NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Feingold KR, Anawalt B, Blackman MR, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-.
ABSTRACT
Subcutaneous adipose tissue diseases involving adipose tissue and its fascia, also known as adipofascial disorders, represent variations in the spectrum of obesity. The adipofascia diseases discussed in this chapter can be localized or generalized and include a common disorder primarily affecting women, lipedema, and four rare diseases, familial multiple lipomatosis, angiolipomatosis, Dercum disease, and multiple symmetric lipomatosis. The fat in adipofascial disorders is difficult to lose by standard weight loss approaches, including lifestyle (diet, exercise), pharmacologic therapy, and even bariatric surgery, due in part to tissue fibrosis. In the management of obesity, healthcare providers should be aware of this difficulty and be able to provide appropriate counseling and care of these conditions. Endocrinologists and primary care providers alike will encounter these conditions and should consider their occurrence during workup for bariatric surgery or hypothyroidism (lipedema) and in those that manifest, or are referred for, dyslipidemia or diabetes (Dercum disease). People with angiolipomas should be worked up for Cowden’s disease where a mutation in the gene PTEN increases their risk for thyroid and breast cancer. This chapter provides details on the pathophysiology, prevalence, genetics and treatments for these adipofascial disorders along with recommendations for the care of people with these diseases. For complete coverage of all related areas of Endocrinology, please visit our on-line FREE web-text, WWW.ENDOTEXT.ORG.
INTRODUCTION
People with subcutaneous adipose tissue (SAT) diseases have fat within this compartment that grows abnormally in amount or structure, often causing pain and other discomfort. Subcutaneous adipose tissue is loose connective tissue, or adipofascia, which is the most common type of connective tissue in vertebrates. The focus of this chapter is on abnormal SAT that has within it changes in blood vessels, lymphatic vessels, immune cells, mesenchymal stem cells, fascia, interstitial matrix organ, or other components that make up loose connective tissue.
The SAT diseases discussed here include lipedema, which commonly occurs in women, and four rare adipose tissue diseases (RAD): familial multiple lipomatosis, angiolipomatosis, Dercum disease, and Madelung disease (1). Adipose tissue in SAT diseases is resistant to loss by usual measures including extreme dietary changes (both hypocaloric and in macronutrient content) and exercise. Because of this, it is often referred to persistent fat tissue. People with diabetes and/or obesity may have a mixture of normal and persistent fat, making the understanding of SAT diseases by clinicians important in the care of these patients. Persistent fat may also be found in conditions where adipose tissue proliferation occurs, such as during infection, in autoimmune diseases, in those with hypermobile joint disorders, or with exposure to environmental toxins. Information on subcutaneous adipose tissue diseases not discussed here can be found in recent reviews and other Endotext chapters, including those covering lipodystrophies (2-4), cellulite (5), obesity (6,7), and other fat depots such visceral fat (abdominal, perirenal, pericardial), and perivascular fat (8).
Along with the gut (9), subcutaneous adipose tissue is thought to be one of the largest endocrine organs in the body (10). Subcutaneous adipose tissue houses immune cells including monocytes/macrophages, mast cells, and lymphocytes, which produce some of the hormones secreted by fat tissue (11,12). Greater amounts of fat and immune cells result in an inflammatory process that can lead to insulin resistance and slow intrinsic pumping of lymphatic vessels, which, in turn, may prolong inflammation in this tissue (13).
Patients, most often women with swelling, have slow blood flow in, and lymph flow out of, depots of increased fat on the abdomen (14,15) or the gynoid area (hips, thighs and buttocks) (16). Poor blood and lymph flow through fat tissue results in accumulation of fluid, cell waste material, proteins, cells and other metabolic products in the extracellular matrix (ECM) around adipocytes and other components of adipofascia, resulting in a hypoxic environment, especially in adipocytes furthest from their nutrient and oxygen sources. These adipocytes then send signals that recruit more immune cells, resulting in a state of sustained inflammation and tissue degradation. Connective tissue then replaces degraded tissue in a process called fibroplasia or fibrosis. When tissue ischemia occurs or ECM accumulation outpaces its degradation, fibrosis may become unchecked and lead to widespread pathological remodeling of the ECM culminating in permanent scar tissue that completely inhibits flow through the adipose tissue (17).
Obesity is a main cause of densification of fascia and fibrosis development in loose connective tissue (18). The result is a fibrotic mesh around adipocytes and fat lobules which has been well described (19). This sick fat, or adisopathy, increases the risk of metabolic disease (20). In addition, more fibrotic adipose tissue is less responsive to mobilization and reduction attempts through diet, exercise, use of weight loss medications, or bariatric surgery (19,21,22). All the SAT disorders in this chapter have a component of fibrosis in the tissue that prevents loss by usual measures. An important goal is to determine why the loose connective tissue in SAT diseases becomes fibrotic and adisopathic to prevent its occurrence and progression and treat when identified.
LIPEDEMA
Lipedema is a common SAT disease that was first described in 1940 at the Mayo clinic by Drs. Allen and Hines (23). A second seminal paper in 1951 provided a description of lipedema that is still commonly used for clinical diagnosis. Lipedema occurs almost exclusively in women but has been reported rarely in men (24-26).
Lipedema fat is located just under the skin on the limbs including upper arms, hips, buttocks, thighs, lower legs, generally sparing the trunk and feet. It feels nodular when palpated, may be painful to touch, and often has prominent superficial veins. Lipedema tissue can be found under the umbilicus and in some woman, a deeper nodular adipofascia is found in the lateral abdomen. This inner nodularity may reflect changes in the ECM that may be a precursor to lipedema fat if abdominal obesity develops. Disease defining key questions and physical examination characteristics can help to establish the diagnosis of lipedema (Figure 1).
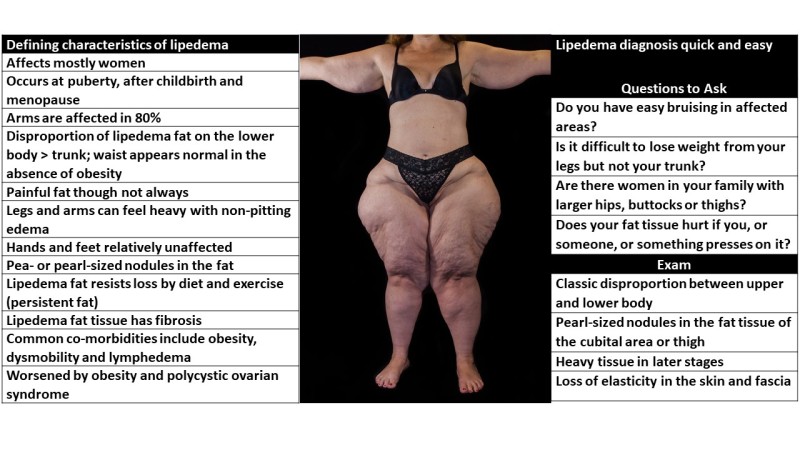
Figure 1.
Characteristics of lipedema that aid in establishment of diagnosis are listed, and many can be seen in the accompanying photo. This patient was diagnosed with Stage 3, type III and IV lipedema without lymphedema (see below). A quick and easy set of questions and exam findings are included to help in diagnosis of women with lipedema.
Classification of Lipedema
Lipedema is classified by stages and types (27). In Stage 1 (Figure 2) the skin surface is normal over an enlarged hypodermis that already has palpable pea-sized nodules in the fat. These pea-sized nodules represent enlargement of and fibrosis in the ECM and in the connective tissue surrounding the fat lobule. Stage 2 skin is uneven with indentations (like cellulite) representing thickening and contraction of underlying connective tissue fibers over increased fat with small to larger hypodermal masses. Lobular extrusions of skin, fat and fascia tissue in Stage 3 represent significant loss of elasticity in the adipofascia drastically inhibiting mobility; blood flow in and lymph flow out of the lobules is reduced resulting in inflammation followed by fibrosis; it is in this stage that fibrosis in the tissue becomes prominent and clearly palpable; fibrosis may or may not affect the skin and the skin may develop thinning and a looser connection to the underlying hypodermis (Figure 1). Modifications of diagnostic criteria for lipedema have been suggested (28).
Lymphedema can occur at any stage, but is more often found in women with Stage 3 lipedema when it is often called lipo-lymphedema or Stage 4 (26). Rather than use this combined term, however, it is preferable to identify the lipemia stage and state whether lymphedema is also present or not. Lymphedema can be identified in women with lipedema by visible swelling of the hands or feet, pitting edema, asymmetry between the size of one limb versus the other, and/or a positive Stemmer sign. A positive Stemmer sign occurs when edema in the limb makes it difficult to pinch skin on the great toe, top of the foot, finger, or dorsal hand. A negative Stemmer sign occurs when only skin is pinched. Other differences between lipedema and lymphedema include symmetry (lipedema tissue occurs symmetrically versus lymphedema, which is usually unilateral), sparing of the hands and feet in lipedema, and report by patients of pain in lipedematous but not lymphedematous tissue.

Figure 2.
Three stages of legs of women with lipedema with subcategories of types. In Stage 1, the skin is smooth, and the legs can appear normal but there is pain, easy bruising and a nodular feel to the fat tissue. In Stage 2, the lipedema fat exhibits a mattress-like pattern indicating fibrosis under the skin that tethers on the skin that can be found on the upper legs (Type II) or extend down to the ankles (Type III). In lipedema Stage 3, there are folds of tissue and the lipedema fat usually extends down to the ankles. For description of the types of lipedema, see Figure 3.
The type of lipedema is defined by its anatomical location (29). Women with Type I lipedema have affected fat on the pelvis, buttocks and hips (saddle bag phenomenon). Women with Type II have affected fat from the buttocks to knees with formation of a tender deposits of fat around the inner side of and below the knee. Women with Type III lipedema have affected fat from the buttocks to ankles where a prominent “cuff,” or ledge, of fat tissue develops. Women with Type IV lipedema fat have affected arms and women with Type V lipedema, a rare type, have only affected lower legs. The most common phenotype of women with lipedema are combinations of II and IV or III and IV (Figure 3).

Figure 3.
Types of lipedema fat. Lipedema fat may be located from the umbilicus down to the bottom of the hips (Type I), down to the medial knees usually including a pad of fat on the inner knee and below the knee (Type II), and down to the ankle (Type III) where a “cuff” of fat develops but spares the dorsal foot. Rarely only the lower legs are affected (Type V). Lipedema affecting the arms alone is rare (Type IV) and, instead, usually is found in combination with Type II or III lipedema. The arms can be variably affected with nodular lipedema fat around the cubit nodes, over the brachioradialis, down the medial arm to the wrist in line with the thumb or 5th digit, the entire lower arm, or the entire arm.
Prevalence of Lipedema
From one specialty lymphedema/obesity clinic in Germany, the prevalence of lipedema in women was estimated to be 11%. Estimates from similar clinics reported prevalence rates of lipedema ranging from 15 to 18.8% (30,31). The prevalence of lipedema in children in the United States in a vascular clinic was reported to be 6.5% (32). Examination of 62 women outside of clinics in Germany found a prevalence rate for all types of lipedema of 39% (33). Using the lowest prevalence estimate in adults of 11%, over 16 million women in the US may be affected with lipedema.
Genetics of Lipedema
The gene or genes underlying lipedema are not known, but another affected immediate family member has been reported in up to 60% of women (34-37). This is compatible with an autosomal dominant inheritance with incomplete penetrance (38) in which an affected parent has a 50% chance of passing lipedema to their child. Supportive of a genetic component, lipedema has been reported in children (32) and as early as infancy by some women. The phenotypic expression of lipedema may vary amongst affected females, especially if there is also obesity in the family. Males that carry the putative gene do not generally exhibit the phenotype, even the fathers of affected daughters.
A mutation in the POU1F1/PIT-1 gene has been shown to cause multiple anterior pituitary deficiencies including thyroxine and growth hormone (GH) deficiency. A PIT-1 mutation was associated with the phenotypic presentation of lipedema in a short mother but not her short son who also carried the mutation, and not in her normal height daughter who did not carry the mutation (39). In mice with GH receptor (GHR) antagonism or lacking GH function, subcutaneous adipose tissue is increased more than other fat depots similar to lipedema in humans (40). No other cases of women with lipedema and a mutation in PIT-1 have been reported to date and women with lipedema are not known to be more likely to have short stature. Classic features of lipedema can be found in people with Williams syndrome caused by a chromosomal 7q11.23 microdeletion of ~1.6 million base pairs, which includes the elastin gene ELN (41). Loss of elasticity results in the reduction of the ability of tissue to contract back after being stretched. Changes in elasticity may therefore allow more fat to grow. These reports suggest there may be more than one genetic mutation causing expression of the lipedema phenotype. Additional genes that may be important in the development of lipedema have been reviewed (42).
Pathophysiology of Lipedema
The cause of lipedema remains unknown. Given the predominance of occurrence in women, it is tempting to consider sex steroids, especially estrogen, as major triggers or contributors of this condition. That knee laxity in women peaks when estrogen levels decline between ovulation and post-ovulation is indictive of estrogen’s effect on connective tissue (43). Other observations that support this effect include reports that lipedema is often first noticed at the time of puberty in young girls and occasionally following pregnancy, when multiple hormone levels are high, including estrogen. Although data in men is sparse, those reported to have lipedema tend to have low testosterone or liver disease, both of which are associated with a relative increase in estrogen levels and therefore a higher estrogen to testosterone ratio (21). While higher levels of testosterone in women with polycystic ovarian syndrome are not protective against lipedema, the adipose tissue in women with this condition may be predisposed to lipedema due to abdominal obesity and inflammation associated with pre-diabetes or diabetes. A causative role for estrogen in the expression of lipedema remains speculative until well-controlled studies are conducted that quantify sex hormone levels, sex hormone receptors, tissue effects, metabolism or sex hormone driven pathways in men and women with lipedema.
Proposed theories to explain lipedema
Theory 1: Abnormal Blood Microvasculature
We and others (36,44,45) have advanced the theory that increased compliance from structural changes in connective tissue results in the ability to hold on to fluids, proteins and other constituents within the ECM and is causally important in the development of lipedema. As in lymphedema, changes in lipedema tissue may occur globally but are likely to also be found regionally in the same limb (46). Over 50% of women with lipedema are thought to have some kind of joint hypermobility consistent with a connective tissue disorder (25). Most women with lipedema and hypermobility fall into the Ehlers Danlos spectrum of disorders, the gene for which is not known (47,48). This hypothesis is consistent with loss of elasticity in tissue resulting in classic features of lipedema in Williams syndrome. Structures in loose connective tissue that contain elastin include blood vessels, lymph nodes, and connective tissue fascia that helps loose connective tissue hold its shape. Initial lymphatic vessels do not have elastic fibers, but elastic fibers support lymphatic vessels to open and close in response to pressure changes in the tissue; loss of elasticity could reduce the ability of lymphatic vessels to open with increased pressure in the ECM. Capillaries do not have elastic fibers but the loose connective tissue surrounding them does; as loose connective tissue enlarges due to growth of adipocytes, capillaries are at risk for dilation and distortion. Dilated and/or distorted capillaries may release their contents into tissues at a higher rate and/or amount in lipedema which initially, lymphatic vessels promptly pump out. Over time, due to compliance in fascia surrounding cells, malfunction of lymphatic vessels, and increased infiltrate leaving altered capillaries fill the ECM, with protein dense and salt-rich (49) deposits that accumulate in the interstitial space clogging flow through the tissue resulting in hypoxia. Hypoxia results in the secretion of hypoxia inducible factor (HIF)-1 by local adipocytes, which stimulates hypoxia response elements on a number of genes including the vascular endothelial growth factor (VEGF) gene and inducing proliferation of stem cells in the adipose tissue (50). Levels of VEGF have been shown to be elevated in women with lipedema (n=9) compared to women without lipedema (n=5) (51), supporting an underlying role for hypoxia in the pathogenesis of lipedema.
Lymph fluid induces adipogenesis when added to adipocytes (52). Therefore, accumulation of pre-lymph fluid in the ECM may be a stimulating factor in adipogenesis. Mesenchymal stem cells isolated from lipedema stromal vascular fraction (SVF), a heterogeneous collection of cells surrounding adipocytes within adipose tissue, contained the connective tissue cell marker CD90+ and endothelial/pericytic marker CD146+ (53). With ~50% of cells in the SVF expressing +CD146+, perivascular cells (pericytes) play a physiological role in vascular development and homeostasis (52). The presence of such high numbers of pericytes is consistent with a chronic capillary injury in lipedema leading to increased need for repair and increased protection of vessels.
As overworked lymphatic vessels eventually lose function, microaneurysms form in the lymphatic vessels in lipedemadous tissue, becoming high risk for breakage and leakage analogous to what happens in lymphedema (54,55). Adipokines, especially large adipokines such as leptin and monocyte chemoattractant protein (MCP)-1, become secreted primarily into the lymphatic system rather than blood capillaries (56). It would then follow that adipokine flow out of lipedema loose connective tissue would be diminished and systemic levels lower (e.g., leptin levels), leading to larger quantities of adipose tissue necessary to achieve weight homeostasis.
Other potential contributors to expression of lipedema include release of lipids from leaky lymphatic vessels in the gut and tissue level (57), which could mediate induction of adipogenesis and have an important role in the development of the loose connective tissue in lipedema (58). Finally, inflammation in response to hypoxia or injuries could facilitate the development of fibrosis within loose connective tissue, not only reducing flow through the tissue further, but also impeding fat loss during weight reduction (19,21,22).
Theory 2: Abnormal Lymphatic Vasculature
Another theory posits that fluid accumulation in the ECM results from a primary defect in lymphatic vessels. Such accumulation enhances permeability issues in surrounding blood microvessels (59). In support, of this hypothesis, one study of women with lipedema and obesity noted a mismatch in the number of lymphatic vessels and the increased numbers of blood vessels in affected tissue (60). Instead there was an increase in the size (area) and area/perimeter ratio of the lymphatic vessels. Increased angiogenesis but fewer numbers and dilated lymphatic vessels has also been reported in a diet-induced obesity model in mice (61). In another supportive study of lipedemadous tissue free of lymphedema, an expansion in the size of lymphatic vessels but no significant changes in transport in of lymphatic fluid was reported (62). However, against this hypothesis of a primary defect in lymphatic tissue as the proximal cause of lipedema is that lymphatic vessel function as determined by lymphangioscintigraphy appears normal in many women with early stages of lipedema and only later can reductions in lymphatic flow rate or function be detected in many women with late stage lipedema (54,63,64).
Markers of Obesity, Cardiometabolic Health, and Aortic Disease in Women with Lipedema
Hypertrophic adipocytes, a marker of an inflammatory environment at risk for insulin resistance and other metabolic dysfunction, are reported in loose connective tissue in lipedema from women regardless of whether they were obese or not (58,65). Adipogenesis has also been identified in lipedema loose connective tissue (58) as has hypertrophy and hyperplasia of adipocytes in people who developed obesity after lifestyle changes. Unhealthy hypertrophic adipocytes undergo necrosis and become surrounded by macrophages that phagocytize the dead adipocytes forming crown like structures on histological exams of tissue. Crown-like structures have also been found in the loose connective tissue of women with lipedema (53,58).
Adipose tissue stem cells collected from subcutaneous adipose tissue from people with obesity have reduced adipogenic potential and proliferative ability (66). The same reduction in adipogenic potential including a reduced capacity to produce leptin by cells in culture was found for adipose tissue removed by tumescent liposuction from women with lipedema compared to women without lipedema (67). These data support the possibility that even in early stages of lipedema when BMI is in the non-obese range, lipedema fat tissue shares characteristics of adipose tissue taken from people with obesity. Thus, even though femoral adipose tissue is known to be cardioprotective (68), this association weakens in later stages of lipedema. The later the stage, the greater the obesity and metabolic risk, including lower high density lipoprotein (HDL) cholesterol levels, higher diastolic and systolic blood pressures, higher reported history of hypertension, and higher percentages of pre-diabetes (69). As such women with advanced lipedema should be closely monitored for these conditions as part of their ongoing care.
Women with lipedema are thought to have a connective tissue disease along the spectrum of hypermobile Ehlers Danlos. Transthoracic 2D echocardiography (2DE) and Doppler imaging revealed that women with Stage 2 lipedema in their early 40s with BMI ~30 kg/m2 had impaired left ventricular apical rotation and left ventricular twist compared to people with lymphedema and those without either disease (70). Another paper by the same group used 2DE and Doppler imaging demonstrated enlarged ascending aortic systolic and diastolic diameters resulting in aortic stiffness in women with lipedema compared to controls (44). Individuals with Williams syndrome with loss of elasticity and features of lipedema also have aortic stiffness (71). These cardiac changes may reflect an underlying connective tissue disorder in women with lipedema and the possible need for cardiovascular screening even if lipid levels and other markers of metabolic syndrome are normal.
Imaging of Lipedema
There are currently no imaging exams that can be used to definitively differentiate lipedema fat from non-lipedemadous adipose tissue. However, some imaging studies may be useful. Nuclear medicine lymphangioscintigraphy (NM LAS) may be helpful in differentiating the presence of lymphedema in patients with lipedema. Flow of Technetium-99m-sulfur colloid injected dermally and taken up by the lymphatic vessels starting at the toe or finger webbing can be normal in lipedema (72), or the lymphatics can be tortuous especially below the knee (73). Other authors found slower lymphatic flow and a marked asymmetry of the lymphatic system in women with lipedema as compared with women without lipedema (74,75).
Dual energy X-ray absorptiometry scans (DEXA) can be used for assessing whole body composition including regional fat mass and lean body mass in addition to bone mineral density; some scanners also estimate visceral fat mass. One study suggested that DEXA can be used to strengthen the confirmation of a diagnosis of lipedema in women, differentiating them from women without lipedema by a cutoff value of 0.46 for fat mass in the legs (kg) adjusted for BMI (76). Even though many women with lipedema also have obesity, the authors assert this cutoff value allows for a separation of lipedema of the legs from women without lipedema regardless of obesity.
Ultrasound of lipedema tissue compared to control tissue or tissue from women with lymphedema demonstrates thinner skin in agreement with previous data (77), and increased thickness and hypoechogenicity of the subcutaneous fat throughout the lower limb suggesting a diffuse increase in aqueous material (78). The hypoechogenicity was most significant in the distal extremity (medial calf) and may provide support to a clinical diagnosis when found. Another group found no difference between ultrasonographic features of women with and without lipedema including compressibility and echogenicity (79). The control women were reported to have obesity or lipohypertrophy, an enlargement of the legs that is phenotypically similar to lipedema but painless. The definition of lipohypertrophy is unclear in the literature where authors have stated that symptoms of lipohypertrophy resolve with elevation suggesting a fluid component associated with the fat tissue (80). In personal communication with the authors, they state the relief of symptoms is due to lowering of pressure on the venous system suggesting that venous disease is important in the diagnosis of lipohypertrophy. Other authors state that lipohypertrophy is a precursor to lipedema which may explain why the latter ultrasound data showed no differences. Clearly, better means of distinguishing lipedema from those with larger legs but no lipedema is needed.
