Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Reuter-Sandquist M; Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Assistant [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2022.
8.1. INTRODUCTION TO UTILIZE PRINCIPLES OF MOBILITY TO ASSIST CLIENTS
Learning Objectives
• Examine types and uses of restraining devices
• Use alternatives to restraints
• Assist with moving or positioning a client
• Promote joint mobility, body alignment, and activity
• Assist with ambulation
• Use client transfer techniques
• Apply prosthetic and orthotic devices
Mobility is the ability to move one’s body parts, change positions, and function safely within the environment. It is one of the most important factors for remaining independent. Immobility, the inability to independently move and change positions, is a major reason why people are admitted to long-term care facilities for assistance to complete their activities of daily living (ADLs). Declining mobility can negatively affect many aspects of one’s health, especially in the musculoskeletal, respiratory, integumentary, circulatory, and digestive systems. Complications of immobility will be further discussed in Chapter 9.
Nursing assistants (NAs) have a major responsibility for assisting clients who have decreased mobility. Some clients require minor assistance to ambulate safely or move from their bed to a chair, whereas other clients require full assistance for repositioning in bed and/or transferring. NAs also assist in maintaining a resident’s level of functioning by promoting joint mobility and applying prosthetics and orthotics. This chapter will review moving and positioning clients, as well as promoting their joint mobility.
In some circumstances, medical restraints may need to be applied to clients who are at risk for hurting themselves or others. This chapter will also review various types of restraints and how to prevent complications that can result from decreased movement.
8.2. MOVING AND POSITIONING CLIENTS
When a resident is admitted to a facility or begins receiving home health care, assessments are completed by health care staff (including nurses, physical therapists, and occupational therapists) to determine their care needs. Examples of assessments include their ability to complete hygiene and grooming needs, as well as the amount and type of assistance required to safely reposition themselves in bed, move in and out of bed into a chair, and walk (if they are able). The findings from these assessments are implemented into the client’s care plan that the nurse and NA carry out. Roles of various therapists will be further discussed in Chapter 9.
Repositioning in Bed
As discussed in the “Skin Care” section in Chapter 5, clients who are immobile must be repositioned every two hours to prevent pressure injuries and other complications of immobility that will be further discussed in Chapter 9. Moving residents must be done carefully because their skin can easily be damaged by improper handling. Due to the effects of aging on the integumentary system, older adults can develop pressure injuries from friction and shear when repositioned or from lying in one position for long periods of time in bed. Pressure injuries (formerly called pressure ulcers or bedsores) are localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure and/or shear.[1]
Shear happens when skin moves one way but the underlying bone and muscle stay fixed or move the opposite direction. Shear can occur when an individual sits up in a bed, chair, or wheelchair, and gravity causes the bone and muscle to slide down while the skin is pulled in the opposite direction by the sheets or clothing. Friction is caused when skin is rubbed by clothing, linens, or another body part and can cause chafing. Chafing typically occurs when the skin has inadequate moisture. See an illustration of sheer and friction in Figure 8.1.[2]
Figure 8.1
Friction and Shear Causing Pressure Injuries
For additional information on friction and shear, visit the Wound Care Education Institute’s Friction vs. Shearing in Wound Care web page.
To prevent friction and shear, residents should be moved in bed with a lift sheet. The lift sheet, also called a draw sheet, is placed between the resident and the bottom or fitted sheet. (Review types of linens in “Making an Unoccupied Bed Checklist” in Chapter 3.) The lift sheet protects the client’s skin by creating a barrier when the client is moved so the friction that occurs happens between the lift sheet and fitted sheet rather than the resident’s skin and the fitted sheet. Lift sheets also protect the client’s skin from bruising and skin tears that can occur when moving the client by assistants putting their hands directly on a client’s limbs. A skin tear is a separation of skin layers caused by shear, friction, and/or blunt force. Lift sheets should always be used to reposition a client who requires assistance, and failing to do so is considered neglectful due to the high probability of skin injury. See Figure 8.2[3] for an image of boosting a resident in bed with a lift sheet.

Figure 8.2
Boosting a Resident in Bed With a Lift Sheet
The steps for boosting a client up in bed include the following components[4]:
- Explain to the patient what will happen and how the patient can help.
- Perform hand hygiene.
- Raise the bed to a safe working height and ensure that the brakes are applied.
- Position the patient in the supine position with the bed flat. Place a pillow at the head of the bed and against the headboard to prevent accidentally bumping the patient’s head on the headboard.
- Stand with your feet shoulder width apart at the bedside between the client’s shoulders and hips with a second assistant in a similar position on the other side of the bed. This position keeps the heaviest part of the client closest to the center of gravity of the assistants.
- Fan-fold the lift sheet toward the patient with your palms facing upwards. This provides a strong grip to move the client up with the lift sheet.
- Ask the patient to tilt their head toward their chest, fold their arms across their chest, and bend their knees to assist with the movement. Let the patient know the move will happen on the count of three. This step prevents injury from occurring to the patient and prepares them for the move.
- Tighten your gluteal and abdominal muscles, bend your knees, and keep your back straight and neutral. Face toward the direction of movement. Using proper body mechanics can help prevent back injury when used appropriately in patient-care situations.
- On the count of three by the lead person, gently slide (not lift) the patient toward the head of the bed, shifting your weight from the foot closest to the end of the bed to the foot closest to the head of the bed, while keeping your back straight and knees slightly bent.
- Replace the pillow under the patient’s head, move them into a different position as indicated, and cover them with a sheet or blanket per their preference.
- Check the patent’s comfort and for proper alignment.
- Ensure the patient remains in the middle of the bed.
- Lower the bed, check that the brakes are locked, and ensure the call light is within reach. Perform hand hygiene.
- Document or report any skin issues or other observed changes with the patient.
Review the “Body Mechanics and Safe Equipment Use” section in Chapter 3 to prevent yourself from injury during repositioning.
Pressure injuries are preventable by repositioning clients at least every two hours and reporting any skin redness or other changes to the nurse for additional interventions. There are several positions that can be used to relieve pressure points and keep residents safe from pressure injuries. Repositioning also promotes improved circulation through movement. Positions are described in the various “Positions” subsections below.
When a resident has an existing pressure injury or a susceptible area, an hourly repositioning schedule is typically implemented (rather than the standard two-hour repositioning schedule considered routine care for all residents requiring assistance with their mobility). Repositioning a client every hour should be documented, indicating the time and the positions the resident was moved from and placed into. An example of documentation is, “At 1400, the resident was repositioned from a right side-lying position to a supine position.”
Body Alignment for Positioning Residents
Similar to how nursing assistants use good body alignment (i.e., good posture) to prevent musculoskeletal injuries to themselves, the same principle should also be applied to residents. Good body alignment not only prevents injury, but also promotes comfort for residents. After repositioning a resident, the NA should stand at the foot of the bed and verify that the resident’s spinal column is straight and parallel to the sides of the bed, as well as ensuring the resident is lying in the middle of the bed (to reduce the risk of accidentally rolling out of bed). See Figure 8.3[5] of an image of a properly aligned mannequin in the lateral position.
Figure 8.3
Properly Aligned Lateral Position
Pressure Relieving Devices
In addition to being caused by friction and shear, pressure injuries can occur in high-risk areas such as bony prominences or where a bone is lying directly on top of another bone. Bony prominences are the areas of the body where a bone lies close to the skin’s surface, such as the back of the head, shoulders, elbows, heels, ankles, tops of the toes, hips, and coccyx (i.e., tailbone). These areas are most susceptible to developing pressure injuries because they have the least amount of cushioning. Placing pillows or other specialized equipment reduces the pressure in these areas and also helps to prevent the resident from rolling out of position.
There are different sizes of pillows and equipment available in facilities to relieve pressure, prevent rolling, and increase client comfort. For example, foam wedges are placed behind a patient’s back to prevent them from returning to the supine position or rolling close to the edge of the bed. See Figure 8.4[6] for images of a wedge cushion and a client positioned using a wedge cushion.

