OVERVIEW
Introduction
Amikacin is a parenterally administered, broad spectrum aminoglycoside antibiotic typically used for severe gram negative infections. Despite widespread use, amikacin has not been associated with instances of acute liver injury.
Background
Amikacin (am" i kay' sin) is a semisynthetic aminoglycoside with a particularly broad antimicrobial activity which is used for severe bacterial infections caused by sensitive agents including those resistant to gentamicin or tobramycin. Like other aminoglycosides, amikacin is thought to act by binding to bacterial ribosomes and inhibiting protein synthesis. Nevertheless, amikacin is considered bacteriocidal as well as bacteriostatic. Amikacin and other aminoglycosides are typically used in combination with a penicillin or cephalosporin for treatment of severe infections with Pseudomonas aeruginosa, Enterobacter, Klebsiella, Serratia and other gram-negative bacteria resistant to less toxic antibiotics. Amikacin is most commonly used for septicemia, bacterial endocarditis, peritonitis, meningitis, pelvic inflammatory disease and pneumonia. Amikacin is also used in therapy of tuberculosis in combination with other antitubercular drugs. Amikacin was approved for use in the United States in 1981 and is available in several generic parenteral formulations. The typical adult dose is 15 mg/kg per day im or iv, usually in two or three divided doses over 5 to 10 days. The dose of amikacin must be modified based upon renal function and monitoring of drug levels is advisable. Common side effects include dizziness, headache, confusion, nausea and skin rash. Importantly, dose related adverse effects of amikacin include oto- and nephrotoxicity, which are shared by all aminoglycosides.
Hepatotoxicity
Intravenous and intramuscular therapy with amikacin has not been linked to serum alkaline phosphatase or aminotransferase elevations, and no convincing cases of symptomatic or icteric hepatotoxicity due to amikacin have been published. Other aminoglycosides have been linked to very rare cases of cholestatic hepatitis, that typically arise within 1 to 3 weeks of starting therapy, often associated with skin rash, fever and sometimes eosinophilia. Recovery typically occurs within 1 to 2 months and chronic injury has not been described. Amikacin as well as other aminoglycosides are not mentioned in large case series of drug induced liver disease and acute liver failure; thus, hepatic injury due to amikacin is very rare if it occurs at all.
Likelihood score: E (unlikely cause of clinically apparent liver injury).
Mechanism of Injury
The cause of the rare occurrence of cholestatic jaundice after aminoglycoside therapy is unknown, but suspected to be a part of a generalized hypersensitivity reaction. Uptake of aminoglycosides into hepatocytes is limited and they are rapidly excreted in the urine; high concentrations are found in mainly in renal tubular cells and hair cells of inner ear perhaps explaining why they are more likely to cause nephro- or oto- rather than hepatotoxicity.
Outcome and Management
The outcome of hepatic injury due to aminoglycosides is usually benign. Acute liver failure and chronic bile duct vanishing syndrome have been not been described after their use. Patients with any form of aminoglycoside hepatotoxicity should probably avoid future systemic aminoglycoside use.
References to the safety and potential hepatotoxicity of amikacin are provided in the Overview section on the Aminoglycosides.
Drug Class: Aminoglycosides
Other Drugs in the Class: Gentamicin, Neomycin, Plazomicin, Streptomycin, Tobramycin
PRODUCT INFORMATION
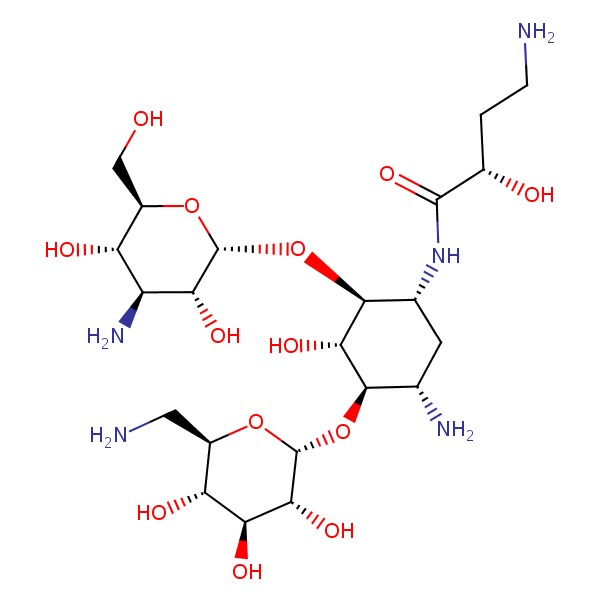
CHEMICAL FORMULA AND STRUCTURE
Publication Details
Publication History
Last Update: April 12, 2019.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Amikacin. [Updated 2019 Apr 12].