Licensed under a Creative Commons Attribution 4.0 International License. To view a copy of this license, visit https://creativecommons.org/licenses/by/4.0/.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Open Resources for Nursing (Open RN); Ernstmeyer K, Christman E, editors. Nursing Skills [Internet]. Eau Claire (WI): Chippewa Valley Technical College; 2021.
5.1. MATH CALCULATIONS INTRODUCTION
Learning Objectives
- Accurately perform calculations using decimals, fractions, percentages, ratios, and/or proportions
- Convert between the metric and household systems
- Use military time
- Use dimensional analysis
- Accurately solve calculations related to conversions, dosages, liquid concentrations, reconstituted medications, weight-based medications, and intravenous infusions and evaluate final answer to ensure safe medication administration
The Institute of Medicine (IOM) has estimated that the average hospitalized patient experiences at least one medication error each day. Nurses are the last step in the medication administration process before the medication reaches the patient, so they bear the final responsibility to ensure the medication is safe. To safely prepare and administer medications, the nurse performs a variety of mathematical calculations, such as determining the number of tablets, calculating the amount of solution, and setting the rate of an intravenous infusion.[1]
Dosage calculation in clinical practice is more than just solving a math problem. Nurses must perform several tasks during drug calculations, such as reading drug labels for pertinent information, determining what information is needed to set up the math calculation, performing the math calculations, and then critically evaluating the answer to determine if it is within a safe dosage range for that specific patient. Finally, the nurse selects an appropriate measurement device to accurately measure the calculated dose or set the rate of administration.[2] This chapter will explain how to perform these tasks related to dosage calculations using authentic problems that a nurse commonly encounters in practice.
References
- 1.
- 2.
- Ozimek, D. (2019). Teaching dosage calculations: Strategies for narrowing the theory-practice gap [Webinar]. The University of Texas at Austin Charles A. Dana Center. https://www
.utdanacenter .org/our-work/higher-education /collaborations /math-for-nurses ↵.
5.2. MATH BASIC CONCEPTS
Measuring Devices
Depending on the type and amount of medication that is being administered, there are several devices used for measuring and administering medications.
A medication cup that is composed of plastic or paper is used to hold and dispense oral medications to a patient. A paper cup is used to administer nonliquid medications, such as tablets or capsules. A plastic medication cup is used to dispense both liquid and nonliquid medications, and calibrated cups are also used to measure liquid medications prior to administration. Calibrated medication cups have labelled measurements such as ounces (oz), cubic centimeters (cc), milliliters (mL), teaspoons (tsp), and tablespoons (Tbs). See Figure 5.1[1] for an image of a calibrated medication cup.

Figure 5.1
Medication Cups
Oral syringes are used to administer liquid medications via the oral route, especially to children, because they allow for precise measurement of small doses. See Figure 5.2[2] for an image of an oral syringe. Oral syringes have different tips than syringes used for injections.

Figure 5.2
Oral Syringes
Syringes are used when administering medications through the parenteral route (i.e., intradermally, subcutaneously, intramuscularly, or intravenously). There are also syringes specifically developed for oral medication administration. Oral medication syringes are commonly orange in color and have a tip that will not allow the oral syringe to be connected to an intravenous injection port. Syringes used for injections are available in many sizes and are selected by the nurse based on the type of injection and the type of medication administered. Both luer lock and slip tip syringes are commonly available for parenteral use. Luer lock syringes have a threaded syringe tip that allow the syringes to be screwed into an injection port. Slip tip syringes do not have a locking mechanism or screw-on connection. Slip tip syringes can be easily attached and removed from different injection devices. Many slip tip syringes are found in foley catheter insertion kits. Common syringe sizes range from 1 mL to 60 mL. See Figure 5.3[3] for an image comparing various sizes of syringes. Syringes are calibrated based on the volume they hold. For example, a 1-mL syringe is calibrated in hundredths and a 3-mL syringe is calibrated in tenths. Syringes that hold larger volumes, such as 5-, 10-, and 12-mL syringes are usually calibrated in fifths (two tenths). Large syringes, such as 60-mL syringes, are calibrated in whole numbers.

Figure 5.3
Various Sizes of Syringes
Special syringes are used to administer insulin and are calibrated in units. See Figure 5.4[4] for an image of an insulin syringe. Insulin syringes are easily identified by a standard orange cap.
Figure 5.4
Insulin Syringe
References
- 1.
- “Medication Cups" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 2.
- “Oral Syringes 3I3A0820.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 3.
- “Syringes 3I3A0446.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 4.
- “Insulin Syringe 3I3A0783.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
5.3. MILITARY TIME
Military time is a method of measuring the time based on the full 24 hours of the day rather than two groups of 12 hours indicated by AM and PM. It is also referred to as using a 24-hour clock. Using military time is the standard method used to indicate time for medication administration. The use of military time reduces potential confusion that may be caused by using AM and PM and also avoids potential duplication when giving scheduled medications. For example, instead of stating medication is due at 7 AM and 7 PM, it is documented on the medication administration record (MAR) as due at 0700 and 1900. See Figure 5.5[1] for an example clock and Table 5.3 for a military time conversion chart.