Finally, widening of lymphatic vessels up to 2 mm has been found by magnetic resonance imaging (MRI) of the legs of women with lipedema; women with lipedema and lymphedema had lymphatic vessel enlargement >3 mm (81). If this dilation of lymphatic vessels is consistent with lymphostatic decompensation (failure of lymphatic vessel function) in lipedema as the authors suggest, then salt should be found in the skin of women with lipedema as lymphatic vessels regulate Na+, Cl– and water in the skin, where reduced lymphatic vessel numbers are paralleled by increased blood pressure (82). Indeed Crescenzi et al. found increased salt in the skin and loose connective tissue of women with lipedema compared to women without lipedema, even in earlier Stage 1 lipedema where women tend to not have obesity (49).
Conditions Associated with Lipedema
Obesity
Women with lipedema are often are often thought of as having common obesity whether or not they meet BMI criteria for this condition. The two striking differences between women with lipedema and women with obesity are that women with lipedema often have tenderness of the affected tissue and/or easy bruising of the skin overlying the lipedema fat, which is not found in women with common obesity (Table 1). However, some women with lipedema do not have pain in their tissues. It is unclear if women with lipedema with pain have the same disease as women without pain. Of note, women with lipedema may have no pain in their lipedema fat tissue when they are well-controlled under treatment regimens, however, they should still be considered to have lipedema. For example, women with lipedema who eat low inflammatory foods, avoiding processed starch and sugar, who exercise most days of the week and wear compression garments on their legs can have minimal to no pain. Therefore, a good history is important to identify a history of pain in the tissue that would be indicate the presence of lipedema. As described above, helpful measures to differentiate women with lipedema from women with common obesity include the disproportionate distribution of their adipose tissue between the trunk and legs, any family history of lipedema, as well as a historical inability to lose much fat from the lipedema-affected areas. On the other hand, when women with obesity and lipedema lose more substantial weight through medical or surgical interventions, they can lose some fat from the areas with lipedema, which can then leave them with rolls of excess skin along in the areas of remaining lipedema fat tissue (Figure 4).
Table 1.
Clinical Similarities and Differences Between Lipedema and Obesity
| Sign/Symptom | Lipedema | Obesity |
|---|---|---|
| Sex affected | Females | Females and Males |
| Onset | Puberty | Any age |
| Increased fat | Common | Common |
| Gynoid disproportion | Common | Possible |
| Influenced by lifestyle | No | Yes |
| Tenderness of the tissue | Common | Absent |
| Easy bruising | Common | Absent |
| Pitting edema | Uncommon | Uncommon |
| Stemmer sign | Negative | Negative |
| Able to lose fat from the legs/hips | Minimal | Common |
Obesity (especially abdominal/visceral obesity) and/or polycystic ovary syndrome can worsen lipedema severity. This is thought to be mediated by increases in adipokines, tumor necrosis factor alpha (TNFα) and leptin that often accompany these conditions, which are associated with venous disease (83). Venous dysfunction that can lead to leakage of fluid back into tissue due to reflux may also be an important contributor to worsening of both lipedema and lymphedema, when present (84,85).

Figure 4.
Fat due to obesity and fat due to lipedema can be intermixed on the legs. With weight loss, the obesity fat can be lost resulting in excess skin and lipedema fat tissue remaining on the legs.
Lymphedema
Women with lipedema are at risk for developing lymphedema, which may happens in lipedema Stage 3 > Stage 2 > Stage 1 (26). The presence of lymphatic disease or lymphedema increases the risk of cellulitis and wounds, which can be difficult to manage and disfiguring. Women with heavy limbs and swelling should be considered for manual lymphatic drainage and deeper tissue therapies such as instrument assisted soft tissue therapies (e.g., Astym therapy, Graston technique) or manual therapies (e.g., myofascial therapies or other deep tissue therapies (86)), followed by compression plus reduction of obese adipofascia to reduce the risk of developing lymphedema.
Dercum Disease (painful lipomas)
Lipedema can be present in the same individual who also has Dercum disease (see below), and in this instance, would be considered a mixed disorder. Authors have tried to differentiate women with lipedema from those with Dercum disease by examining populations and finding that people with Dercum disease tend to have other pain disorders including higher pain scores, fibromyalgia, abdominal pain, and migraines, and more often have lipomas, cognitive dysfunction and shortness of breath; whereas women with lipedema have more often fibrotic tissue, easy bruising, hypermobile joints, venous disease and edema of the feet (25).
Numerous other conditions apart from those described above have been associated with lipedema (Table 2). Of note, hypothyroidism is found in 27% of women with lipedema (25,26). In one case, a woman with lipedema was described as having lymphedema and multiple symmetric lipomatosis (91).
Table 2.
| Musculoskeletal | Soft Tissue | Vascular | Other |
|---|---|---|---|
| Gait disturbance | Obesity; fat deposits | Lymphedema/Idiopathic Edema | Pain |
| Change in posture (e.g., lordosis) | Loss of skin elasticity | Dilated Capillaries Microangiopathy | Psychological distress/anxiety |
| Genu valgum and arthritis of the knees | Thinning of the skin | Bruising | Shortness of breath |
| Ankle pronation | Lipomas | Varicose veins Venous insufficiency | Cellulitis |
| Hypermobile joints (Hypermobile Ehlers Danlos?) | Cellulite; fibrosis | Cherry angiomas | Slow metabolic rate |
Clinical Care of Women with Lipedema
Depending on whether the astute clinician makes the diagnosis of lipedema during the course of taking a history and physical, affected patients may more typically seek care for an associated co-morbidity. For example, women with lipedemia who have thyroid disease and/or obesity may regularly be referred by their primary care provider to an Endocrinologist. Endocrinologists should be clued in to a possible diagnosis of lipedema in women who present with difficulty losing weight from their hips, buttocks and legs, and who are convinced they have a thyroid issue, but thyroid labs are normal. In desperation, patients with lipedema may ask for a “complete set of thyroid labs” including thyroid stimulating hormone (TSH), free T4, free T3, reverse T3 and thyroid peroxidase (TPO) antibodies to ensure that there is no thyroid issue, which may cause tension during a clinical visit when a provider chooses not to order all these laboratories. Other times, women with joint hypermobility are often cared for by rheumatologists and orthopedic surgeons, and those with lipedema and venous disease are often followed by vascular surgeons, physical therapists and lymphedema specialists.
Diagnosis
Once the possibility of lipedema is considered, a good medical history will include an assessment of the food eaten, patterns of exercise, and a timeline of development of lipedema signs and symptoms with special attention to hormonal transitions in women including puberty, pregnancy, or menopause. Additionally, helpful findings on history include pain and easy bruising in affected areas and a family history of similar traits in other female members. The upper arms and legs should then be examined for physical manifestations of lipedema as described in more detail below. In the author’s experience, diagnosing lipedema in a woman who presents thinking they have another condition, such as thyroid disease but with normal thyroid function tests, and providing education and treatment recommendations can be transformative for the patient’s life and greatly enhance the patient-physician relationship.
The physical exam to diagnose lipedema can be performed quickly if a woman can be seen in her underwear after donning a gown. Visual inspection to establish disproportionality between the upper and lower body fat should be done initially and include a measure of the waist and hip ratio, which is also helpful in diagnosing central obesity. Following this, examination (both visually and by palpation of fat tissues) should be performed with special attention to characteristics described in Table 3.
Table 3.
Examination of Subcutaneous Fat for Lipedema, With or Without Obesity
| No Obesity | |
| Head | Normal |
| Neck | Normal |
| Arms | Normal (nodular fat tissue may be found around cubital nodes) |
| Wrist | Normal |
| Hands | Normal; Stemmer sign negative (no edema) |
| Abdomen | Normal (nodules may be found deep laterally or under the umbilicus) |
| Buttocks | Increased loose connective tissue; may be nodular and heavy |
| Hips | Increased loose connective tissue; may be nodular and heavy |
| Thighs | Increased loose connective tissue; may be nodular and heavy |
| Medial knee | Nodular or enlarged fat pad; usually tender |
| Under knee | Fat pad; may be nodular |
| Shin | May be covered in fat making the shin hard to palpate |
| Lateral malleolus | May have fat pad underneath |
| Ankle | Cuff may be very small but present in Type III lipedema |
| Feet | Normal; stemmer sign negative |
| Skin | Bruising; livedo reticularis; may see peau d’orange with long-standing disease |
| With Obesity | |
| Head | May have hair loss and increased fat |
| Neck | May have filling of the supraclavicular fossae |
| Arms | Nodular fat tissue on upper and/or lower arms and around cubital nodes; hanging fat on upper arm that may be heavy |
| Wrist | A cuff of fat may be present; bend the hand back to easily see the cuff |
| Hands | Fat may be found at the base of the thumb, between the MCP joints or over the hand |
| Abdomen | Increased deposit of fat above and/or below umbilicus |
| Buttocks | Increased loose connective tissue; may be nodular and usually heavy |
| Hips | Increased loose connective tissue; may be nodular and heavy |
| Thighs | Increased loose connective tissue; may be nodular and usually heavy |
| Medial knee | Nodular fat pad; usually tender |
| Under knee | Fat pad; may be nodular |
| Shin | Usually covered in fat making the shin hard to palpate |
| Lateral malleolus | May have fat pad underneath |
| Ankle | Cuff present in Type III lipedema |
| Feet | May have increased fat; Stemmer sign negative (no edema) when no lymphedema |
| Skin | Bruising; livedo reticularis; may see peau d’orange with long-standing disease |
| There is a wide variation in the phenotype of lipedema (see Figure 2 Types) therefore lack of one or more physical exam finding does not negative the presence of lipedema. | |
At present, lipedema does not have an International Classification of Disease (ICD)-10 code but an ICD-11 code of EF02.2 has been proposed. In the meantime, other ICD-10 codes useful when caring for patients with lipedema are listed in Table 4.
Table 4.
ICD-10 Codes for Clinical Visits for Patients with Lipedema
| Sign/Symptom | ICD-10 Code |
|---|---|
| Lymphedema/Swelling (may be non-pitting) | I89.0 |
| Edema unspecified | R60.9 |
| Lipomatosis not elsewhere classified | E88.2 |
| Chronic pain | G89.4 |
| Venous insufficiency | I87.2 |
| Varicose veins | I83.10 |
| Overweight | E66.3 |
| Other Obesity | E66.8 |
| Obesity (ICD-10 code varies by BMI) | Z68 |
Treatments for Lipedema
Food Plans
Many women with lipedema bring along family members that can attest to their healthy or minimal eating and beneficial exercise patterns as they tend not to be initially believed by healthcare providers. There is very little data on the use of diets to reduce lipedema fat. Although poorly studied, it is generally accepted that lipedema fat is resistant to weight loss mediated through lifestyle, which compounds patients’ frustrations when weight loss expectations are not met. In the absence of specific recommendations, dietary counseling can focus on establishing healthy eating patterns for overall health improvement and weight management.
Food plans are important in helping manage obesity that accompanies lipedema with a minimal goal of stabilizing weight and a maximal goal of losing obesity weight. The most successful food plans are those with low processed carbohydrates including added sugars that reduce insulin levels and inflammation and, therefore, reduce adipogenesis (95); fasting between meals (no snacking) has been suggested (96). One group used a 1200 calorie diet along with complete decongestive therapy to reduce volume in the legs of women with lipedema (97), but evidence for long-term weight loss maintenance by this approach is lacking.
Exercise
Exercise is important for women living with lipedema as the muscle action helps pump blood and lymph fluid through the limbs. However, women with lipedema have ~67% of the normative value for quadriceps muscle strength compared to women without this condition matched for age and BMI (98). One theory is that fibrosis from the fat tissue extends into and reduces muscle function. The Dutch guidelines for lipedema recommend graded exercise programs aimed at strength training and conditioning for women with unhealthy lifestyles or physical limitations, although they recognize that the body parts affected by lipedema tend to increase in tissue volume despite activity (80). These authors also state that exercise and heat can increase swelling and pain in the lipedematous areas. Anecdotally, women with lipedema appear to benefit greatly from water exercises, which may be in part due to the compressive effect of water on the body that helps mobilize fluid and soften fibrotic tissues, as well as from water jets that may also help reduce fluid in the adipofascia. Some women with lipedema have a concern about showing their bodies in public due to the commonality of public body shaming (99). Cropped pant, swim tights and other swimwear coverings have enabled more women with lipedema to feel comfortable during public swimming. Garments with compression are generally recommended for women with lipedema to wear during land-based exercises especially, when using Nordic poles that improve the adipofasica of the arms and legs.
Compression Garments
Compression garments are usually worn on the legs with a high waist (to treat fat on the abdomen) and on the arms as needed. Compression can be lower in millimeters of mercury (mm Hg) for lipedema than for lymphedema. For example, 15-25 mm Hg or Class I 20-30 mm Hg, compared to Class II 30-40 mm Hg or Class III 40-50 mm Hg. The type of knit for a lower pressure garment can be circular knit, which means it is seamless and is knitted on a round cylinder. Circular knit garments have more stretch and are best suited for women with lipedema that have less lymphedema or swelling. They can also stretch to fit any shape and size. Flat knit garments have less stretch and therefore provide better edema control. Flat knit is recommended especially for women with lipedema who have an ankle cuff or unusual shape requiring a custom fit and usually have a seam. A durable medical equipment (DME) order can be provided to patients to take to a medical supply store if they are able to get insurance coverage for compression garments. Therapists treating patients with lipedema can provide guidance on compression wear.
Venous Disease
Venous insufficiency has been documented in 25% of women with lipedema (92,100). When pitting edema is present, venous insufficiency should be investigated in women with lipedema by a venous duplex ultrasound of the legs. These studies are performed in a vascular lab and should specify to look at the greater and lesser veins of the legs to evaluate for venous insufficiency and not just thrombus. Care should be taken to treat venous disease conservatively first as there is no data showing correction of venous insufficiency by surgical means will improve lipedema. Anecdotally in reports from women with or without lipedema, lymphedema can occur after surgical treatment of venous insufficiency of the greater saphenous vein (101).
Bariatric Surgery
Women with lipedema without some upper body obesity may respond poorly to bariatric surgery with regard to weight loss (102) and often feel like failures or are mistakenly told (directly or indirectly) by their providers that it was their fault, with devastating psychological impact. Indeed, women that lose minimal weight from their lower abdomen, hips, and legs after bariatric surgery should be examined for the presence of lipedema. Even with less-than-expected weight loss, patients with lipedema should still be considered candidates for bariatric surgery as several procedures (e.g., laparoscopic gastric bypass and sleeve gastrectomy) have shown weight-independent benefits on glucometabolic outcomes, especially prediabetes and diabetes, and cardiovascular risk. When women do lose weight and it includes a portion of their lipedema-affected regions, it often results in accentuation of the “saddle bag” look (See Figure 4) and may worsen their body image anxieties. Optimally, women with lipedema should be identified prior to bariatric surgery, counseled on their condition and how it might influence their overall weight-loss response, and be offered complete decongestive therapy and compression garments to reduce the risk of developing lymphedema after bariatric surgery and to improve weight loss success. In addition, pre-surgery is a good time to initiate consultation with a plastic surgeon regarding options of removal of excess skin removal once weight stability is established post-operatively (usually between 1 and 3 years).
Liposuction
Women with lipedema typically have several medically necessary reasons for undergoing liposuction to remove lipedema fat, including:
- Loss of mobility
- Reduced quality of life
- Joint damage or altered gait
- Chronic pain
- Failure to improve signs and symptoms associated with lipedema despite conservative therapy
Complete decongestive therapy including manual lymphatic drainage, compression garments, a healthy eating plan, and as much activity as allowed or possible are important before liposuction to improve outcomes. Due to the increased vascularity of the lipedematous tissue and blood loss with liposuction, post-procedure anemia is not uncommon. Therefore, labs prior to surgery should include a complete blood count (CBC) with platelet level as well as coagulation labs to include activated prothrombin time (aPTT), prothrombin time (PT), thrombin time (TT), and fibrinogen. People with normal coagulation labs and easy bruising can have hereditary and acquired platelet defects, hereditary disorders of vascular and perivascular tissues including Ehlers Danlos Syndrome, and other disorders of blood clotting. Any woman with lipedema and a personal or family history of bleeding or clotting should work with a healthcare provider to determine if additional testing is needed before liposuction surgery (103).
Removal of lipedema fat by liposuction that spares lymphatic vessels (wet, not dry, technique) has been performed primarily in Europe, especially in Germany, since the 1990s (104-107). The fat is saturated with Klein solution which includes saline or lactated Ringers solution, an anesthetic such as lidocaine or prilocaine, epinephrine, sodium bicarbonate buffer(108), usually without steroid (109). This tumescent technique provides turgor to the tissue allowing blunt microcannula to slide through the fat tissue avoiding creation of shearing forces and tissue damage. When power assisted, tiny, rapid vibrations of the microcannula break up fat which is then suctioned out of the tissue. Water jet assisted liposuction (WAL) uses jets of saline and Klein solution to release fat for suction with minimal damage to cells and vessels(106) without the waiting period required to tumesce the tissue. Laser assisted tumescent liposuction is another technique which some reserve for fibrotic areas such as the posterior thighs.
Most affected women undergo liposuction in stages, involving removal of an area of lipedema fat from the lower body and arms followed by a period of recovery and healing before returning to remove an adjacent region. The average number of surgeries for a women with Stage II lipedema ranged between two and three (110), but some had more than five (37). Patients are either awake during the liposuction procedure with or without conscious sedation (104,111,112), or general anesthesia, the former allowing for rapid recovery (111). Some medications used in general anesthesia reduce the pumping activity of lymphatic vessels (113-116). Prior to undergoing liposuction by a qualified surgeon, therefore, a patient should have a thorough understanding of the surgeon’s technique, whether the surgeon uses general anesthesia along with the type of analgesia, the number of surgeries performed by the surgeon and outcomes and their complication rate. After liposuction, the surgically treated areas may be quite tender and uncomfortable for days to weeks.
Most studies on liposuction are from surgeons performing the procedure, are not randomized or controlled, and do not include external oversight of data collection. Nevertheless, current data are compelling for benefit. Twenty-five women with lipedema had significant improvements in pain, tension in the legs, excessive warmth, muscle cramps, leg heaviness, tired legs, swelling, itching, general involvement of the skin, difficulty walking, quality of life, and appearance of the legs six months post-liposuction surgery (104). A larger study of 85 women from the same clinic demonstrated significant improvements six months after surgery for all complaints with the greatest improvement in quality of life (110). In a longer study from a different clinic, 21 women over an average of 3.7 years after their first liposuction procedure and 2.9 years after the second liposuction showed improvement in the parameters of body disproportion, swelling, edema and quality of life, except for bruising which improved in all but two of the women (105). A retrospective study of women with Stage I or II lipedema from the same clinic, four, and eight years after liposuction, showed sustained improvements during follow-up for parameters including pain, sensitivity to pressure, edema, bruising, restriction of movement, cosmetic impairment, reduction of overall quality of life and overall impairment (117). The most interesting data was the reduced need for combined decongestive therapy four years after liposuction, which decreased further after eight years (37).
Any surgery, including liposuction, requires that efficacy of the procedure and the medical necessity be demonstrated to the insurance company. What are currently needed are well conducted randomized, controlled trials of sufficient numbers of patients with lipedema to determine which patients do and do not benefit from liposuction. In the meantime, documenting patient baseline characteristics and outcomes by surgeons in the United States will be important to understand the benefits of liposuction for lipedema in the US population compared to reports from other countries (e.g., Germany). It is notable that surgeons agree that quality of life is strongly and consistently improved by liposuction (104,110,117,118).
Complete Decongestive Therapy
Complete decongestive therapy (CDT) is commonly recommended for the treatment of lymphedema and includes skin care, education on home exercise programs, manual lymphatic drainage (MLD) therapy, wrapping as needed to reduce fluid build-up, and skin care recommendations performed by physical and occupational therapists and licensed massage therapists that have undergone additional training. Many women with lipedema benefit from CDT with reduced pain, limb volume and capillary fragility (119-121). Near-infrared fluorescence lymphatic imaging (NIRFLI) has added additional techniques to MLD including the “Fill and Flush” method (122). Complete decongestive therapy also improves lymph flow in brain lymphatic vessels (123). Deeper tissue therapies to reduce fibrosis in the lipedema tissues may also be beneficial for patients with lipedema.
Pneumatic Compression Devices
Studies have shown the benefit of advanced pneumatic compression devices (PCDs) in the treatment of lymphedema. There are also studies on the benefits of PCDs in the treatment of lipedema (119,124). Important for the distorted and dilated capillaries in lipedema (36,88), PCDs decrease capillary fragility (120), improving vessel quality. Along with manual therapy to improve flow of fluid through lipedema tissue, PCDs are also recommended in conjunction with liposuction surgery for lipedema (110). If a woman with lipedema responds well to manual therapy, or she tries a PCD and has a reduction in tissue volume, she should be offered PCD therapy to continue treatment at home when insurance will no longer cover CDT or when distance or commitments prevent regular professional visits. The PCD should ideally be an E0652 device with a segmented, multi-ported pump that allows for individual pressure calibration at each port. This allows the patient to alter pressure in areas of severe pain or for different shaped tissue. Pump garments should wrap around and treat the abdomen and pelvis when the legs are pumped, and the chest when the arms are pumped. If basic compression pumps are prescribed (E0650; E0651), compression garments to protect the abdomen, pelvis, chest and/or head should be worn during pumping. Without these compression garments, fluid is pushed up the leg into the abdominal and pelvic area where it accumulates due to lymphatic dysfunction. As this fluid sits in the tissue with all its nutrients and protein, evidence suggests it may stimulate further adipogenesis (125). With an E0652 pump, the abdomen is treated along with the leg and the chest is treated along with the arm preventing pooling of lymph fluid. PCDs can be easily ordered by writing a prescription for durable medical equipment with multiple suppliers.
Deep Tissue Therapy
Women with lipedema treated with deep tissue manual therapy have reduced pain, fat tissue on the legs, tissue volume, tissue fibrosis and leaky or fibrotic vessels (86,126). This deep tissue therapy is in the spectrum of meridian massage shown to reduce body weight (127) and is thought to improve lymphatic flow through lipedema fat tissue. Massage also reduced fat in preterm infants (128). Instrument-assisted soft tissue (IAST) therapy has cc in lipedema fat tissue with noted reduction in palpable fibrosis after treatment. Instrument-assisted soft tissue techniques include Astym therapy, which increased fibroblast activation and number, production of fibronectin, movement, and decreased pain in patients with fibrosis (129) and Graston technique which reduces pain and improves movement (130), and are performed by physical therapists who can be located on websites for these techniques. Traditional Chinese gua sha tools or bian stones have been used to improve pain and function (131) as has cupping (132). Pressure required to occlude lymphatic function in the upper limb was found to be 86 mm Hg, suggesting that deeper treatment into the tissue is safe, for example at pressures ranging from 15 to 25 mm Hg used to reduce scars (133), and will not damage lymphatic vessels (122).