Figure 8.4
Wedge Cushion Used for Positioning. Used under Fair Use.
Positions
Common positions used for repositioning patients are supine, Fowler’s, lateral, Sims’, and prone positions.
Supine Position
The most common sleeping position is the supine position, where the client is lying flat on their back as demonstrated in Figure 8.5.[7] Pillows or wedges can be placed on each side of the resident to promote comfort or to support a limb that is immobile or has impaired function. A pillow should also be placed underneath their calves to keep their heels off the bed and prevent pressure that can cause pressure injuries. (This pillow placement under the calves is often referred to as “floating the heels.”) After repositioning the client, the NA should be able to place their hand underneath the client’s heels to verify there is no contact by the heels on the mattress.
Figure 8.5
Supine Position
If a resident is highly susceptible to pressure injuries of the heels, they may have specialized soft foam boots, as illustrated in Figure 8.6,[8] that support the ankles and keep the heels floated off the bed. A foot cradle may also be used to keep sheets and blankets off the tops of the toes if the resident has a history of skin injury in that area.
Figure 8.6
Inside of Foam Boot (left) and a Foam Boot Supporting a Heel
Fowler’s Position
In Fowler’s position, the client is lying on their back with their head elevated between 30 and 90 degrees, as illustrated in Figure 8.7.[9] Residents should be placed in Fowler’s position any time they are eating or drinking or when oral care is provided. Fowler’s position is also used to increase lung expansion for those with breathing difficulties, such as those that occur with heart failure. It may also be used for comfort during leisure activities such as watching television or reading. Additionally, residents receiving tube feeding should never have their head placed below a 30-degree angle because this can cause aspiration of the fluids.

Figure 8.7
Fowler’s Position
However, Fowler’s position increases the risk of friction and shear on the coccyx and gluteal muscles as the client slides down in bed. This risk can be reduced by concurrently raising the lower portion of the bed or by putting multiple pillows below the lower legs. These actions bend the knees and reduce the pull of gravity that causes the resident to slide down in bed. A pillow can also be placed below the feet to prevent them from contacting the foot of the bed.
Lateral or Side-Lying Position
Lateral (side-lying) position places the resident on their left or right side as shown in Figure 8.8.[10] This position relieves pressure on the coccyx and can increase blood flow to the fetus in pregnant women. The top arm and leg can be placed in a flexed position in any range that is comfortable to the resident. Supports should be placed behind the back to keep the resident from rolling to the supine position. Additionally, supports should be placed between the top knee and the bed or other knee and between the top elbow and rib cage or the bed, depending on the location of the elbow joint. These supports will alleviate pressure between the bony prominences in these areas. The pillow underneath the resident’s head should also be adjusted for comfort and alignment checked from the foot of the bed.
Figure 8.8
Lateral (Side-Lying) Position
The most common rotation of positions for repositioning residents is to rotate them from supine position to lateral position, to supine position, to lateral position on the opposite side. See the “Positioning Supine to Lateral (Side-Lying) Skills Checklist” for the steps to move a resident from the supine to lateral (side-lying) position.
Sims’ Position
Sims' position is very similar to the lateral position, but the client is always placed on their left side and their left arm is placed behind the body (rather than in front of the body). Sims’ position is commonly used for administration of a suppository or an enema. Depending on your state’s scope of practice, you may be delegated to give an enema, or the nurse may ask you to prepare the patient for an enema by placing them in the Sims’ position as pictured in Figure 8.9.[11]
Figure 8.9
Sim’s Position
Prone Position
In the prone position, the client is placed on their stomach with their head turned to one side, as seen in Figure 8.10.[12] Pillows should be placed underneath the shins to relieve pressure. Pillows (or wedges) can also be placed on both sides of the patient, and the head pillow should be readjusted for comfort.
Figure 8.10
Prone Position
Prone is the least commonly used position, especially in older adults due to their neck immobility. This position may be used for a client with a surgical wound on the back side of their body or to improve respiratory status in clients with respiratory conditions like COVID-19.
References
- 1.
- Edsberg, L. E., Black, J. M., Goldberg, M., McNichol, L., Moore, L., & Sieggreen, M. (2016). Revised national pressure ulcer advisory panel pressure injury staging system: Revised pressure injury staging system. Journal of Wound, Ostomy, and Continence Nursing: Official Publication of The Wound, Ostomy and Continence Nurses Society, 43(6), 585–597. 10.1097/WON.0000000000000281 ↵ 10.1097/WON.0000000000000281. [PMC free article: PMC5098472] [PubMed: 27749790] [CrossRef] [CrossRef]
- 2.
- “Shear Force” and “Shear Force Closeup” by Meredith Pomietlo at Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 3.
- “Book-pictures-2015-572.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-5-positioning-a-patient-on-the-side-of-a-bed/ ↵. - 4.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 5.
- “Lateral Position.jpg” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 6.
- “6105kmeOsGL
._AC_SL1000_.jpg” by unknown author is used on the basis of Fair Use. ↵. - 7.
- “supine.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-4-positioning-a-patient-in-bed/ ↵. - 8.
- “Foam Boot” and “Foam Boot Supporting a Heel” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 9.
- “degreeLow.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-4-positioning-a-patient-in-bed/ ↵. - 10.
- “lateral.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-4-positioning-a-patient-in-bed/ ↵. - 11.
- “sims.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-4-positioning-a-patient-in-bed/ ↵. - 12.
- “prone.jpg” by unknown author is licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-4-positioning-a-patient-in-bed/ ↵.
8.3. PROMOTING JOINT MOBILITY AND ACTIVITY
Actions for maintaining the musculoskeletal system and preventing complications will be discussed in Chapter 11. These actions can be summarized by the phrase, “Use it or lose it,” meaning the functioning of the musculoskeletal system declines quickly when it is not being used. Small, everyday activities help maintain flexibility in joints, muscle strength, and healthy bone density. The NA can help residents maintain their musculoskeletal health by encouraging them to do as many activities for themselves as possible.
While it may be faster to perform ADLs for a resident, allowing them to provide care for themselves not only maintains musculoskeletal function but also gives them a sense of control that can enhance their self-esteem and quality of life. Here are ways NAs can encourage residents to participate in their self-cares:
- Allow residents to dress themselves to maintain flexibility in their shoulders, wrists, hips, and knee joints. Using buttons and zippers helps to maintain flexibility in the fingers, as well as promoting hand-eye coordination.
- When toileting a resident, encourage them to walk into the bathroom rather than bringing them in their wheelchair to the toilet or commode.
- Encourage residents to walk to meals (with assistance as needed) rather than being transported by wheelchair.
- Play board games or card games to promote upper body mobility, as well as to stimulate their cognitive status.
- Encourage residents to feed themselves. If they require extensive assistance, offer finger foods they can hold and eat more easily.
- Ask residents to wash their face, brush their teeth, or shave. Prepare the soap and washcloth, toothbrush and toothpaste, or razor, and assist in completing the task as needed.
- If a resident can’t walk, take off the foot pedals from their wheelchair (if it is safe to do so). Encourage them to move their feet while sitting to propel themselves around the facility independently.
- Inform residents of scheduled daily activities and promote movement and social interaction.
