better position to identify and subsequently avoid biased assessors.
The Assessment Setting
Like screening, assessments must be conducted in private, and patients must be assured that the information they provide is confidential. Patients often will not reveal information about drug or alcohol use because they fear that information will be shared with their family members or employers or be used against them by law enforcement agencies or health insurance organizations. Prior to conducting an assessment, assessors should review current legal protections with the patient and discuss the limitations that apply to sharing information. (See Appendix B for a detailed discussion of confidentiality as it pertains to substance abuse.)
Assessment Components
Assessment comprises a medical and psychological history along with family, social, sexual, and drug use histories and a physical examination. (The physical examination and the interviews to obtain histories may be split, with a primary care clinician performing the physical and a nonmedical substance abuse specialist conducting the interviews. When this occurs, close collaboration between the two providers is essential.) In its 1990 report, Broadening the Base of Treatment for Alcohol Problems, the Institute of Medicine recommended conducting "sequential" and "multidimensional" assessments for alcohol problems (Institute of Medicine, 1990). The Consensus Panel recommends the same approach when assessing for other drug-related problems. Essentially, sequential assessment entails separating "the process of assessment into a series of stages, each of which may or may not lead into the next stage" (Institute of Medicine, 1990, p. 249; Skinner, 1981) depending on the information obtained previously. In this model, a broad-based assessment is conducted first. If the information compiled suggests that other problems may be present, such as a psychiatric disorder, then a series of progressively more intense procedures would be initiated to confirm and characterize that finding. This approach not only provides information needed for treatment planning, it saves both patient and assessor time. Moreover, by ensuring that "further information is necessary [it also] justifies its increased cost" (adapted from Skinner, 1981, in Institute of Medicine, 1990, p. 250).
A multidimensional approach to assessment ensures that the variety of factors that impinge on an individual's substance abuse (level, pattern, and history of use; signs and symptoms of use; and consequences of use) are considered when evaluating individual patient problems and recommending treatment (Institute of Medicine, 1990). Detailed characterization not only helps assessors match patients to appropriate available services, it also provides information useful in anticipating relapse triggers and planning for relapse management (see Chapter 5).
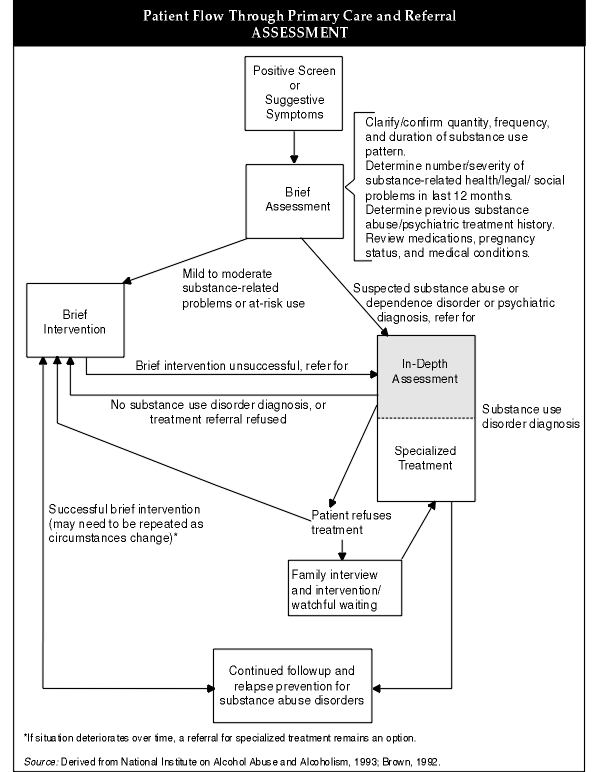
A number of assessment instruments elicit similar information (see Appendix C), and specialized substance abuse treatment assessors may use one or more with patients. Administering an instrument can take from 90 minutes to 2 hours, depending on the instrument(s). Training is frequently required, and costs for purchase and required staff time can be substantial. While primary care clinicians trained or experienced in addiction medicine may use the instruments described in the appendix, many clinicians will not because they lack the time, training, and resources to do so. Based on members' clinical experience, the Consensus Panel recommends that an assessment include at least the components presented in Figure 4-1.