Psychological Support
Women with lipedema have often spent years looking for answers and help for their condition. Healthcare providers often hold strong negative attitudes and stereotypes about people with obesity, which may reduce the quality of care they provide to women with lipedema (134). Poor quality of life associated with mobility and appearance-related stress associated with lipedema can result in depression (87). For many patients, they experience a huge sense of relief when they finally get a diagnosis of lipedema after trying a myriad of diets and exercise programs, even bariatric surgery to lose the lipedema fat. In addition to treatment recommendations in this chapter, there are a number of things a healthcare provider can do to help improve the lives of people living with lipedema: 1) Reduce focus on body weight in lipedema and provide education on improving metabolism, reducing inflammation and improving quality of the lipedema fat tissue (reducing fibrosis); 2) Use motivational interviewing focusing on strides made to improve markers of health including healthy eating, activity, metabolic lab markers, and social interactions; 3) Ensure that the clinic environment is welcoming with tables and chairs that allow women with larger lower bodies to be comfortable; 4) Ensure that patients with lipedema have identity safety in clinic situations and encourage healthy social interactions at home and in on-line social groups that also provide safe affiliations known to improve satisfaction of life for women with lipedema (135); and 5) Ensure that the continuum of care includes adequate referral resources for counselling, physical therapy and message, and when indicated pain management specialists. Including providers that understand lipedema and the physical and the psychological burden this diagnosis carries for patients is especially important (134).
Medications and Supplements
There are no medications and supplements specifically for lipedema. Instead, recommendations regarding use of medications and supplements for the treatment of lipedema should focus on reducing tissue inflammation, fibrosis, swelling, pain, and pharmacologic weight loss management for those who are overweight or have obesity. Supplements used for lipedema are, in part, based on literature for lymphedema and venous disease, both complications of lipedema. Some medications exacerbate symptoms in lipedema and should be avoided (Table 5).
Sympathomimetic Amines
Sympathomimetic amines (SA) such as phentermine and amphetamine are approved by the food and drug administration (FDA) for the treatment of obesity. Sympathomimetic amines bind to adrenergic receptors (AR) located on adipocytes to induce lipolysis, reducing the storage of fat. Adrenergic receptors are also located on blood vessels and lymphatic vessels. Activating AR on blood vessels induces vasoconstriction. Activating AR on lymphatic vessels improves the efficiency of lymphatic pumping by increasing the force of contraction (136); medications or supplements that improve lymphatic pumping are lymphagogues. Amphetamine and dextroamphetamine alone or in combination are also FDA-approved for the treatment of attention deficit disorder (ADD), attention deficit hyperactivity disorder (ADHD), and narcolepsy. The use of SA for treatment of lipedema may be beneficial in reducing fat and improving lymphatic pumping. A retrospective questionnaire study found that low dose sympathomimetic amines improved quality of life, reduced weight, clothing size, pain and leg heaviness in women with lipedema (137). Contraindications of sympathomimetic amines include advanced arteriosclerosis, symptomatic cardiovascular disease, moderate to severe hypertension, hyperthyroidism, known hypersensitivity or idiosyncrasy to the sympathomimetic amines, and glaucoma.
Diosmin
Diosmin is a bioflavonoid found in the rind of citrus fruit and is traditionally prescribed for the treatment of inflammation associated with chronic venous insufficiency. Diosmin was shown to reduce oxidative stress markers in people with chronic venous insufficiency (138). Diosmin also functions as a lymphagogue, and in combination with its anti-inflammatory activity, reduces edema (138). Women with lipedema who have a feeling of heaviness in their legs, obvious edema, chronic venous insufficiency or Stage II and III lipedema report feeling less pain and improved swelling on diosmin based on the author’s experience. Diosmin can be found over the counter or ordered by prescription as a medical food. Placing lemons, limes or other citrus in water to soak before drinking is a way to intake diosmin throughout the day.
Metformin
There are no current medications that can be used to reduce fibrosis already present in lipedema fat tissue, for which liposuction and deep tissue therapy are better modalities. Metformin and resveratrol have been shown to reduce the development of hypoxia-inducible factor (HIF)-1 inflammation and fibrosis in mice fed a high fat diet (139). Metformin also prevented fibrosis and restored glucose uptake in fat after insulin stimulation, although it did not prevent side effects of doxorubicin that included tissue loss and inflammatory response (140). Metformin should be considered early in women with obesity and lipedema Stages II and III where fibrosis in the fat tissue is prominent, as well as in women who have signs of metabolic syndrome (69).
Selenium
Selenium is a mineral found in the soil and in high concentration in Brazil nuts (Bertholletia excelsa). Selenium has been demonstrated to have anti-inflammatory effects on multiple levels of the inflammatory cascade (141-144). Edema was significantly decreased after selenium intake in two placebo-controlled trials for people with lymphedema (145,146) and improved complete decongestive therapy while reducing the incidence of erysipelas infections in patients with chronic lymphedema (145). Each Brazil nut contains approximately 200 mcg of selenium with a no observed adverse effects for dietary intake of selenium up to 800 mcg daily (147). Care must be taken to follow blood selenium levels as selenium deficiency and excess can both adversely affect glucose and lipid metabolism and potentiate the risk of development of type 2 diabetes in several animal studies, with less clear associations in human studies (148). One case report of a woman with lipedema showed reduced leg volume with a combination of selenium and Butcher’s broom (149).
Table 5:
Medications and Supplements to Avoid When Treating People with Lipedema
| Medication | Used for | Reason to avoid |
|---|---|---|
| Thiazolidinediones | Diabetes | Increases subcutaneous fat tissue; fluid retention |
| Calcium channel blockers | Hypertension | Fluid retention |
| Oral Corticosteroids* | Reduce inflammation | Weaken tissue; fluid retention; rebound inflammation |
| NSAIDs | Pain | Fluid retention |
| Sex hormones | Hormone replacement | Fluid retention; implicated to effect development of lipedema |
| Beta blockers | Cardiac health | Fluid retention |
| Clonidine | Hypertension | Fluid retention |
| Gabapentin | Pain | Fluid retention |
| Furosemide** | Edema | Concentrates protein in the interstitial organ eventually halting fluid flux |
- *
Nasal or inhaled corticosteroids have less effect; oral corticosteroids should be used when medically necessary
- **
Aldactone and hydrochlorothiazide have less adverse effects in women with lipedema
NSAIDs: Non-steroidal anti-inflammatory drugs
Concluding Remarks on Lipedema
Lipedema is a common disease mostly in women resulting in an enlargement of the adipofascia on the limbs due to excess fibrosis in the tissue that typically defies expectations for loss by lifestyle, weight-loss medications, and bariatric/metabolic surgical interventions. The presence of fibrosis, especially in the interstitial spaces where it may serve to restrict blood and lymph out flow, is thought to contribute to the resistance of this tissue to weight loss. Women with lipedema should be recognized prior to weight loss efforts so that expectations can be discussed, and manual therapies and other treatments can be considered to improve outcomes. Medications and supplements can be tried, but liposuction should be considered for women with lipedema who fail conservative measures and following weight loss with medications and/or bariatric surgery. There is a wide variety of presentations of lipedema in women due to co-morbidities and other genetic and environmental influences. Therefore, every affected woman should be considered on a spectrum and treatments personalized.
FAMILIAL MULTIPLE LIPOMATOSIS
Familial multiple lipomatosis (FML) is a rare adipose disorder (RAD) of multiple lipomas in subcutaneous fat (OMIM 151900). Some members in an FML family may have only a few lipomas whereas others may have hundreds to thousands; it is not understood why there is unequal penetrance in families. Lipomas usually are not painful or tender to the touch except while growing; they may also cause a slight feeling of itching or burning when forming. Some lipomas can be tender if they develop in areas of pressure such as on the back of the legs, the lower back (pressure from a chair), or the lateral wrist due to repetitive stress such as comes from using a computer mouse (150,151). Another example of trauma-induced lipomatous growth includes movement of the xiphoid process (152).
According to older FML literature (153), "pain may suddenly develop in one of the lipomas (called lipoma dolorosa), and will gradually extend to involve more and more of the discrete lipomas.” The authors state that lipoma dolorosa syndrome in families with FML is not the same as Dercum disease (see below) (154). This is confusing as individuals with painful lipomas in an FML family have been described as having Dercum disease. While painful lipomas in a person with FML may also be on the spectrum of Dercum disease, a more precise name is FML with painful lipomas, especially when a family history of FML is known.
It is interesting that by observation in some families with FML, the men will develop lipomas and the women often develop obesity in line with lipedema. This suggests an overlap between the development of one fat disorder (FML) and another (lipedema) and should prompt more detailed questions regarding other potentially affected family members.
Prevalence of FML
Familial multiple lipomatosis is considered to be a rare disease with an estimated prevalence of 1/50,000 (155).
Genetics of FML
Familial multiple lipomatosis is usually inherited in an autosomal dominant manner with males and females equally affected. The gene High Mobility Group AT-Hook 2 (HMGA2; 12q15) has been implicated in FML but is not thought to be causative. A mutation in partner and localizer of breast cancer (BRCA2, DNA-repair associated gene), called PALB2, was described in a family with FML (156). PALB2 is an intranuclear protein that anchors BRCA2 to nuclear structures. PALB2 mutations are associated with a 2-fold increased risk of breast cancer, a Fanconi anemia subset, pancreatic cancer and ovarian cancer (156).
Conditions Associated with FML
In case reports, FML has been associated other rare or unusual disorders (Table 6). Because multiple lipomas are often linked with mutations in tumor suppressor genes, FML can be considered clinically to be a marker for the presence of an underlying tumor suppression gene mutation and affected patients and their families should be appropriately screened.
For example, in MEN-1, lipomas have been reported in association with a recessive mutation in a tumor suppressor gene (157). In a family with retinoblastoma and multiple lipomas, the lipomas were present in people with a gene mutation in the RB1 gene who did not develop retinoblastomas (158). Multiple lipomas in Cowden's disease can be due to a germline inactivation of PTEN/MMAC1 that renders a person susceptible to thyroid and breast malignancies (159). Other genes including other tumor suppressor genes have been implicated in the growth of lipomas (160). For example, a mutation was found in the tumor suppression gene PALB2 in a family with multiple lipomas suggestive of a diagnosis of FML (156). And finally, lipomatosis like that of FML has also been reported in two cases after chemotherapy (161,162), a treatment known to be associated with an increased risk of cancer development. Because of these associations, people with multiple lipomas should be considered at increased risk for cancers and a referral to a geneticist considered.
Table 6.
Disorders Found in Association with Multiple Lipomas
| Atypical mole syndrome (163) |
| Gastroduodenal lipomatosis (no gastroduodenal lipomatosis in proband’s mother) (164) |
| Celiac disease (165) |
| Cowden’s disease (159) |
| Gastrointestinal stromal tumor (166) |
| Interhemispheric brain lipoma with corpus callosum hypoplasia and the malformation of cortical development in a young woman with refractory epilepsy (167) |
| Neurofibromatosis (NF1) (168) |
| Multiple endocrine neoplasia (MEN)-1 (169) |
| Retinoblastoma (Rb1) (158) |
| Legius Syndrome (SPRED 1); autosomal dominant; multiple café-au-lait macules and skin fold freckling, ± macrocephaly, a Noonan-like appearance, learning difficulties and/or attention deficit in children and lipomas in adults (170) |
Pathophysiology of FML
The pathophysiology of lipoma growth in FML is not known. Single lipomas of subcutaneous fat tissue are the most common benign tumor growths in humans and may be induced by genetic changes, trauma, inflammation, or other causes. As detailed above, multiple lipomas tend to be linked with tumor suppression genes. People with FML are known to be insulin sensitive, therefore an insulin-resistant metabolic cause of FML is unlikely (171). Additionally, the presence of the lipomas themselves do not confer insulin resistance.
Imaging of Lipomas in FML
Lipomas in FML are identified by palpation as connected to skin, surrounded by fat or connected to other structures such as muscle or solid fascial structures. Localized pain can assist in finding smaller lipomas. Silky or tight clothing can also assist in palpation. Sonographic evaluation is the best most inexpensive means to identify lipomas other than palpation, but the average sensitivity for three Radiologists when retrospectively reviewing sonographic exams of lipomas was only 48%, and average accuracy was 59% (172). Magnetic resonance imaging without contrast can be used to find lipomas (173), but small lipomas, lipomas without a capsule, and lipomas with minimal fibrosis or surrounding edema remain difficult to identify. Radiologists were able to render the correct diagnosis for lipoma versus liposarcoma in 69% of cases (174). Computed tomography (CT) scans have been used to differentiate lipomas from liposarcomas (175) but should be used after sonography and MRI to avoid excess radiation exposure.
Evaluation of the Patient With FML
The initial workup for people with FML includes a family history of lipomas and cancer, and any associated conditions such as nevi or neuropathy. The exam incudes assessment for multiple lipomas usually located on the trunk, lower back, arms, and thighs; rarely on the upper back or calves. Skin should be examined for nevi and cherry angiomas, the latter seen commonly with multiple lipomatosis (176). Due to the associated cancer risk, the exam includes examination of the thyroid and breasts for nodules. Reflexes should be checked along with monofilament and/or vibration assessments for peripheral neuropathy. Cancer screening as appropriate for sex and age should be advised, and appropriate labs ordered (Table 7). Although there is no definitive association of FML with dyslipidemia, statin therapy may be helpful in lowering lipoma size (177) and so a lipid panel is also appropriate.
Table 7.
The FML Workup
| Family history | Lipomas; cancer; nevi; celiac; neuropathy |
| Medical history | Lipomas; cancer; nevi; celiac; neuropathy |
| Physical Exam | |
| Lipomas | Trunk, arms, low back, flanks, abdomen, thigh. Attached to skin, muscle, other. |
| Skin | Nevi; cherry angiomas |
| Thyroid | Nodules |
| Nervous system | Reflexes; skin sensory exam (monofilament) |
| Laboratory Studies | |
| Thyroid | TSH |
| Blood fats | Lipid panel; other per family history |
| Fibrin clot (found in angiolipoma) | D-dimer |
| Food/gluten intolerance | Celiac panel |
Treatment of FML
The current management of FML includes screening for associated conditions such as cancer (Table 7) and consideration of a referral to genetics for tumor suppressor gene workups as needed. A healthy diet and an exercise plan to avoid or reduce obesity is important as obesity in families with FML can be associated with pain (154) and, anecdotally, triathletes notice a reduction in lipoma size during high intensity training. A statin has been shown to reduce a lipoma in a case report (177). Painful lipomas or those that interfere with activities of daily living can be excised as needed but these procedures can cause numerous scars (Figure 5). Massive amounts of lipomas can occur on the arms, hips/flanks, buttocks and thighs. Therefore, this condition can be psychologically devastating and people with severe FML do not consider it benign.

Figure 5.
Multiple scars after excision of lipomas in FML.
Liposuction is an option to excision of lipomas in people with FML as it provides good results in terms of skin appearance, and there is reported lack of recurrence or growth or development of other lipomas in the same area for at least 12 months (178). Injections of collagenase have been shown to shrink or destroy lipomas with minimal pain and good cosmetic result in a published abstract (179). Similar data were found for the detergent, deoxycholic acid (180), but anecdotally care should be taken not to inject too much detergent that can remain in the tissue requiring excision to remove. Additional treatments such as cryotherapy have been suggested and reviewed (181). More data is needed for the efficacy of injections and other therapies for the lipomas in FML as they are preferable to more invasive and scarring surgical techniques.
Concluding Remarks on FML
Familial multiple lipomatosis is a rare disease of multiple lipomas often associated with mutations in a tumor suppressor gene. Therefore, people identified with FML should be assessed for cancer. Liposuction should be considered to remove symptomatic lipomas and is preferable to surgical excision as multiple excisions leave many scars.
ANGIOLIPOMATOSIS
Angiolipomatosis also known as angiolipoma microthromboticum (OMIM 206550) is a rare disease of multiple angiolipomas and connective tissue that occurs commonly in men and usually begins after puberty; one case of a child with an angiolipoma in a family in which the father also had angiolipomatosis has been reported (182). Angiolipomas have been described as vascular malformations or vascular lipomas where blood vessels occupy between 10-90% of the angiolipoma. In families with familial angioliopomatosis, lipomas and angiolipomas can exist in the same person. Subcutaneous angiolipomas usually occur on the trunk and limbs, rarely on the head, hands, or feet (183). The angiolipomas can be the size of a rice grain, pea, a marble or much larger and are tender to the touch and can be associated with intense pain. Angiolipomas may or may not be visible and may be palpable or non-palpable depending on their location and size. Numerous case reports describe epidural or extradural spinal angiolipomas, and rare cases report colonic (184), bronchial (185), joint (186), and testicular angiolipomas (187). Angiolipomas are known to be painful, although not always, and should be distinguished from other painful neoplasms (188). One case of angiolipomatosis was reported to occur after treatment with corticosteroids (189).
The loose connective tissue of angiolipomas contains adipose cells, fibrotic tissue, vessels with fibrin clots, and mast cells as salient features (Figure 6). Due to the large number of vessels, angiolipomas are bluish in color through the skin. Interestingly, the vessels in angiolipomas can grow from the dermis into the territory of the epidermis making the vessels palpable as small raised areas on the skin (Figure 7). A plethora of capillary “cherry” angiomas where a capillary grows and dilates through the epidermis may be found on the skin in areas of angiolipomas (Figure 8).
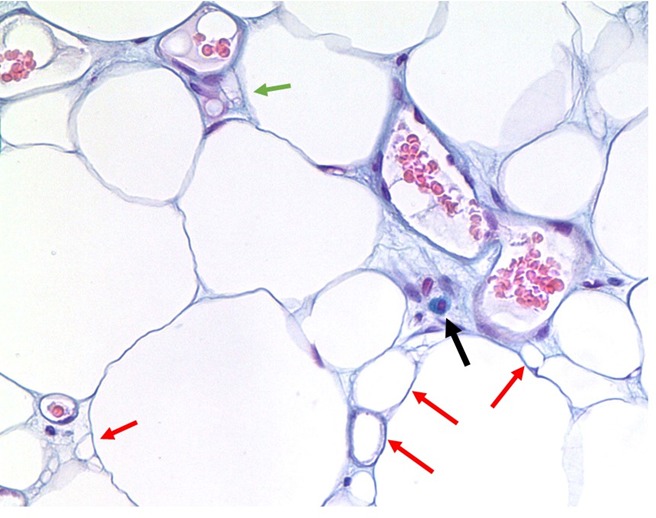
Figure 6.
Angiolipoma with mast cell with enlarged multiple vessel lumens and degraded tissue. The black arrow points to a classic fried egg appearance of a mast cell stained with Alcian Blue in angiolipoma tissue. Red arrows point to small fat cell remnants likely non-functional as evidenced by the absence of nuclei. Blood vessels are numerous and large for location. The green arrow demonstrates the remnant of a capillary. Connective tissue is evident especially in the area surrounding the mast cell as bluish fibers. Magnification 100X.

Figure 7.
Multiple cherry angiomas present on the legs and arms of a woman with angiolipomatosis.

Figure 8.
Histological features of angiolipomas. A. Small area of hypervascularity in an angiolipoma (40X). B. Blood vessels in an angiolipoma grow up and through the epidermis and are palpable on the skin (40X). C. Empty and presumed dead and non-functional vessel on the left containing an eosinophil next to two functional blood vessel lumens containing red blood cells (100X). Microthrombi can be seen as pale areas especially between the right side of the dead vessel and the lumen of the active vessel. Dead vessels may result in hypoxia and ischemia causing pain. D. Non-functioning blood vessel to the right and smaller fat cells surrounded by an enlarged interstitial organ (40X).
Prevalence of Angiolipomatosis
The prevalence of angiolipomatosis is unknown but it is considered to be a rare disease (190,191).
Genetics of Angiolipomatosis
Angiolipomatosis most often occurs sporadically, but a family history can be identified in a minority of cases as autosomal dominant (192) or autosomal recessive (193,194). There are no known genes identified to date for angiolipomatosis.
Pathophysiology of Angiolipomatosis
Angiolipomas likely arise from fascia and therefore may also be painful because fascia is highly innervated, and when inflamed, is a likely source of pain (195). Inflamed fascia has robust angiogenesis (196) and may be important in the initial development of angiolipomas as resident mesenchymal cells in fascia can develop into adipocytes (197). It is thought that microthrombi in angiolipomas leads to necrosis of blood vessels, adipocytes and other components of adipofascia. Other hypotheses regarding pain include nerve damage from limited blood flow and tethering by fibrotic tissue.
Subcutaneous angiolipomas are assumed to be congenital in origin where pubertal hormones may induce differentiation of adult adipose-derived stromal adipogenic precursors that reside in adipofascia; these precursors develop into adipocytes in intimate association with blood vessels (197). Vascular proliferation is thought to occur after repeated trauma to the fascia resulting in the development of an angiolipoma. However, there is a question of whether angiolipomas can become autonomous as a cancer. Two of three cases of angiolipomas in one publication suggest a neoplastic nature for these tumors due to deletion of parts of chromosome 13, a region containing the retinoblastoma gene, a tumor suppressor gene (198). The neoplastic nature of angiolipomas should be considered in individuals with significant numbers of angiolipomas and anti-neoplastic treatments considered when other conservative therapies fail.
Imaging of Angiolipomatosis
Identification of angiolipomas in tissue by Ga-PSMA PET/CT (199), magnetic resonance imaging (200), and ultrasound (201) allows surgeons to identify superficial and deeper angiolipomas targeted for removal.
Treatment of Angiolipomatosis
Surgical
The only definitive treatment of angiolipomas to date is individual resection by excision or liposuction (202). Angiolipomas are typically removed if they are painful or restrict movement. A surgical emergency may occur to prevent hemorrhage of angiolipomas which can compress the spinal cord (203,204). Karyotypes of DNA from the angiolipomas should be assessed to determine the neoplastic nature of the angiolipomas so as to prepare the patient for the potential of multiple resections throughout life (198).
A concern with resection of lipomas is that inflammation is often a sequela of the removal process. As fascia plays an important role in the pathophysiology of angiolipomas, generation of inflammation in the fascia by surgical techniques has been anecdotally noted to incite a pain crisis. Removal of angiolipomas must therefore be considered carefully and manual or IAST therapies for the fascia should be considered after any surgery to speed recovery and reduce pain.
Pain Management
The necrosis of tissue in angiolipomas and inflammation of fascia with all of its nerve endings can cause severe pain in individuals with angiolipomatosis. In a case report from Germany, the systemic administration of acetylsalicylic acid, diclofenac, ketotifen, ranitidine, tramadol, or tilidine combined with naloxone did not provide adequate pain relief. In contrast, the antidepressant doxepin, which also has antihistaminergic effects to control the release of mast cell mediators, demonstrated good therapeutic efficiency for the pain from angiolipomas (205). Depending on the mast cell burden in angiolipomas and their systemic effects including flushing, itching, nausea, diarrhea, angioedema, pain and a cadre of other signs and symptoms (206,207), individuals with angiolipomatosis may be considered to have mast cell disease or mast cell activation disease. Treatments to reduce the burden of mast cells in angiolipomas such as histamine 1 and/or histamine 2 receptor blockers, montelukast, non-steroidal anti-inflammatory drugs, antihistaminergic bioflavonoids such as quercetin or pycnogenol, amphetamines, and possibly stronger immunosuppressants that have been used for mastocytosis such as sunitinib (208) or mast cell activation syndrome such as tofacitinib (209) or imatinib (210) may provide benefit for pain and growth of angiolipomas. Non-neoplastic therapy for mast cell activation disease should be considered prior to the use of antineoplastic agents, which have been described extensively (211). Patients with angiolipomatosis can have a poor quality of life due to extreme pain and fatigue and consider suicide. In these individuals, use of anti-neoplastic agents should be considered early.