Figure 5.5
Military Time Clock
- Conversion of an AM time to military time simply involves removing the colon and adding a zero to the time. For example, 6:30 AM becomes 0630.
- Conversion of a PM time to military time involves removing the colon and adding 1200 to the time. For example, 7:15 PM becomes 1915.
Table 5.3
Military Time Conversion Chart
| Normal Time | Military Time | Normal Time | Military Time |
|---|---|---|---|
| 12:00 AM | 0000 | 12:00 PM | 1200 |
| 1:00 AM | 0100 | 1:00 PM | 1300 |
| 2:00 AM | 0200 | 2:00 PM | 1400 |
| 3:00 AM | 0300 | 3:00 PM | 1500 |
| 4:00 AM | 0400 | 4:00 PM | 1600 |
| 5:00 AM | 0500 | 5:00 PM | 1700 |
| 6:00 AM | 0600 | 6:00 PM | 1800 |
| 7:00 AM | 0700 | 7:00 PM | 1900 |
| 8:00 AM | 0800 | 8:00 PM | 2000 |
| 9:00 AM | 0900 | 9:00 PM | 2100 |
| 10:00 AM | 1000 | 10:00 PM | 2200 |
| 11:00 AM | 1100 | 11:00 PM | 2300 |
Practice Problems: Military Time
Practice converting military time using the following problems. The answers are found in the Answer Key (Math Calculations Chapter section) at the end of the book.
- 1.
A patient has a medication scheduled for 1930. What time does this indicate? Include AM or PM.
- 2.
As you prepare to administer a PRN dose of pain medication, you notice the previous dose was administered at 0030. What time does this indicate? Include AM or PM.
- 3.
You administer medication to a patient at 9 AM. How should this be documented in military time?
- 4.
You administer medication to a patent at 10 PM. How should this be documented in military time?
References
- 1.
- "Military Time Clock 3I3A0711.jpg" by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
5.4. EQUIVALENCIES
The nurse performs a variety of calculations in the clinical setting including intake and output conversions, weight conversions, dosages, volumes, and rates. The metric system is typically used when documenting and performing calculations in the clinical setting. Dosages may be calculated and converted into micrograms (mcg), milligrams (mg), milliequivalents (mEq), and grams (gm); volumes may be calculated in cubic centimeters (cc), milliliters (mL), and liters (L); and rates may be calculated in drops per minute (gtt/min), milliliters per hour (mL/hr), or units per hour (units/hr). Each of these types of calculations will be described in the following sections. Let’s begin by discussing equivalencies.
Equivalency is a mathematical term that refers to two values or quantities that are the same amount. For example, one cup is equivalent to eight ounces. Nurses must memorize common household and metric equivalents to perform drug calculations and convert quantities easily.
Household Equivalencies
The household system of measurement is familiar to patients and includes drops, teaspoons, tablespoons, ounces, cups, and pounds. See Table 5.4a for common household measurement conversions and abbreviations that must be memorized by nurses.
Table 5.4a
Common Household Conversions
| Measurement and Abbreviation | Common Conversions |
|---|---|
| drop (gtt) | 10, 12, 15 or 20 gtt = 1 mL |
| microdrop (mcgtt) | 60 mcgtt = 1 mL |
| teaspoon (tsp) | 1 tsp = 5 mL |
| tablespoon (Tbsp or Tbs) | 1 Tbsp = 3 tsp = 15 mL |
| ounce (oz) | 1 oz = 30 mL |
| pound (lb) | 1 lb = 16 oz |
| cup (C) | 1 C = 8 oz = 240 mL |
| pint (pt) | 1 pt = 2 C |
| quart (qt) | 1 qt = 4 C |
| gallon (gal) | 1 gal = 4 qt |
Metric Equivalencies
The metric system is organized by units of 10. The basic units of measurement in the metric system include meter for length, liter for volume, and gram for weight. The decimal point is easily moved either to the right or left with multiplication or division in units of 10. For example, there are 1,000 mL in 1 liter, and 0.5 liters is the same as 500 mL. See Table 5.4b for a metric equivalency chart.
When converting to a smaller unit, the decimal moves to the right →→→→→→→→→→
When converting to a larger unit, the decimal moves to the left. ←←←←←←←←←←←
Table 5.4b
Common Metric Equivalencies in Health Care
|
Kilo-
1000 units |
Hecto-
100 units |
Deca-
10 units |
1
Unit |
Deci-
0.1 units |
Centi-
0.01 units |
Milli-
0.001 units |
Nurses often need to convert household measurements to metric equivalents or vice versa. See Table 5.4c for common metric conversions that nurses must memorize.
Table 5.4c
Common Metric Conversions in Health Care
| Metric Measurement | Common Conversions |
|---|---|
| 1 kilogram (kg) | 1 kg = 2.2 pounds = 1000 grams |
| 1 centimeter (cm) | 1 in = 2.54 cm = 25.4 mm |
| 37 degrees Celsius | 98.6 degrees F |
| 1 liter | 1000 mL = 1000 cc |
| 1 gram | 1000 mg |
| 1 mg | 1000 mcg |
Table 5.4 d
Common Standard Conversions in Health Care
| Standard Measurement | Common Conversions |
|---|---|
| 1 tsp | 5 mL |
| 1 Tbsp | 15 mL |
| 1 ounce | 30 mL |
Other Measurements
The nurse encounters other miscellaneous measurements in practice, such as:
- Units (U): Units are used in insulin, heparin, and pitocin, dosages.
- International Units (IU): International units are used for vitamins, such as Vitamin D 600 IU.
- Milliequivalents (mEq): Milliequivalents are used in electrolyte replacement, such as Potassium 40 mEq.
- Percentages: Percentages are used in intravenous (IV) fluids, such as 0.9% Normal Saline IV fluid, meaning 9 g of NaCl are diluted in 1000 mL water.
- Ratios: Ratios are used in medications such as Epinephrine 1:1000, meaning 1 gram of Epinephrine is diluted in 1000 mL of fluid (equivalent to 1 mg/mL).
Practice Problems: Household and Metric Equivalents
Practice converting household and metric equivalents using the following problems and referencing Tables 5.4a-c. The answers are found in the Answer Key (Math Calculations Chapter section) at the end of the book.
- 1.
A prescription for a child is written as 1 teaspoon every 4 hours. How many milliliters (mL) will you draw up in an oral syringe?
- 2.
A patient’s prescription states to administer one ounce of medication. How many milliliters will you measure in the medication cup?
- 3.
A patient’s prescription states to administer 0.5 grams of medication. How many milligrams will you administer?
- 4.
A baby weighs 3.636 kilograms. How many grams does this convert to?
- 5.
A patient’s pupils are 7 mm in size. How many centimeters does this convert to?
References
- 1.
- RegisteredNurseRN. (2015, February 4). What is the metric table for nursing calculations? [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/aGMLRnWGanM ↵. - 2.
- RegisteredNurseRN. (2015, February 5). Metric conversions made easy | How solve in metric conversions w/ dimensional analysis (Vid 1). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/0N6SmKVWZdI ↵.
5.5. ROUNDING
Follow agency policy for rounding. When performing calculations, do not round until calculating the final answer. Dosages of oral liquid medications for adults are typically rounded to the tenth for doses over 1 mL, with 0.05 and above rounding up and 0.04 and lower rounding down. For example, 17.276 rounds to 17.3, and 17.248 rounds to 17.2. For doses less than 1 mL, the dosage is rounded to the hundredth. For example, 0.0467 rounds to 0.05.
For pediatric patients, it is important to be as precise as possible to avoid medication errors. Oral liquid medications less than 1 mL should be rounded to the hundredth. For example, 0.276 rounds to 0.28, and 0.243 rounds to 0.24.
When rounding, it is also important to use critical thinking to evaluate your final answer. For example, a drop cannot be administered as a fraction of a drop, so drops are rounded to the nearest whole number.
Avoiding Medication Errors with Decimals
There are two very important standards of practice for documenting decimals to avoid medication errors:[1]
- Use leading zeros for decimals (i.e., use 0.6 mg)
- Do not use trailing zeros (i.e., do not use 6.0 mg)
Practice Problems: Rounding
Practice rounding using the following problems. The answers are found in the Answer Key (Math Caculations Chapter) at the end of the book.
- 1.
Round the liquid dose for an adult that is calculated as 6.5349.
- 2.
Round the liquid dose for a child that is calculated as 6.5349.
- 3.
Round the liquid dose for an adult that is calculated as 5.479.
- 4.
Round the liquid dose for a child that is calculated as 5.479.
- 5.
Round the liquid dose for an adult that is calculated as 0.1947.
- 6.
Round the liquid dose for a child that is calculated as 0.1947.
- 7.
Round the liquid dose for an adult that is calculated as 0.1968.
- 8.
Round the liquid dose for a child that is calculated as 0.1968.
References
- 1.
- Saljoughian M. Avoiding medication errors. U.S. Pharmacist. 2020;45(10) https://www
.uspharmacist .com/article/avoiding-medication-errors ↵
5.6. USING DIMENSIONAL ANALYSIS
A common method used to perform calculations with different units of measurement is called dimensional analysis. Dimensional analysis is a problem-solving technique where measurements are converted to equivalent units of measure by multiplying a given unit of measurement by a fractional form of 1 to obtain the desired unit of administration. This method is also referred to as creating proportions that state equivalent ratios. Equivalencies described in Section 5.7 are used to set up ratios with the fractional form of 1 to achieve the desired unit the problem is asking for. The units of measure that must be eliminated to solve the problem are set up on the diagonal so that they can be cancelled out. Lines are drawn during the problem-solving process to show that cancellation has occurred.[1]
When setting up a dosage calculation using dimensional analysis, it is important to begin by identifying the goal unit to be solved. After the goal unit is set, the remainder of the equation is set up using fractional forms of 1 and equivalencies to cancel out units to achieve the goal unit. It is important to understand that when using this problem-solving method, the numerator and denominator are interchangeable because they are expressing a relationship.[2] Let’s practice using dimensional analysis to solve simple conversion problems of ounces to milliliters in Section 5.7 “Conversions” to demonstrate the technique.
Video Review of Dimensional Analysis[3]
References
- 1.
- Esser, P. (2019). Dimensional analysis in nursing. Southwest Technical College. https:
//swtcmathscience .wixsite.com/swtcmath /dimensional-analysis-in-nursing ↵. - 2.
- Esser, P. (2019). Dimensional analysis in nursing. Southwest Technical College. https:
//swtcmathscience .wixsite.com/swtcmath /dimensional-analysis-in-nursing ↵. - 3.
- RegisteredNurseRN. (2015, February 4). Dimensional analysis for nursing & nursing students for dosage calculations nursing school. [Video]. YouTube. All rights reserved. Used with permission. https://youtu
.be/6dyM2puXbgc ↵.
5.7. CONVERSIONS
Ounces to Milliliters
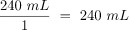
When caring for patients, nurses often need to convert between ounces and milliliters. Although these equivalencies are typically memorized, let’s start with a simple problem of converting ounces to milliliters to demonstrate the technique of dimensional analysis.
Practice Problem #1: Ounces to Milliliters
A patient drank an 8 ounce can of juice. The nurse must document the intake in milliliters. How many milliliters of juice did the patient drink?
Here is an example of how to solve this conversion problem using dimensional analysis.
- 1.
Identify the unit being solved for as the goal. In this example, we want to convert the patient’s oral intake from ounces to milliliters, so we are solving for milliliters (mL):