8.4. ASSISTING CLIENTS TO TRANSFER
It is important to note that most injuries that happen to clients and staff occur when clients are being transferred. Safety is an integral component of moving clients and should receive the highest priority. Special consideration should be given to these items to prevent injury from occurring:
- Gait belt fit and placement
- Brakes on the bed
- Brakes on the wheelchair
- Brakes released on the lift
- Placement of nonskid footwear
- Resident’s proximity to the lift
- Objects in the room that may be a hazard during the movement
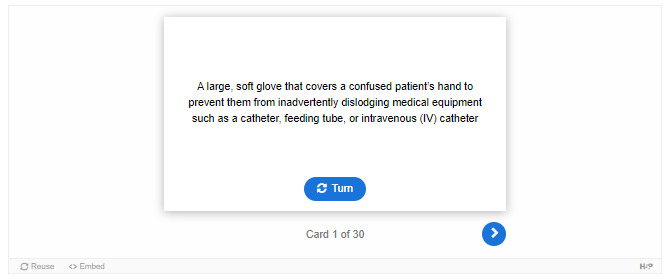
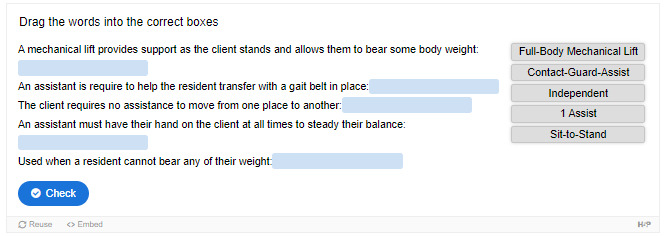
Nursing assistants should always review a client’s care plan for their current transfer status before moving them. Transfer status refers to how a resident moves from one place to the other, such as from a bed to wheelchair or wheelchair to toilet. Physical therapists (i.e., health specialists who evaluate and treat movement disorders) assess clients and make recommendations for how clients should be safely transferred. Transfer status orders are determined by how much body weight a client can independently bear and how much weight an assistant is required to support. Transfer status orders include these types of orders:
- Independent: The client requires no assistance to move from one place to another.
- Contact-Guard-Assist (CGA): One assistant must have their hand on the client at all times to steady their balance.
- 1 assist (1A): One assistant is required to help the resident transfer (with a gait belt in place).
- 2 assist (2A): Two assistants are required to help the resident transfer (with a gait belt in place).
- Sit-to-Stand: A sit-to-stand mechanical lift is required to help a resident transfer. A sit-to-stand mechanical lift provides support as the client stands while allowing them to bear some body weight and maintain joint mobility and leg strength. (Using a gait belt would require extensive assistance and could cause injury to the client or the staff.) Sit-to-stands may be completed with one or two assistants, as determined by the physical therapist and agency policy.
- Full-Body Mechanical Lift: A full-body mechanical lift is required when the resident cannot bear any of their weight when transferred from bed to chair and back. (“Full-body mechanical lift” is a generic term. The facility or organization may refer to this type of lift by the manufacturer of the lift, such as a “Hoyer lift” or “PAL lift.”) Full-body mechanical lifts may be portable or attached to the ceiling. Two assistants are always required for transfer with full-body mechanical lifts for safety purposes. Due to federal liability laws, the health care professional moving the lift must be 18 years of age or older.
Assisting to Seated Position or Dangling
When transferring a client using a 1A, 2A, or sit-to-stand transfer method, first assist the resident to move to a seated position on the side of their bed. Residents who can transfer with one of these methods are able to bear some or most of their weight and should be able to move partially on their own. Use your hands on the person’s limbs to direct the movement, and use the lift sheet (similar to when boosting a client up in bed).
Due to heart and circulation changes that occur with age, orthostatic hypotension can occur when a person moves suddenly from a lying to sitting position or from a sitting to standing position. Orthostatic hypotension is a sudden drop in blood pressure that can cause clients to feel dizzy and increase their risk for falls with position changes. Some clients may experience vertigo, a sensation that the room is spinning. To prevent orthostatic hypotension and these symptoms, tell the person to dangle (i.e., sit up on the edge of the bed) for a few moments before continuing with the transfer. Dangling gives the cardiovascular system time to regulate blood pressure and blood flow to the brain, thus preventing dizziness and falls. Ask the client if they are feeling dizzy before you proceed with transferring. See Figure 8.11[1] for illustration of the steps to safely assist a client to a seated position[2]:

Figure 8.11
Assisting a Resident to a Seated Position
- Lock the brakes on the bed.
- Raise the bed to a working height.
- Stand facing the head of the bed at a 45-degree angle with your feet apart, with one foot in front of the other. Stand next to the waist of the resident.
- Ask the resident to turn onto their side, facing you, as they move closer to the edge of the bed. Use the lift sheet to assist the resident if needed.
- Place one hand behind the resident’s shoulders, supporting their neck and vertebrae.
- Place the other hand around the resident’s knees.
- On the count of three, instruct the resident to use their elbows to push up against the bed and then grasp the side rail. Support their shoulders as they move to a seated position. Shift your weight from the front foot to the back foot as you assist them to sit. Do not allow the resident to place their arms around your shoulders because this can cause serious back injuries.
- As you shift your weight, gently grasp the resident’s outer thighs with your other hand and help them slide their feet off the bed to dangle or touch the floor. This step helps the resident sit and move their legs off the bed at the same time. As you perform this action, bend your knees and keep your back straight and neutral. Move the resident as one entire unit (rather than the upper body followed by the lower body).
- Lower the bed so the resident’s feet touch the floor.
- Observe the resident for symptoms of orthostatic hypotension or vertigo. Ask if they are feeling dizzy before attempting any further movement.
- Check that the resident is wearing nonskid footwear before transferring.
If the resident is having difficulty moving during this procedure, use the lift sheet to pull them closer to you or to assist them from a lying to a seated position. The head of the bed can be raised before they turn on their side to support their core strength and to reduce the weight the assistant must bear. During this entire process, do not use the resident’s limbs to move them but rather move them with the trunk of their body to prevent shear and injury to their limbs and skin.
After the person is sitting upright and states they are not experiencing dizziness, apply a gait belt for a 1A or 2A transfer. The gait belt should be placed around their waist while considering the location of their breasts and abdominal folds. See Figure 8.12[3] for an image of applying a gait belt. The fit of the gait belt should be snug, but you should be able to put your fingers underneath the gait belt for support. As the resident stands and their core muscles contract, the gait belt can loosen and tend to slide up, so it is important for it to be snug. If the belt is too long, it can get caught in the patient’s legs during transfer, so tuck the excess length back into the belt. Gait belts should not be used for clients with abdominal wounds or some types of heart conditions; a different transfer method should be in the care plan. Contact the nurse if you have concerns about using a gait belt based on the client’s condition.

Figure 8.12
Applying a Gait Belt
Place nonskid footwear on the resident before transferring them from the bed to the chair. These preparations should be done before the wheelchair or sit-to-stand is brought closer to the bed to reduce the risk of injury from the resident inadvertently hitting the lift or chair while moving.
The steps to complete a one person assist (1A) are listed in the “Transfer From Bed to Chair With a Gait Belt” Skills Checklist. If a two-person assist (2A) is required, the same steps are used, but the assistants stand on each side of the resident to provide additional support during the transfer.
View the following video showing a transfer of a patient from a bed to a regular chair[4]: Assisting From Bed to Chair With a Gait Belt or Transfer Belt.
Transferring with Mechanical Lifts
Mechanical lifts include sit-to-stand lifts and full-body lifts. Some facilities have full-body mechanical lifts that are attached to the ceiling of the room. See Figure 8.13[5] of an image of a sit-to-stand lift and Figure 8.14[6] of an image of a full-body mechanical lift and mechanical swing. NAs should be aware of agency policy regarding transferring clients using mechanical lifts; for safety purposes, most agencies require two NAs or a nurse and an NA to transfer clients using a mechanical lift.

Figure 8.13
Sit-to-Stand Lift
Figure 8.14
Full-Body Mechanical Lift and Mechanical Sling
The legs of portable full-body mechanical lifts can be placed in a closed or open position. The open position provides the greatest stability due to a wide base of support. See Figure 8.15[7] for an image comparing the legs of a portable full-body mechanical lift in a closed and open position.
