OVERVIEW
Introduction
Ivermectin is an antiinfective agent with activity against several parasitic nematodes and scabies and is the treatment of choice for onchocerciasis (river blindness). It is typically given as one or two oral doses. Ivermectin therapy has been associated with minor, self-limiting serum aminotransferase elevations and very rare instances of clinically apparent liver injury.
Background
Ivermectin (eye" ver mek" tin) is a macrocyclic lactone and semisynthetic derivative of avermectin which is produced by Streptomyces avermitilis. Ivermectin has potent activity against several parasites and arthropods. It believed to act by interference with a glutamate gated chloride channel, which interferes with the parasite's neural and neuromuscular transmission. It has a broad spectrum of activity against several nematodes (Ascaris, Trichuris, Ancylostoma), cestodes (Taenia) and trematodes (Fasciola, Schistosoma). Ivermectin has particularly potent activity against onchocerciasis (river blindness) and lymphatic filariasis, which are important endemic diseases in Africa and South America. Ivermectin was approved for use in the United States in 1996 for strongyloidiasis and onchocerciasis. In other countries it is also approved for use in scabies, lice infestation and ascariasis. Ivermectin is available in tablets of 3 mg under the brand name Stromectol. For treatment of strongyloidiasis, the recommended dose for adults is a single oral dose of 15 mg (200 μg/kg). Ivermectin is also available in topical forms for therapy of rosacea and head lice. Oral ivermectin is generally well tolerated, but side effects can include diarrhea, gastrointestinal upset, headaches, fever, rash and itching, most of which are due to the effect of ivermectin on the helminth and a reaction to their death, release and expulsion.
In cell culture systems, ivermectin has activity against several viruses including the novel coronavirus known as Severe Acute Respiratory Syndrome coronavirus-type 2 (SARS-CoV-2), the cause of the global pandemic of respiratory illness that was first recognized in late 2019 (COVID-19). In face of the growing burden of severe illness posed by COVID-19, drugs with antiviral activity against SARS-CoV-2 in vitro were often tried (repurposed) to ameliorate the course and prevent mortality. Ivermectin was evaluated in several open label trials with suggestive evidence of benefit, but in more carefully designed, larger trials ivermectin in doses of 20 to 14 mg daily for 3 to 5 days had little or no effect in either preventing infection or ameliorating its outcome.
Hepatotoxicity
Single dose therapy with ivermectin has been associated with a low rate of serum aminotransferase elevations. A single case of clinically apparent liver injury has been reported after ivermectin use (Case 1). The onset of injury occurred 1 month after a single dose and was characterized by a hepatocellular pattern of serum enzyme elevations without jaundice. Recovery was rapid and complete. In trials of ivermectin to prevent SARS-CoV-2 infection and to ameliorate the course of early as well as severe COVID-19, serum aminotransferase elevations were not uncommon but were no more frequent among patients receiving ivermectin than among those receiving placebo or a comparator drug.
Likelihood score: D (possible rare cause of mild clinically apparent liver injury).
Mechanism of Injury
Ivermectin acts by interference with chloride channels that are important in neuromuscular activity in parasitic worms and protozoa, but has little activity against mammalian neural transmission. The mechanism by which it might cause liver injury is unknown.
Outcome and Management
Ivermectin is usually well tolerated and the liver injury reported with its use has been mild and self-limited in course. Ivermectin has not been associated with acute liver failure or chronic liver injury.
Drug Class: Anthelmintic Agents
CASE REPORT
Case 1. Acute liver injury due to ivermectin.(1)
A 20 year old woman from the Cameroon who had been living in Switzerland for 5 years was found to have a migrating worm in her right sclera which was removed and identified as Loa loa. She had eosinophilia (18.5%) and microfilaremia and was treated with albendazole (600 mg daily) for 21 days. She subsequently had reduced but continued low levels of microfilia in the blood and three months later was treated with a single dose of ivermectin (15 mg orally). One month later, when seen for routine follow up, she complained of abdominal pain, and serum aminotransferase levels, which had been normal, were markedly elevated (Table). Serum bilirubin and alkaline phosphatase levels were normal. She had no history of liver disease or known risk factors for viral hepatitis other than country of origin. She did not drink alcohol and was not taking other medications, over-the-counter products or herbals. Tests for hepatitis A, B, and C and Epstein Barr virus infection were negative. A liver biopsy showed acute hepatocellular necrosis, apoptotic bodies, lymphocytic lobular infiltrates and no fibrosis. She improved clinically within days and serum aminotransferase levels fell rapidly, becoming normal three months later. Because of continuing low levels of microfilaremia, she was treated with diethylcarbamazine for 29 days with subsequent loss of microfilariae and no further problems or serum enzyme elevations.