Many individuals with angiolipomatosis require opioid pain management and should be under the care of pain management specialists. Unfortunately, opioids can activate mast cells requiring concurrent treatment of mast cell signs and symptoms (212). Opioids should not be withheld during a pain crisis, and in fact may need to be escalated before weaning back down after the pain crisis has resolved.
Concluding Remarks on Angiolipomatosis
People with angiolipomas have severe pain that can be out of proportion to the outward appearance of the individual. Treatment with mast cell stabilizers, pain medications, and surgical treatments of angiolipomas are all important in management. More research is needed for this rare disease to enable individuals with angiolipomas to live a full and active life.
DERCUM DISEASE
Dercum disease (DD; OMIM 103200) is a term used to describe extremely painful adipofascial tissue that is resistant to loss by diet and exercise and poorly responsive to analgesics. Other names include adiposis dolorosa (a term that is also used to describe women with lipedema) and Morbus Dercum. While Dercum disease is defined as painful fatty masses accompanied by other signs and symptoms of a chronic healing cycle disorder (25) (213), there remains a lot of confusion in the literature as to what exactly Dercum disease is. One review article stated that people with Dercum disease have obesity and chronic pain (214), which can easily be confused with people who have obesity and chronic pain for a variety of reasons including fibromyalgia. The old classification of Dercum disease and a new classification remain inadequate to differentiate the overlapping disorders that are bundled together as Dercum disease (65,215,216) because they describe only the phenotype and not the history (Table 8).
Table 8.
Comparison of Outdated Classifications of Dercum Disease.
| Older Classification | Previous Recent Classification |
|---|---|
| Type I: Diffuse Type. Widespread occurrence of painful lipomas in a diffuse manner | Diffuse Type. Diffusely painful adipose tissue that may present as painful folds of fats containing fat nodules that feel like pearls located around lymph node beds. Mostly resembles lipedema but extends or start in the trunk which differentiates it from lipedema |
| Type II: Generalized Nodular | Nodular type. Intense pain in and around grape-like clustered lipomas of variable size most commonly on the arms, legs, lower back or thorax; can include angiolipomas. Most resembles familial multiple lipomatosis |
| Type III. Localized Nodular | Nodular type. Intense pain in and around grape-like clustered lipomas of variable size in defined areas; can include angiolipomas |
| Type IV: Juxta-articular | NA |
| NA | Mixed Type: Combination of diffuse and nodular |
A better classification of painful adipofascia considers the history of the disease (Table 9). For example, women with lipedema who become obese and/or develop lymphedema can metabolically become toxic or ill leading to the growth of painful masses in fat tissue. The etiology of these masses is likely due to the presence of inflammation known to slow lymphatic pumping leaving more pre-lymph fluid in the ECM, inducing adipogenesis, as lymph (even pre-lymph) makes fat grow. Women with lipedema, obesity, and painful fatty masses have dominated some studies on Dercum disease leading the authors to describe women with Dercum disease as having obesity and chronic pain (214). The masses that develop in women with lipedema and metabolic syndrome are similar to those that develop on the abdomens of people who have obesity and do not have lipedema. These tender masses resolve with weight loss and have been called Ander’s disease or adiposis tuberosa simplex (217). A good history taken from a woman with lipedema and the label Dercum disease, may reveal the development of lipedema earlier in life and additional weight gain later in life with development of tender masses, allowing treatment to be focused on lipedema and obesity rather than on Dercum disease.
Table 9.
Conditions with Painful Adipofascia which Have Been Labeled as Dercum Disease
| Types | Comments |
|---|---|
| Obesity-associated | Non-painful lipomas resolve with weight loss (Ander’s disease) |
| Lipedema with obesity and/or lymphedema | Painful lipomas resolve with weight loss; lipedema fat tissue remains |
| Familial multiple lipomatosis (FML) with obesity | Lipomas may get smaller and pain reduce with weight loss |
| Angiolipomas with or without obesity | Weight loss does not affect angiolipomas but is important to reduce inflammation |
| Localized due to trauma(218) | Multiple lipomas in an area of trauma and not just a single lipoma; likely due to injury of the fascia as with angiolipomas |
| Toxic/infectious; present around lymph node beds or diffuse with or without obesity | Likely due to a healing cycle disorder, infection, methylation deficiency, high oxalate or other toxin overload. |
Signs and symptoms of Dercum disease include chronic pain, fatigue, brain fog, insomnia, cardiac arrhythmia most often tachycardia (palpitations), gastrointestinal distress often similar to irritable bowel syndrome, muscle weakness, tremor or jerking of muscles (myoclonus), joint pains, insulin resistance and diabetes, hypothyroidism, and other autoimmune disorders (219). The signs and symptoms of Dercum disease have been suggested to be in the spectrum of fibromyalgia (220).
Dr. Dercum’s first patient was a woman with obesity with fat similar to a woman with Stage 3 lipedema (221). Dr. Dercum and his medical resident described rapid changes in fat tissue shape and size in real time suggestive of edema or fluid shifts. Therefore, involvement of the lymphatic system is likely in Dercum disease. Irregular and thickened lymphatic vessels have been described in Dercum disease suggesting that an altered lymphatic system can contribute to changes in the adipofascial tissue that found by palpation (222). Once people with Dercum disease are more accurately described by phenotype, there will be a better chance of finding a gene or biomarkers.
Prevalence of Dercum Disease
Many women with lipedema have been miscategorized as having Dercum disease when actually they have lipedema and metabolic syndrome, making the prevalence estimate of 1/1000 for Dercum disease in Sweden too high (223). There are no other prevalence studies of Dercum disease although the angiolipomatosis type is considered rare and the obesity- or lipedema-associated types are likely common, but these individuals are better described with what they have, angiolipomas, obesity, or lipedema respectively, with metabolic disease rather than lumping them all together as Dercum disease simply due to the presence of pain in the tissue.
Genetics of Dercum Disease
There is(are) currently no known gene(s) for Dercum disease. Continuing to include people with angiolipomas, FML, and lipedema under the same moniker of Dercum disease will make it very difficult to discover genes important for these diseases when examining populations. The study of genes for specific families may be more helpful to find gene mutations that can then be assessed in individuals with painful adipofascia.
One family with familial multiple lipomatosis was found to have members that developed pain in the lipomas consistent with Dercum disease (adiposis dolorosa). While many of the family members with FML and pain also had obesity, not all were. Therefore the authors concluded that “adiposis dolorosa may in fact be an expression of familial multiple lipomas” (154). It remains unclear, however, why some individuals would develop pain and some not in a family with FML. Fascia can become inflamed for a variety of reasons including surgery, trauma, infection, toxin or drug exposure, and development of obesity. Lipomas in people with FML are often connected by a tail of connective tissue to solid fascial structures in the body, and fascia is a source of preadipocytes (Figure 9). It may be that lipomas in FML are a marker of fascial disease and that pain in and around the lipomas depends on the amount and extent of inflammation present. Other genes may modify susceptibility to prolonged inflammation including those yet to be identified in fibromyalgia (224).

Figure 9.
Lipomas with fascial component. A. Lipoma with obvious tail of connective tissue. Removal of the fascia is important along with the lipoma to reduce additional growth in the area of removal. B. Long piece of connective tissue weaving amongst multiple lipomas during resection.
Pathophysiology of Dercum Disease
The pathophysiology of Dercum disease needs to be determined by type, something that very few papers have done so accurately. In mostly women with lipedema type Dercum disease, substance P was lower in the spinal fluid compared to controls (225), confirming a strong pain component is present when women with lipedema develop obesity and metabolic syndrome. In another study, interleukin-6 levels were elevated in the fat from women with Dercum disease compared to women without lipedema supporting Dercum disease as an inflammatory disorder (226). Weight stabilization and when possible, weight loss in patients with obesity should be a focus for women who have developed metabolic disease, in addition to caring for their lipedema.
The juxta-articular type of Dercum disease where nodules in the adipofascial tissue are present around joints had been associated with rheumatoid arthritis (227). Lymph nodes are present around many joints including the elbow (cubit nodes), knees (popliteal nodes), and hips (femoral nodes), and in these locations adipofacial nodules have been found. Cases of juxta-articular Dercum disease suggest that inflammation in the adipofascia around joints may reduce lymphatic pumping in these areas resulting in a backup of fluid in the interstitial body leading to densification of fascia and eventually fibrosis around lobules of fat making them palpable as nodules. These nodules are tender due to inflammation of the fascia and nerves. As an example, a woman with rheumatoid arthritis was treated with tocilizumab, a humanized monoclonal antibody of class IgG1, targeting interleukin-6 receptors, and developed painful fatty masses of her knees documented by MRI (228). A similar pathophysiology would be likely for the trauma-induced Dercum disease.
Familial multiple lipomatosis and angiolipomas have been previously discussed including why pain develops in angiolipomas. It is unclear why a person with FML would suddenly develop pain in and around lipomas qualifying for a diagnosis of Dercum disease (FML type with pain). The presence of inflammation occurring in the body of a person with FML such as from obesity, trauma, hypermobile joint spectrum disorders, arthritis and any other inflammatory condition that includes the fascia in the inflammatory process likely accounts for the development of pain in FML. Resolving the inflammation in the fascia may reduce the pain and return the diagnosis back to FML alone.
One theory on the origin of Dercum Disease is based on the work of Robert Naviaux in which a failure of healing of inflammation occurs (213). According to Naviaux, a normal healing cycle includes normal wakefulness, restorative sleep, fitness and healthy aging. The cell “danger response” is an evolutionarily conserved cellular metabolic response activated when a cell encounters a threat that could injure or kill it, examples of which can be microbial, chemical, physical, or psychological in nature. Chronic disease occurs when cells fail to heal or contain inflammation, and a toxic repeating loop of incomplete recovery and re-injury occurs. Chronic pain disorders are included by Naviaux as a healing disorder and the author feels many people with Dercum disease fall into this category.
Imaging of Dercum Disease
The most inexpensive means to document lipomas in the adipofascia of people with Dercum disease is by ultrasound. Ultrasound findings include a hyperechogeneity (higher density) to the lipoma suggesting fibrotic tissue and no increased Doppler signal (minimal blood flow) (229).
Magnetic resonance imaging of the tissue of people with Dercum disease has found lymphedema in a woman and multiple lipomas in a man (230). Nodular type lipomas have also been visualized by MRI in the tissue of people with Dercum disease (229). The lipomas were multiple, oblong, fatty lesions in the superficial subcutaneous adipose tissue, mostly < 2 cm in long axis diameter. A nodular ("blush-like") fluid signal was also found without the presence of contrast. According to Richard Semelka, MD, gadolinium contrast should not be used in people with Dercum disease unless absolutely necessary to avoid any risk for development of gadolinium deposition disease (231,232). MRI images demonstrate variability in the tissue of people with Dercum disease, from lymphedema to distinct lipomas, and exemplify the different phenotypes under the moniker of Dercum disease. To date there are no confirmed connections between multiple lipomas as in FML or trauma-induced Dercum disease and development of lymphedema.
Conditions Associated with Dercum Disease
Dercum disease has been associated with many conditions such as disrupted sleep cycle, headaches, cognitive difficulties, tachycardia, shortness of breath, and gastrointestinal symptoms (219). Many of these symptoms are consistent with mast cell activation disease (MCAD). Therefore, MCAD is considered an associated condition in Dercum disease. Diabetes is common in Dercum disease (25,219) and cardiovascular disease should be evaluated for and treated in any person with Dercum disease especially if blood markers of inflammation are high, such as C-reactive protein. A woman with Dercum disease had a dysfunctional arteriolar venous reflex in her arm suggesting a blood vascular or nerve problem in Dercum disease (233). Another case of a woman with the FML type of painful lipomas was described who had dizziness followed by left sided sensory-motor deficit suggestive of a vascular origin (234). Anecdotally, some of the author’s patients with Dercum disease also have postural orthostatic tachycardia syndrome (POTS). Fibromyalgia is often an accompanying diagnosis in people with Dercum disease as are other pain syndromes such as migraines (25).
Many people with Dercum disease become concerned that the painful lipomas can spread throughout the body as with cancer. Once case of a lipoma on the uterus of a woman with Dercum disease is known to the author, and two women with Dercum disease had invasive calcaneal lipomas that were resected. Other lipomas in people with Dercum disease have been identified in the gastrointestinal system but these need to be verified. Lipomatous hypertrophy of the interatrial septum was found in one person with Dercum disease (235), but this type of fat can also be associated with obesity (236). Altered lymphatics were found in a few cases of Dercum disease (222). One family had Dercum disease with dysarthria, visual pursuit defect and progressive dystonia (237).
General swelling, a sensation of a “heaviness” in tissue, increased pain in one limb, or aching limbs all suggest that a lymphatic dysfunction may be present, which can be evaluated using lymphangioscintigraphy, which is performed in most nuclear medicine departments, or near infrared lymphatic imaging using indocyanine green, which is not yet to the point of being readily clinically available. Finding altered lymphatic function can change clinical management by steering practitioners towards prescribing manual lymphatic drainage therapy and compression garments to contain and support lymphatic flow.
Treatment of Dercum Disease
To maintain a healthy weight or lose excess adipofascial tissue, people with Dercum disease should be encouraged to eat a healthy diet such as Mediterranean, DASH, low processed sugar, plant-based low inflammatory foods, or foods that are low in histamine if mast cell activation disease is present or suspected; they should also undertake a graded exercise program.
Pain management of Dercum disease
Signs and symptoms common in people with Dercum disease, including pain. should be treated symptomatically (Table 10). Opioids are often used for pain treatment for Dercum disease, but doses can escalate over time and care should be taken to try and find additional alternative treatments.
Table 10.
Medications Used to Treat Pain and Other Symptoms in People with Dercum Disease
| Medication | Comments |
|---|---|
| Deoxycholic acid (238) | Injection of deoxycholic acid reduced pain and size of lipomas in a man with FML type of Dercum disease |
| Doxepin (205) | Has antihistaminergic activity therefore useful for pain, depression and mast cell activation disease |
| Intravenous lidocaine (239) | Ketamine is often used in addition to or in place of lidocaine if not effective |
| Topical lidocaine (240) | Often combined with other medications in topical form such as EMLA (241) |
| Metformin (242) | Useful for metabolic disease and when inflammatory markers are high |
| Mexiletine and amitriptyline (243) | Mexilitine has been described as oral lidocaine and offers an alternative to opioids |
| Low dose naltrexone (244) | Effective for fibromyalgia pain, a condition often present in Dercum disease |
| Pregabalin (245) | Gabapentin has also been shown to reduce pain (246) but may increase edema |
| Sympathomimetic amines (137) | Phentermine, dextroamphetamine, amphetamine; sympathomimetic amines resolved lipomas and liver fat in two cases of Dercum disease. |
Non-Medication Treatment of Dercum disease
People with Dercum disease should be offered manual or IAST therapies or pool/water therapy to reduce pain, improve mobility and impede progression of the disease. Manual lymphatic drainage combined with pregabalin improved weight and pain in a woman with Dercum disease (245). It has also been reported that fascia improved, pain reduced, and fat was lost after women with lipedema and Dercum disease received deep tissue therapy (86,126).
Liposuction has been used as treatment for Dercum disease (247), reducing pain by one point on a visual analogue scale (248) and improving insulin sensitivity (249). Surgeons removing lipomas by liposuction must have experience in the removal of fibrotic tissue and manual or IAST therapies should be performed before and after any surgery to keep inflammation levels at a minimum.
Transcutaneous frequency rhythmic electrical modulation system (FREMS) reduced pain and the size of lipomas in one case of Dercum disease (250). Cycling hypobaric air around ten people with Dercum disease improved pain and mental quality of life after five days of therapy (251). Cycling air around the body by sequential pneumatic compression pump therapy is also useful for people with Dercum disease due to the presence of lymphatic dysfunction (222,229).
Concluding Remarks on Dercum Disease
People with Dercum disease have painful lipomas and other signs and symptoms of a healing disorder. The different types of Dercum disease need to be delineated before any gene or biomarker can be found. The pain and associated signs and symptoms of Dercum disease should be treated to improve quality of life. People with Dercum disease may be at high risk for cardiovascular disease and cardiovascular risk factors should be closely monitored and treated when appropriate.
MULTIPLE SYMMETRIC LIPOMATOSIS
Multiple symmetric lipomatosis (MSL; OMIM#151800) also known as Madelung disease, Launois-Bensaude syndrome, cephalothoracic lipodystrophy, and benign symmetric lipomatosis is a rare disease first described by Brodie in 1846.This disorder is clearly not benign. Madelung reported data on 33 cases, but the classical description of the disease is attributed to Launois and Bensaude who published a detailed account of 65 cases in 1898. The literature on MSL was initially dominated by research on men with alcoholism; however, people who do not consume alcohol (252), women, and children are also affected (253).
There are different types of MSL described initially by two different groups and reclassified in 2018 based on a German cohort of 45 patients (Table 11 and Figure 10) (91).
Table 11.
Types of Multiple Symmetric Lipomatosis (Locations of Abnormal Fat Tissue)
| Types | Old Classification (254) | Old Classification (255) | New German Classification (91) |
|---|---|---|---|
| I | Neck, shoulders, supraclavicular triangle, and proximal upper limbs | Neck, upper back, shoulder girdle, and upper arms | Ia: Neck |
| Ib: Neck, shoulder girdle, upper arms | |||
| Ic: Neck, shoulder girdle, upper arms, chest, abdomen, upper and lower back | |||
| II | Abdomen and thighs | Shoulder girdle, deltoid region, upper arms, and thorax | Hips, bottom, and upper legs |
| III | Thigh or female type similar to lipedema | Gynecoid type: Thighs and medial side of the knees | General distribution skipping head, forearms, and lower legs |
| IV | NA | Abdominal type: Abdomen | NA |

Figure 10.
Two different presentations of MSL. The man has MSL with a Charcot Marie Tooth presentation with increased fat on the upper body even after multiple resections, and the woman on the right has increased fat on the arms and upper back consistent with the old classification of MSL Type II.
Women tend to have Type II MSL and the authors state that it is difficult to differentiate women with lipedema from women with MSL type II. Criteria the authors used to distinguish the two are “the hips and bottom are affected [in Type II MSL] which are not affected in patients suffering from lipedema.” Lipedema, however, does affect the hips and buttocks in Types I-III lipedema (Figure 3). Finding a gene or biomarker for lipedema and MSL will be ultimately be helpful in distinguishing these adipofascial disorders.
In rare cases, MSL SAT can invade the muscles of the tongue (256,257), vocal cords (258), and periorbital area (259). Tracheal or esophageal compression can occur resulting in superior vena cava syndrome (260).
Prevalence of MSL
Multiple symmetric lipomatosis is considered rare occurring 1:25,000 in a primarily male Italian population (261) and 1:25,000 in a German population where females outnumbered men 2.5:1 (91).
Genetics of MSL
Multiple deletions of mitochondrial DNA, and the myoclonus epilepsy and ragged red fibers (MERRF) tRNA(Lys) A>G(8344) mutation have been found in some cases of MSL (262,263) but not in others (264,265). Chalk et al. found no mitochondrial pathology or mutations in four siblings with MSL with a pattern favoring autosomal recessive (265). Another study examined individuals with mitochondrial mutations and found that MSL was a rare sign of mitochondrial disease with a strong association between multiple lipomas and lysine tRNA mutations (266). If triglyceride cannot be mobilized from fat, then along with adipogenesis (via microRNAs), fat would be expected to increase. Indeed, a mutation in the LIPE gene coding for hormone sensitive lipase was found to be mutated in a family with MSL and lipodystrophy (267).
Mutations in the MFN2 gene coding for mitofusin 2 have been found to cause MSL with Charcot Marie Tooth Disease (268). Mitofusin 2 helps to regulate the morphology of mitochondria by controlling the fusion process. Individuals with mutations in MFN2 have increased fat on the upper part of the body and a lipodystrophy or lack of fat on other aspects of the body. These data support pathophysiology of MSL hypothesis 1 above for the development of MSL but also support hypothesis 2 in that alcohol may cause widespread damage to mitochondria.
Pathophysiology of MSL
Hypothesis 1: Brown Adipose Tissue
The dorsocervical fat pad (buffalo hump) is thought to be a location of brown adipose tissue found both in MSL (264,269,270) and HIV-associated lipodystrophy (271-274) suggesting that the abnormal fat tissue in both of these conditions arises from brown adipocytes (275). Uncoupling protein (UCP)-1 has been shown to be activated in HIV-associated lipodystrophy and in agreement, calcyphosine-like (CAPSL), important in early adipogenesis, was down-regulated and uncoupling protein (UCP)-1 upregulated in eleven individuals, one with familial MSL and ten with sporadic MSL disease (276). Stromal vascular cells grown out of MSL fat tissue resulted in multiloculated adipocytes consistent with brown adipocytes (277,278). These data suggest that altered pre-adipocyte mesenchymal stem cells, adipogenesis and energy metabolism are important in development of MSL fat. In support, microRNAs miR-125a-3p and miR-483-5p are significantly increased in the fat of patients with MSL. These microRNAs promote adipogenesis through regulating the RhoA/ROCK1/ERK1/2 pathway (279). Finally, stem cells from MSL tissue showed significantly higher proliferative activity (280) suggesting a defect in regulation of adipogenesis. That brown fat was not found by 18 F-fluorodeoxyglucose (18 F-FDG) uptake using PET/CT in areas of MSL tissue (281) does not rule out the brown fat hypothesis as there may be browning of MSL fat rather than as strict replication of brown adipocytes.
Hypothesis 2: Inflammation, Alcohol and the Lymphatic System
Further research is needed to determine the exact pathophysiology involved in the development of MSL fat tissue, but the fact that alcohol is damaging to many tissues in the body suggests that inflammation may play a role. Interleukin-6 levels were elevated in MSL tissue compared to unaffected tissue (280), and ethanol intake increases CYP2E1 activity in adipose tissue, leading to apoptosis of adipocytes through activation of the pro-apoptotic Bcl-2 family protein Bid, resulting in activation of complement via C1q, and adipose tissue inflammation (282).
The liver produces over 50% of lymphatic fluid that enters the thoracic lymphatic ducts in the great veins in the neck (283). When the liver is fatty or cirrhotic, the liver produces even more lymphatic fluid (284). That many men with men with MSL develop fat around the neck in the location of the thoracic ducts or abdomen where the digestive tract transports approximately 2/3 of lymphatic fluid, becomes intriguing and may suggest involvement of the lymphatic system. Women have more developed vasculature, including lymphatics, in subcutaneous adipose tissue and therefore, if lymphatic vessels are important in the pathophysiology of MSL, they could be expected to have a different phenotype than men. Rats provided acute alcohol intoxication were found to have mesenteric lymphatic hyperpermeability (thoracic duct was not examined), a peri-lymphatic adipose tissue inflammatory response, and an altered systemic adipokine profile (285). When lymphatic vessels leak, fat grows (52). Alcohol and other mediators of lymphatic vessel leakage may therefore play a role in MSL.