Figure 8.15
Portable Full-Body Mechanical Lift With Legs in a.) Closed Position and b.) Open Position
When transferring a client from their bed to wheelchair using a sit-to-stand or portable full-body mechanical lift, the wheelchair should be positioned near the bed while also allowing enough room for the lift to rotate towards the chair. Because the lift will have to slide underneath the bed, check for any cords or equipment under the bed that can cause the lift to get tangled. Raising the bed height just before placing the lift under the bed should also alleviate potential problems.
The lift has greatest stability when its legs are open with a wide base of support, but some beds do not have enough space underneath to allow the legs to be open. If this is the case, open the legs as soon as possible when moving the lift from under the bed to provide a stable base.
Sit-to-stand and full-body lifts have brakes, but brakes should not be applied when the resident is standing in the sit-to-stand or raised off the bed in a full-body lift. (If the client’s weight shifts while the brakes are on, it can cause the lift to tip and endanger the resident, as well as the assistants.)
Before initiating a transfer, verify that the lift will support the weight of the resident. Most mechanical lifts have a weight capacity of 400 pounds. Bariatric lifts are used to support a client weighing 600 or more pounds. See Figure 8.16[8] for locating the weight capacity on a lift.

Figure 8.16
Weight Capacity of a Mechanical Lift
Full-body mechanical lifts have different types of slings used to lift the client. Slings may be full-body or split-leg (butterfly). The type of sling used is determined by the physical therapist, based on the client’s strength and mobility, and should be noted in the resident’s care plan. A sling has various loops to connect it to the lift and are often color-coded to ensure the resident’s body is in proper position for transferring. See Figure 8.17[9] for images of a full-body sling and Figure 8.18[10] for images of a split-leg (butterfly) sling.
Figure 8.17
a.) Front of Full-Body Sling; b.) Back of Full-Body Sling; c.) Loops (right)

Figure 8.18
a.) Front of Split-Leg (Butterfly) Sling and b.) Back of Split-Leg (Butterly) Sling
The top of a full-body sling should be placed above the resident’s head and should end just above the knee joint to avoid hyperextending the knees when they are suspended in the lift. The top of a split-leg (butterfly) sling should be placed at shoulder height, and the bottom of the sling should be around the buttocks. Depending on hip mobility, the split-leg sling may be crossed between the client’s legs or placed around their legs (often referred to as a “basket”). See Figure 8.19[11] for an image of a mannequin prepared to transfer using a crossed sling and Figure 8.20[12] for an image of transferring a mannequin with the sling wrapped around their legs (i.e., a “basket” approach).
Figure 8.19
a.) Preparing to Transfer With Crossed Sling and b.) Suspended in a Crossed Sling
Figure 8.20
a.) Preparing to Transfer With a “Basket” Approach b.) Suspended in a Sling With a “Basket” Approach
The handles of the sling should face away from the client, allowing the assistants to position the client in their chair or bed. (Do not move clients by directly contacting their limbs because this can cause injury.)
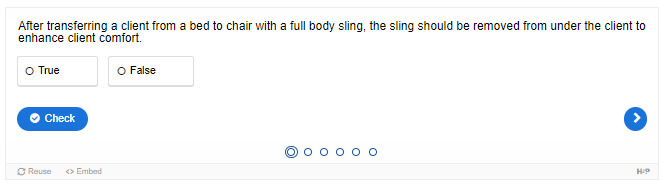
After transferring a client from a bed to a chair using a full-body sling, the sling should remain under the resident while they are seated in a wheelchair or other chair. When placing the resident back in bed, the sling is then removed. However, when transferring a client using a split-leg (butterfly) sling, it can be removed from underneath the client in the chair and replaced before they are transferred again.
See the Skills Checklists “Transfer From Bed to Chair With Sit-to-Stand” and “Transfer From Bed to Chair With Mechanical Lift” for steps for providing safe transfers with both types of lifts. Each brand of sit-to-stand and mechanical lift has some variances; the facility where you work will provide specific training on their lifts.
Watch the following YouTube video for a demonstration of moving a resident with a sit-to-stand[13]: Aidacare Training Video – Manual Handling – Sit To Stand.
Explore the following YouTube video[14] on a mechanical lift completed with a butterfly or split-leg sling: Aidacare Training Video – Manual Handling – Lie To Sit
References
- 1.
- “Book-pictures-2015-5851.jpg,” “Book-pictures-2015-587.jpg,” and “Book-pictures-2015-588.jpg” by unknown authors are licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-5-positioning-a-patient-on-the-side-of-a-bed/ ↵. - 2.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 3.
- “Sept-22-2015-119.jpg” and “Sept-22-2015-121-001.jpg” by unknown authors are licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-5-positioning-a-patient-on-the-side-of-a-bed/ ↵. - 4.
- Thompson Rivers University Open Learning. (n.d.). Assisting from bed to chair with a gait belt or transfer belt [Video]. Thompson Rivers University Open Learning. All rights reserved. https://barabus
.tru.ca /nursing/assisting_from_bed.html ↵. - 5.
- 6.
- 7.
- “Portable Full-Body Mechanical Lift With Legs in Closed Position” and “Portable Full-Body Mechanical Lift With Legs in Open Position” by Myra Reuter for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 8.
- “Weight Capacity of a Mechanical Lift” by Myra Reuter for Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 9.
- “Front of Full-Body Sling,” “Back of Full-Body Sling,” and “Loops” by Myra Reuter for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 10.
- “Front of Full-Body Sling,” “Back of Full-Body Sling,” and “Loops” by Myra Reuter for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 11.
- “Preparing to Transfer With Crossed Sling” and “Suspended in a Crossed Sling” by Myra Reuter for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 12.
- “Preparing to Transfer With a ‘Basket’ Approach” and “Suspended in a Sling With a ‘Basket’ Approach” by Myra Reuter for Chippewa Valley Technical College are licensed under CC BY 4.0 ↵.
- 13.
- Aidacare. (2017, July 5). Aidacare training video - Manual handling - Sit To stand [Video]. YouTube. All rights reserved. https://youtu
.be/L914lkoub6E ↵. - 14.
- Aidacare. (2017, July 5). Aidacare training video – Manual handling – Lie to sit [Video]. YouTube. All rights reserved. https://youtu
.be/3GOgp_HX4JQ ↵.
8.5. ASSISTING WITH AMBULATION
Ambulation is the medical term used for walking. Ambulation provides weight-bearing activity that promotes bone health and joint mobility. A physical therapist will determine if a person can safely walk independently, with the assistance of one or two people, or if they require an assistive device such as a cane or walker. This information is documented in their nursing care plan. Similar to when assisting a client to transfer with a gait belt, the nursing assistant should place nonskid footwear on the person and allow them to dangle on the edge of the bed before standing to ambulate. For specific steps, see the “Ambulation From Wheelchair” Skills Checklist.
If a resident requires assistance with a cane, the cane should be placed on the resident’s stronger side. The resident should step forward with the strong leg and then use the cane and the weaker leg for the next step.
There are three types of walkers: a standard walker, a two-wheeled walker (2WW), and a four-wheeled walker (4WW). The type of walker a resident should use is recommended by the physical therapist. A 2WW or standard walker allows for more support and a slower gait, whereas a 4WW is used by clients with better balance and mobility.
View a YouTube video[1] of an instructor demonstrating helping clients with ambulatory assistive devices:
Regardless of the assistive device used for ambulation, the NA should remind the resident to stand up straight and look forward when walking. The resident should be encouraged to take purposeful steps and to not shuffle their feet. The NA should stand to one side of the resident and slightly behind them, with one hand on their gait belt. If the resident has a weaker side, the NA should stand on that side. The NA’s fingertips should be facing upwards underneath the gait belt for proper support. If the resident loses their balance while in this position, the NA’s arm will allow them to use their bicep muscle, rather than their forearm, to steady the client. The bicep is larger and stronger than the forearm and can provide better support.
A second staff member can follow a resident who is ambulating with assistance with their wheelchair in case they experience weakness or dizziness. If the client needs to sit while ambulating, the wheelchair brakes should be applied before they sit, or in an emergent situation, the NA should block the back of the wheelchair with their body to ensure stability when the resident sits.