Key Points
Laboratory Values
Comment
Without routine monitoring this mild case of anicteric hepatitis might have gone unrecognized. Because most studies of anthelmintic therapies have been done without routine monitoring of liver tests, the true rate of liver injury and even clinically apparent liver disease due to these agents may be underappreciated. On the other hand, this episode of acute hepatitis may have been due to an unrelated incurrent illness (hepatitis E for instance). Because the reaction occurred after a single dose of ivermectin, however, rechallenge would not be appropriate.
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Ivermectin – Generic, Stromectol®
DRUG CLASS
Anthelmintic Agents
Product labeling at DailyMed, National Library of Medicine, NIH
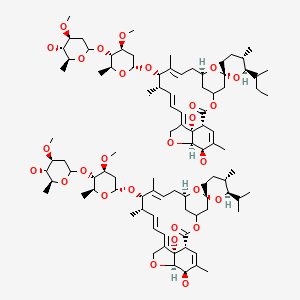
CHEMICAL FORMULA AND STRUCTURE
CITED REFERENCE
- 1.
- Veit O, Beck B, Steuerwald M, Hatz C. First case of ivermectin-induced severe hepatitis. Trans R Soc Trop Med Hyg. 2006;100:795–7. [PubMed: 16682062]
ANNOTATED BIBLIOGRAPHY
References updated: 09 April 2021
- Zimmerman HJ. Antihelminthics. Hepatic injury from antimicrobial agents. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 626-8.(Expert review of hepatotoxicity of anthelmintics written in 1999; ivermectin is not discussed).
- McCarthy J, Loukas A, Hotez PJ. Chemotherapy of helminth infections. In, Brunton LL, Chabner KA, Knollman KC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 12th ed. Amsterdam: Elsevier, 2011, pp.1443-61.(Textbook of pharmacology and therapeutics; ivermectin is a semisynthetic avermectin, a novel class of macrocyclic lactones with activity against nematodes and arthropods and commonly used in veterinary medicine).
- Shikiya K, Zaha O, Niimura S, Uehara T, Ohshiro J, Kinjo F, Saito A, et al. Kansenshogaku Zasshi. 1994;68:13–20. [Clinical study on ivermectin against 125 strongyloidiasis patients] Japanese. [PubMed: 8138669](Abstract only: among 125 patients with strongyloidiasis treated with ivermectin [6 mg, 2 oral doses 2 weeks apart], 14% had serum enzyme elevations, but all were self-limiting and asymptomatic).
- Gardon J, Gardon-Wendel N. Cemanga-Ngangue, Kamgno J, Chippaux JP, Boussinesq M. Serious reactions after mass treatment of onchocerciasis with ivermectin in an area endemic for Loa loa infection. Lancet. 1997;350:18–22. [PubMed: 9217715](In a mass treatment program for onchocerciasis, 0.1% of 17,877 people treated developed severe reactions including neurological impairment and one death; reactions correlated with high pretreatment L. loa microfilaremia counts; no mention of jaundice or hepatitis).
- Dunyo SK, Nkrumah FK, Simonsen PE. A randomized double-blind placebo-controlled field trial of ivermectin and albendazole alone and in combination for the treatment of lymphatic filariasis in Ghana. Trans R Soc Trop Med Hyg. 2000;94:205–11. [PubMed: 10897370](Placebo controlled trial of ivermectin, albendazole or the combination in 1425 persons from filariasis-endemic villages; showed clear reduction in microfilarial levels with ivermectin alone or in combination; side effects were mild and self-limited, no mention of liver injury).
- Zaha O, Hirata T, Kinjo F, Saito A, Fukuhara H. Efficacy of ivermectin for chronic strongyloidiasis: two single doses given 2 weeks apart. J Infect Chemother. 2002;8:94–8. [PubMed: 11957127](50 patients with strongyloides infection were treated with two single doses of ivermectin; 98% efficacy and mild side effects only, 1 patient had minimal, transient ALT elevation [40 U/L]).
- Guzzo CA, Furtek CI, Porras AG, Chen C, Tipping R, Clineschmidt CM, Sciberras DG, et al. Safety, tolerability, and pharmacokinetics of escalating high doses of ivermectin in healthy adult subjects. J Clin Pharmacol. 2002;42:1122–33. [PubMed: 12362927](Multiple, escalating dose [30-120 mg] study of ivermectin; side effects were mild, transient and no more common than with placebo; 2% of 51 ivermectin- vs 6% of 17 placebo-recipients had transient ALT elevations [2-2.5 times ULN]).
