OVERVIEW
Introduction
Nortriptyline is a tricyclic antidepressant that is also used in smoking cessation. Nortriptyline can cause mild and transient serum enzyme elevations and is rare cause of clinically apparent acute and chronic cholestatic liver injury.
Background
Nortriptyline (nor trip' ti leen) is a tricyclic antidepressant which acts by inhibition of reuptake of serotonin and norepinephrine in synaptic clefts, thus increasing brain levels of these neurotransmitters. Nortriptyline was approved for use in the United States in 1964 for the treatment of depression. It is also used for smoking cessation and is commonly used in the United States, with more than 3 million prescriptions being filled yearly. Nortriptyline is available in generic forms and under the brand names of Aventyl and Pamelor in 10, 25, 50 and 75 mg tablets. An oral solution is also available. The typical recommended dose for depression is 25 mg three or four times daily, increasing based upon effect and tolerance to as much as 150 mg daily. The typical dose for smoking cessation is 25 mg daily, gradually increasing to a maximum of 100 mg daily. Common side effects include drowsiness, dizziness, restlessness, headache, blurred vision, dry mouth, constipation, and urinary retention.
Hepatotoxicity
Liver test abnormalities have been reported to occur in up to 16% of patients being treated with tricyclic antidepressants, but elevations are uncommonly above 3 times the upper limit of normal. The aminotransferase abnormalities are usually mild, asymptomatic and transient, reversing even with continuation of medication. Rare instances of clinically apparent acute liver injury have been reported due to nortriptyline. The onset of jaundice is usually within 2 to 3 months of starting nortriptyline and the predominant enzyme pattern has been hepatocellular. Several acute instances of nortriptyline hepatotoxicity with marked elevations in serum aminotransferase levels and acute liver failure have been described. Signs and symptoms of hypersensitivity and autoimmunity are usually not present.
Likelihood score: C (probable rare cause of clinically apparent liver injury).
Mechanism of Injury
The mechanism by which nortriptyline causes serum aminotransferase elevations and acute liver injury is not known. It undergoes extensive hepatic metabolism and a possible cause of liver injury is production of a toxic intermediate of metabolism.
Outcome and Management
The serum aminotransferase elevations that occur on nortriptyline therapy are usually self-limited and do not require dose modification or discontinuation of therapy. The acute hepatitis caused by nortriptyline can be severe and lead to acute liver failure. No cases of chronic liver injury or vanishing bile duct syndrome have been reported with nortriptyline therapy. While cross reactivity of hepatic injury with other tricyclic antidepressants has rarely been described, amitriptyline is metabolized to nortriptyline which is its active form. Thus, switching to amitriptyline after nortriptyline toxicity should be avoided. Switching to other forms of antidepressants such as the selective serotonin reuptake inhibitors is likely to be safe.
Drug Class: Antidepressant Agents
Other Drugs in the Subclass, Tricyclics: Amitriptyline, Amoxapine, Clomipramine, Desipramine, Doxepin, Imipramine, Protriptyline, Trimipramine
PRODUCT INFORMATION
REPRESENTATIVE TRADE NAMES
Nortriptyline – Aventyl®, Pamelor®
DRUG CLASS
Antidepressant Agents
Product labeling at DailyMed, National Library of Medicine, NIH
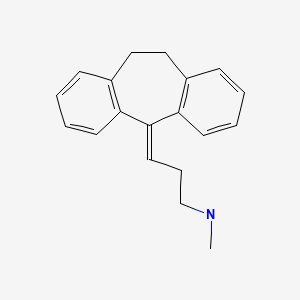
CHEMICAL FORMULA AND STRUCTURE
ANNOTATED BIBLIOGRAPHY
References updated: 05 April 2020
Abbreviations: MAO inhibitor, monoamine oxidase inhibitor; SSRI, selective serotonin reuptake inhibitor; SNRI, serotonin and norepinephrine reuptake inhibitor.
- Zimmerman HJ. Tricyclic antidepressants. In, Zimmerman HJ. Hepatotoxicity: the adverse effects of drugs and other chemicals on the liver. 2nd ed. Philadelphia: Lippincott, 1999, pp. 495-8.(Expert review of hepatotoxicity published in 1999; hepatic injury caused by tricyclic antidepressants is less frequent and less consistent than with monoamine oxidase inhibitors).