If a resident starts to fall while standing or ambulating, do not attempt to stop their fall or catch the resident because this can cause you to injure your back. Instead, move behind the patient and take one step back with one leg so you have a wide base of support. Support the patient around their waist or hip area or grab the gait belt. Bend one of your legs and place it between the patient’s legs from behind. Slowly slide the patient down your bent leg, lowering yourself to the floor at the same time. Always protect the resident’s head to prevent head injury. After the resident is on the floor, do not move them. For witnessed or unwitnessed falls, notify the nurse immediately for assessment. After the nurse has completed the assessment and met the resident’s immediate needs, use a mechanical lift to transfer the resident back to a wheelchair or bed. An incident report will be completed by the nurse, and the NA will be asked to give a statement on what occurred and their actions in response to the situation.[2] See Figure 8.21[3] for an image of lowering a resident who is falling to the floor.

Figure 8.21
Lowering a Client Who is Falling to the Floor
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Ambulatory Assistive Devices. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/ATn7OOP4Jko ↵. - 2.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 3.
- “Sept-22-2015-132-001.jpg” and “Sept-22-2015-133.jpg” by unknown authors are licensed under CC BY 4.0. Access for free at https://opentextbc
.ca /clinicalskills/chapter /3-7-fall-prevention/ ↵.
8.6. APPLYING PROSTHETICS AND ORTHOTICS
Prosthetics are an addition or attachment to the body that replicates the function of a lost or dysfunctional limb.[1] An orthotic is a support, brace, or splint used to support, align, prevent, or correct the function of movable parts of the body. Shoe inserts are the most common orthotics and are intended to correct an abnormal or irregular walking pattern. Other orthotics include neck braces, back supports, knee braces, and wrist supports.[2] NAs apply prosthetics and orthotics to residents following the therapist’s instructions. Incorrectly applying these devices can cause harm or injury to the resident, so you must understand the correct placement of these supports. If you are unsure, seek guidance from your supervising nurse before placing any prosthetics or orthotics.
One of the main concerns with prosthetic or orthotic devices is skin irritation. Prosthetics typically have a protective sleeve that goes over the limb prior to placing the device. The sleeve gives the prosthetic some security to prevent displacement while also protecting the skin. After the prosthetic is attached, always ask the resident if it is comfortable or if they feel any areas of pressure that may damage the skin. Most orthotics, splints, or braces are padded, but some can be applied over thin clothing. Be sure to review the resident’s nursing care plan regarding how long and at what times any supportive devices should be worn and removed. See Figure 8.22[3] for a device that prevents foot drop.

Figure 8.22
Supportive Brace to Prevent Foot Drop
References
- 1.
- 2.
- Stoppler, M. C. (Ed.). (2021, March 29). Medical definition of orthotic. MedicineNet. https://www
.medicinenet .com/orthotic/definition.htm ↵. - 3.
8.7. RESTRAINTS AND RESTRAINT ALTERNATIVES
Restraints are devices used in health care settings to prevent patients from causing harm to themselves or others when alternative interventions have not been effective. A restraint is a device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement. While restraints are typically used in acute care settings, they may be used in some circumstances in long-term care settings for safety purposes. However, restraints restrict mobility and can affect a client’s dignity, self-esteem, and quality of life; every possible measure to ensure safety should be considered before a restraint is implemented. An order from a health care provider is required to implement a restraint, and agency policy must be strictly followed.[1]
Restraints include physical devices (such as a tie wrist device), chemical restraints, or seclusion. The Joint Commission defines a chemical restraint as a drug used to manage a patient’s behavior, restrict the patient’s freedom of movement, or impair the patient’s ability to appropriately interact with their surroundings that is not standard treatment or dosage for the patient’s condition. It is important to note that the definition states the medication “is not standard treatment or dosage for the patient’s condition.” Seclusion is defined as the confinement of a patient in a locked room from which they cannot exit on their own. It is generally used as a method of discipline, convenience, or coercion. Seclusion limits freedom of movement because, although the patient is not mechanically or chemically restrained, they cannot leave the area.[2]
Although restraints are used with the intention to keep a patient safe, they impact a patient’s psychological safety and dignity and can cause additional safety issues and, in some cases, death. A restrained person has a natural tendency to struggle and try to remove the restraint and can fall or become fatally entangled in the restraint. Furthermore, immobility that results from the use of restraints can cause pressure injuries, contractures, and muscle loss. Restraints take a large emotional toll on the patient’s self-esteem and may cause humiliation, fear, and anger.[3]
Restraint Guidelines
The American Nurses Association (ANA) has established evidence-based guidelines that a restraint-free environment is considered the standard of care. The ANA encourages the reduction of patient restraints and seclusion in all health care settings. Restraining or secluding patients is viewed as contrary to the goals and ethical traditions of nursing because it violates the fundamental patient rights of autonomy and dignity. However, the ANA also recognizes there are times when there is no viable option other than restraints to keep a patient safe, such as during an acute psychotic episode when patient and staff safety are in jeopardy due to aggression or assault. The ANA also states that restraints may be justified in some patients with severe dementia or delirium when they are at risk for serious injuries such as a hip fracture due to falling.[4]
The ANA provides the following guidelines: When restraint is necessary, documentation of application of the restraint should be done by more than one witness. Once restrained, the patient should be treated with humane care that preserves human dignity. In those instances where restraint, seclusion, or therapeutic holding is determined to be clinically appropriate and adequately justified, registered nurses who possess the necessary knowledge and skills to effectively manage the situation must be actively involved in the assessment, implementation, and evaluation of the selected emergency measure, adhering to federal regulations and the standards of The Joint Commission regarding appropriate use of restraints and seclusion.[5]
Nursing documentation is vital when restraints are applied and includes information such as patient behavior necessitating the restraint, alternatives to restraints that were attempted, the type of restraint used, the time it was applied, the location of the restraint, and patient education regarding the restraint. Frequent monitoring according to agency guidelines and provision of basic needs (food, fluids, and toileting) must also be documented.[6]
Any health care facility that accepts Medicare and Medicaid reimbursement must follow federal guidelines for the use of restraints. These guidelines include the following[7]:
- When a restraint is the only viable option, it must be discontinued at the earliest possible time.
- Orders for the use of seclusion or restraint can never be written as a standing order or PRN (as needed).
- The treating physician must be consulted as soon as possible if the restraint or seclusion is not ordered by the patient’s treating physician.
- A physician or licensed independent practitioner must see and evaluate the need for the restraint or seclusion within one hour after the initiation.
- The patient in seclusion or restraints must be routinely monitored according to agency policy. Generally, the best practice for physical restraints is continuous visual monitoring or visual checks at least every 15 minutes. Some agencies require a 1:1 patient sitter when restraints are applied. Physical restraints should be removed every 1 to 2 hours for range of motion exercise and skin checks.
- Each written order for a physical restraint or seclusion is limited to 4 hours for adults, 2 hours for children and adolescents ages 9 to 17, or 1 hour for patients under 9. The original order may only be renewed in accordance with these limits for up to a total of 24 hours. After the original order expires, a physician or licensed independent practitioner (if allowed under state law) must see and assess the patient before issuing a new order.
In addition to continually monitoring the site of a physical restraint for skin issues, a physical restraint should only be secured to the bed with a quick-release knot in case of emergency.