- Veit O, Beck B, Steuerwald M, Hatz C. First case of ivermectin-induced severe hepatitis. Trans R Soc Trop Med Hyg. 2006;100:795–7. [PubMed: 16682062](20 year old Cameroon woman with L. Loa infection developed symptoms and serum aminotransferase elevations 1 month after single dose of ivermectin [bilirubin 1.3 mg/dL, AL 907 U/L, Alk P 61 U/L], resolving in next 3 months: Case 1).
- Sparsa A, Bonnetblanc JM, Peyrot I, Loustaud-Ratti V, Vidal E, Bédane C. Ann Dermatol Venereol. 2006;133:784–7. [Systemic adverse reactions with ivermectin treatment of scabies] French. [PubMed: 17072195](72 year old man developed nausea and abdominal pain 3 days after single dose of ivermectin for scabies with ALT 2.5 times ULN, with resolution in 2 weeks; no mention of bilirubin).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease collected in the US between 2003 and 2008, none were attributed to an anthelmintic agent).
- Devarbhavi H, Dierkhising R, Kremers WK, Sandeep MS, Karanth D, Adarsh CK. Single-center experience with drug-induced liver injury from India: causes, outcome, prognosis, and predictors of mortality. Am J Gastroenterol. 2010;105:2396–404. [PubMed: 20648003](313 cases of drug induced liver injury were seen over a 12 year period at a large hospital in Bangalore, India; none were attributed to anthelmintic agents]).
- Ferrajolo C, Capuano A, Verhamme KM, Schuemie M, Rossi F, Stricker BH, Sturkenboom MC. Drug-induced hepatic injury in children: a case/non-case study of suspected adverse drug reactions in VigiBase. Br J Clin Pharmacol. 2010;70:721–8. [PMC free article: PMC2997312] [PubMed: 21039766](Worldwide pharmacovigilance database contained 9036 hepatic adverse drug reactions in children, none of which were attributed to an anthelmintic agent).
- Drugs for parasitic infections. Treat Guidel Med Lett. 2013;11 Suppl:e1–31.(Brief description of drugs for parasitic infections in adults and children as well as a table of their major side effects; ivermectin is useful in treatment of ascariasis, cutaneous larva migrans, filariasis, lice infestation, strongyloidiasis, and trichuriasis).
- Muñoz J, Ballester MR, Antonijoan RM, Gich I, Rodríguez M, Colli E, Gold S, Krolewiecki AJ. Safety and pharmacokinetic profile of fixed-dose ivermectin with an innovative 18mg tablet in healthy adult volunteers. PLoS Negl Trop Dis. 2018;12:e0006020. [PMC free article: PMC5773004] [PubMed: 29346388](Pharmacokinetic study compared fixed doses of ivermectin [16 or 32 mg] vs weight-based doses in 57 healthy volunteers, found equivalent plasma levels with all doses and there were no adverse events).
- Barda B, Sayasone S, Phongluxa K, Xayavong S, Keoduangsy K, Odermatt P, Puchkov M, Huwyler J, Hattendorf J, Keiser J. Efficacy of moxidectin versus ivermectin against Strongyloides stercoralis infections: a randomized, controlled noninferiority trial. Clin Infect Dis. 2017;65:276–81. [PubMed: 28369530](Among 127 subjects with Strongyloides stercoralis infection treated with a single dose of moxidectin or ivermectin, response rates were 94% and 95%, adverse event rates were similar and "none of the participants reported any side effect from treatment at any time point").
- Kircik LH, Del Rosso JQ, Layton AM, Schauber J. Over 25 Years of Clinical Experience With Ivermectin: An overview of safety for an increasing number of indications. J Drugs Dermatol. 2016;15:325–32. [PubMed: 26954318](Ivermectin has been used for more than 25 years for an expanding number of helminthic infections with an excellent safety profile both in humans and other mammals, probably because of its high specificity for invertebrate neuronal ion channels and because it does not cross the human blood-brain barrier; no mention of hepatotoxicity or ALT elevations).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, no cases were attributed to ivermectin).