The figure also includes additional questions on certain sensitive topics for situations in which primary care clinicians cannot refer for specialized assessment and require additional information in order to make a reasonable decision about the need for formal substance abuse treatment. In addition to the elements listed under the Mental Health History component in Figure 4-1, primary care clinicians contemplating a possible referral for treatment should evaluate level of cognition because it is such an important measure of a patient's ability to participate in treatment. Results of a mental status examination can support diagnoses of intoxication, withdrawal, depression, and suicidal tendencies and signal the possibility of psychosis and organic states such as dementia.
Assessment Instruments
Assessment instruments assist in gathering consistent information, clarifying and elaborating on information obtained through the patient history and physical examination, and establishing a baseline against which patient progress can be monitored. Instruments are not a substitute for clinical judgment, but the uniformity they introduce to the assessment process helps to ensure that key areas are not overlooked (Institute of Medicine, 1990). Standardized tools have already been tested for reliability and validity and offer assessors ready-made and carefully sequenced questions that are easy to use in patient interviews and relatively simple to score (National Institute on Drug Abuse, 1994). Some instruments can be self-administered, are available in multiple languages, are computerized, and are in the public domain. However, many require that those administering them be trained in their use.
Although the Consensus Panel does not recommend the use of assessment instruments in the primary care setting because of the time, training, and resources required to administer them properly, clinician members of the Panel with training in addiction medicine have had experience with a number of standardized assessment tools and found them effective. Appendix C describes selected assessment instruments and provides information on ordering them. Clinicians interested in reviewing instruments for possible use with their patients should consider
- The literacy levels required to take them
- Whether instruments can be easily administered to patients with language or comprehension problems
- If the questions are both appropriate for and sensitive to the kinds of problems encountered in primary care
- Whether the time and costs involved are reasonable (National Institute on Drug Abuse, 1994)
Supplementing Assessment Results
Collateral reports and laboratory tests are tools used to supplement and, in some cases, augment the information obtained during the intensive assessment.
Collateral Reporting
Collateral reporting (information supplied by family and friends) can help a clinician validate substance use because patients do not always reply honestly to assessment questions, especially those concerning illicit drug use. In addition, some patients cannot recall information accurately because of cognitive impairments. Collateral reports can be useful in determining or confirming
- Which substances a patient used
- Age at first use
- Frequency of use
Quantities used per occasion
- Duration of periods of abstinence
- Concurrent or sequential choice of substances
- Dysfunctional or inappropriate use of alcohol or prescription drugs (e.g., using anxiolytics or alcohol to induce sleep or sedatives to reduce anxiety)
However, before a clinician can obtain information from family members and significant others, the patient must give consent. In some cases, permission may be denied or family members will refuse to cooperate or cannot be contacted. While less than ideal, assessors in this situation may ask the patient, "Has anybody told you that you're doing this too often?" or "Has anybody complained about your behavior when you use?" Because people with substance use disorders are often "in denial," responses that provide a perspective that differs from the patient's account of his use and its consequences frequently suggest a problem. Sometimes, patients' explanations for why their interpretation conflicts with those of family and friends also can be useful in gauging a patient's understanding of his situation and readiness to change: "My wife is so rigid, drinking just loosens me up. When I'm uninhibited, she gets nervous." Or, "I just smoke pot to relax. What my Mom really doesn't like are my friends."
Supporting Laboratory Tests
Common laboratory tests for direct measures of recent alcohol use include blood alcohol content (BAC) levels, urine, BreathalyzersTM, and recheck BreathalyzersTM. These tests measure current use and are used for the most part by law enforcement and hospital emergency room personnel (National Institute on Alcohol Abuse and Alcoholism, 1993). Drug tests include analysis of urine, hair, and saliva, though the latter two are not commonly used.
Midanik reports that 71 percent of patients' self-reports matched the findings on their BreathalyzerTM tests when the patients knew the test would be given (Midanik, 1989). While studies of illicit drug use show varying reliability in patient self-reports, clinical experience with patients involved in alcohol-related motor vehicle crashes has found surprisingly high accuracy, considering the legal ramifications, in self-reports of alcohol consumption (Cherpitel, 1989; Gibb et al., 1984). Patients, however, may be more likely to provide accurate reports if they believe that disclosure may be important to their care for an illness or injury. Because of the limitations of self-reporting and of under-reporting due to the stigma associated with problem drinking, many assessors use laboratory testing to
- Confirm recent use (prior to recommending methadone, for example)
- Validate suspicions about recent use
- Support findings from the assessment pointing to chronic use
- Provide information about alcohol- and other drug-related physical problems (e.g., liver damage)
Alcohol: Blood alcohol concentration (BAC) determinations
Testing for blood alcohol concentrations (BACs) provides a short-term indicator useful in assessing current impairment caused by alcohol. Tests are typically conducted following involvement in traffic or other serious accidents or injuries where excessive drinking may be a factor. Blood alcohol concentrations are measured in milligrams (mg) of alcohol per deciliter (dl) of blood. This figure is converted to a percentage. One hundred mg/dl equals 100 mg percent or 0.1 percent. Thus, a BAC of 0.1 mg percent is equivalent to a concentration in blood of 100 mg of alcohol per deciliter of blood.