Disorders Associated with MSL
Associated disorders include liver disease, dyslipidemia, metabolic syndrome, hypertriglyceridemia, hypothyroidism, diabetes mellitus, and peripheral and autonomic neuropathy (Figure 11).

Figure 11.
Disorders often associated with MSL (Madelung disease). Copyright © 2018 Szewc et al. (286). This work is published and licensed by Dove Medical Press Limited. Full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution – Non Commercial (unported, v3.0) License (http://creativecommons.org/licenses/by-nc/3.0/).
Morbidity and mortality in MSL is thought to be high with sudden non-coronary death accounting for a large percentage of deaths in one series of primarily men (254). The neuropathology of MSL is a distal axonal demyelination different from that associated with alcohol intake and impairment of autonomic function has been suggested as a possible cause of sudden death; this impairment seems to prevalently involve the autonomic nervous system and not related to a high alcohol intake.
Treatment of MSL
Anyone with MSL should be encouraged to stop intake of alcohol. The only definitive treatment of MSL is liposuction or excision of the MSL tissue. The advantages of lipectomy is more complete removal of MSL tissue and better control of iatrogenic damage to nearby structures. Liposuction, however, achieves good cosmetic results and is simpler and less invasive than lipectomy (287). Multiple symmetric lipomatosis tissue tends to recur after liposuction and even excision. Therefore, other treatments are needed to slow down the progression of this disease to improve quality of life. Some believe that combining excision with liposuction can reduce recurrence (288).
Mesotherapy is a procedure that involves injections of multiple substances such as pharmaceuticals and/or vitamins into subcutaneous fat to reduce the fat tissue or cellulite. Such substances include phosphatidylcholine, multivitamins, pentoxifylline, aminophylline, hyaluronic acid, yohimbine, collagenase and others. Mesotherapy has been used to treat MSL but the injections can cause fibrosis which can make excision or liposuction difficult (289).
Concluding Remarks on MSL
Multiple symmetric lipomatosis is a rare adipofasial disorder associated with alcohol use, but not always. The pathophysiology is unknown but may involve early adipogenesis, mitochondrial dysfunction, and brown adipose tissue formation. Women with MSL may have lipedema and vice versa, therefore a gene or biomarker is needed to identify people with different types of MSL. Surgical treatment remains the only therapy for MSL.
OVERALL CONCLUSIONS ON ADIPOFASCIAL DISEASES
Aipofascial diseases occur when there is an increase in adipofascial tissue on the body that becomes fibrotic and is resistant to loss by lifestyle change. Until such time that better understanding of the pathophysiology of these disorder hints at other treatment modalities, these disorders often require removal by surgical means. Many of the diseases overlap, making identification difficult and will remain so until additional genes or biomarkers are clinically available. A comparison table of the five adipofascial disorders presented in this chapter can be helpful (Table 12).
Table 12.
Comparison of Adipofascial Diseases
| Characteristic | Lipedema | DD | MSL | FML | Angiolipomas |
|---|---|---|---|---|---|
| Fat Location | Limbs | Global | Upper body | Trunk, arms, thighs | Global |
| Diet-resistant fat | Yes | Yes | Yes | Yes | Yes |
| Lipomas | + | +++ | +++ | +++ | +++ |
| Time SAT change | Puberty | Adult | Adult | Child, adult | Young adult |
| Painful SAT | Yes | Yes | Not usually | Not usually | Yes |
| Sex | Female | Female | Male | Male, female | Male, female |
| Lymphatic dysfunction | Yes | Yes | Yes | Possible | Unknown |
| Prevalence | Common | Rare | Rare | Rare | Rare |
| Associated conditions | Lymphedema | Autoimmune; diabetes | Neuropathy | Moles; neuropathy | Unknown |
| Inheritance Pattern | Autosomal dominant; incomplete penetrance | Autosomal dominant; sex-specific influence | Autosomal dominant or recessive | Autosomal dominant | Autosomal dominant; spontaneous |
| Gene | None | None | LIPE (267) MFN2 (268) tRNALys(266) | PALB2(156) | None |
| Biomarkers | None | None | miRNA (279) | None | None |
Abbreviations: miRNA: microRNA; PALB2; Partner and localizer of BRCA2
REFERENCES
- 1.
- Herbst KL. Rare adipose disorders (RADs) masquerading as obesity. Acta Pharmacol Sin 2012; 33:155-172. doi: 1 10.1038/aps.2011.1153. [PMC free article: PMC4010336] [PubMed: 22301856] [CrossRef]
- 2.
- Luong Q, Huang J, Lee KY. Deciphering White Adipose Tissue Heterogeneity. Biology (Basel) 2019; 8(2).biology8020023. doi: 80200 10.8023390/biology8020023. [PMC free article: PMC6628053] [PubMed: 30978929] [CrossRef]
- 3.
- Hussain I, Patni N, Garg A. Lipodystrophies, dyslipidaemias and atherosclerotic cardiovascular disease. Pathology 2019; 51:202-212. doi: 2 10.1016/j.pathol.2018.1011.1004. Epub 2018 Dec 1027. [PMC free article: PMC6402807] [PubMed: 30595509] [CrossRef]
- 4.
- Akinci B, Sahinoz M, Oral E. Lipodystrophy Syndromes: Presentation and Treatment. In: Feingold KR AB, Boyce A, Chrousos G, Dungan K, Grossman A, Hershman JM, Kaltsas G, Koch C, Kopp P, Korbonits M, McLachlan R, Morley JE, New M, Perreault L, Purnell J, Rebar R, Singer F, Trence DL, Vinik A, Wilson DP, ed. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-2018.
- 5.
- Hogan S, Velez MW, Kaminer MS. Updates on the understanding and treatment of cellulite. Semin Cutan Med Surg 2018; 37:242-246. doi: 2 10.12788/j.sder.12018.12056. [PubMed: 30475930] [CrossRef]
- 6.
- van der Valk ES, van den Akker ELT, Savas M, Kleinendorst L, Visser JA, Van Haelst MM, Sharma AM, van Rossum EFC. A comprehensive diagnostic approach to detect underlying causes of obesity in adults. Obes Rev 2019; 20:795-804. doi: 7 10.1111/obr.12836. Epub 12019 Mar 12831. [PMC free article: PMC6850662] [PubMed: 30821060] [CrossRef]
- 7.
- Kyrou I, Randeva HS, Tsigos C, Kaltsas G, Weickert MO. Clinical Problems Caused by Obesity. In: Feingold KR AB, Boyce A, Chrousos G, Dungan K, Grossman A, Hershman JM, Kaltsas G, Koch C, Kopp P, Korbonits M, McLachlan R, Morley JE, New M, Perreault L, Purnell J, Rebar R, Singer F, Trence DL, Vinik A, Wilson DP, ed. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-2018.
- 8.
- Gruzdeva O, Borodkina D, Uchasova E, Dyleva Y, Barbarash O. Localization of fat depots and cardiovascular risk. Lipids Health Dis 2018; 17:218. doi: 2 10.1186/s12944-12018-10856-12948. [PMC free article: PMC6138918] [PubMed: 30219068] [CrossRef]
- 9.
- Ahlman H. Nilsson. The gut as the largest endocrine organ in the body. Ann Oncol. 2001;12:S63–68. [PubMed: 11762354]
- 10.
- Coelho M, Oliveira T, Fernandes R. Biochemistry of adipose tissue: an endocrine organ. Archives of medical science. AMS. 2013;9:191–200. [PMC free article: PMC3648822] [PubMed: 23671428]
- 11.
- Chung KJ, Nati M, Chavakis T, Chatzigeorgiou A. Innate immune cells in the adipose tissue. Rev Endocr Metab Disord 2018; 19:283-292. doi: 2 10.1007/s11154-11018-19451-11156. [PubMed: 29922964] [CrossRef]
- 12.
- Del Corno M, Conti L, Gessani S. Innate Lymphocytes in Adipose Tissue Homeostasis and Their Alterations in Obesity and Colorectal Cancer. Front Immunol 2018; 9:2556.: 10.3389/fimmu.2018.02556. eCollection 02018. [PMC free article: PMC6230679] [PubMed: 30455701] [CrossRef]
- 13.
- Chen Y, Rehal S, Roizes S, Zhu HL, Cole WC, von der Weid PY. The pro-inflammatory cytokine TNF-alpha inhibits lymphatic pumping via activation of the NF-kappaB-iNOS signaling pathway. Microcirculation. 2017;24(3) [PMC free article: PMC5404961] [PubMed: 28231612] [CrossRef]
- 14.
- Arngrim N, Simonsen L, Holst JJ, Bulow J. Reduced adipose tissue lymphatic drainage of macromolecules in obese subjects: a possible link between obesity and local tissue inflammation? Int J Obes (Lond) 2013; 37:748-750. doi: 7 10.1038/ijo.2012.1098. Epub 2012 Jul 1033. [PubMed: 22751255] [CrossRef]
- 15.
- Blaak EE, van Baak MA, Kemerink GJ, Pakbiers MT, Heidendal GA, Saris WH. Beta-adrenergic stimulation and abdominal subcutaneous fat blood flow in lean, obese, and reduced-obese subjects. Metabolism. 1995;44:183–187. [PubMed: 7869913]
- 16.
- L'Hermitte F, Behar A, Paries J, Cohen-Boulakia F, Attali JR, Valensi P. Impairment of lymphatic function in women with gynoid adiposity and swelling syndrome. Metabolism. 2003;52:805–809. [PubMed: 12870153]
- 17.
- Kumar V, Abbas AK, Fausto N. Tissue renewal and repair: regeneration, healing, and fibrosis. In: Abbas VKAK, Fausto N, eds. Pathologic Basis of Disease. Philadelphia, PA, USA: Elsevier Saunders; 2005.
- 18.
- Usunier B, Benderitter M, Tamarat R, Chapel A. Management of fibrosis: the mesenchymal stromal cells breakthrough. Stem Cells Int 2014; 2014:340257.: 10.1155/2014/340257. Epub 342014 Jul 340214. [PMC free article: PMC4123563] [PubMed: 25132856] [CrossRef]
- 19.
- Sun K, Tordjman J, Clement K, Scherer PE. Fibrosis and adipose tissue dysfunction. Cell Metab 2013; 18:470-477. doi: 4 10.1016/j.cmet.2013.1006.1016. Epub 2013 Aug 1015. [PMC free article: PMC3795900] [PubMed: 23954640] [CrossRef]
- 20.
- Crewe C, An YA, Scherer PE. The ominous triad of adipose tissue dysfunction: inflammation, fibrosis, and impaired angiogenesis. J Clin Invest 2017; 127:74-82. doi: 10.1172/JCI88883. Epub 82017 Jan 88883. [PMC free article: PMC5199684] [PubMed: 28045400] [CrossRef]
- 21.
- Chabot K, Gauthier MS, Garneau PY, Rabasa-Lhoret R. Evolution of subcutaneous adipose tissue fibrosis after bariatric surgery. Diabetes Metab 2017; 43:125-133. doi: 1 10.1016/j.diabet.2016.1010.1004. Epub 2016 Nov 1011. [PubMed: 27843076] [CrossRef]
- 22.
- Bel Lassen P, Charlotte F, Liu Y, Bedossa P, Le Naour G, Tordjman J, Poitou C, Bouillot JL, Genser L, Zucker JD, Sokolovska N, Aron-Wisnewsky J, Clement K. The FAT Score, a Fibrosis Score of Adipose Tissue: Predicting Weight-Loss Outcome After Gastric Bypass. J Clin Endocrinol Metab 2017; 102:2443-2453. doi: 24 10.1210/jc.2017-00138. [PubMed: 28419237] [CrossRef]
- 23.
- Allen EV, Hines EAJ. Lipedema of the legs: A syndrome characterised by fat legs and orthostatic edema. Proc Staff Meet Mayo Clin. 1940;15:184–187.
- 24.
- Fife CE, Maus EA, Carter MJ. Lipedema: a frequently misdiagnosed and misunderstood fatty deposition syndrome. Adv 2010; 23:81-92; quiz 93-84. [PubMed: 20087075]
- 25.
- Beltran K, Herbst KL. Differentiating lipedema and Dercum's disease. Int J Obes (Lond). 2017;41:240–245. [PubMed: 27857136]
- 26.
- Herbst K, Mirkovskaya L, Bharhagava A, Chava Y, Te CH. Lipedema Fat and Signs and Symptoms of Illness, Increase with Advancing Stage. Archives of Medicine. 2015;7:1–8.
- 27.
- Meier-Vollrath I, Schmeller W. Lipoedema — current status, new perspectives. . Journal der Deutschen Dermatologischen Gesellschaft. 2004;2:181–186. [PubMed: 16281634]
- 28.
- Wold LE, Hines EA Jr, Allen EV. Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med. 1951;34:1243–1250. [PubMed: 14830102]
- 29.
- Coppel T, Cunneen J, Fetzer S, Gordon K, Hardy D, Jones J, McCarroll A, O'Neill C, Smith S, White C, Williams A. Best Practice Guidelines: The management of lipoedema. Wounds UK 2017;13(1). http://www.wounds-uk.com/best-practice-statements/best-practice-guidelines-the-management-of-lipoedema.
- 30.
- Herpertz U. Krankheitsspektrum des Lipödems an einer Lymphologischen Fachklinik - Erscheinungsformen, Mischbilder und Behandlungsmöglichkeiten. vasomed 1997:301-307.
- 31.
- Forner-Cordero I, Szolnoky G, Forner-Cordero A, Kemény L. Lipedema: an overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome - systematic review. Clinical Obesity. 2012;2:86–95. [PubMed: 25586162]
- 32.
- Schook CC, Mulliken JB, Fishman SJ, Alomari AI, Grant FD, Greene AK. Differential diagnosis of lower extremity enlargement in pediatric patients referred with a diagnosis of lymphedema. Plast Reconstr Surg 2011; 127:1571-1581. doi: 15 10.1097/PRS.1570b1013e31820a31864f31823. [PubMed: 21187804] [CrossRef]
- 33.
- Marshall M, Schwahn-Schreiber C. Prävalenz des Lipödems bei berufstätigen Frauen in Deutschland (Lipödem-3-Studie). Phlebologie. 2011;3:127–134.
- 34.
- Schmeller W, Meier-Vollrath I. Lipödem-aktuelles zu einem weitgehend unbekannter Krankheitsbild. Aktuelle Dermatologie. 2007;33:1–10.
- 35.
- Greer KE. Lipedema of the legs. Cutis. 1974;14:98.
- 36.
- Földi E, Földi M. Das Lipödem. In: Földi M, Földi E, Kubik S, eds. Lehrbuch der Lymphologie für Mediziner, Masseure und Physiotherapeuten. Munich Elsevier, Urban&Fischer; 2005:443-453.
- 37.
- Schmeller W, Hueppe M, Meier-Vollrath I. Tumescent liposuction in lipoedema yields good long-term results. Br J Dermatol 2012; 166:161-168. doi: 1 10.1111/j.1365-2133.2011.10566.x. Epub 12011 Nov 10517. [PubMed: 21824127] [CrossRef]
- 38.
- Child AH, Gordon KD, Sharpe P, Brice G, Ostergaard P, Jeffery S, Mortimer PS. Lipedema: an inherited condition. Am J Med Genet A 2010; 152A:970-976. doi: 9 10.1002/ajmg.a.33313. [PubMed: 20358611] [CrossRef]
- 39.
- Bano G, Mansour S, Brice G, Ostergaard P, Mortimer PS, Jeffery S, Nussey S. Pit-1 mutation and lipoedema in a family. Exp Clin Endocrinol Diabetes. 2009;118:377–380. [PubMed: 19609847]
- 40.
- Berryman DE, List EO, Coschigano KT, Behar K, Kim JK, Kopchick JJ. Comparing adiposity profiles in three mouse models with altered GH signaling. Growth Horm IGF Res 2004; 14:309-318. doi: 3 10.1016/j.ghir.2004.1002.1005. [PubMed: 15231300] [CrossRef]
- 41.
- Waxler JL, Guardino C, Feinn RS, Lee H, Pober BR, Stanley TL. Altered body composition, lipedema, and decreased bone density in individuals with Williams syndrome: A preliminary report. [PMC free article: PMC5490490] [PubMed: 28254647]
- 42.
- Paolacci S, Precone V, Acquaviva F, Chiurazzi P, Fulcheri E, Pinelli M, Buffelli F, Michelini S, Herbst KL, Unfer V, Bertelli M. Genetics of lipedema: new perspectives on genetic research and molecular diagnoses. European Review for Medical and Pharmacological Sciences. 2019;23:5581–5594. [PubMed: 31298310]
- 43.
- Zazulak BT, Paterno M, Myer GD, Romani WA, Hewett TE. The effects of the menstrual cycle on anterior knee laxity: a systematic review. Sports Med 2006; 36:847-862. doi: 8 10.2165/00007256-200636100-200600004. [PubMed: 17004848] [CrossRef]
- 44.
- Szolnoky G, Nemes A, Gavaller H, Forster T, Kemeny L. Lipedema is associated with increased aortic stiffness. Lymphology. 2012;45:71–79. [PubMed: 23057152]
- 45.
- Jagtman BA, Kuiper JP, Brakkee AJ. Phlebologie. 1984;37:315–319. [Measurements of skin elasticity in patients with lipedema of the Moncorps "rusticanus" type] [PubMed: 6494267]
- 46.
- Stanton AW, Svensson WE, Mellor RH, Peters AM, Levick JR, Mortimer PS. Differences in lymph drainage between swollen and non-swollen regions in arms with breast-cancer-related lymphoedema. Clin Sci (Lond). 2001;101:131–140. [PubMed: 11473486]
- 47.
- Kumar B, Lenert P. Joint Hypermobility Syndrome: Recognizing a Commonly Overlooked Cause of Chronic Pain. Am J Med 2017; 130:640-647. doi: 6 10.1016/j.amjmed.2017.1002.1013. Epub 2017 Mar 1010. [PubMed: 28286166] [CrossRef]
- 48.
- Tinkle B, Castori M, Berglund B, Cohen H, Grahame R, Kazkaz H, Levy H. Hypermobile Ehlers-Danlos syndrome (a.k.a. Ehlers-Danlos syndrome Type III and Ehlers-Danlos syndrome hypermobility type): Clinical description and natural history. Am J Med Genet C Semin Med Genet 2017; 175:48-69. doi: 10.1002/ajmg.c.31538. Epub 32017 Feb 31531. [PubMed: 28145611] [CrossRef]
- 49.
- Crescenzi R, Marton A, Donahue PMC, Mahany HB, Lants SK, Wang P, Beckman JA, Donahue MJ, Titze J. Tissue Sodium Content is Elevated in the Skin and Subcutaneous Adipose Tissue in Women with Lipedema. Obesity (Silver Spring) 2018; 26:310-317. doi: 3 10.1002/oby.22090. Epub 22017 Dec 22027. [PMC free article: PMC5783748] [PubMed: 29280322] [CrossRef]
- 50.
- Kakudo N, Morimoto N, Ogawa T, Taketani S, Kusumoto K. Hypoxia Enhances Proliferation of Human Adipose-Derived Stem Cells via HIF-1a Activation. PLoS One 2015; 10:e0139890. doi: 01398 10.0131371/journal.pone.0139890. eCollection 0132015. [PMC free article: PMC4605777] [PubMed: 26465938] [CrossRef]
- 51.
- Siems W, Grune T, Voss P, Brenke R. Anti-fibrosclerotic effects of shock wave therapy in lipedema and cellulite. Biofactors. 2005;24:275–282. [PubMed: 16403988]
- 52.
- Harvey NL, Srinivasan RS, Dillard ME, Johnson NC, Witte MH, Boyd K, Sleeman MW, Oliver G. Lymphatic vascular defects promoted by Prox1 haploinsufficiency cause adult-onset obesity. Nat Genet 2005; 37:1072-1081. Epub 2005 Sep 1018. [PubMed: 16170315]
- 53.
- Priglinger E, Wurzer C, Steffenhagen C, Maier J, Hofer V, Peterbauer A, Nuernberger S, Redl H, Wolbank S, Sandhofer M. The adipose tissue-derived stromal vascular fraction cells from lipedema patients: Are they different? Cytotherapy 2017; 19:849-860. doi: 8 10.1016/j.jcyt.2017.1003.1073. Epub 2017 Apr 1025. [PubMed: 28454682] [CrossRef]
- 54.
- Amann-Vesti BR, Franzeck UK, Bollinger A. Microlymphatic aneurysms in patients with lipedema. Lymphology. 2001;34:170–175. [PubMed: 11783595]
- 55.
- Stallworth JM, Hennigar GR, Jonsson HT Jr, Rodriguez O. The chronically swollen painful extremity. A detailed study for possible etiological factors. Journal of the American Medical Association. 1974;228:1656–1659. [PubMed: 4406664]
- 56.
- Miller NE, Michel CC, Nanjee MN, Olszewski WL, Miller IP, Hazell M, Olivecrona G, Sutton P, Humphreys SM, Frayn KN. Secretion of adipokines by human adipose tissue in vivo: partitioning between capillary and lymphatic transport. American journal of physiology Endocrinology and metabolism. 2011;301:E659–667. [PubMed: 21750269]
- 57.
- Homan EA, Kim YG, Cardia JP, Saghatelian A. Monoalkylglycerol ether lipids promote adipogenesis. J Am Chem Soc 2011; 133:5178-5181. doi: 51 10.1021/ja111173c. Epub 112011 Mar 111123. [PMC free article: PMC4761264] [PubMed: 21428285] [CrossRef]
- 58.
- Suga H, Araki J, Aoi N, Kato H, Higashino T, Yoshimura K. Adipose tissue remodeling in lipedema: adipocyte death and concurrent regeneration. J Cutan Pathol. 2009;3:3. [PubMed: 19281484]
- 59.
- Szel E, Kemeny L, Groma G, Szolnoky G. Pathophysiological dilemmas of lipedema. Med Hypotheses 2014; 83:599-606. doi: 5 10.1016/j.mehy.2014.1008.1011. Epub 2014 Aug 1023. [PubMed: 25200646] [CrossRef]
- 60.
- AL-Ghadban S. Cromer W, Allen M, Ussery C, Badowski M, Harris D, Herbst KL. Dilated Blood and Lymphatic Microvessels, Angiogenesis, Increased Macrophages, and Adipocyte Hypertrophy in Lipedema Thigh Skin and Fat Tissue. Journal of Obesity. 2019 [PMC free article: PMC6425411] [PubMed: 30949365]
- 61.
- Weitman ES, Aschen SZ, Farias-Eisner G, Albano N, Cuzzone DA, Ghanta S, Zampell JC, Thorek D, Mehrara BJ. Obesity impairs lymphatic fluid transport and dendritic cell migration to lymph nodes. PLoS One 2013; 8:e70703. doi: 707 10.71371/journal.pone.0070703. eCollection 0072013. [PMC free article: PMC3741281] [PubMed: 23950984] [CrossRef]
- 62.