- Ouédraogo AL, Bastiaens GJ, Tiono AB, Guelbéogo WM, Kobylinski KC, Ouédraogo A, Barry A, et al. Efficacy and safety of the mosquitocidal drug ivermectin to prevent malaria transmission after treatment: a double-blind, randomized, clinical trial. Clin Infect Dis. 2015;60:357–65. [PubMed: 25414262](Among 120 patients with Plasmodium falciparum infection given a single or repeated dose of artemether-lumefantrine with or without ivermectin, and no serious adverse events or "significant" biochemical abnormalities arose).
- Caly L, Druce JD, Catton MG, Jans DA, Wagstaff KM. The FDA-approved drug ivermectin inhibits the replication of SARS-CoV-2 in vitro. Antiviral Res. 2020;178:104787. [PMC free article: PMC7129059] [PubMed: 32251768](In cell culture, ivermectin was found to inhibit SARS-CoV-2 viral replication with greater than 90% decrease in viral RNA levels within 24 hours).
- Schmith VD, Zhou JJ, Lohmer LRL. The approved dose of ivermectin alone is not the ideal dose for the treatment of COVID-19. Clin Pharmacol Ther. 2020;108:762–5. [PMC free article: PMC7267287] [PubMed: 32378737](Administration of ivermectin to experimental animals in doses of up to 10 times the approved dose in humans failed to achieve the concentrations in lung tissue that were associated with antiviral activity in cell culture, suggesting that higher doses would be needed to show an effect in human COVID-19 infection).
- Rajter JC, Sherman MS, Fatteh N, Vogel F, Sacks J, Rajter JJ. Use of ivermectin is associated with lower mortality in hospitalized patients with coronavirus disease 2019: the ivermectin in COVID nineteen study. Chest. 2021;159:85–92. [PMC free article: PMC7550891] [PubMed: 33065103](Among 280 patients with COVID-19 in four Florida hospitals, prehospitalization administration of ivermectin [173 patients, typically given a single dose of 200 ug/kg] was associated with lower mortality [15% vs 25%] but similar durations of hospitalization; no mention of adverse events).
- Szente Fonseca SN, de Queiroz Sousa A, Wolkoff AG, Moreira MS, Pinto BC, Valente Takeda CF, Rebouças E, et al. Risk of hospitalization for Covid-19 outpatients treated with various drug regimens in Brazil: Comparative analysis. Travel Med Infect Dis. 2020;38:101906. [PMC free article: PMC7604153] [PubMed: 33137493](Among 3307 Northern Brazilian patients with confirmed COVID-19, the risk of hospitalization was less among those treated with prednisone or hydroxychloroquine or both, but not those treated with ivermectin compared to those who were not treated as outpatients; no mention of adverse events).
- Camprubí D, Almuedo-Riera A, Martí-Soler H, Soriano A, Hurtado JC, Subirà C, Grau-Pujol B, et al. Lack of efficacy of standard doses of ivermectin in severe COVID-19 patients. PLoS One. 2020;15(11):e0242184. [PMC free article: PMC7657540] [PubMed: 33175880](Outcomes of severe COVID-19 infection were similar among 13 hospitalized patients who were treated with a single dose of ivermectin to a matched untreated group; no mention of adverse events).
- Ahmed S, Karim MM, Ross AG, Hossain MS, Clemens JD, Sumiya MK, Phru CS, et al. A five-day course of ivermectin for the treatment of COVID-19 may reduce the duration of illness. Int J Infect Dis. 2021;103:214–6. [PMC free article: PMC7709596] [PubMed: 33278625](Among 70 hospitalized patients with COVID-19, viral clearance was more rapid in those treated with 5 days of ivermectin alone [9.7 days] compared to placebo [12.7 days] or the combination of ivermectin and doxycycline [11.5 days], while duration of hospitalization and frequency of symptoms was similar; there were no serious adverse events and no deaths).
- Pott-Junior H, Bastos Paoliello MM, Miguel AQC, da Cunha AF, de Melo Freire CC, Neves FF, da Silva de Avó LR, et al. Use of ivermectin in the treatment of Covid-19: A pilot trial. Toxicol Rep. 2021;8:505–10. [PMC free article: PMC7942165] [PubMed: 33723507](Among 30 hospitalized patients with COVID-19 treated with one of 3 doses of ivermectin [at an uncertain daily dose or duration] or with “standard of care”, the time to SARS-CoV-2 RNA negativity and rapidity of decline was similar in the three groups as were symptoms and adverse events; no mention of ALT levels and hepatotoxicity).