A woman weighing 150 pounds would achieve a level of 100 mg/dl if she drank approximately four drinks in an hour (six drinks in an hour for a 200-pound man), with a standard drink defined as 12 ounces of beer, 1_ ounces of liquor or distilled spirits, or 5 ounces of wine. However, individuals' alcohol metabolism varies not only according to gender and body weight, but also by food ingested, speed of alcohol consumption, age, and physical condition, among other factors.
In men, impairment from alcohol consumption has been shown to occur at the level of 50 mg/dl, though fine motor skills can be impaired at lower levels. In women and elderly persons, impairment may occur at even lower levels. The probability that an auto crash will occur begins to rise when the driver's BAC exceeds 40 mg/dl (American Medical Association, 1986), and climbs steeply as BAC moves up to 100 mg/dl. Most people demonstrate impaired driving at levels of 50 to 70 mg/dl.
Most persons metabolize alcohol at a rate of 15 to 25 mg per hour. Thus, the longer the time between imbibing and testing, the lower the BAC. Vomiting also may eliminate alcohol from the stomach before it reaches the blood.
A single elevated blood alcohol level does not provide information about the regularity and severity of alcohol abuse unless the counts are extremely high. For example, a level of 200 or higher without noticeable intoxication indicates a high degree of tolerance to alcohol, which suggests alcohol dependence.
In emergency situations or hospital-based settings, especially when responding to trauma victims, BACs contribute information important to clinicians in devising effective treatment plans. However, the Consensus Panel does not recommend their routine use in the office-based primary care setting.
Alcohol: Gamma-glutamyl transferase (GGT)
Alcohol, almost all types of liver disease, and a variety of other diseases including hepatitis, pancreatic cancer, and diabetes mellitus, can increase the activity of the enzyme gamma-glutamyl transferase (GGT) in the blood. GGT tests measure damage to liver cells; a rise in GGT levels has been correlated with an increase in alcohol intake (Persson et al., 1990). Because other conditions, as well as age, lifestyle, and gender, also affect its activity levels, GGT is an imperfect indicator of heavy alcohol use. Nevertheless, among problem drinkers and alcoholics, it can be useful in encouraging patients to provide honest answers to assessment questions, in evaluating the health impact of chronic, heavy alcohol use, and in monitoring progress in treatment (National Institute on Alcohol Abuse and Alcoholism, 1993). Based on their clinical experience, members of the Consensus Panel recommend checking the GGT as part of the assessment process. If it is elevated, lowering it can serve as a measurable goal of treatment.
Two relatively new tests, carbohydrate-deficient transferrin (CDT) and aspartate aminotransferase (AST) appear to have some value in identifying heavy alcohol consumption, and researchers are investigating a number of other measures in an effort to develop improved diagnostic tools. Until large-scale studies begin to confirm their effectiveness for screening and assessment, these tests will be used primarily by researchers (National Institute on Alcohol Abuse and Alcoholism, 1993).
Illicit drugs: Urine tests
Typically, urine tests for illicit drugs provide information on a patient's recent use of sedative-hypnotics, cocaine, opiates, and cannabis, although screening for other drugs (e.g., phencyclidine or LSD) can be specially requested. Patients who have used drugs within 72 hours prior to the test -- regardless of whether they are dependent on the drug or are using it for the first time -- will screen positive. A drug user who knows that testing is likely or who, for a variety of other reasons, has abstained from drugs (other than marijuana) within that time period will test negative. Since marijuana is fat-soluble, its metabolites can be detected in urine for 2 weeks or longer, depending on the sensitivity of the test and the patient's pattern of use.
Testing methods differ in sensitivity. Enzyme immunoassay (EIA) and radioimmunoassay (RIA) are commonly used for routine drug screening (Sullivan, 1995). Gas chromatography-mass spectrometry (GC-MS) is a separate technology that is considerably more sensitive and is used to confirm positives from EIA and RIA tests. Some laboratories automatically confirm all positive tests with GC-MS. If a laboratory does not follow this procedure and an assessor is using the results for any purpose other than clinical confirmation (e.g., when an employment- or court-mandated screen is positive and job security or legal status is threatened as a result), the positive test should always be verified by GC-MS.