View a YouTube video[8] of an instructor demonstration of a tying a quick release knot:
Side Rails
Side rails and enclosed beds may also be considered a restraint, depending on the purpose of the device. Recall the definition of a restraint as “a device, method, or process that is used for the specific purpose of restricting a patient’s freedom of movement or access to movement.” If the purpose of raising the side rails is to prevent a patient from voluntarily getting out of bed or attempting to exit the bed, then use of the side rails would be considered a restraint. On the other hand, if the purpose of raising the side rails is to prevent the patient from inadvertently falling out of bed, then it is not considered a restraint. If a patient does not have the physical capacity to get out of bed, regardless if side rails are raised or not, then the use of side rails is not considered a restraint.[9]
Full side rails are generally only found on beds in acute care. In long-term care, beds usually have a transfer loop that is a much smaller side rail. The transfer loop allows the resident to support themselves while repositioning in bed and standing up from the bed. The smaller size of this type of side rail reduces the risk of the resident becoming entrapped and injured from the device. Full side rails may be ordered by the physician if they allow the resident to reposition independently. If a resident’s bed in a long-term care setting has full side rails and they are not used for repositioning, they should always be lowered when care is complete, and a staff member is no longer present in the room. Acute care settings have different regulations regarding full side rails; review specific agency policy.[10]
Hand Mitts
A hand mitt is a large, soft glove that covers a confused patient’s hand to prevent them from inadvertently dislodging medical equipment such as a catheter, feeding tube, or intravenous (IV) catheter. See Figure 8.23[11] for an image of a hand mitt. Hand mitts are considered a restraint by The Joint Commission if they are used under these circumstances:

Figure 8.23
Hand Mitt
- Pinned or otherwise attached to the bed or bedding
- Applied so tightly that the patient’s hands or finger are immobilized
- Are so bulky that the patient’s ability to use their hands is significantly reduced
- Cannot be easily removed by the patient in the same manner it was applied by staff, considering the patient’s physical condition and ability to accomplish this objective
View the following YouTube video for applying hand mitts[12]: Hand Control Mittens With Tie Closure.
Vests
A vest restraint is worn on the upper body and has ties that secure it to a chair or bed frame, allowing the restrained person to sit or lie in bed.
View the following YouTube video on properly using a vest restraint[13]: Criss Cross Vest.
Other Restraints
Common items can be considered restraints when used improperly. A general rule is if any device limits the mobility, freedom of movement, or access to one’s body, it is considered a restraint. The resident must be able to independently remove any device that is utilized when directed to do so. This action shows that the resident can cognitively and physically control their environment. Here are some examples of how common devices can be considered a restraint:
- Wheelchair brakes that are left on with a resident who cannot independently release them are considered a restraint because it prevents the resident from moving freely throughout their environment.
- Lap trays (used for meals or supporting an immobile limb) are considered a restraint if it impairs the resident’s ability to move.
- Self-release seat belts can be used to keep a resident positioned properly in their wheelchair, but the resident must be able to remove the seat belt if asked to do so.
- Gait belts must be removed after residents have completed a transfer. They should not be left on during meals or activities for convenience because they can cause discomfort.
Restraint Alternatives
There are many interventions available to keep residents safe without applying restraints. When a potentially unsafe behavior is occurring, the health care team should look at all the factors surrounding the behavior to determine the root cause. After the root cause is determined, the staff can implement appropriate redirection. Common risks and appropriate interventions include the following:
If a resident continues to attempt to self-transfer without assistance:
- Offer toileting every hour
- Offer the opportunity to lie down after meals
- Assist in ambulation (if their condition permits) throughout the day
- Place a motion alarm in the doorway or near the foot of the bed
- Use a pressure or tab alarm in the wheelchair
If a resident is agitated or aggressive towards other residents:
- Offer an individual activity such as board games, crafts, or movies
- Ambulate or take them for a walk in their wheelchair
- Give them something to hold such as a stuffed animal
- Offer a blanket
- Ask about pain, hunger, or toileting needs
If a resident wanders or wants to leave the facility:
- Allow them to self-propel in wheelchair in a safe area
- Offer an individual activity such as board games, crafts, or movies
- Ambulate or take them for a walk in their wheelchair
- Apply a wanderguard to the wheelchair or their wrist or ankle
Motion sensors, pressure or tab alarms, and wanderguards are all alarms. There are many facilities that choose not to use alarms because they can be disruptive to the environment due to the noise and can reduce the dignity of the resident. If implemented incorrectly, they may not deter the unsafe behavior but merely notify staff the behavior is occurring or has occurred. If an alarm is indicated in the care plan, the NA is responsible for making sure the alarm is functioning and properly placed as indicated in the care plan. Behavioral and environmental interventions, as previously discussed, should be considered before alarms are put in place.
For more information on alarms, view the following YouTube videos:
Wanderguard[14]: Prevent Wandering With Smart Caregiver Fall Prevention and Anti-Wandering Products
Pressure alarm[15]: TL-2020 With Corded Bed Pad
References
- 1.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 2.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 3.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 4.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 5.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 6.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 7.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 8.
- Chippewa Valley Technical College. (2022, December 3). Quick Release Knot. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/S7LbOclRQcw ↵. - 9.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 10.
- This work is a derivative of Nursing Fundamentals by Chippewa Valley Technical College and is licensed under CC BY 4.0 ↵.
- 11.
- 12.
- DeRoyal. (2015, May 31). Hand control mittens with tie closure [Video]. YouTube. All rights reserved. https://youtu
.be/7gCp40b9Bcs ↵. - 13.
- DeRoyal. (2015, March 31). Criss cross vest [Video]. YouTube. All rights reserved. https://youtu
.be/tJ7k8hWzFLI ↵. - 14.
- Smart Caregiver. (2017, May 26). Prevent wandering with Smart Caregiver fall prevention and anti-wandering products [Video]. YouTube. All rights reserved. https://youtu
.be/TTMPmg-atPM ↵. - 15.
- Smart Caregiver. (2021, June 24). TL-2020 with corded bed pad [Video]. YouTube. All rights reserved. https://youtu
.be/JtsCLkEmQ6A ↵.
8.8. SKILLS CHECKLIST: POSITIONING SUPINE TO LATERAL (SIDE-LYING)
- 1.
Gather Supplies: Four pillows
- 2.
Routine Pre-Procedure Steps:
- Knock on the client’s door.
- Perform hand hygiene.
- Introduce yourself and identify the resident.
- Maintain respectful, courteous, and professional communication at all times.
- Provide for privacy.
- Explain the procedure to the client.
- 3.
Procedure Steps:
- Position the bed flat.
- Raise the bed height.
- Raise the side rail on the side of the bed the resident will be facing after repositioning for safety.
- Move to the working side of the bed, which is opposite the side rail that was raised.
- Explain to the resident that you will move them closer to you before turning on the count of three.
- From the working side of the bed using the lift sheet, count to three and move the resident towards you.
- Instruct the resident to move their arm closest to the raised side rail away from their body. If able, the resident should grasp the side rail with the hand closest to you, reaching across their own body.
- Raise the resident’s knee that is closest to you to assist in turning.
- Explain that you will turn the resident towards the side rail on the count of three.
- Count to three and use the lift sheet to turn the resident towards the raised side rail.
- Ensure that the resident’s face never comes close to the side rail or becomes covered by the pillow.
- Check that the resident is not lying on their bottom arm.
- Place a pillow behind the resident’s back, ensuring they will not roll back to the supine position.
- Move to the end of the bed and check that the resident is in correct body alignment.
- Verify that the resident is in the middle of the bed.
- Place a pillow between the resident’s top arm and their rib cage or the bed, ensuring the elbow is not directly on their ribs.
- Place a pillow under the top knee, ensuring the knee is not resting directly on the other knee or the ankle is not on top of the other ankle.
- Adjust the pillow under the resident’s head for comfort.
- 4.
Post-Procedure Steps:
- Check on resident comfort and ask if anything else is needed.
- Ensure the bed is low and locked. Check the brakes.
- Place the call light or signaling device within reach of the resident.
- Open the door and privacy curtain.
- Perform hand hygiene.
- Document repositioning and report any abnormal skin findings to the nurse.
View a YouTube video[1] of an instructor demonstration of positioning from the supine to lateral side-lying position:
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Positioning a Client from the Supine to the Lateral (Side-Lying) Position. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/kIw9IhPhsBA ↵.