- Brautigam P, Foldi E, Schaiper I, Krause T, Vanscheidt W, Moser E. Analysis of lymphatic drainage in various forms of leg edema using two compartment lymphoscintigraphy. Lymphology. 1998;31:43–55. [PubMed: 9664268]
- 63.
- Witte CL, Witte MH, Unger EC, Williams WH, Bernas MJ, McNeill GC, Stazzone AM. Advances in imaging of lymph flow disorders. Radiographics. 2000;20:1697–1719. [PubMed: 11112825]
- 64.
- Gould DJ, El-Sabawi B, Goel P, Badash I, Colletti P, Patel KM. Uncovering Lymphatic Transport Abnormalities in Patients with Primary Lipedema. J Reconstr Microsurg 2019; 23:0039-1697904. [PubMed: 31546262]
- 65.
- Brorson H, Fagher B. Lakartidningen. 1996;93:1430–1433-1436. [Dercum's disease. Fatty tissue rheumatism caused by immune defense reaction?] [PubMed: 8667732]
- 66.
- Roldan M, Macias-Gonzalez M, Garcia R, Tinahones FJ, Martin M. Obesity short-circuits stemness gene network in human adipose multipotent stem cells. FASEB J 2011; 25:4111-4126. doi: 41 10.1096/fj.4110-171439. Epub 172011 Aug 171416. [PubMed: 21846837] [CrossRef]
- 67.
- Bauer AT. D VL, Lossagk K, Hopfner U, Kirsch M, Moog P, Bauer H, Machens HG, Schmauss D. Adipose stem cells from lipedema and control adipose tissue respond differently to adipogenic stimulation in vitro. Plast Reconstr Surg. 2019;6:0000000000005918. [PubMed: 31461015]
- 68.
- Piche ME, Vasan SK, Hodson L, Karpe F. Relevance of human fat distribution on lipid and lipoprotein metabolism and cardiovascular disease risk. Curr Opin Lipidol 2018; 29:285-292. doi: 2 10.1097/MOL.0000000000000522. [PubMed: 29994839] [CrossRef]
- 69.
- Torre YS, Wadeea R, Rosas V, Herbst KL. Lipedema: friend and foe. Horm Mol Biol Clin Investig 2018; 33(1)./j/hmbci.ahead-of-print/hmbci-2017-0076/hmbci-2017-0076.xml. doi: 20 10.1515/hmbci-2017-0076. [PMC free article: PMC5935449] [PubMed: 29522416] [CrossRef]
- 70.
- Nemes A, Kormanyos A, Domsik P, Kalapos A, Kemeny L, Forster T, Szolnoky G. Left ventricular rotational mechanics differ between lipedema and lymphedema: Insights from the three-dimensional speckle tracking echocardiographic MAGYAR-path study. Lymphology. 2018;51:102–108. [PubMed: 30422432]
- 71.
- Kozel BA, Danback JR, Waxler JL, Knutsen RH, de Las Fuentes L, Reusz GS, Kis E, Bhatt AB, Pober BR. Williams syndrome predisposes to vascular stiffness modified by antihypertensive use and copy number changes in NCF1. Hypertension 2014; 63:74-79. doi: 10.1161/HYPERTENSIONAHA.1113.02087. Epub 02013 Oct 02014. [PMC free article: PMC3932371] [PubMed: 24126171] [CrossRef]
- 72.
- Witte CL, Witte MH, Unger EC, Williams WH, Bernas MJ, McNeill GC, Stazzone AM. Advances in Imaging of Lymph Flow Disorders. RadioGraphics. 2000;20:1697–1719. [PubMed: 11112825]
- 73.
- Forner-Cordero I, Olivan-Sasot P, Ruiz-Llorca C, Munoz-Langa J. Lymphoscintigraphic findings in patients with lipedema. Rev Esp Med Nucl Imagen Mol 2018; 37:341-348. doi: 3 10.1016/j.remn.2018.1006.1008. Epub 2018 Aug 1028. [PubMed: 30166264] [CrossRef]
- 74.
- Bilancini S, Lucchi M, Tucci S, Eleuteri P. Functional lymphatic alterations in patients suffering from lipedema. Angiology. 1995;46:333–339. [PubMed: 7726454]
- 75.
- Tiedjen KV, Knorz S. Different Methods of diagnostic imaging in lymphedema, lipedema and venous disorders: Indirect lymphography, xeroradiography, CT and isotope lymphography. In: Cluzan RV, Pecking AP, Lokiec FM, eds. Progress in lymphology: XIII, Int. Congress of Lymphology. Amsterdam: Elsevier Science Publishers B.V.; 1992.
- 76.
- Dietzel R, Reisshauer A, Jahr S, Calafiore D, Armbrecht G. Body composition in lipoedema of the legs using Dual-Energy-X-Ray-Absorptiometry - a case control study. Br J Dermatol. 2015;1:13697. [PubMed: 25641018]
- 77.
- Dimakakos PB, Stefanopoulos T, Antoniades P, Antoniou A, Gouliamos A, Rizos D. MRI and ultrasonographic findings in the investigation of lymphedema and lipedema. Int Surg. 1997;82:411–416. [PubMed: 9412843]
- 78.
- Iker E, Mayfield CK, Gould DJ, Patel KM. Characterizing Lower Extremity Lymphedema and Lipedema with Cutaneous Ultrasonography and an Objective Computer-Assisted Measurement of Dermal Echogenicity. Lymphat Res Biol. 2019:7. [PubMed: 30615553]
- 79.
- Hirsch T, Schleinitz J, Marshall M, Faerber G. Is the differential diagnosis of lipoedema by means of high-resolution ultrasonography possible? Phlebologie. 2018:47.
- 80.
- Halk AB, Damstra RJ. First Dutch guidelines on lipedema using the international classification of functioning, disability and health. Phlebology. 2016;12:0268355516639421. [PubMed: 27075680]
- 81.
- Lohrmann C, Foeldi E, Langer M. MR imaging of the lymphatic system in patients with lipedema and lipo-lymphedema. Microvasc Res 2009; 77:335-339. Epub 2009 Jan 2027. [PubMed: 19323976]
- 82.
- Machnik A, Neuhofer W, Jantsch J, Dahlmann A, Tammela T, Machura K, Park JK, Beck FX, Muller DN, Derer W, Goss J, Ziomber A, Dietsch P, Wagner H, van Rooijen N, Kurtz A, Hilgers KF, Alitalo K, Eckardt KU, Luft FC, Kerjaschki D, Titze J. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med 2009; 15:545-552. doi: 5 10.1038/nm.1960. Epub 2009 May 1033. [PubMed: 19412173] [CrossRef]
- 83.
- Allison MA, Cushman M, Callas PW, Denenberg JO, Jensky NE, Criqui MH. Adipokines are associated with lower extremity venous disease: the San Diego population study. J Thromb Haemost 2010; 8:1912-1918. doi: 19 10.1111/j.1538-7836.2010.03941.x. [PMC free article: PMC4078899] [PubMed: 20546124] [CrossRef]
- 84.
- Greene AK. Diagnosis and Management of Obesity-Induced Lymphedema. Plast Reconstr Surg 2016; 138:111e-118e. doi: 1 10.1097/PRS.0000000000002258. [PubMed: 27348673] [CrossRef]
- 85.
- Mortimer PS. Implications of the lymphatic system in CVI-associated edema. Angiology. 2000;51:3–7. [PubMed: 10667636] [CrossRef]
- 86.
- Ibarra M, Eekema A, Ussery C, Neuhardt D, Garby K, Herbst KL. Subcutaneous adipose tissue therapy reduces fat by dual X-ray absorptiometry scan and improves tissue structure by ultrasound in women with lipoedema and Dercum disease. Clin Obes 2018; 8:398-406. doi: 3 10.1111/cob.12281. Epub 12018 Sep 12224. [PubMed: 30248251] [CrossRef]
- 87.
- Dudek JE, Bialaszek W, Ostaszewski P, Smidt T. Depression and appearance-related distress in functioning with lipedema. Psychol Health Med. 2018;3:1–8. [PubMed: 29614880]
- 88.
- Foldi E, Foldi M. Lipedema. In: Foldi M, Foldi E, eds. Foldi's Textbook of Lymphology. Munich, Germany: Elsevier GmbH; 2006:420.
- 89.
- Stutz JJ. All about lipedema. human med AG 2015;
- 90.
- Bulbena A, Baeza-Velasco C, Bulbena-Cabre A, Pailhez G, Critchley H, Chopra P, Mallorqui-Bague N, Frank C, Porges S. Psychiatric and psychological aspects in the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet 2017; 175:237-245. doi: 2 10.1002/ajmg.c.31544. Epub 32017 Feb 31510. [PubMed: 28186381] [CrossRef]
- 91.
- Schiltz D, Anker A, Ortner C, Tschernitz S, Koller M, Klein S, Felthaus O, Schreml J, Schreml S, Prantl L. Multiple Symmetric Lipomatosis: New Classification System Based on the Largest German Patient Cohort. Plast Reconstr Surg Glob Open 2018; 6:e1722. doi: 17 10.1097/GOX.0000000000001722. eCollection 0000000000002018 Apr. [PMC free article: PMC5977945] [PubMed: 29876171] [CrossRef]
- 92.
- Wold LE, Hines EA Jr, Allen EV. Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med. 1951;34:1243–1250. [PubMed: 14830102]
- 93.
- Hodson S, Eaton SE. Lipoedema management: Gaps in our knowledge. Journal of Lymphoedema. 2013;8:30–34.
- 94.
- Partsch H, Stoberl C, Urbanek A, Wenzel-Hora BI. Clinical use of indirect lymphography in different forms of leg edema. Lymphology. 1988;21:152–160. [PubMed: 3199874]
- 95.
- Ehrlich C, Iker E, Herbst KL, Kahn LA, Sears DD, Kenyon M. Lymphedema and Lipedema Nutrition Guide. Foods, vitamins, minerals, and supplements. San Francisco: Lymph Notes.
- 96.
- Reich-Schupke S, Schmeller W, Brauer WJ, Cornely ME, Faerber G, Ludwig M, Lulay G, Miller A, Rapprich S, Richter DF, Schacht V, Schrader K, Stucker M, Ure C. S1 guidelines: Lipedema. J Dtsch Dermatol Ges 2017; 15:758-767. doi: 7 10.1111/ddg.13036. [PubMed: 28677175] [CrossRef]
- 97.
- Khalaf MM, Ashem HA. Suggested physical therapy protocol for reduction of lipomatosis dolorosa of the legs. Egyptian Journal of Medical Human Genetics. 2013;14:103–108.
- 98.
- van Esch-Smeenge J, Damstra RJ, Hendrickx AA. Muscle strength and functional exercise capacity in patients with lipoedema and obesity: a comparative study. Journal of Lymphoedema. 2017;12:27–31.
- 99.
- Westermann S, Rief W, Euteneuer F, Kohlmann S. Social exclusion and shame in obesity. Eat Behav 2015; 17:74-6.: 10.1016/j.eatbeh.2015.1001.1001. Epub 2015 Jan 1010. [PubMed: 25615911] [CrossRef]
- 100.
- Sandhofer M, Schauer P, Sandhofer M, Anderhuber F. Lipödem. Journal für Ästhetische Chirurgie. 2017;10:61–70.
- 101.
- Heitink MV, Schurink GWH, de Pont CDJM, van Kroonenburgh MJPG, Veraart JCJM. Lymphedema after Greater Saphenous Vein Surgery. EJVES Extra. 2009;18:41–43.
- 102.
- Bast JH, Ahmed L, Engdahl R. Lipedema in patients after bariatric surgery. Surg Obes Relat Dis 2016; 12:1131-1132. doi: 11 10.1016/j.soard.2016.1104.1013. Epub 2016 Apr 1114. [PubMed: 27317598] [CrossRef]
- 103.
- Neutze D, Roque J. Clinical Evaluation of Bleeding and Bruising in Primary Care. Am Fam Physician. 2016;93:279–286. [PubMed: 26926815]
- 104.
- Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema-results of a study with 25 patients. J Dtsch Dermatol Ges 2011; 9:33-40. doi: 10.1111/j.1610-0387.2010.07504.x. Epub 02010 Sep 07507. [PubMed: 21166777] [CrossRef]
- 105.
- Schmeller W, Meier-Vollrath I. Tumescent liposuction: a new and successful therapy for lipedema. J Cutan Med Surg. 2006;10:7–10. [PubMed: 17241565]
- 106.
- Stutz JJ, Krahl D. Water jet-assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic Plast Surg 2009; 33:153-162. doi: 1 10.1007/s00266-00008-09214-y. Epub 02008 Jul 00229. [PubMed: 18663515] [CrossRef]
- 107.
- Wollina U, Goldman A, Heinig B. Microcannular tumescent liposuction in advanced lipedema and Dercum's disease. G 145:151-159. [PubMed: 20467389]
- 108.
- Gadelha Alcidarta dR, de Miranda Leão TL. Rule of four: a simple and safe formula for tumescent anesthesia in dermatologic surgical procedures. Surgical & Cosmetic Dermatology. 2009;1:99–102.
- 109.
- Sattler G, Rapprich S, Hagedorn M. Tumeszenz-Lokalanästhesie – Untersuchung zur Pharmakokinetik von Prilocain. Zeitschrift fur Hautkrankheiten. 1997;7:522–525.
- 110.
- Rapprich S, Baum S, Kaak I, Kottmann T, Podda M. Treatment of lipoedema using liposuction. Results of our own surveys. Phlebologie. 2015;44:121–132.
- 111.
- Pollock H, Forman S, Pollock T, Raccasi M. Conscious sedation/local anesthesia in the office-based surgical and procedural facility. Clin Plast Surg 2013; 40:383-388. doi: 3 10.1016/j.cps.2013.1004.1014. Epub 2013 May 1023. [PubMed: 23830746] [CrossRef]
- 112.
- Amron D. 2016 Liposuction Panel. Living with Lipedema and Dealing with Dercum's Disease,; 2016; St. Louis, Missouri.
- 113.
- Hattori J, Yamakage M, Seki S, Okazaki K, Namiki A. Inhibitory effects of the anesthetics propofol and sevoflurane on spontaneous lymphatic vessel activity in rats. Anesthesiology. 2004;101:687–694. [PubMed: 15329593]
- 114.
- Takeshita T, Morio M, Kawahara M, Fujii K. Halothane-induced changes in contractions of mesenteric lymphatics of the rat. Lymphology. 1988;21:128–130. [PubMed: 3221719]
- 115.
- McHale NG, Thornbury KD. The effect of anesthetics on lymphatic contractility. Microvasc Res. 1989;37:70–76. [PubMed: 2921950]
- 116.
- Quin JW, Shannon AD. The effect of anaesthesia and surgery on lymph flow, protein and leucocyte concentration in lymph of the sheep. Lymphology. 1975;8:126–135. [PubMed: 1214507]
- 117.
- Baumgartner A, Hueppe M, Schmeller W. Long-term benefit of liposuction in patients with lipoedema.A follow-up study after an average of 4 and 8 years. Br J Dermatol. 2015;17:14289. [PubMed: 26574236]
- 118.
- Rapprich S, Loehnert M, Hagedorn M. Therapy of lipoedema syndrome by liposuction under tumescent local anaesthesia. Ann Dermatol Venereol 2002; 129:1S711-
- 119.
- Szolnoky G, Borsos B, Barsony K, Balogh M, Kemeny L. Complete decongestive physiotherapy with and without pneumatic compression for treatment of lipedema: a pilot study. Lymphology. 2008;41:40–44. [PubMed: 18581957]
- 120.
- Szolnoky G, Nagy N, Kovacs RK, Dosa-Racz E, Szabo A, Barsony K, Balogh M, Kemeny L. Complex decongestive physiotherapy decreases capillary fragility in lipedema. Lymphology. 2008;41:161–166. [PubMed: 19306662]
- 121.
- Szolnoky G, Varga E, Varga M, Tuczai M, Dosa-Racz E, Kemeny L. Lymphedema treatment decreases pain intensity in lipedema. Lymphology. 2011;44:178–182. [PubMed: 22458119]
- 122.
- Belgrado JP, Vandermeeren L, Vankerckhove S, Valsamis JB, Malloizel-Delaunay J, Moraine JJ, Liebens F. Near-Infrared Fluorescence Lymphatic Imaging to Reconsider Occlusion Pressure of Superficial Lymphatic Collectors in Upper Extremities of Healthy Volunteers. Lymphat Res Biol 2016; 14:70-77. doi: 10.1089/lrb.2015.0040. Epub 2016 May 1011. [PMC free article: PMC4926199] [PubMed: 27167187] [CrossRef]
- 123.
- Iliff JJ, Wang M, Liao Y, Plogg BA, Peng W, Gundersen GA, Benveniste H, Vates GE, Deane R, Goldman SA, Nagelhus EA, Nedergaard M. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci Transl Med 2012; 4:147ra111. doi: 1 10.1126/scitranslmed.3003748. [PMC free article: PMC3551275] [PubMed: 22896675] [CrossRef]
- 124.
- Macdonald JM, Sims N, Mayrovitz HN. Lymphedema, lipedema, and the open wound: the role of compression therapy. Surg Clin North Am. 2003;83:639–658. [PubMed: 12822730]
- 125.
- Schneider M, Conway EM, Carmeliet P. Lymph makes you fat. Nat Genet. 2005;37:1023–1024. [PubMed: 16195715]
- 126.
- Herbst KL, Ussery C, Eekema A. Pilot study: whole body manual subcutaneous adipose tissue (SAT) therapy improved pain and SAT structure in women with lipedema. LID - 10.1515/hmbci-2017-0035 [doi] LID - /j/hmbci.ahead-of-print/hmbci-2017-0035/hmbci-2017-0035.xml [pii]. Horm Mol Biol Clin Investig 2017; [PubMed: 28930626] [CrossRef]
- 127.
- Yan B-h, Peng Q-s, Wei Q-h, Feng F. The effect of meridian massage on 8M, 8MI, WC and HC in simple obesity patients: a randomized controlled trial. World Journal ofAcupuncture-Moxibustion (WJAM) 2014; 24:6-9, 50.
- 128.
- Moyer-Mileur LJ, Haley S, Slater H, Beachy J, Smith SL. Massage Improves Growth Quality by Decreasing Body Fat Deposition in Male Preterm Infants. The Journal of pediatrics. 2013;162:490–495. [PMC free article: PMC3549027] [PubMed: 23062248]
- 129.
- Sevier TL, Stegink-Jansen CW. Astym treatment vs. eccentric exercise for lateral elbow tendinopathy: a randomized controlled clinical trial. PeerJ 2015; 3:e967.: 10.7717/peerj.7967. eCollection 2015. [PMC free article: PMC4451036] [PubMed: 26038722] [CrossRef]
- 130.
- Lee JH, Lee DK, Oh JS. The effect of Graston technique on the pain and range of motion in patients with chronic low back pain. J Phys Ther Sci 2016; 28:1852-1855. doi: 18 10.1589/jpts.1828.1852. Epub 2016 Jun 1828. [PMC free article: PMC4932073] [PubMed: 27390432] [CrossRef]
- 131.
- Braun M, Schwickert M, Nielsen A, Brunnhuber S, Dobos G, Musial F, Ludtke R, Michalsen A. Effectiveness of traditional Chinese "gua sha" therapy in patients with chronic neck pain: a randomized controlled trial. Pain Med 2011; 12:362-369. doi: 3 10.1111/j.1526-4637.2011.01053.x. Epub 02011 Jan 01028. [PubMed: 21276190] [CrossRef]
- 132.
- Mehta P, Dhapte V. Cupping therapy: A prudent remedy for a plethora of medical ailments. J Tradit Complement Med 2015; 5:127-134. doi: 1 10.1016/j.jtcme.2014.1011.1036. eCollection 2015 Jul. [PMC free article: PMC4488563] [PubMed: 26151023] [CrossRef]
- 133.
- Ai JW, Liu JT, Pei SD, Liu Y, Li DS, Lin HM, Pei B. The effectiveness of pressure therapy (15-25 mmHg) for hypertrophic burn scars: A systematic review and meta-analysis. Sci Rep. 2017;7:40185. [PMC free article: PMC5215680] [PubMed: 28054644] [CrossRef]
- 134.
- Phelan SM, Burgess DJ, Yeazel MW, Hellerstedt WL, Griffin JM, van Ryn M. Impact of weight bias and stigma on quality of care and outcomes for patients with obesity. Obes Rev 2015; 16:319-326. doi: 3 10.1111/obr.12266. Epub 12015 Mar 12265. [PMC free article: PMC4381543] [PubMed: 25752756] [CrossRef]
- 135.
- Dudek JE, Bialaszek W, Ostaszewski P. Quality of life in women with lipoedema: a contextual behavioral approach. Qual Life Res 2016; 25:401-408. doi: 4 10.1007/s11136-11015-11080-x. Epub 12015 Jul 11128. [PubMed: 26216585] [CrossRef]
- 136.
- McHale NG, Allen JM, Iggulden HL. Mechanism of alpha-adrenergic excitation in bovine lymphatic smooth muscle. Am J Physiol. 1987;252:H873–878. [PubMed: 3034080]
- 137.
- Herbst KL, Abu-Zaid L, Fazel MT. Question-Based Self-Reported Experience of Patients with Subcutaneous Adipose Tissue (SAT) Disease Prescribed Sympathomimetic Amines. Medical Research Archives. 2019;7:1–17.
- 138.
- Feldo M, Wozniak M, Wojciak-Kosior M, Sowa I, Kot-Wasik A, Aszyk J, Bogucki J, Zubilewicz T, Bogucka-Kocka A. Influence of Diosmin Treatment on the Level of Oxidative Stress Markers in Patients with Chronic Venous Insufficiency. Oxid Med Cell Longev 2018; 2018:2561705.: 10.1155/2018/2561705. eCollection 2562018. [PMC free article: PMC6136498] [PubMed: 30228853] [CrossRef]
- 139.
- Li X, Li J, Wang L, Li A, Qiu Z, Qi LW, Kou J, Liu K, Liu B, Huang F. The role of metformin and resveratrol in the prevention of hypoxia-inducible factor 1alpha accumulation and fibrosis in hypoxic adipose tissue. Br J Pharmacol 2016; 173:2001-2015. doi: 20 10.1111/bph.13493. Epub 12016 May 13415. [PMC free article: PMC4882491] [PubMed: 27059094] [CrossRef]
- 140.
- Biondo LA, Batatinha HA, Souza CO, Teixeira AAS, Silveira LS, Alonso-Vale MI, Oyama LM, Alves MJ, Seelaender M, Neto JCR. Metformin Mitigates Fibrosis and Glucose Intolerance Induced by Doxorubicin in Subcutaneous Adipose Tissue. Front Pharmacol 2018; 9:452.: 10.3389/fphar.2018.00452. eCollection 02018. [PMC free article: PMC5952005] [PubMed: 29867463] [CrossRef]
- 141.
- Conley SM, Bruhn RL, Morgan PV, Stamer WD. Selenium's effects on MMP-2 and TIMP-1 secretion by human trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2004;45:473–479. [PubMed: 14744887]
- 142.