Much like supplemental laboratory tests for alcohol, urine tests may be used during assessment to encourage honest responses to questions, to confirm suspicions about use when it is denied, and to verify use of heroin prior to referral or admission to a methadone program. During treatment, urine tests help to monitor progress and, in methadone programs, help ensure that patients are ingesting their methadone.
Since primary care patients frequently provide urine specimens for analysis, collecting urine for drug testing theoretically could be conducted with minimal disruption in the primary care setting if staff were willing to implement appropriate chain of custody and confidentiality procedures. However, urines cannot be collected deceptively. Prior to screening a specimen for drugs, the patient's permission must always be obtained (see Appendix B for more on confidentiality).
Some drug users tamper with specimens to avoid detection, even if they have granted permission for testing. Some may substitute another person's sample, dilute the specimen, or add epsom salts and sodium bicarbonate to it to neutralize pH. For this reason, urine samples should be checked for temperature, color, and consistency (sediment). Some specimen containers are equipped with temperature strips, and some laboratories routinely assess samples for color and other anomalies.
Although not required, a positive urine screen, together with findings from a patient's history, mental assessment, and physical examination, provides strong support for a diagnosis of substance use disorder.
Making the Diagnosis
The categorical classification of "Substance-Related Disorders" in the DSM-IV provides the standard against which a formal diagnosis is made. Within this large category, 11 different classes of substances, including alcohol, are considered. Disorders are divided into two broad groups: "Substance Use Disorders," which includes "Substance Dependence" and "Substance Abuse," and "Substance-Induced Disorders," which includes a host of disorders ranging from "Substance Intoxication" and "Substance Withdrawal" to "Substance-Induced Anxiety Disorder." Using the DSM-IV criteria, an assessor makes a drug-specific diagnosis by disorder. DSM-IV diagnoses include alcohol abuse, alcohol dependence, cocaine intoxication, and hallucinogen abuse (American Psychiatric Association, 1994a).
Assessors use the information compiled during the personal history, interview, physical examination, and other patient-specific assessments such as the mental status examination to determine the DSM-IV diagnosis (many assessors rely on The Quick Reference to the Diagnostic Criteria from DSM-IV to facilitate diagnosis during the assessment process [American Psychiatric Association, 1994b]). In addition to helping assessors characterize a patient's problem, another advantage of a DSM-IV diagnosis is that its standard nomenclature and classification system are generally understood by those other clinicians who may be collaborating in a patient's treatment, and such diagnoses are accepted by health insurance companies. The DSM-IV diagnostic criteria for substance dependence and substance abuse appear in Figures 4-2 and 4-3.
Once an assessor has made a diagnosis, the next critical step is to work with the patient in determining the level and type of services that the patient needs. Over the past several years, the substance abuse treatment field, led by the American Society of Addiction Medicine (ASAM), has been grappling with the concept and implementation of patient placement criteria that identify both major problem areas that should be considered in designing an individual treatment plan and the array of services most likely to address those problems. ASAM's Patient Placement Criteria for the Treatment of Substance-Related Disorders, Second Edition (ASAM PPC-2) offers guidelines that are consistent with the DSM-IV to help assessors and other clinicians evaluate the "severity and intensity of service required" (American Society of Addiction Medicine, 1996, p. 14). See TIP 13, The Role and Current Status of Patient Placement Criteria in the Treatment of Substance Use Disorders, for more on patient placement criteria (CSAT, 1995a).
Central to this evolving model of patient placement is that level of care and service mix may change as patient needs dictate. When selecting the level of care, the goal should be the least restrictive treatment that is effective. ASAM's criteria help focus attention on an individual's needs (American Society of Addiction Medicine, 1996). Rather than forcing a fit between a patient and a single program, those criteria provide information that frees assessors and patients to critically evaluate assessment results, investigate various options in the community, and construct a plan that incorporates needed services from a variety of resources. The realities of service availability and insurance coverage, however, ultimately affect both the level and type of service a patient receives.
- Chapter 4—Assessment - A Guide to Substance Abuse Services for Primary Care Clin...Chapter 4—Assessment - A Guide to Substance Abuse Services for Primary Care Clinicians
Your browsing activity is empty.
Activity recording is turned off.
See more...