8.9. SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH A GAIT BELT
- 1.
Gather Supplies: Gait belt, wheelchair, and nonskid footwear
- 2.
Routine Pre-Procedure Steps:
- Knock on the client’s door.
- Perform hand hygiene.
- Introduce yourself and identify the resident.
- Maintain respectful, courteous, and professional communication at all times. Provide for privacy.
- Provide for privacy. Explain the procedure to the client.
- Explain the procedure to the client.
- 3.
Procedure Steps:
- Check the brakes on the bed to ensure they are locked.
- Remove the foot pedals from the wheelchair if needed.
- Assist the resident to a seated position on the side of the bed with their feet on the floor; allow them to dangle their feet for a few minutes.
- Assist the resident in putting on nonskid footwear.
- Place the gait belt on the resident.
- Position the wheelchair at the head or foot of the bed so the resident will move towards the wheelchair with the stronger side of their body. The wheelchair should touch the side of the bed.
- Lock the brakes on the wheelchair.
- Ask the resident if they feel dizzy or light-headed.
- Face the resident and place each of your feet in front of the resident’s feet to prevent them from slipping.
- Instruct the resident to push up on the bed to aid in standing on the count of three.
- Grasp the gait belt with both hands, with your palms and fingertips pointing up.
- Count to three and assist the resident to stand.
- Assist the resident to pivot.
- Instruct the resident to grasp the arms of the wheelchair when they can feel the back of their knees are in contact with the wheelchair seat.
- Assist the resident to a seated position in the wheelchair.
- Remove the gait belt gently to avoid skin injury.
- Release the wheelchair brakes.
- 4.
Post-Procedure Steps:
- Check on resident comfort and ask if anything else is needed.
- Ensure the bed is low and locked. Check the brakes.
- Place the call light or signaling device within reach of the resident.
- Open the door and privacy curtain.
- Perform hand hygiene.
- Document and report any skin issues, pain with movement, or any other changes noted with the resident.
View a YouTube video[1] of an instructor demonstration of transfer from bed to chair with a gait belt:
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Transfer From Bed to Chair With a Gait Belt. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/pyoHSHef90c ↵.
8.10. SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH SIT-TO-STAND
- 1.
Gather Supplies: Wheelchair, lift, and nonskid footwear. Check agency policy for assistance requirements and the client’s care plan for current transfer status.
- 2.
Routine Pre-Procedure Steps:
- Knock on the client’s door.
- Perform hand hygiene.
- Introduce yourself and identify the resident.
- Maintain respectful, courteous, and professional communication at all times.
- Provide for privacy.
- Explain the procedure to the client.
- 3.
Procedural Steps:
- Position the wheelchair appropriately, remove the foot pedals, and lock the brakes. Provide ample room to rotate the lift from the bed to the wheelchair without hitting other objects.
- Place the transfer sling under the resident’s armpits with the handles facing away from the resident.
- Secure the transfer sling with the seat belt or by crossing the sling straps following manufacturer’s recommendations.
- Raise the bed to allow the legs of the lift to go underneath the bed.
- Open the legs of the lift if the bed allows room to do so.
- Ask the resident to put their feet onto the base of the lift. When bringing the lift closer to the resident, ensure that the arms of the lift do not hit the resident’s head or arms.
- Secure the strap at the base of the lift around the calves of the resident if available.
- Check that the resident’s feet are completely on the base.
- Place the sling behind the resident’s back and under their armpits on both sides. Secure the sling clasp in front of the patient around their chest/waist.
- Connect the transfer sling to the lift ensuring equal length is attached on each side of the sling.
- Instruct the resident to place their hands on the handles of the lift arms.
- Check that the sling remains under both of the resident’s armpits and their arms are outside of the lift arms.
- Ensure the resident is not experiencing any dizziness before they stand.
- Instruct the resident that you will begin raising the lift. Ask them to pull up with their arms and straighten their legs. (If the resident is not currently able to perform these actions, a sit-to-stand should not be used.)
- Use the lift to raise the resident to a standing position.
- Slowly move the lift away from the bed. Open the legs of the lift if they are closed underneath the bed.
- Slowly move the lift towards the wheelchair.
- After the back of the resident’s knees touch the wheelchair seat, explain that you will lower them to the chair. Do not apply the brakes on the lift because they can cause the resident’s legs to be compressed by the lift as they are lowered to the chair.
- While lowering the resident into the wheelchair, assist them to sit all the way back in the wheelchair by guiding the handle on the sling towards the back of the wheelchair seat.
- After the resident is seated in the chair, remove the leg strap and sling from the lift. Instruct the resident to release their hands from the lift.
- Slowly move the lift away from the resident, ensuring the lift does not hit the resident’s head or arms.
- Ask the resident to lean slightly forward and remove the sling.
- Release the wheelchair brakes.
- 4.
Post-Procedure Steps:
- Check on resident comfort and ask if anything else is needed.
- Ensure the bed is low and locked. Check the brakes.
- Place the call light or signaling device within reach of the resident.
- Open the door and privacy curtain.
- Perform hand hygiene.
- Document and report any skin issues, pain with movement, or any other changes noted with the resident.
View a YouTube video[1] of an instructor demonstration of transfer from bed to chair with a sit to stand:
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Transfer from Bed to Chair with a Sit to Stand. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/zs_CIYylxtU ↵.
8.11. SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH MECHANICAL LIFT
- 1.
Gather Supplies: Mechanical lift, lift sling, second person to assist, and a wheelchair. Review agency policy for mechanical lifts. NOTE: The driver of the lift must be at least 18 years old.
- 2.
Routine Pre-Procedure Steps:
- Knock on the client’s door.
- Perform hand hygiene.
- Introduce yourself and identify the resident.
- Maintain respectful, courteous, and professional communication at all times.
- Provide for privacy.
- Explain the procedure to the client.
- 3.
Procedure Steps:
- Raise the bed to a working height.
- Instruct the resident to cross their arms over their chest to avoid rolling on top of their arm.
- Using the lift sheet, roll the resident to one side. Coordinate movement with the resident and the second assistant to avoid injury.
- Position the lift sling underneath the resident from the shoulders to the buttocks. Fan-fold the sling in the middle to allow the second assistant to pull it through on the other side. The handles should be facing away from the resident.
- Ensure the lift sling is on top of the lift sheet.
- Inform the resident they will be rolling over the gathered fabric of the sling.
- (Second assistant) Using the lift sheet, initiate rolling the resident towards the first assistant with the resident’s arms still crossed, coordinating movement with the resident and first assistant.
- (Second assistant) Pull the lift sling from underneath the resident, smoothing out any wrinkles.
- Using the lift sheet, gently roll the resident back to the supine position.
- Check that the resident is positioned in the center of the lift sling and their head and knees will be properly supported when lifted.
- Check the body alignment of the resident.
- Move the full-body mechanical lift into position over the resident, ensuring the lift does not come into contact with any part of the resident.
- Raise the head of the bed to avoid pulling on the sling when connecting it to the lift.
- Hook the top loops of the sling to the lift per manufacturer’s guidelines, ensuring the loops are the same lengths on each side.
- Hook the bottom loops of the sling to lift per manufacturer’s guidelines, ensuring the loops are the same lengths on each side.
- Position the wheelchair appropriately and lock the brakes. Provide ample room to rotate the lift from the bed to the wheelchair without hitting other objects.
- Recline the wheelchair slightly if able.
- Instruct the resident to cross their arms over their chest.
- Prepare to support the resident’s feet by having the second assistant move to the same side of the bed as the driver and the lift.
- Inform the resident you will be raising the lift and moving them to the wheelchair.
- Raise the lift until the resident is no longer in contact with the bed while the second assistant guides the resident’s feet.
- Position the resident over the wheelchair with the main support of the lift to one side, thus avoiding the resident’s feet coming into contact with the lift support.
- After the driver of the lift moves behind the wheelchair, have the resident grasp the handles on the lift sling.