- Chaccour C, Casellas A, Blanco-Di Matteo A, Pineda I, Fernandez-Montero A, Ruiz-Castillo P, Richardson MA, et al. The effect of early treatment with ivermectin on viral load, symptoms and humoral response in patients with non-severe COVID-19: A pilot, double-blind, placebo-controlled, randomized clinical trial. EClinicalMedicine. 2021;32:100720. [PMC free article: PMC7816625] [PubMed: 33495752](Among 24 outpatients with recent onset of symptoms of COVID-19 treated with a single dose of ivermectin [400 µg/kg] or placebo, all 24 still had detectable viral RNA although in lower titers at day 7 and resolution of symptoms was similar, although slightly better in the ivermectin group).
- Lima-Morales R, Méndez-Hernández P, Flores YN, Osorno-Romero P, Cuecuecha-Rugerio E, Nava-Zamora A, Hernández-Galdamez DR, et al. Effectiveness of a multidrug therapy consisting of Ivermectin, Azithromycin, Montelukast, and Acetylsalicylic acid to prevent hospitalization and death among ambulatory COVID-19 cases in Tlaxcala, Mexico. Int J Infect Dis. 2021;105:598–605. [PMC free article: PMC7872854] [PubMed: 33578014](Among 768 ambulatory adults with recent onset of COVID-19 symptoms, the 481 who received combination oral therapy with ivermectin [12 mg single dose], azithromycin [500 mg for 4 days] montelukast [for 21 days] and aspirin [for 30 days] were more likely to recover within 2 weeks [84% vs 59%] than patients not given this regimen, and were also less likely to be hospitalized [9% vs 31%] and to die [3% vs 18%], and “most participants did not experience any side effects”; no mention of ALT elevations or hepatotoxicity).
- Behera P, Patro BK, Singh AK, Chandanshive PD, Ravikumar SR, Pradhan SK, Pentapati SSK, et al. Role of ivermectin in the prevention of SARS-CoV-2 infection among healthcare workers in India: A matched case-control study. PLoS One. 2021;16(2):e0247163. [PMC free article: PMC7886121] [PubMed: 33592050](Among 186 healthcare workers in India who developed COVID-19 infection compared to 186 matched uninfected controls, ivermectin prophylaxis was more frequent in controls [41% vs 22%] and the difference was most evident in those who took two doses of ivermectin [300 mg 4 days apart], and there were no adverse side effects).
- Babalola OE, Bode CO, Ajayi AA, Alakaloko FM, Akase IE, Otrofanowei E, Salu OB, et al. Ivermectin shows clinical benefits in mild to moderate COVID19: A randomised controlled double-blind, dose-response study in Lagos. QJM. 2021 Feb 18: hcab035. Epub ahead of print. [PMC free article: PMC7928689] [PubMed: 33599247](Among 62 patients with COVID-19 infection treated with ivermectin [6 or 12 mg every 84 hours] vs lopinavir/ritonavir, the days to viral RNA negativity was shorted with ivermectin [6.0 and 4.6 vs 9 days], but there were no differences in symptoms or outcomes of infection and no serious adverse events, while ALT and AST levels decreased slightly in all three groups while Alk P levels rose slightly).
- López-Medina E, López P, Hurtado IC, Dávalos DM, Ramirez O, Martínez E, Díazgranados JA, et al. Effect of ivermectin on time to resolution of symptoms among adults with mild COVID-19: a randomized clinical trial. JAMA. 2021;325(14):1426–35. [PMC free article: PMC7934083] [PubMed: 33662102](Among 400 patients with symptomatic but mild COVID-19 treated with ivermectin [300 mg daily] or placebo for 5 days, the time to resolution of symptoms was similar in the two groups [10 vs 12 days] as were adverse event rates [77% vs 81%] and serious adverse event rates [1% vs 1%], with no mention of ALT elevations or hepatotoxicity).
- Galan LEB, Santos NMD, Asato MS, Araújo JV, de Lima Moreira A, Araújo AMM, Paiva ADP, et al. Phase 2 randomized study on chloroquine, hydroxychloroquine or ivermectin in hospitalized patients with severe manifestations of SARS-CoV-2 infection. Pathog Glob Health. 2021 Mar 8;:1–8. Epub ahead of print. [PMC free article: PMC7938655] [PubMed: 33682640](Among 168 Brazilian adults hospitalized with severe COVID-19 pneumonia who were treated with oral doses of chloroquine, hydroxychloroquine or ivermectin [10 or 14 mg for 3 days], the mortality rate was similar in all three groups [22%, 21% and 23%] as were adverse event rates including serum aminotransferase elevations [25% vs 22% vs 26%].
Publication Details
Publication History
Last Update: April 9, 2021.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Ivermectin. [Updated 2021 Apr 9].