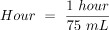
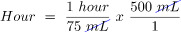
2. Set up the numerator in the first fraction to match the desired unit to be solved. In this case, we want to know how many milliliters should be documented, so mL is placed in the numerator. To complete the fraction, we add information already known. In this example, we know that 30 mL is equivalent to 1 ounce, so 30 mL is added to the numerator and 1 ounce is added to the denominator:
3. Add the second fraction to the equation. When using dimensional analysis, fractions are set up so the same units are diagonal from each other so they cancel each other out, leaving the desired unit. For this problem, the second fraction is set up to include ounces in the numerator so that it will cancel out ounces in the denominator of the first fraction. “8” is then added to the numerator because we know from the problem that the patient consumed 8 ounces. “1” is then added to the denominator because the purpose of the second fraction is to cancel out units:
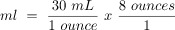
4. Cancel out similar units that are diagonal to each other. After canceling out ounces, we are left with our desired units of mL:
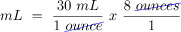
5. Multiply across the numerators and then multiply across the denominators:

6. Divide the numerator by the denominator to get the final answer with the desired goal unit:
Practice Problem #2: Ounces to Milliliters
In a similar manner, dimensional analysis can be used to calculate a patient’s total liquid intake on their meal tray. See Figure 5.6[1] for an example of a patient’s meal tray in a hospital setting.

Figure 5.6
Meal Tray
Sample scenario: Your patient consumed 8 ounces of coffee, 4 ounces of orange juice, and 4 ounces of milk. How many milliliters of intake will you document?
Calculate using dimensional analysis.
- 1.
Add up the total intake in ounces:

2. Start by identifying mL as the goal unit for which you are solving. In this case, we want to know the number of milliliters:

3. Create the first fraction by matching milliliters in the numerator. Then, using known equivalency that 30 mL is equal to 1 ounce, place 30 in the numerator and 1 ounce in the denominator:
4. Create the second fraction to cross out units. You know you want to cross out ounces, so place ounces in the numerator. Then, add the known amount of ounces consumed, which was 16:
5. Multiply across the numerators and then the denominators. Divide the numerator by the denominator of 1 for the final answer in mL:

Video Review of Calculating Intake and Output[2]
Pounds to Kilograms
Converting pounds to kilograms is typically memorized as an equivalency, but let’s practice using the technique of dimensional analysis.
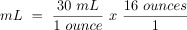
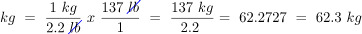
Sample problem: The patient entered their weight as 137 pounds on their intake form. Convert the patient’s weight to kilograms to document it in the electronic medical record. Round your answer to the nearest tenth. Calculate using dimensional analysis.
- 1.
Start by identifying kg as the goal unit for which you are solving. Then, set up the first fraction so that the numerator matches the goal unit of kg. For the denominator, add 2.2 lbs because the known equivalency is 1 kg is equivalent to 2.2 pounds. Set up the second fraction with pounds in the numerator so that pounds will cross out diagonally to eliminate this unit. Then, add the patient’s known weight (137 lb) in the numerator, with 1 in the denominator because the function of this fraction is to cross out units. Multiply across the numerators and then the denominators. Finally, divide the final fraction to solve the problem.
Review the following modules within SWTC’s Dimensional Analysis in Nursing page for more information about solving tablet problems.
Modules 1.0 – 1.4
References
- 1.
- 2.
- RegisteredNurseRN. (2018, February 26). Intake and output nursing calculation practice problems NCLEX review (CNA, LPN, RN) I and O. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/a6ovyZIs9tg ↵.
5.8. TABLET DOSAGE
When tablets are prescribed for a patient, the dosage of the tablets supplied is often different from the prescription, and nurses must calculate the number of tablets to administer. Dimensional analysis can be used to calculate the number of tablets to administer. Let’s practice using dimensional analysis using a practice problem.
Practice Problem: Tablet Dosage
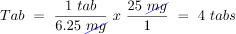
Jane Doe recently had her prescription changed by her provider from Carvedilol 6.25 mg twice daily to Carvedilol 25 mg once daily. Jane shows you her prescription bottle (see Figure 5.7[1]) and asks, “How many pills can I take every day so I can use up what I have before purchasing another refill?” How many 6.25 mg tablets will you instruct Jane to take based on the new prescribed dose of Carvedilol 25 mg once daily?
Figure 5.7
Prescription Bottle of Carvedilol
Solve this question by using dimensional analysis.
- 1.
Start by identifying the goal unit for which you are solving, which is a tablet (tab) in this scenario:

2. Set up the first fraction with tab in the numerator to match the goal unit. From the prescription bottle, we know that one of the supplied tablets has a concentration of 6.25 mg, so place 1 in the numerator and 6.25 mg in the denominator:
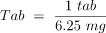
3. Set up the second fraction with the intent to cross out mg, so place mg in the numerator. By reviewing the prescription, we know the new dosage prescribed is 25 mg, so place 25 in the numerator, and 1 in the denominator to cross off units:
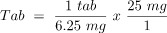
4. Cross out mg diagonally:
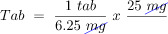
5. Multiply across the numerators and denominators, and then divide the final fraction to solve the problem:
Review the following modules within SWTC’s Dimensional Analysis in Nursing page for more information about solving tablet problems.
Modules 1.5 – 1.7
Please practice tablet dosage calculations with the following interactive learning activity.
References
- 1.
- “Carvedilol Rx Bottle Label Fig. 5.PNG" by Jody Myhre-Oechsle, Chippewa Valley Technical College, Open RN is licensed under CC BY 4.0 ↵.
- 2.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 1 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/HDmRmoi929U ↵. - 3.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 5 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/taMmPMVDzC0 ↵. - 4.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 6 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/vAY1xd2Y9kc ↵. - 5.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug Calculations for nursing students part 7 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/XN1Die8jTE ↵.
5.9. LIQUID CONCENTRATIONS
Medications can also be supplied in liquid instead of tablets or capsules. Liquid concentrations are typically provided in milligrams (mg) per a given number of milliliters (mL). The nurse must calculate how many milliliters (mL) to administer based on the prescribed dose in milligrams (mg). Let’s practice using dimensional analysis to solve how much liquid medication to administer based on the prescription and the medication supplied.
Practice Problem: Liquid Concentrations
John Smith has been prescribed Phenergan as needed every 4-6 hours for nausea and vomiting. John is feeling nauseated and is requesting another dose of Phenergan. It has been 8 hours since the last dose was given. How many mL will you administer?
Prescription: Phenergan 12.5 mg IV PRN every 4 to 6 hours for nausea and vomiting.
Drug Supplied: See Figure 5.8[1] for an image of the label of the drug as it is supplied.
Figure 5.8
Phenergan Medication Label
Solve this question by using dimensional analysis.
- 1.
Start by identifying mL as the goal unit for which you are solving because you need to know how many mL of medication to administer:

2. Set up the first fraction with mL in the numerator to match the goal unit. In this problem, we know from the drug label that 1 mL contains 25 mg of medication, so plug in 1 in numerator and 25 mg in the denominator:

3. Set up the second fraction to cross out mg, so place mg in the numerator. We know from the order that the new dosage prescribed is 12.5 mg, so plug in 12.5 next to mg in the numerator and 1 in the denominator to cross off units:

4. Cross out mg diagonally:
5. Multiply across the numerators and denominators, and then divide the final fraction to solve the problem:

Video Reviews of How to Use Dimensional Analysis to Calculate Oral Medication Dosages[2],[3],[4],[5]:
Review the following modules within SWTC’s Dimensional Analysis in Nursing page for more information about solving liquid problems.
Modules 1.8 – 1.9
Please practice liquid dosing calculations with the following interactive learning activity.
References
- 1.
- “Phenergan Label Fig. 8.PNG" by Jody Myhre-Oechsle, Chippewa Valley Technical College, Open RN is licensed under CC BY 4.0 ↵.
- 2.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 2 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/VHHpGeu9sNw ↵. - 3.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 4 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/f6bpA3usjkI ↵. - 4.
- RegisteredNurseRN. (2015, February 21). Dosage calculations | Nursing drug calculations | Oral medications problems nursing school (Video 3). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/zZ3M747ChrQ ↵. - 5.
- RegisteredNurseRN. (2018, April 25). Weight-based calculations | Drug medication calculations by weight nursing students (Video 6). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/F_LfMcRT8aY ↵.
5.10. RECONSTITUTED MEDICATION
In the previous section, we calculated medication doses that were provided in a liquid form in a given concentration. Medications are also commonly supplied in dry form, such as powders or crystals, that must be reconstituted with fluid before they are administered parenterally by injection. Reconstitution is the process of adding a liquid diluent to a dry ingredient to make a specific concentration of liquid. See Figure 5.9[1] for an example of a vial of medication that requires reconstitution. When reconstituting medications, it is important to follow the reconstitution instructions carefully so the medication is prepared in the correct concentration. When calculating the dosage of reconstituted medication to administer to the patient, the amount of fluid used to dilute the medication must also be considered. Let’s practice using dimensional analysis to determine how much of a reconstituted medication should be administered.