- Lewin MH, Arthur JR, Riemersma RA, Nicol F, Walker SW, Millar EM, Howie AF, Beckett GJ. Selenium supplementation acting through the induction of thioredoxin reductase and glutathione peroxidase protects the human endothelial cell line EAhy926 from damage by lipid hydroperoxides. Biochim Biophys Acta. 2002;1593:85–92. [PubMed: 12431787] [CrossRef]
- 143.
- Horvathova M, Jahnova E, Gazdik F. Effect of selenium supplementation in asthmatic subjects on the expression of endothelial cell adhesion molecules in culture. Biol Trace Elem Res. 1999;69:15–26. [PubMed: 10383096]
- 144.
- Kiremidjian-Schumacher L, Roy M, Glickman R, Schneider K, Rothstein S, Cooper J, Hochster H, Kim M, Newman R. Selenium and immunocompetence in patients with head and neck cancer. Biol Trace Elem Res. 2000;73:97–111. [PubMed: 11049203]
- 145.
- Micke O, Bruns F, Schäfer U, Kisters K, Hesselmann S, Willich N. Selenium in the treatment of acute and chronic lymphedema. Trace Elements and Electrolytes. 2000;17:206–209.
- 146.
- Kasseroller RG, Schrauzer GN. Treatment of secondary lymphedema of the arm with physical decongestive therapy and sodium selenite: a review. Am J Ther. 2000;7:273–279. [PubMed: 11486162]
- 147.
- Medicine Io. Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. Washington, DC: The National Academies Press. [PubMed: 25077263]
- 148.
- Prabhu KS, Lei XG. Selenium. Adv Nutr 2016; 7:415-417. doi: 4 10.3945/an.3115.010785. Print 012016 Mar. [PMC free article: PMC4785479] [PubMed: 26980826] [CrossRef]
- 149.
- Nourollahi S, Mondry TE, Herbst KL. Bucher’s Broom and Selenium Improve Lipedema: A Retrospective Case Study. Alternative and Integrative Medicine. 2013;2:1–7.
- 150.
- Rabbiosi G, Borroni G, Scuderi N. Familial multiple lipomatosis. Acta Derm Venereol. 1977;57:265–267. [PubMed: 71835]
- 151.
- Mohar N. Familial multiple lipomatosis. Acta Derm Venereol. 1980;60:509–513. [PubMed: 6162336]
- 152.
- Tana C, Tchernev G. Images in clinical medicine. Familial multiple lipomatosis. N Engl J Med 2014; 371:1237. doi: 12 10.1056/NEJMicm1316241. [PubMed: 25251618] [CrossRef]
- 153.
- Pack GT, Ariel IM. Tumors of the Soft Somatic Tissues: A Clinical Treatise. New York: Hoeber-Harper.
- 154.
- Campen R, Mankin H, Louis DN, Hirano M, Maccollin M. Familial occurrence of adiposis dolorosa. J Am Acad Dermatol. 2001;44:132–136. [PubMed: 11148491]
- 155.
- Ware R, Mane A, Saini S, Saini N. Familial multiple lipomatosis—a rare syndrome diagnosed on FNAC. International Journal of Medical Science and Public Health. 2016;5:367–369.
- 156.
- Reddy N, Malipatil B, Kumar S. A rare case of familial multiple subcutaneous lipomatosis with novel PALB2 mutation and increased predilection to cancers. Hematol Oncol Stem Cell Ther 2016; 9:154-156. doi: 1 10.1016/j.hemonc.2016.1001.1001. Epub 2016 Jan 1027. [PubMed: 26845227] [CrossRef]
- 157.
- Singh G, Jialal I. Multiple Endocrine Neoplasia Type 1 (MEN I, Wermer Syndrome). 2019;
- 158.
- Genuardi M, Klutz M, Devriendt K, Caruso D, Stirpe M, Lohmann DR. Multiple lipomas linked to an RB1 gene mutation in a large pedigree with low penetrance retinoblastoma. Eur J Hum Genet. 2001;9:690–694. [PubMed: 11571558]
- 159.
- Liaw D, Marsh DJ, Li J, Dahia PL, Wang SI, Zheng Z, Bose S, Call KM, Tsou HC, Peacocke M, Eng C, Parsons R. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet. 1997;16:64–67. [PubMed: 9140396] [CrossRef]
- 160.
- Yehia L, Ni Y, Sesock K, Niazi F, Fletcher B, Chen HJL, LaFramboise T, Eng C. Unexpected cancer-predisposition gene variants in Cowden syndrome and Bannayan-Riley-Ruvalcaba syndrome patients without underlying germline PTEN mutations. PLoS Genet 2018; 14:e1007352. doi: 10073 10.1001371/journal.pgen.1007352. eCollection 1002018 Apr. [PMC free article: PMC5933810] [PubMed: 29684080] [CrossRef]
- 161.
- Bracaglia R, D'Ettorre M, Gentileschi S, Mingrone G, Tambasco D. Multiple lipomatosis after stem cell trasplant and chemotherapy: a case report. Eur Rev Med Pharmacol Sci. 2014;18:413–415. [PubMed: 24563443]
- 162.
- Cronin PA, Myers E, Redmond HP, O'Reilly S, Kirwan WO. Lipomatosis: an unusual side-effect of cytotoxic chemotherapy? Acta Derm Venereol 2010; 90:303-304. doi: 3 10.2340/00015555-00010823. [PubMed: 20526554] [CrossRef]
- 163.
- Tsao H, Sober AJ. Multiple lipomatosis in a patient with familial atypical mole syndrome. Br J Dermatol. 1998;139:1118–1119. [PubMed: 9990390]
- 164.
- Djuric-Stefanovic A, Ebrahimi K, Sisevic J, Saranovic D. Gastroduodenal Lipomatosis in Familial Multiple Lipomatosis. Med Princ Pract 2017; 26:189-191. doi: 1 10.1159/000454714. Epub 000452016 Nov 000454724. [PMC free article: PMC5588370] [PubMed: 27884011] [CrossRef]
- 165.
- Sayar I, Demirtas L, Gurbuzel M, Isik A, Peker K, Gulhan B. Familial multiple lipomas coexisting with celiac disease: a case report. J Med Case Rep. 2014;8:309. [PMC free article: PMC4170234] [PubMed: 25227743] [CrossRef]
- 166.
- Arabadzhieva E, Yonkov A, Bonev S, Bulanov D, Taneva I, Ivanova V, Dimitrova V. A rare combination between familial multiple lipomatosis and extragastrointestinal stromal tumor. Int J Surg Case Rep 2015; 14:117-20.: 10.1016/j.ijscr.2015.1007.1027. Epub 2015 Jul 1031. [PMC free article: PMC4573610] [PubMed: 26263450] [CrossRef]
- 167.
- Nunes JC, Martins RF, Bastos A, Claudino LS, Guarnieri R, Lima Dde C, Schroeder HK, Lin K, Walz R. Brain lipoma, corpus callosum hypoplasia and polymicrogyria in familial multiple lipomatosis. Clin Neurol Neurosurg 2013; 115:1157-1159. doi: 11 10.1016/j.clineuro.2012.1109.1023. Epub 2012 Oct 1130. [PubMed: 23116686] [CrossRef]
- 168.
- Oktenli C, Gul D, Deveci MS, Saglam M, Upadhyaya M, Thompson P, Consoli C, Kocar IH, Pilarski R, Zhou XP, Eng C. Unusual features in a patient with neurofibromatosis type 1: multiple subcutaneous lipomas, a juvenile polyp in ascending colon, congenital intrahepatic portosystemic venous shunt, and horseshoe kidney. Am J Med Genet A. 2004;127:298–301. [PubMed: 15150783]
- 169.
- Morelli A, Falchetti A, Weinstein L, Fabiani S, Tomassetti P, Enzi G, Carraro R, Bordi C, Tonelli F, Brandi ML. RFLP analysis of human chromosome 11 region q13 in multiple symmetric lipomatosis and multiple endocrine neoplasia type 1-associated lipomas. Biochem Biophys Res Commun 1995; 207:363-368. doi: 3 10.1006/bbrc.1995.1196. [PubMed: 7531972] [CrossRef]
- 170.
- Bianchi M, Saletti V, Micheli R, Esposito S, Molinaro A, Gagliardi S, Orcesi S, Cereda C. Legius Syndrome: two novel mutations in the SPRED1 gene. Hum Genome Var 2015; 2:15051.: 10.1038/hgv.2015.1051. eCollection 2015. [PMC free article: PMC4785569] [PubMed: 27081556] [CrossRef]
- 171.
- D'Ettorre M, Gniuli D, Guidone C, Bracaglia R, Tambasco D, Mingrone G. Insulin sensitivity in Familial Multiple Lipomatosis. Eur Rev Med Pharmacol Sci. 2013;17:2254–2256. [PubMed: 23893194]
- 172.
- Inampudi P, Jacobson JA, Fessell DP, Carlos RC, Patel SV, Delaney-Sathy LO, van Holsbeeck MT. Soft-tissue lipomas: accuracy of sonography in diagnosis with pathologic correlation. Radiology 2004; 233:763-767. doi: 7 10.1148/radiol.2333031410. Epub 2333032004 Oct 2333031414. [PubMed: 15486212] [CrossRef]
- 173.
- Coran A, Ortolan P, Attar S, Alberioli E, Perissinotto E, Tosi AL, Montesco MC, Rossi CR, Tropea S, Rastrelli M, Stramare R. Magnetic Resonance Imaging Assessment of Lipomatous Soft-tissue Tumors. In Vivo 2017; 31:387-395. doi: 3 10.21873/invivo.11071. [PMC free article: PMC5461449] [PubMed: 28438867] [CrossRef]
- 174.
- O'Donnell PW, Griffin AM, Eward WC, Sternheim A, White LM, Wunder JS, Ferguson PC. Can Experienced Observers Differentiate between Lipoma and Well-Differentiated Liposarcoma Using Only MRI? Sarcoma. 2013;2013:6. [PMC free article: PMC3872425] [PubMed: 24385845]
- 175.
- Wolfe SW, Bansal M, Healey JH, Ghelman B. Computed tomographic evaluation of fatty neoplasms of the extremities. A clinical, radiographic, and histologic review of cases. Orthopedics. 1989;12:1351–1358. [PubMed: 2798244]
- 176.
- Cherry hemangiomas and lipomas with a peculiar distribution. Journal of the American Academy of Dermatology. 2017;76:AB68.
- 177.
- Self TH, Akins D. Dramatic reduction in lipoma associated with statin therapy. Journal of the American Academy of Dermatology. 2008;58:S30–S31. [PubMed: 18191694]
- 178.
- Al-basti HA, El-Khatib HA. The use of suction-assisted surgical extraction of moderate and large lipomas: long-term follow-up. Aesthetic Plast Surg. 2002;26:114–117. [PubMed: 12016495]
- 179.
- Gerut ZE. Abstract: The Enzymatic Dissolution of Human Fat. Plast Reconstr Surg Glob Open. 2017;5:66–67.
- 180.
- Mlosek RK, Malinowska S, Wozniak W. Lipoma removal using a high-frequency ultrasound-guided injection of a Class III CE-marked device-Empirical findings. J Cosmet Dermatol 2019; 18:469-473. doi: 4 10.1111/jocd.12681. Epub 12018 Jul 12619. [PubMed: 30027646] [CrossRef]
- 181.
- Boyer M, Monette S, Nguyen A, Zipp T, Aughenbaugh WD, Nimunkar AJ. A review of techniques and procedures for lipoma treatment. Clincial Dermatology. 2015;3:105–112.
- 182.
- Kanamori Y, Takezoe T, Takahashi M, Nakano N, Matsuoka K, Osaku M. A case of an 8-year-old boy who was strongly suspected of suffering from familial angiolipomatosis. Journal of Pediatric Surgery Case Reports. 2015;3:255–256.
- 183.
- Yeo ED, Chung BM, Kim EJ, Kim WT. Infiltrating angiolipoma of the foot: magnetic resonance imaging features and review of the literature. Skeletal Radiol 2018; 47:859-864. doi: 8 10.1007/s00256-00017-02870-00258. Epub 02018 Jan 00210. [PubMed: 29322209] [CrossRef]
- 184.
- Nissen A, Yi F. Rare cause of colonic intussusception in an adult. BMJ Case Rep 2017; 2017.:bcr-2017-221976. doi: 2219 10.221136/bcr-222017-221976. [PMC free article: PMC5604696] [PubMed: 28918406] [CrossRef]
- 185.
- Wu Z, Wan H, Shi M, Li M, Wang Z, Yang C, Gao W, Li Q. Bronchoscopic resection of bronchial angiolipoma: A rare case report. Mol Clin Oncol 2016; 5:850-852. doi: 8 10.3892/mco.2016.1069. Epub 2016 Nov 3891. [PMC free article: PMC5228196] [PubMed: 28101361] [CrossRef]
- 186.
- Ilyas G, Turgut A, Ayaz D, Kalenderer O. Intraarticular Giant Size Angiolipoma of the Knee Causing Lateral Patellar Dislocation. Balkan Med J 2016; 33:691-694. doi: 6 10.5152/balkanmedj.2016.141269. Epub 142016 Nov 141261. [PMC free article: PMC5156469] [PubMed: 27994926] [CrossRef]
- 187.
- Srivastava A, Gupta N, Joice GA, Wright EJ. Management and Excision of a 15 cm Paratesticular Angiolipoma. Urol Case Rep 2017; 15:8-10.: 10.1016/j.eucr.2017.1007.1004. eCollection 2017 Nov. [PMC free article: PMC5565739] [PubMed: 28856106] [CrossRef]
- 188.
- Naversen DN, Trask DM, Watson FH, Burket JM. Painful tumors of the skin: "LEND AN EGG. J Am Acad Dermatol. 1993;28:298–300. [PubMed: 8436643]
- 189.
- Clayman E, King K, Harrington MA. Corticosteroid-Associated Angiolipomatosis. Eplasty 2017; 17:ic9. eCollection 2017. [PMC free article: PMC5389016] [PubMed: 28458766]
- 190.
- Namba M, Kohda M, Mimura S, Nakagawa S, Ueki H. Angiolipoma in brothers. J Dermatol. 1977;4:255–257. [PubMed: 15461357]
- 191.
- Howard WR, Helwig EB. Angiolipoma. Arch Dermatol. 1960;82:924–931. [PubMed: 13716236]
- 192.
- Garib G, Siegal GP, Andea AA. Autosomal-dominant familial angiolipomatosis. Cutis. 2015;95:E26–29. [PubMed: 25671454]
- 193.
- Abbasi NR, Brownell I, Fangman W. Familial multiple angiolipomatosis. Dermatology Online Journal. 2007;13(1):3. http://dermatology
.cdlib .org/131/cases/NYUcases/101805_5 .html#9#9 Accessed 11/19/2007. [PubMed: 17511936] - 194.
- Hapnes SA, Boman H, Skeie SO. Familial angiolipomatosis. Clin Genet. 1980;17:202–208. [PubMed: 7363507]
- 195.
- Wilke J, Schleip R, Klingler W, Stecco C. The Lumbodorsal Fascia as a Potential Source of Low Back Pain: A Narrative Review. Biomed Res Int. 2017:1–6. [PMC free article: PMC5444000] [PubMed: 28584816]
- 196.
- Yoshida K, Ito H, Furuya K, Ukichi T, Noda K, Kurosaka D. Angiogenesis and VEGF-expressing cells are identified predominantly in the fascia rather than in the muscle during the early phase of dermatomyositis. Arthritis Res Ther 2017; 19:272. doi: 2 10.1186/s13075-13017-11481-z. [PMC free article: PMC5721588] [PubMed: 29216907] [CrossRef]
- 197.
- Su X, Lyu Y, Wang W, Zhang Y, Li D, Wei S, Du C, Geng B, Sztalryd C, Xu G. Fascia Origin of Adipose Cells. Stem Cells 2016; 34:1407-1419. doi: 14 10.1002/stem.2338. Epub 2016 Mar 1407. [PubMed: 26867029] [CrossRef]
- 198.
- Panagopoulos I, Gorunova L, Andersen K, Lobmaier I, Bjerkehagen B, Heim S. Consistent Involvement of Chromosome 13 in Angiolipoma. Cancer Genomics Proteomics. 2018;15:61–65. [PMC free article: PMC5822184] [PubMed: 29275363] [CrossRef]
- 199.
- Dekker I, van der Leest M, van Rijk MC, Gerritsen WR, Arens AIJ. 68Ga-PSMA Uptake in Angiolipoma. Clin Nucl Med 2018; 43:757-758. doi: 7 10.1097/RLU.0000000000002236. [PubMed: 30153142] [CrossRef]
- 200.
- Kitagawa Y, Miyamoto M, Konno S, Makino A, Maruyama G, Takai S, Higashi N. Subcutaneous angiolipoma: magnetic resonance imaging features with histological correlation. J Nippon Med Sch. 2014;81:313–319. [PubMed: 25391700]
- 201.
- Bang M, Kang BS, Hwang JC, Weon YC, Choi SH, Shin SH, Kwon WJ, Hwang CM, Lee SY. Ultrasonographic analysis of subcutaneous angiolipoma. Skeletal Radiol 2012; 41:1055-1059. doi: 10 10.1007/s00256-00011-01309-x. Epub 02011 Nov 00258. [PubMed: 22064985] [CrossRef]
- 202.
- Kaneko T, Tokushige H, Kimura N, Moriya S, Toda K. The treatment of multiple angiolipomas by liposuction surgery. J Dermatol Surg Oncol. 1994;20:690–692. [PubMed: 7930016]
- 203.
- Horiuchi K, Yamada T, Sakai K, Okawa A, Arai Y. Hemorrhagic Sudden Onset of Spinal Epidural Angiolipoma. Case Rep Orthop 2018; 2018:5231931.: 10.1155/2018/5231931. eCollection 5232018. [PMC free article: PMC6051123] [PubMed: 30057841] [CrossRef]
- 204.
- Lacour M, Gilard V, Marguet F, Curey S, Perez A, Derrey S. Sudden paraplegia due to spontaneous bleeding in a thoracic epidural angiolipoma and literature review. Neurochirurgie 2018; 64:73-75. doi: 10.1016/j.neuchi.2017.1008.1003. Epub 2018 Feb 1019. [PubMed: 29472020] [CrossRef]
- 205.
- Behrendt H, Faes J, Ruzicka T. Hautarzt. 1992;43:139–142. [Multiple angiolipomas--analgesics therapy with doxepin] [PubMed: 1374370]
- 206.
- Afrin L, Molderings G. A concise, practical guide to diagnostic assessment for mast cell activation disease. World Journal of Hematology. 2014;3:1–17. [PMC free article: PMC3069946] [PubMed: 21418662]
- 207.
- Afrin LB, Pohlau D, Raithel M, Haenisch B, Dumoulin FL, Homann J, Mauer UM, Harzer S, Molderings GJ. Mast cell activation disease: An underappreciated cause of neurologic and psychiatric symptoms and diseases. Brain Behav Immun 2015; 50:314-21.: 10.1016/j.bbi.2015.1007.1002. Epub 2015 Jul 1018. [PubMed: 26162709] [CrossRef]
- 208.
- Molderings GJ, Afrin LB, Hertfelder HJ, Brettner S. Case Report: Treatment of systemic mastocytosis with sunitinib. 1000Res 2017; 6:2182.: 10.12688/f11000research.13343.12681. eCollection 12017. [PMC free article: PMC5946163] [PubMed: 29770197] [CrossRef]
- 209.
- Afrin LB, Fox RW, Zito SL, Choe L, Glover SC. Successful targeted treatment of mast cell activation syndrome with tofacitinib. Eur J Haematol 2017; 99:190-193. doi: 1 10.1111/ejh.12893. Epub 12017 May 12893. [PubMed: 28382662] [CrossRef]
- 210.
- Malik F, Ali N, Jafri SIM, Ghani A, Hamid M, Boigon M, Fidler C. Continuous diphenhydramine infusion and imatinib for KIT-D816V-negative mast cell activation syndrome: a case report. J Med Case Rep 2017; 11:119. doi: 1 10.1186/s13256-13017-11278-13253. [PMC free article: PMC5402659] [PubMed: 28438191] [CrossRef]
- 211.
- Molderings GJ, Haenisch B, Brettner S, Homann J, Menzen M, Dumoulin FL, Panse J, Butterfield J, Afrin LB. Pharmacological treatment options for mast cell activation disease. Naunyn Schmiedebergs Arch Pharmacol 2016; 389:671-694. doi: 6 10.1007/s00210-00016-01247-00211. Epub 02016 Apr 00230. [PMC free article: PMC4903110] [PubMed: 27132234] [CrossRef]
- 212.
- Baldo BA, Pham NH. Histamine-releasing and allergenic properties of opioid analgesic drugs: resolving the two. Anaesth Intensive Care 2012; 40:216-235. doi: 2 10.1177/0310057X1204000204. [PubMed: 22417016] [CrossRef]
- 213.
- Naviaux RK. Metabolic features and regulation of the healing cycle-A new model for chronic disease pathogenesis and treatment. Mitochondrion. 2018;9:30105–30103. [PubMed: 30099222]
- 214.
- Hansson E, Svensson H, Brorson H. Review of Dercum's disease and proposal of diagnostic criteria, diagnostic methods, classification and management. Orphanet J Rare Dis. 2012;7:23. [PMC free article: PMC3444313] [PubMed: 22546240] [CrossRef]
- 215.
- Giudiceandrea V. L’adiposis dolorosa (malattia di Dercum). Riv Patol Nerv Ment. 1900;V:289–304.
- 216.
- Roux J, Vitaut M. Maladie de Dercum (Adiposis dolorosa). Revue Neurol (Paris). 1901;9:881–888.
- 217.
- Anders JM. Adiposis tuberosa simplex. The American Journal of the Medical Sciences (1827-1924) 1908; 135:325-333.
- 218.
- Hao D, Olugbodi A, Udechukwu N, Donato AA. Trauma-induced adiposis dolorosa (Dercum's disease). BMJ Case Rep 2018; 2018.:bcr-2017-223869. doi: 2238 10.221136/bcr-222017-223869. [PMC free article: PMC5878302] [PubMed: 29592996] [CrossRef]
- 219.
- Herbst KL, Asare-Bediako S. Adiposis Dolorosa is More than Painful Fat. The Endocrinologist. 2007;17:326–344.
- 220.
- Stormorken H, Brosstad F, H. S. The fibromyalgia syndrome: A member of the painful lipo[mato]sis family? In: Pederson JA, ed. New Research on Fibromyalgia. New York: Nova Science Publishers, Inc.; 2006.
- 221.
- Dercum FX. A subcutaneous connective-tissue dystrophy of the arms and back, associated with symptoms resembling myxoedema. University Medical Magazine Philadelphia. Vol 11888:140-150.
- 222.
- Rasmussen JC, Herbst KL, Aldrich MB, Darne CD, Tan IC, Zhu B, Guilliod R, Fife CE, Maus EA, Sevick-Muraca EM. An abnormal lymphatic phenotype is associated with subcutaneous adipose tissue deposits in Dercum's disease. Obesity. 2014;9:20836. [PMC free article: PMC4180796] [PubMed: 25044620]
- 223.