- Instruct the resident you will be lowering the lift sling.
- (Second assistant) Lower the lift while the driver gently pulls up on the sling to get the resident’s back positioned upright and against the back of the wheelchair.
- (Second assistant) Guide the resident’s feet to keep their body aligned and avoid coming in contact with the left.
- Remove the sling from the lift after the resident is properly seated.
- Carefully move the lift away from the resident, avoiding the resident’s head and limbs from coming into contact with the lift.
- Tuck the lift sling into the wheelchair, keeping the fabric smooth to avoid skin issues and keeping loops away from any moving parts of the wheelchair.
- 4.
Post-Procedure Steps:
- Check on resident comfort and ask if anything else is needed.
- Ensure the bed is low and locked. Check the brakes.
- Place the call light or signaling device within reach of the resident.
- Open the door and privacy curtain.
- Perform hand hygiene.
- Document and report any skin issues, pain with movement, or any other changes noted with the resident.
View a YouTube video[1] of an instructor demonstration of transfer from bed to chair with a mechanical lift:
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Transfer from Bed to Chair with a Mechanical Lift. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/sqkE7MNndyE ↵.
8.12. SKILLS CHECKLIST: AMBULATION FROM WHEELCHAIR
- 1.
Gather Supplies: Gait belt, wheelchair, nonskid footwear, and assistive devices if needed (walker or cane)
- 2.
Routine Pre-Procedure Steps:
- Knock on the client’s door.
- Perform hand hygiene.
- Introduce yourself and identify the resident.
- Maintain respectful, courteous, and professional communication at all times. Provide for privacy.
- Provide for privacy. Explain the procedure to the client.
- Explain the procedure to the client.
- 3.
Procedure Steps:
- Check the brakes on the wheelchair to ensure they are locked.
- Verify the resident is wearing nonskid footwear.
- Properly place the gait belt around the resident’s waist.
- Check the gait belt for tightness by slipping your fingers between the gait belt and the resident.
- Ask the resident if they feel dizzy or light-headed.
- Face the resident and place each of your feet in front of the resident’s feet to prevent them from slipping.
- Instruct the resident to push up on the wheelchair arms on the count of three to assist with standing.
- Count to three and assist the resident to a standing position.
- Provide the resident’s assistive device, as needed.
- Move to the weak side of the resident, slightly behind them. Hold the gait belt with your palms and fingertips pointing upwards.
- Stabilize the resident as they ambulate for the desired duration.
- Assist the resident to pivot/turn in front of the wheelchair.
- Ensure the wheelchair brakes are locked.
- Instruct the resident to grasp the arms of the wheelchair when the back of their knees touch the wheelchair seat.
- Assist the resident to a seated position in the wheelchair.
- Remove the gait belt.
- Release the wheelchair brakes.
- 4.
Post-Procedure Steps:
- Check on resident comfort and ask if anything else is needed.
- Ensure the bed is low and locked. Check the brakes.
- Place the call light or signaling device within reach of the resident.
- Open the door and privacy curtain.
- Perform hand hygiene.
- Document and report any skin issues, pain with movement, or any other changes noted with the resident.
View a YouTube video[1] of an instructor demonstration of ambulation from a wheelchair:
References
- 1.
- Chippewa Valley Technical College. (2022, December 3). Ambulation From a Wheelchair. [Video]. YouTube. Video licensed under CC BY 4.0. https://youtu
.be/jtj95sPrc_k ↵.
VIII. GLOSSARY
- Ambulation
A medical term used for walking.
- Bariatric lifts
Mechanical lifts that support a client weighing 600 or more pounds.
- Body alignment
Good posture principles that prevent musculoskeletal injuries.
- Bony prominences
Areas of the body where a bone lies close to the skin’s surface, such as the back of the head, shoulders, elbows, heels, ankles, tops of the toes, hips, and coccyx.
- Chemical restraint
A drug used to manage a patient’s behavior, restrict the patient’s freedom of movement, or impair the patient’s ability to appropriately interact with their surroundings, that is not standard treatment or dosage for the patient’s condition.
- Coccyx
Tailbone.
- Dangle
Sitting up on the edge of bed for a few minutes before standing to prevent orthostatic hypotension and dizziness.
- Foam boots
Specialized soft boots used to support the ankles and keep the heels floated off the bed.
- Foot cradle
A device used to keep the sheets and blankets off the tops of a client’s toes.
- Fowler’s position
A position where the client is lying on their back with their head elevated between 30 and 90 degrees.
- Friction
Injury caused to skin when it is rubbed by clothing, linens, or another body part.
- Hand mitt
A large, soft glove that covers a confused patient’s hand to prevent them from inadvertently dislodging medical equipment such as a catheter, feeding tube, or intravenous (IV) catheter.
- Immobility
The loss of independent control of one’s body to change positions and function safety within the environment.
- Lateral (side-lying) position
A position that places the client on their left or right side to relieve pressure on the coccyx or increase blood flow to the fetus in pregnant women.
- Mobility
The ability to move one’s body parts, change positions, and function safely within the environment. It is one of the most important factors for remaining independent.
- Orthostatic hypotension
A sudden drop in blood pressure that can cause clients to feel dizzy and increase their risk for falls.
- Orthotic
A support, brace, or splint used to support, align, prevent, or correct the function of movable parts of the body.
- Physical therapists
Health specialists who evaluate and treat movement disorders.
- Pressure injuries
Localized damage to the skin or underlying soft tissue, usually over a bony prominence, as a result of intense and prolonged pressure and/or shear.
- Prone position
A position where the client is placed on their stomach with their head turned to one side.
- Prosthetics
An addition or attachment to the body that replicates the function of a lost or dysfunctional limb.
- Restraints
Devices used in health care settings to prevent patients from causing harm to themselves or others when alternative interventions are not effective.
- Seclusion
The confinement of a patient in a locked room from which they cannot exit on their own. It is generally used as a method of discipline, convenience, or coercion.
- Shear
Injury to skin that occurs when skin moves one way, but the underlying bone and muscle stay fixed or move the opposite direction.
- Sims’ position
A position similar to the lateral position, but the client is always placed on their left side and their left arm is placed behind their body.
- Skin tear
A separation of skin layers caused by shear, friction, and/or blunt force.
- Supine position
A position where the client is lying flat on their back.
- Transfer status
How a resident moves from one place to the other, such as from a bed to wheelchair or a wheelchair to toilet.
- Transfer status orders
Orders that establish how much assistance is required for moving a client based on how much body weight they can independently bear and how much weight an assistant is required to support. Transfer status orders include independent, contact-guard-assist (CGA), 1 assist (1A), 2 assist (2A), sit-to-stand lift, or full-body mechanical lift.
- Vertigo
A sensation that the room is spinning.
- INTRODUCTION TO UTILIZE PRINCIPLES OF MOBILITY TO ASSIST CLIENTS
- MOVING AND POSITIONING CLIENTS
- PROMOTING JOINT MOBILITY AND ACTIVITY
- ASSISTING CLIENTS TO TRANSFER
- ASSISTING WITH AMBULATION
- APPLYING PROSTHETICS AND ORTHOTICS
- RESTRAINTS AND RESTRAINT ALTERNATIVES
- SKILLS CHECKLIST: POSITIONING SUPINE TO LATERAL (SIDE-LYING)
- SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH A GAIT BELT
- SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH SIT-TO-STAND
- SKILLS CHECKLIST: TRANSFER FROM BED TO CHAIR WITH MECHANICAL LIFT
- SKILLS CHECKLIST: AMBULATION FROM WHEELCHAIR
- LEARNING ACTIVITIES
- GLOSSARY
- Chapter 8: Utilize Principles of Mobility to Assist Clients - Nursing AssistantChapter 8: Utilize Principles of Mobility to Assist Clients - Nursing Assistant
Your browsing activity is empty.
Activity recording is turned off.
See more...