Figure 5.9
Dry Medication Requiring Reconstitution
Practice Problem: Reconstituted Medication
Patient Information:
Name: Liam Vang, DOB: 04/04/20xx, Age 8, Allergies: NKDA, Weight: 60 kg
Provider Order: Cefazolin 500 mg IM every 8 hours
Medication Supplied: See Figure 5.10[2] for the drug label of the medication as it is supplied.
FIgure 5.10
Drug Label of Cefazolin
- 1.
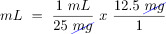
Start by reading the order and the drug label. Liam has an order to receive 500 mg of Cefazolin. The vial of medication in powder form states there are 500 mg per vial. The powder must be reconstituted before it can be administered. The reconstitution instructions on the label state to add 2 mL of sterile water to the vial to reconstitute the powder into a liquid form for injection. The label states that after the powder is reconstituted with the 2 mL of diluent, the concentration of fluid will be 225 mg/mL. See a close-up image of reconstitution instructions in Figure 5.11.[3]

Figure 5.11
Reconstitution Instructions
When setting up the problem, we need to identify the correct information to include in the equation. There are several numbers we may be tempted to try to incorporate into our equation, such as 500 mg per vial, 2 mL diluent, and approximate volume of 2.2 mL. These are numbers specific to the reconstitution process. However, keep in mind that our final goal is to calculate the number of mL of fluid to administer after the medication is reconstituted, so this will be the goal unit. The other piece of important information that the drug label states is that the reconstituted medication will provide a concentration of 225 mg/mL.
2. Start by identifying the goal unit for which you are solving, which is mL to administer as an injection:

3. Set up the first fraction by matching the numerator to the goal unit of mL. In this problem, we know from the drug label that the known concentration of the reconstituted medication is 225 mg per mL, so add 1 mL to the numerator and 225 mg to the denominator:

4. Set up the second fraction with mg in the numerator with the intent to cross off mg diagonally. Look at the given information to determine how it relates to mg. The order tells us to give Liam 500 mg of the medication. Place 500 in the numerator of the second fraction with one in the denominator so that mg will cross off diagonally:
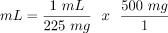
5. Cross off units diagonally. Multiply across the numerators and the denominators, and then divide the final fraction for the answer in mL:
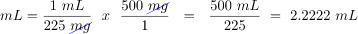
6. Because the patient is a child, round to hundredth for the final answer: 2.22 mL
Please practice medication reconstitution calculations with the following interactive learning activity.
References
- 1.
- 2.
- “Cefazolin Label Fig. 9.PNG" by Jody Myhre-Oechsle, Chippewa Valley Technical College, Open RN is licensed under CC BY 4.0 ↵.
- 3.
- “Reconstitution Instructions.png" by Jody Myhre-Oechsle, Chippewa Valley Technical College, Open RN is licensed under CC BY 4.0 ↵.
- 4.
- Southwest Tech Math/Science Center. (2018, April 25). Entry-level drug calculations for nursing students part 3 – Pharmacology, nursing math*. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/g9nqo-aZuHE ↵. - 5.
- RegisteredNurseRN. (2015, October 7). Dosage calculations made easy | Reconstitution calculation medication problems nursing students (10). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/TK3ZAaMuhYk ↵.
5.11. WEIGHT-BASED CALCULATIONS
Liquid medications are often prescribed based on the patient’s weight. Dimensional analysis can be used to determine the amount of liquid medication the patient will receive based on their weight, the provider order, and the concentration of medication supplied.
Practice Problem: Weight-Based Calculations
Patient Information:
Name: Aidan Smith, DOB: 5/09/20xx, Age 4, Allergies: NKDA, Weight: 22 pounds
Prescription: Tylenol 15mg/kg PO every 4-6 hours for pain or fever
Medication Supplied: See Figure 5.12[1] for the drug label of the medication supplied.

Figure 5.12
Acetaminophen
Aidan had his last dose of Tylenol eight hours ago and now has a fever of 38 degrees Celsius. Calculate the amount of Tylenol you will prepare and administer to Aidan using dimensional analysis.
- 1.
Review the medication label. We see that acetaminophen (Tylenol) is supplied in a concentration of 160 mg in 5 mL.
- 2.
Set up the equation by starting with the goal unit for which we are solving, which, in this case, is milliliters of liquid medication to administer:

3. Set up the first fraction by matching the numerator to mL. Place in the known amount of mL from the drug label, which is 5. Add 160 mg to the denominator because the medication supplied has a known concentration amount of 160 mg in 5 mL:
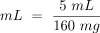
4. Create the second fraction with the intent to cross out units by placing mg in the numerator. Look for other important information in the problem related to mg. The prescription is for 15 mg of acetaminophen (Tylenol) for each kg of weight. Add 15 the numerator and 1 kg in the denominator because 15 mg of Tylenol are ordered for every 1 kg of patient weight:
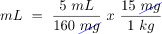
5. Create the third fraction with the intent to cross out kg, so place kg in the numerator. Look for important information in the problem related to kg. The patient’s chart tells us their weight is 22 pounds. Add 1 kg to the numerator and then place 2.2 lb (based on a known equivalency) in the denominator:
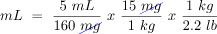
6. Place lb in the numerator of the fourth fraction with the intent to cross out pounds. Look at the information provided and see that the patient weighs 22 pounds. Add 22 pounds in the numerator and 1 in the denominator with the intent to cross off units:
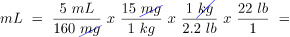
7. Cancel out units diagonally:
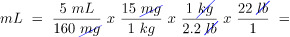
8. After canceling out similar units, we are left with mL, our goal unit, so we can complete the calculation. Multiply across the numerators and the denominators, and then divide the final fraction for the answer:
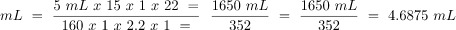
9. Round your final answer. Because the patient is a child, round the final answer to the hundredth, so the final answer is 4.69 mL.
Review the following module within SWTC’s Dimensional Analysis in Nursing Page for more information about solving weight-based problems.
Modules 1.12
Please practice weight-based calculations with the interactive learning activity below.
References
- 1.
- This work is a derivative of tylenol-01
.jpg, courtesy of the U.S.National Library of Medicine. This image is included on the basis of Fair Use. ↵.
5.12. SAFE DOSAGE RANGE
When administering calculated liquid medication, it is important to double-check that the dosage administered is within a safe range. Safe ranges of dosages are provided in drug reference materials. Medication errors often occur in children, who have smaller ranges of safe dosage than adults due to their smaller weight.
When verifying that a dosage is within a safe range based on a patient’s weight, begin by completing the dosage calculation. Then, calculate the low and high ends of the safe dosage range. Finally, verify that the calculated dose is within this range.
Practice Problem: Safe Dosage Range
Declan is an 8-month-old infant who weighs 7 kg. He has been prescribed acetaminophen 100 mg every 4-6 hours PO for a fever. The recommended dosage range for infants is 10-15 mg/kg/dose. Calculate the acceptable dosage range for Declan and determine if the prescribed dose is safe.
- 1.
Calculate the low end of the safe dosage. Start by identifying the goal unit. For this problem we want to know the dose in milligrams:

2. To set up the problem, match the numerator in the first fraction to the desired unit to be solved, which in this case is mg. Based on information known from the problem, we know that the recommended low dose is 10 mg per kg, so add 1 kg to the denominator:

3. Create the second fraction with the intent to cross out units. Place kg in the numerator. Look to the problem for information related to kg. We know that Declan weighs 7 kg, so place 7 in the numerator and 1 in the denominator with the intent to cross off units:
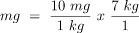
4. Cross off units. Multiply across the numerators and then the denominators, and then divide the final fraction for the final low dose answer in mg:
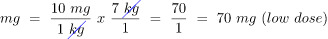
5. Calculate the high dose. Set up a similar equation, but this time using the high dose information of 15 mg per kg:
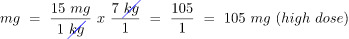
6. Based on the calculations, the safe dosage range for Declan is 70 mg – 105 mg. Compare the prescribed dose to the low- and high-dose range calculations to determine if it is safe. Declan was prescribed 100 mg. It falls within the calculated safe dosage range of 70 – 105 mg, so, yes, this is a safe dose for Declan.
Video Review of Safe Pediatric Dosage Calculations[1]:
Please practice dosage range calculations with the interactive activity below.
References
- 1.
- RegisteredNurseRN. (2016, September 13). Safe dose dosage range pediatric calculations nursing drug math (Video 7). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/QRdIVGaQf7Q ↵.
5.13. INTRAVENOUS INFUSIONS
So far in this chapter, we have practiced using dimensional analysis to determine dosage calculations for medications given orally and parenterally (by injection). Medications can also be administered intravenously (IV). There are two methods for administering intravenous medications: infusion pump or gravity using IV drip tubing.
In the United States, intravenous medications are most commonly administered via an infusion pump for patient safety. When an infusion pump is used to administer IV medications, it is typically programmed by the nurse in milliliters per hour (mL/hour). However, situations may occur when an infusion pump is not available, so the nurse must also know how to calculate drip rates using IV drip tubing to administer a medication by gravity. There are different types of IV drip tubing, and each type provides a specific number of drops of medication per milliliter.
As we perform math calculations related to IV medication administration, we are ultimately ensuring that our patients are receiving the correct dose over the correct period of time to avoid adverse effects from too-rapid or too-slow intravenous administration. Specific math calculations for IV infusion by gravity and IV infusion by pump are further described in the following sections.
5.14. IV INFUSION BY GRAVITY
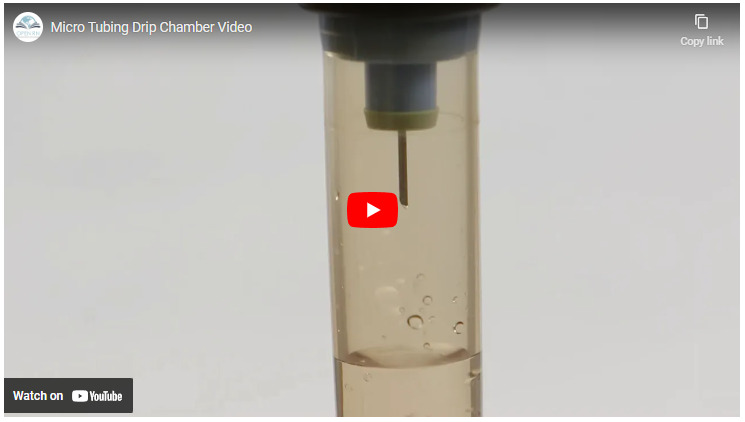
IV drip tubing comes in a variety of sizes called drop factors. The drop factor is the number of drops in one mL of solution using gravity IV tubing. The drop factor is printed on the IV tubing package. Macrodrip tubing includes tubing with drop factors of 10, 12, 15, or 20 drops per mililiter and is typically used to deliver general IV solutions to adults. Microdrip tubing includes tubing with a drop factor of 60 drops per milliliter. It is typically used to deliver precise amounts of medication in small drops to children and infants. See Figure 5.13[1] for an image of microdrip and macrodrip tubing.
Figure 5.13
Microdrip and Macrodrip IV Tubing
Video Review of Micro Tubing Drip Chamber[2]
In the sample problems below, you will be calculating the number of drops needed per minute to achieve the quantity of fluid to be infused per hour in the provider order.
Practice Problem: IV Infusion (Example 1)
Let’s practice calculating the rate of IV infusion by gravity using macrodrip tubing.
Patient Information:
Name: Elaina Dimas, DOB: 12/09/20xx, Age 6, Allergies: NKDA, Weight: 15 kg
Diagnosis: Dehydration
Prescription: 0.9% Sodium Chloride 500 mL IV bolus over four hours
See Figure 5.14[3] for the IV fluid supplied.
Figure 5.14
0.9% Sodium Chloride in 500 mL
See Figure 5.15[4] for IV tubing supplied.
Figure 5.15
Microdrip Tubing
Solve using dimensional analysis.
- 1.
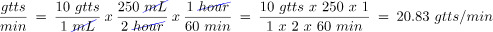
To set up the problem, begin by identifying the goal unit(s) for which we are solving. When calculating infusion rates by gravity, we need to calculate how many drops (gtts) of the solution will be infused each minute. This will allow us to count the actual drops dripping from the tubing and regulate the rate so the volume of infusion is delivered in the time ordered. Set up the problem by identifying the goal unit to solve, but instead of solving for one unit, we will be solving for two units: drops (gtts) and minutes:

2. Set up the first fraction by matching drops (gtts) in the numerator to the goal unit. Review the tubing provided to determine how many drops per minute are administered with this type of tubing. In this example, the tubing is labelled as 60 gtts/mL. Place 60 in the numerator for how many drops are administered by the tubing in 1 mL, and then add 1 mL to the denominator:
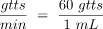
3. Set up the second fraction with the intent to cross off mL, so place mL in the numerator. Look for information provided in the problem related to mL. The prescription is for 500 mL of solution over four hours. Place 500 into the numerator, and place 4 hours in the denominator, and then cross off the mL units:

4. Calculate the minutes to achieve our goal unit of drops per minute. Create the third fraction with hour in the numerator with the intent to cross off hour units. Using equivalencies, we know that 1 hour is equivalent to 60 minutes, so plug in 60 minutes in the denominator. Cancel out hours. Evaluate if we have reached our goal units. This equation now matches the goal of units/min and can be solved:
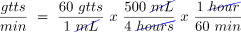
5. Multiply across the numerators and denominators, and then divide the final fraction.