- Fagher B, Monti M, Nilsson-Ehle P, Akesson B. Fat-cell heat production, adipose tissue fatty acids, lipoprotein lipase activity and plasma lipoproteins in adiposis dolorosa. Clin Sci (Lond). 1991;81:793–798. [PubMed: 1662586]
- 224.
- Bordoni B, Marelli F, Morabito B, Cavallaro F, Lintonbon D. Fascial preadipocytes: another missing piece of the puzzle to understand fibromyalgia? Open Access Rheumatol 2018; 10:27-32.: 10.2147/OARRR.S155919. eCollection 152018. [PMC free article: PMC5935082] [PubMed: 29750060] [CrossRef]
- 225.
- Hansson E, Manjer J, Svensson H, Aberg M, Fagher B, Ekman R, Brorson H. Neuropeptide levels in Dercum's disease (adiposis dolorosa). Reumatismo 2012; 64:134-141. doi: 1 10.4081/reumatismo.2012.4134. [PubMed: 22842296] [CrossRef]
- 226.
- Herbst KL, Coviello AD, Chang A, Boyle DL. Lipomatosis-associated inflammation and excess collagen may contribute to lower relative resting energy expenditure in women with adiposis dolorosa. Int J Obes (Lond) 2009; 33:1031-1038. Epub 2009 Jul 1021. [PMC free article: PMC3964847] [PubMed: 19621017]
- 227.
- Weinberger A Fau - Wysenbeec AJ, Wysenbeec Aj Fau - Pinkhas J, Pinkhas J. Juxta-articular adiposis dolorosa associated with rheumatoid arthritis. Report of 2 cases with good response to local corticosteroid injection. [PubMed: 3442969]
- 228.
- Baudart P, Cesini J, Marcelli C. Atypical juxta-articular form of Dercum's disease in a patient treated with tocilizumab for rheumatoid arthritis. Joint Bone Spine. 2017;2:30202–30206. [PubMed: 29198885]
- 229.
- Tins BJ, Matthews C, Haddaway M, Cassar-Pullicino VN, Lalam R, Singh J, Tyrrell PN. Adiposis dolorosa (Dercum's disease): MRI and ultrasound appearances. Clin Radiol. 2013;25:00199–00192. [PubMed: 23809264]
- 230.
- Petscavage-Thomas JM, Walker EA, Bernard SA, Bennett J. Imaging findings of adiposis dolorosa vs. massive localized lymphedema. Skeletal Radiol. 2015;13:13. [PubMed: 25672948]
- 231.
- Semelka RC, Ramalho J, Vakharia A, AlObaidy M, Burke LM, Jay M, Ramalho M. Gadolinium deposition disease: Initial description of a disease that has been around for a while. Magn Reson Imaging 2016; 34:1383-1390. doi: 13 10.1016/j.mri.2016.1307.1016. Epub 2016 Aug 1313. [PubMed: 27530966] [CrossRef]
- 232.
- Semelka RM. The Odd Fellow Collection of Modern Diseases: Fibromyalgia, Dercum's Disease, Multiple Chemical Sensitivity, Gadolinium Deposition Disease. RICHARD SEMELKA, MD. CONSULTING. Vol 2019. https://www
.richardsemelka .com/single-post /2019/02/13/The-Odd-Fellow-Collection-of-Modern-Diseases-Fibromyalgia-Dercums-Disease-Multiple-Chemical-Sensitivity-Gadolinium-Deposition-Disease2019. - 233.
- Skagen K, Petersen P, Kastrup J, Norgaard T. The regulation of subcutaneous blood flow in patient with Dercum's disease. Acta Derm Venereol. 1986;66:337–339. [PubMed: 2430406]
- 234.
- Cantone M, Lanza G, Pennisi M, Bella R, Schepis C, Siragusa M, Barone R, Ferri R. Prominent neurological involvement in Dercum disease. J Neurol 2017; 264:796-798. doi: 7 10.1007/s00415-00017-08415-00411. Epub 02017 Feb 00413. [PubMed: 28194532] [CrossRef]
- 235.
- Miraglia E, Visconti B, Bianchini D, Calvieri S, Giustini S. An uncommon association between lipomatous hypertrophy of the interatrial septum (LHIS) and Dercum's disease. Eur J Dermatol. 2013;19:19. [PubMed: 23782949]
- 236.
- Laura DM, Donnino R, Kim EE, Benenstein R, Freedberg RS, Saric M. Lipomatous Atrial Septal Hypertrophy: A Review of Its Anatomy, Pathophysiology, Multimodality Imaging, and Relevance to Percutaneous Interventions. J Am Soc Echocardiogr 2016; 29:717-723. doi: 7 10.1016/j.echo.2016.1004.1014. Epub 2016 Jun 1017. [PubMed: 27288088] [CrossRef]
- 237.
- Kyllerman M, Brandberg G, Wiklund LM, Mansson JE. Dysarthria, progressive parkinsonian features and symmetric necrosis of putamen in a family with painful lipomas (Dercum disease variant). Neuropediatrics. 2002;33:69–72. [PubMed: 12075486] [CrossRef]
- 238.
- Wipf A, Lofgreen S, Miller DD, Farah RS. Novel Use of Deoxycholic Acid for Adiposis Dolorosa (Dercum Disease). Dermatol Surg. 2019;14:0000000000001800. [PubMed: 30789509]
- 239.
- Atkinson RL. Intravenous lidocaine for the treatment of intractable pain of adiposis dolorosa. Int J Obes. 1982;6:351–357. [PubMed: 7129748]
- 240.
- Desai MJ, Siriki R, Wang D. Treatment of pain in Dercum's disease with Lidoderm (lidocaine 5% patch): a case report. Pain Med 2008; 9:1224-1226. Epub 2008 Mar 1211. [PubMed: 18346067]
- 241.
- Reggiani M, Errani A, Staffa M, Schianchi S. Is EMLA effective in Dercum's disease? Acta Derm Venereol. 1996;76:170–171. [PubMed: 8740288]
- 242.
- Labuzek K, Liber S, Suchy D, Okopiea BA. A successful case of pain management using metformin in a patient with adiposis dolorosa. Int J Clin Pharmacol Ther 2013; 51:517-524. doi: 5 10.5414/CP201878. [PubMed: 23611575] [CrossRef]
- 243.
- Tiesmeier J, Warnecke H, Schuppert F. Dtsch Med Wochenschr. 2006;131:434–437. [An uncommon cause of recurrent abdominal pain in a 63-year-old obese woman] [PubMed: 16493566]
- 244.
- Parkitny L, Younger J. Reduced Pro-Inflammatory Cytokines after Eight Weeks of Low-Dose Naltrexone for Fibromyalgia. Biomedicines 2017; 5(2).biomedicines5020016. doi: 50200 10.5023390/biomedicines5020016. [PMC free article: PMC5489802] [PubMed: 28536359] [CrossRef]
- 245.
- Lange U, Oelzner P, Uhlemann C. Dercum's disease (Lipomatosis dolorosa): successful therapy with pregabalin and manual lymphatic drainage and a current overview. Rheumatol Int. 2005;2008(29):17–22. Epub 2008 Jul. [PubMed: 18604537]
- 246.
- Landheer JA, Toonstra J. Dercum's disease: Successful treatment with gabapentin. Nederlands Tijdschrift voor Dermatologie en Venereologie 2009; 19(5):265-267:265-267.
- 247.
- Wollina U, Goldman A, Heinig B. Microcannular tumescent liposuction in advanced lipedema and Dercum's disease. G Ital Dermatol Venereol. 2010;145:151–159. [PubMed: 20467389]
- 248.
- Hansson E, Svensson H, Brorson H. Liposuction may reduce pain in Dercum's disease (adiposis dolorosa). Pain Med 2011; 12:942-952. doi: 9 10.1111/j.1526-4637.2011.01101.x. Epub 02011 Apr 01111. [PubMed: 21481169] [CrossRef]
- 249.
- Berntorp E, Berntorp K, Brorson H, Frick K. Liposuction in Dercum's disease: impact on haemostatic factors associated with cardiovascular disease and insulin sensitivity. J Intern Med. 1998;243:197–201. [PubMed: 9627156]
- 250.
- Martinenghi S, Caretto A, Losio C, Scavini M, Bosi E. Successful Treatment of Dercum's Disease by Transcutaneous Electrical Stimulation: A Case Report. Medicine (Baltimore) 2015; 94:e950. doi: 9 10.1097/MD.0000000000000950. [PMC free article: PMC4616524] [PubMed: 26091459] [CrossRef]
- 251.
- Herbst KL, Rutledge T. Pilot study: rapidly cycling hypobaric pressure improves pain after 5 days in adiposis dolorosa. Journal of Pain Research. 2010;3:147–153. [PMC free article: PMC3004643] [PubMed: 21197318]
- 252.
- El Ouahabi H, Doubi S, Lahlou K, Boujraf S, Ajdi F. Launois-bensaude syndrome: A benign symmetric lipomatosis without alcohol association. Ann Afr Med. 2017;16:33–34. [PMC free article: PMC5452705] [PubMed: 28300050] [CrossRef]
- 253.
- Kratz C, Lenard HG, Ruzicka T, Gartner J. Multiple symmetric lipomatosis: an unusual cause of childhood obesity and mental retardation. Eur J Paediatr Neurol. 2000;4:63–67. [PubMed: 10817486]
- 254.
- Enzi G, Busetto L, Ceschin E, Coin A, Digito M, Pigozzo S. Multiple symmetric lipomatosis: clinical aspects and outcome in a long-term longitudinal study. Int J Obes Relat Metab Disord. 2002;26:253–261. [PubMed: 11850759]
- 255.
- Donhauser G, Vieluf D, Ruzicka T, Braun-Falco O. Hautarzt. 1991;42:311–314. [Benign symmetric Launois-Bensaude type III lipomatosis and Bureau-Barriere syndrome] [PubMed: 1874620]
- 256.
- Ettl T, Gaumann A, Ehrenberg R, Reichert TE, Driemel O. Encapsulated lipomas of the tongue in benign symmetric lipomatosis. J Dtsch Dermatol Ges. 2019;2009(7):441–444. Epub 2009 Jan. [PubMed: 19192164]
- 257.
- Lopez-Ceres A, Aguilar-Lizarralde Y, Villalobos Sanchez A, Prieto Sanchez E, Valiente Alvarez A. Benign symmetric lipomatosis of the tongue in Madelung's disease. J Craniomaxillofac Surg. 2008;2006(34):489–493. Epub 2006 Dec. [PubMed: 17157517]
- 258.
- Birnholz JC, Macmillan AS Jr. Advanced laryngeal compression due to diffuse, symmetric lipomatosis (Madelung's disease). Br J Radiol. 1973;46:245–249. [PubMed: 4720736]
- 259.
- Laure B, Sury F, Tayeb T, Corre P, Goga D. Launois-Bensaude syndrome involving the orbits. J 39:21-23. Epub 2010 Aug 2014. [PubMed: 20709560]
- 260.
- Enzi G. Multiple symmetric lipomatosis: an updated clinical report. Medicine (Baltimore). 1984;63:56–64. [PubMed: 6318013]
- 261.
- Enzi G, Biondetti PR, Fiore D, Mazzoleni F. Computed tomography of deep fat masses in multiple symmetrical lipomatosis. Radiology. 1982;144:121–124. [PubMed: 7089242]
- 262.
- Klopstock T, Naumann M, Schalke B, Bischof F, Seibel P, Kottlors M, Eckert P, Reiners K, Toyka KV, Reichmann H. Multiple symmetric lipomatosis: abnormalities in complex IV and multiple deletions in mitochondrial DNA. Neurology. 1994;44:862–866. [PubMed: 8190288]
- 263.
- Berkovic SF, Andermann F, Shoubridge EA, Carpenter S, Robitaille Y, Andermann E, Melmed C, Karpati G. Mitochondrial dysfunction in multiple symmetrical lipomatosis. Ann Neurol. 1991;29:566–569. [PubMed: 1650162]
- 264.
- Klopstock T, Naumann M, Seibel P, Shalke B, Reiners K, Reichmann H. Mitochondrial DNA mutations in multiple symmetric lipomatosis. Molecular and Cellular Biochemistry. 1997;174:271–275. [PubMed: 9309699]
- 265.
- Chalk CH, Mills KR, Jacobs JM, Donaghy M. Familial multiple symmetric lipomatosis with peripheral neuropathy. Neurology. 1990;40:1246–1250. [PubMed: 2166247]
- 266.
- Musumeci O, Barca E, Lamperti C, Servidei S, Comi GP, Moggio M, Mongini T, Siciliano G, Filosto M, Pegoraro E, Primiano G, Ronchi D, Vercelli L, Orsucci D, Bello L, Zeviani M, Mancuso M, Toscano A. Lipomatosis Incidence and Characteristics in an Italian Cohort of Mitochondrial Patients. Front Neurol 2019; 10:160.: 10.3389/fneur.2019.00160. eCollection 02019. [PMC free article: PMC6402385] [PubMed: 30873109] [CrossRef]
- 267.
- Zolotov S, Xing C, Mahamid R, Shalata A, Sheikh-Ahmad M, Garg A. Homozygous LIPE mutation in siblings with multiple symmetric lipomatosis, partial lipodystrophy, and myopathy. Am J Med Genet A 2017; 173:190-194. doi: 1 10.1002/ajmg.a.37880. Epub 32016 Nov 37811. [PMC free article: PMC5788284] [PubMed: 27862896] [CrossRef]
- 268.
- Sawyer SL, Cheuk-Him Ng A, Innes AM, Wagner JD, Dyment DA, Tetreault M, Majewski J, Boycott KM, Screaton RA, Nicholson G. Homozygous mutations in MFN2 cause multiple symmetric lipomatosis associated with neuropathy. Hum Mol Genet 2015; 24:5109-5114. doi: 51 10.1093/hmg/ddv5229. Epub 2015 Jun 5117. [PubMed: 26085578] [CrossRef]
- 269.
- Kodish ME, Alsever RN, Block MB. Benign symmetric lipomatosis: functional sympathetic denervation of adipose tissue and possible hypertrophy of brown fat. Metabolism. 1974;23:937–945. [PubMed: 4412181]
- 270.
- Busetto L, Strater D, Enzi G, Coin A, Sergi G, Inelmen EM, Pigozzo S. Differential clinical expression of multiple symmetric lipomatosis in men and women. Int J Obes Relat Metab Disord. 2003;27:1419–1422. [PubMed: 14574355]
- 271.
- Carr A, Miller J, Law M, Cooper DA. A syndrome of lipoatrophy, lactic acidaemia and liver dysfunction associated with HIV nucleoside analogue therapy: contribution to protease inhibitor-related lipodystrophy syndrome. Aids. 2000;14:F25–32. [PubMed: 10716495]
- 272.
- Engelson ES. HIV lipodystrophy diagnosis and management. Body composition and metabolic alterations: diagnosis and management. AIDS Read. 2003;13:S10–14. [PubMed: 12762288]
- 273.
- Lo JC, Mulligan K, Tai VW, Algren H, Schambelan M. "Buffalo hump" in men with HIV-1 infection. Lancet. 1998;351:867–870. [PubMed: 9525364]
- 274.
- Heath KV, Hogg RS, Chan KJ, Harris M, Montessori V, O'Shaughnessy MV, Montanera JS. Lipodystrophy-associated morphological, cholesterol and triglyceride abnormalities in a population-based HIV/AIDS treatment database. Aids. 2001;15:231–239. [PubMed: 11216932]
- 275.
- Urso R, Gentile M. Are 'buffalo hump' syndrome, Madelung's disease and multiple symmetrical lipomatosis variants of the same dysmetabolism? Aids. 2001;15:290–291. [PubMed: 11216947]
- 276.
- Lindner A, Marbach F, Tschernitz S, Ortner C, Berneburg M, Felthaus O, Prantl L, Kye MJ, Rappl G, Altmüller J, Thiele H, Schreml S, Schreml J. Calcyphosine-like (CAPSL) is regulated in Multiple Symmetric Lipomatosis and is involved in Adipogenesis. Scientific Reports. 2019;9:8444. [PMC free article: PMC6559987] [PubMed: 31186450]
- 277.
- Zancanaro C, Sbarbati A, Morroni M, Carraro R, Cigolini M, Enzi G, Cinti S. Multiple symmetric lipomatosis. Ultrastructural investigation of the tissue and preadipocytes in primary culture. Lab Invest. 1990;63:253–258. [PubMed: 2381166]
- 278.
- Cinti S, Enzi G, Cigolini M, Bosello O. Ultrastructural features of cultured mature adipocyte precursors from adipose tissue in multiple symmetric lipomatosis. Ultrastruct Pathol. 1983;5:145–152. [PubMed: 6670139]
- 279.
- Chen K, He H, Xie Y, Zhao L, Zhao S, Wan X, Yang W, Mo Z. miR-125a-3p and miR-483-5p promote adipogenesis via suppressing the RhoA/ROCK1/ERK1/2 pathway in multiple symmetric lipomatosis. Sci Rep. 2015;5:11909. [PMC free article: PMC4493643] [PubMed: 26148871] [CrossRef]
- 280.
- Prantl L, Schreml J, Gehmert S, Klein S, Bai X, Zeitler K, Schreml S, Alt E, Gehmert S, Felthaus O. Transcription Profile in Sporadic Multiple Symmetric Lipomatosis Reveals Differential Expression at the Level of Adipose Tissue-Derived Stem Cells. Plast Reconstr Surg 2016; 137:1181-1190. doi: 11 10.1097/PRS.0000000000002013. [PubMed: 27018673] [CrossRef]
- 281.
- Moonen MPB, Nascimento EBM, van Kroonenburgh M, Brandjes D, van Marken Lichtenbelt WD. Absence of (18) F-fluorodeoxyglucose uptake using Positron Emission Tomography/Computed Tomography in Madelung's disease: A case report. Clin Obes 2019; 9:e12302. doi: 123 10.11111/cob.12302. Epub 12019 Feb 12327. [PMC free article: PMC6593737] [PubMed: 30815996] [CrossRef]
- 282.
- Sebastian BM, Roychowdhury S, Tang H, Hillian AD, Feldstein AE, Stahl GL, Takahashi K, Nagy LE. Identification of a cytochrome P4502E1/Bid/C1q-dependent axis mediating inflammation in adipose tissue after chronic ethanol feeding to mice. J Biol Chem 2011; 286:35989-35997. doi: 359 10.31074/jbc.M35111.254201. Epub 252011 Aug 254219. [PMC free article: PMC3195631] [PubMed: 21856753] [CrossRef]
- 283.
- Dumont AE, Mulholland JH. Flow rate and composition of thoracic-duct lymph in patients with cirrhosis. N Engl J Med. 1960;263:471–4. [PubMed: 13818600] [CrossRef]
- 284.
- Ludwig J, Linhart P, Baggenstoss AH. Hepatic lymph drainage in cirrhosis and congestive heart failure. A postmortem lymphangiographic study. Arch Pathol. 1968;86:551–562. [PubMed: 5681441]
- 285.
- Souza-Smith FM, Siggins RW, Molina PE. Mesenteric Lymphatic-Perilymphatic Adipose Crosstalk: Role in Alcohol-Induced Perilymphatic Adipose Tissue Inflammation. Alcohol Clin Exp Res 2015; 39:1380-1387. doi: 13 10.1111/acer.12796. Epub 12015 Jul 12794. [PMC free article: PMC5102000] [PubMed: 26147204] [CrossRef]
- 286.
- Szewc M, Sitarz R, Moroz N, Maciejewski R, Wierzbicki R. Madelung's disease - progressive, excessive, and symmetrical deposition of adipose tissue in the subcutaneous layer: case report and literature review. Diabetes Metab Syndr Obes 2018; 11:819-825.: 10.2147/DMSO.S181154. eCollection 182018. [PMC free article: PMC6263218] [PubMed: 30538518] [CrossRef]
- 287.
- Chen CY, Fang QQ, Wang XF, Zhang MX, Zhao WY, Shi BH, Wu LH, Zhang LY, Tan WQ. Madelung's Disease: Lipectomy or Liposuction? Biomed Res Int 2018; 2018:3975974.: 10.1155/2018/3975974. eCollection 3972018. [PMC free article: PMC5840946] [PubMed: 29682541] [CrossRef]
- 288.
- Constantinidis J, Steinhart H, Zenk J, Gassner H, Iro H. Combined surgical lipectomy and liposuction in the treatment of benign symmetrical lipomatosis of the head and neck. Scand J Plast Reconstr Surg Hand Surg. 2003;37:90–96. [PubMed: 12755508]
- 289.
- Andou E, Komoto M, Hasegawa T, Mizuno H, Hayashi A. Surgical excision of madelung disease using bilateral cervical lymphnode dissection technique-its effect and the influence of previous injection lipolysis. Plast Reconstr Surg Glob Open 2015; 3:e375. doi: 3 10.1097/GOX.0000000000000337. eCollection 0000000000002015 Apr. [PMC free article: PMC4422206] [PubMed: 25973353] [CrossRef]
- Review Lipomatoses.[Ann Endocrinol (Paris). 2024]Review Lipomatoses.Dupuis H, Lemaitre M, Jannin A, Douillard C, Espiard S, Vantyghem MC. Ann Endocrinol (Paris). 2024 Jun; 85(3):231-247. Epub 2024 Jun 12.
- Review Genetic syndromes with localized subcutaneous fat tissue accumulation.[Acta Biomed. 2019]Review Genetic syndromes with localized subcutaneous fat tissue accumulation.Precone V, Barati S, Paolacci S, Salgarello M, Visconti G, Gentileschi S, Guerri G, Gagliardi L, Aquilanti B, Matera G, et al. Acta Biomed. 2019 Sep 30; 90(10-S):90-92. Epub 2019 Sep 30.
- Review Rare adipose disorders (RADs) masquerading as obesity.[Acta Pharmacol Sin. 2012]Review Rare adipose disorders (RADs) masquerading as obesity.Herbst KL. Acta Pharmacol Sin. 2012 Feb; 33(2):155-72.
- Review Lipedema: Insights into Morphology, Pathophysiology, and Challenges.[Biomedicines. 2022]Review Lipedema: Insights into Morphology, Pathophysiology, and Challenges.Poojari A, Dev K, Rabiee A. Biomedicines. 2022 Nov 30; 10(12). Epub 2022 Nov 30.
- Subcutaneous adipose tissue therapy reduces fat by dual X-ray absorptiometry scan and improves tissue structure by ultrasound in women with lipoedema and Dercum disease.[Clin Obes. 2018]Subcutaneous adipose tissue therapy reduces fat by dual X-ray absorptiometry scan and improves tissue structure by ultrasound in women with lipoedema and Dercum disease.Ibarra M, Eekema A, Ussery C, Neuhardt D, Garby K, Herbst KL. Clin Obes. 2018 Dec; 8(6):398-406. Epub 2018 Sep 24.
- Subcutaneous Adipose Tissue Diseases: Dercum Disease, Lipedema, Familial Multipl...Subcutaneous Adipose Tissue Diseases: Dercum Disease, Lipedema, Familial Multiple Lipomatosis, and Madelung Disease - Endotext
Your browsing activity is empty.
Activity recording is turned off.
See more...