6. The final answer is 125 drops/minute.
Practice Problem: IV Infusion (Example 2)
Let’s practice a second problem using different types of IV drip tubing and a different time to be infused.
Patient Information:
Name: Amber Gomez, DOB: 08/26/20xx, Age 26, Allergies: NKDA, Weight: 50 kg
Provider Order: Lactated Ringers 250 mL IV bolus over 2 hours
Fluid Supplied: See Figure 5.16[5] for the fluid supplied.
Figure 5.16
0.9% Normal Saline 250 mL
Tubing Supplied: See Figure 5.17[6] for the tubing available.

Figure 5.17
Macrodrip Tubing
Round drops to the nearest whole number for a final answer of 21 drops/minute.
Video Review of Solving IV Drip Factor Problems[7]
Review the following module within SWTC’s Dimensional Analysis in Nursing page for more information about solving drop rates.
Module 1.11
Please practice flow rate calculations with the interactive activity below.
References
- 1.
- “Microdrip Tubing” and “Macrodrip Tubing” by Deanna Hoyord, Chippewa Valley Technical College HPS Lab is licensed under CC BY 4.0 ↵.
- 2.
- Open RN Project. (2020, December 9). Micro Tubing Drip Chamber Video. [Video]. YouTube. Licensed under CC BY 3.0. https://youtu
.be/reH50eHpmSQ ↵. - 3.
- “0.9% Sodium Chloride 500 ml” by Deanna Hoyord, Chippewa Valley Technical College HPS Lab is licensed under CC BY 4.0 ↵.
- 4.
- “Microdrip Tubing” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 5.
- “0.9% Sodium Chloride 250 ml” by Deanna Hoyord, Chippewa Valley Technical College HPS Lab is licensed under CC BY 4.0 ↵.
- 6.
- “Macrodrip Tubing” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 7.
- RegisteredNurseRN. (2015, September 28). Dosage calculations for nursing students on IV drip rate factors made easy (Video 4). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/W5VIc6f0fBA ↵.
5.15. IV INFUSION BY PUMP
Intravenous (IV) infusion pumps are the second method used to administer intravenous medications and fluids. See Figure 5.18[1] for an image of an IV pump. Infusion pumps provide an additional safeguard by using a pump to provide an exact amount of fluid per hour to prevent medications from being inadvertently administered too slowly or too quickly. While IV pumps are intended to improve patient safety, the nurse is still responsible for safely setting up the pump. The flow rate using IV pumps is typically calculated in mL/hour. There are many different types of infusion pumps, so the nurse should become familiar with the pumps used at the clinical agency and seek assistance when working with unfamiliar equipment. For additional information about IV infusions, see the “IV Therapy Management” chapter.

Figure 5.18
IV Infusion Pump
Practice Problem: Infusion by Pump (Example 1)
Let’s use the same information from the problem for the patient named Amber Gomez in the “IV Infusion by Gravity” subsection, but instead we will calculate the rate of infusion using an IV infusion pump.
Name: Amber Gomez, DOB: 08/26/xxxx, Age 26, Allergies: NKDA, Weight: 50 kg
Prescription: Lactated Ringers 200 mL IV bolus over 2 hours
Solve using dimensional analysis:
- 1.
Start by identifying the goal units for which you are solving, which is mL per hour:

2. Set up the first fraction by matching mL in the numerator. Look at the known information in the problem related to mL. The prescription is to administer 200 mL IV bolus over 2 hours, so put 200 mL in the numerator and 2 hours in the denominator:
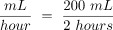
3. Because the units match the goal unit of mL/hour, divide the numerator by the denominator for the final answer:
Practice Problem: Infusion by Pump (Example 2)
Let’s practice another problem calculating flow rate via IV infusion pump, but this time the prescription states the rate in minutes instead of hours.
Patient Information:
Name: Ashley Hanson, DOB: 09/29/20xx, Age 21, Allergies: NKDA
Diagnosis: Dehydration
Prescription: Lactated Ringers 100 mL IV bolus over 30 minutes
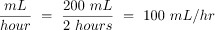
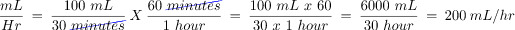
- 1.
Start by setting the goal units being solved. In this case, the pump will still be set for mL per hour:

2. Set up the first fraction by matching the numerator to mL. Look for additional information in the problem related to mL. The order states that 100 mL should be administered over 30 minutes. Place 100 mL in the numerator and 30 minutes in the denominator:
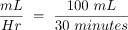
3. Because the pump will be set in mL/hour, convert minutes to hours. Add a second fraction with the intent of crossing off minutes. Place minutes in the numerator so the units will cross out diagonally. Using the known equivalency of 60 minutes in an hour, plug in 60 minutes in the numerator and 1 hour in the denominator. Cross off units diagonally. Multiple across the numerators and the denominators, and then divide for the final answer in mL/hr:
Review the following module within SWTC’s Dimensional Analysis in Nursing page for more information about solving weight-based problems.
Module 1.10
Please practice flow rate by infusion pump calculations below.
References
- 1.
- 2.
- RegisteredNurseRN. (2015, September 30). Dosage calculations for nursing students made easy on IV infusion rate calculations (Video 5). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/rRN3DifaMWo ↵. - 3.
- RegisteredNurseRN. (2015, February 9). Dosage calculations | Nursing drug calculations | IV medications problems nursing school (Vid 2). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/N9gZVo_Sc60 ↵.
5.16. IV COMPLETION TIME
In addition to calculating IV flow rates, nurses also commonly calculate when an infusion will be completed so they will know when to discontinue the infusion or hang another IV bag. Let’s practice calculating how long it will take an IV infusion to complete.
Practice Problem: IV Completion Time (Example 1)
Patient Information:
Name: Amanda Parks, DOB: 09/29/xxxx, Allergies: NKDA, Weight: 70 kg
Prescription: 0.9% Sodium Chloride IV at 75 mL/hr
Fluid Supplied: See Figure 5.19[1] for the IV fluid bag supplied.
Figure 5.19
0.9% Normal Saline in 500 mL
- 1.
Begin by setting up the goal unit being solved for, which is an hour:

2. Set up the first fraction by matching the numerator to hour. Look at the information in the problem related to hours. The order states the IV should be administered at 75 mL per hour, so add 75 mL to the denominator:
3. Set up the second fraction with the intent to cancel out mL, so add mL to the numerator of the second fraction. Look at the information in the problem related to mL. By looking at the bag, we know there are 500 mL to infuse, so place 500 in the numerator and place 1 in the denominator with the intent to cross out units:
4. Cross off units then multiply across the numerators and denominators. Divide the final fraction for the final answer:

5. When performing calculations related to time, it is important to remember that anything after the decimal is a portion of an hour and needs to be converted to minutes. To finish the answer, multiply 60 minutes X 0.6667 = 40.02 minutes. The final answer is the infusion will be completed in 6 hours and 40 minutes.
Practice Problem: IV Completion Time (Example 2)
Now let’s add a start time to the above problem and calculate what time the infusion will end. We determined that the IV infusion will take 6.6667 hours to infuse 500 mL at 75 mL/hr.
Let’s assume the infusion started at 0800.
- 1.
Add the total infusion time to the start time of the infusion, so add 6 hours to the start time of 0800. Use military time and put a “0” before the six for 6 hours:
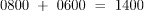
2. Add the minutes to the time:

3. Answer: Our infusion will be complete at 1440.
Video Review of Calculating IV Infusion Times[2]:
Please practice IV completion rates with the interactive learning activity below.
References
- 1.
- “0.9% Sodium Chloride in 500 ml” by Deanna Hoyord, Chippewa Valley Technical College is licensed under CC BY 4.0 ↵.
- 2.
- RegisteredNurseRN. (2015, February 21). IV infusion time calculations nursing | Dosage calculations practice for nursing student (Vid 9). [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/QPAeGgVkxBY ↵.
5.17. MULTI-STEP CALCULATIONS
Sometimes multi-step calculations are required, especially for medications used in critical care. There are many different ways to solve multi-step calculations, so it is important to select a method that works for you that is consistently accurate. Let’s practice a multi-step calculation for a medication supplied in mg/mL but is prescribed based on micrograms (mcg) per kilogram (kg) per minute, and the patient’s weight is provided in pounds.
Practice Problem: Multi-Step Calculations
Patient Information:
Name: Ideen Hanson, DOB: 09/29/19xx, Allergies: NKDA, Weight: 180 lbs
Diagnosis: Hypertension
Prescription: Begin initial infusion of Nipride at 0.5 mcg/kg/min
Medication Supplied: See Figure 5.20[1] for the drug label of the medication supplied.
Figure 5.20
Nipride Label
Problem: What rate (in mL/hr) should the nurse set the pump to begin the infusion?
- 1.
Set up the goal units to solve for, which is mL/hr.

2. Review the problem. The prescription is based on mcg/kg/min. Having three elements can create confusion when setting up the equation using dimensional analysis, so it can be easier to eliminate one element by doing some preliminary steps. First convert the patient weight to kilograms (kg) by dividing 180 pounds/2.2= 81.8181 kg. Now multiply the micrograms (mcg) ordered by weight in kg to determine the amount of medication to administer per minute: 81.8181 x 0.5 mcg = 40.9090 mcg/minute. Use this information as you set up your problem.
3. Start by identifying the unit you are solving for, which is mL/hour. Then set up the first fraction. Match the numerator to mL. Look to the problem for information related to mL. On the drug label, we see that 50 mg of Nipride is supplied in 250 mL of D5W. Place 250 in the numerator, and then 50 mg in the denominator:
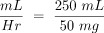
4. Set up the second fraction with the intent to cross off mg by placing 1 mg in the numerator. Based on the known equivalency that 1000 mcg are equal to 1 mg, place 1000 mcg in the denominator:
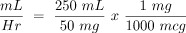
5. Cross off mg diagonally. Set up the third equation with the intent to cross off mcg by placing it in the numerator. Place the information previously calculated, which was 40.9090 mcg/minute:
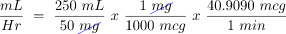
6. Cross off mcg diagonally. Set up the fourth fraction with the intent to cross off minutes. Based on the known equivalency of 60 minutes in 1 hour, place 60 in the numerator and 1 hour in the denominator:
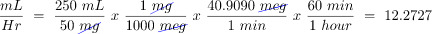
7. Cross off min diagonally. Review the equation to ensure the goal unit has been met. It has been met, so multiply across the numerators and the denominators, and then divide the final fraction:
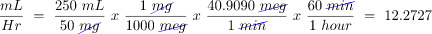
8. Depending on the agency policy and available pump settings, round to 12.27 mL/hour.
References
- 1.
- "Nipride Label" by Jody Myhre-Oechsle, Chippewa Valley Technical College, Open RN is licensed under CC BY 4.0 ↵.
- 2.
- RegisteredNurseRN. (2018, July 26). Heparin drip calculation practice problems for nurses | Dosage calculations nursing. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/10y4gRdnCy8 ↵. - 3.
- RegisteredNurseRN. (2019, February 8). Dopamine IV drip calculation & nursing considerations pharmacology implications. [Video]. YouTube. All rights reserved. Video used with permission. https://youtu
.be/R2XMro13dD0 ↵.
V. GLOSSARY
- Dimensional analysis
Dimensional analysis is a problem-solving technique where measurements are converted to a different (but equivalent) unit of measure by multiplying with a fractional form of 1 to obtain a desired unit of administration.
- Drop factor
The number of drops in one mL of solution when fluids or medications are administered using gravity IV tubing.
- Equivalency
Two values or quantities that are the same amount. For example, one cup is equivalent to eight ounces.
- Macrodrip tubing
Gravity IV tubing with drop factors of 10, 15, or 20 drops per milliliter that are typically used to deliver general IV solutions for adults.
- Medication cup
A small plastic or paper cup used to dispense oral medications. Some plastic medication cups have calibration marks for measuring medication amounts.
- Microdrip tubing
Gravity IV tubing with a drop factor of 60 drops per milliliter.
- Military time
A method of measuring the time based on the full 24 hours of the day rather than two groups of 12 hours indicated by AM and PM.
- Oral syringe
A specific type of syringe used to measure and/or administer medications via the oral route.
- Reconstitution
The process of adding a liquid diluent to a dry ingredient to make a liquid in a specific concentration.
- Syringe
A medical device used to administer parenteral medication into tissue or into the bloodstream. Syringes can also be used to withdraw blood or fluid.
- MATH CALCULATIONS INTRODUCTION
- MATH BASIC CONCEPTS
- MILITARY TIME
- EQUIVALENCIES
- ROUNDING
- USING DIMENSIONAL ANALYSIS
- CONVERSIONS
- TABLET DOSAGE
- LIQUID CONCENTRATIONS
- RECONSTITUTED MEDICATION
- WEIGHT-BASED CALCULATIONS
- SAFE DOSAGE RANGE
- INTRAVENOUS INFUSIONS
- IV INFUSION BY GRAVITY
- IV INFUSION BY PUMP
- IV COMPLETION TIME
- MULTI-STEP CALCULATIONS
- LEARNING ACTIVITIES
- V. GLOSSARY
- Chapter 5 Math Calculations - Nursing SkillsChapter 5 Math Calculations - Nursing Skills
Your browsing activity is empty.
Activity recording is turned off.
See more...