- Larrey D, Ripault MP. Antidepressants. Hepatotoxicity of psychotropic drugs and drugs of abuse. In, Kaplowitz N, DeLeve LD, eds. Drug-induced liver disease. 3rd ed. Amsterdam: Elsevier, 2013, pp. 447-52.(Review of tricyclic antidepressant hepatotoxicity mentions that clinically apparent liver injury due to tricyclics including nortriptyline is rare and presents with various patterns of serm enzyme elevations with latencies ranging from 1 week to 1 year, commonly with immunoallergic features and often exhibiting cross-hepatotoxicity among different tricyclics).
- O'Donnell JM, Bies RR, Shelton RC. Drug therapy of depression and anxiety disorders. In, Brunton LL, Hilal-Dandan R, Knollman BC, eds. Goodman & Gilman’s the pharmacological basis of therapeutics. 13th ed. New York: McGraw-Hill, 2018, pp. 267-77.(Textbook of pharmacology and therapeutics).
- Klerman GL, Cole JO. Clinical pharmacology of imipramine and related antidepressant compounds. Pharmacol Rev. 1965;17:101–41. [PubMed: 14294030](Extensive review of structure, pharmacology, clinical effects, mechanisms of action, drug interactions, and side effects of tricyclic antidepressants; jaundice is reported to occur in 0.5-1% of subjects, but usually resolves rapidly with stopping).
- Clarke AE, Maritz VM, Denborough MA. Phenothiazines and jaundice. Aust N Z J Med. 1972;2:376–82. [PubMed: 4144624](Chlorpromazine and amitriptyline cause precipitation of proteins when added to human bile in vitro and hepatotoxicity of these agents may relate to this characteristic).
- Fiori MG. Tricyclic antidepressants: a review of their toxicology. Curr Dev Psychopharmacol. 1977;4:71–110. [PubMed: 340145](Review of cardiac, hepatic, neurological, fetal and psychotoxicity of tricyclic antidepressants; most cases of hepatotoxicity have been attributed to hypersensitivity, but tricyclics are taken up and extensively metabolized by hepatocytes).
- Døssing M, Andreasen PB. Drug-induced liver disease in Denmark. An analysis of 572 cases of hepatotoxicity reported to the Danish Board of Adverse Reactions to Drugs. Scand J Gastroenterol. 1982;17:205–11. [PubMed: 6982502](Among 572 cases of drug induced liver disease seen between 1968-78 in Denmark, psychotropic agents accounted for 93 cases, 54 of which were due to chlorpromazine; tricyclics not specifically mentioned).
- Larrey D, Rueff B, Pessayre D, Algard M, Geneve J, Benhamou JP. Cross hepatotoxicity between tricyclic antidepressants. Gut. 1986;27:726–7. [PMC free article: PMC1433318] [PubMed: 3721296](39 year old woman developed abdominal pain 2 weeks after starting amineptine [a tricyclic antidepressant] with fever and eosinophilia [bilirubin 1.2 mg/dL, ALT 1360 U/L, Alk P 1.5 times ULN], resolving rapidly on stopping but recurring 7 days after starting clomipramine [ALT 1050 U/L, Alk P 1.5 times ULN], again resolving rapidly upon stopping).
- Genève J, Larrey D, Pessayre D, Benhamou JP. Structure tricyclique des medicaments et hepatotoxicite. Gastroenterol Clin Biol. 1987;11:242–9. [PubMed: 2884161](Review of structural similarity and hepatotoxicity of tricyclic antidepressants focusing on amineptine, imipramine and amitriptyline).
- Pirmohamed M, Kitteringham NR, Park BK. Idiosyncratic reactions to antidepressants: a review of the possible mechanisms and predisposing factors. Pharmacol Ther. 1992;53:105–25. [PubMed: 1641399](Review of idiosyncratic reactions to antidepressants; possible mechanism of injury being production of a chemically reactive metabolite that is either directly toxic or induces a hypersensitivity reaction).
- Berson A, Fréneaux E, Larrey D, Lepage V, Douay C, Mallet C. Possible role of HLA in hepatotoxicity. An exploratory study. J Hepatol. 1994;20:336–42. [PubMed: 8014443](Human leukocyte antigen [HLA] haplotypes done on 71 patients with drug induced liver disease; among 12 cases due to tricyclics [7 amineptine, 3 amitriptyline, 2 clomipramine], 6 [50%] had HLA A11 including 2 of the 3 amitriptyline cases; 12% of controls harbored this allele).
- Berkelhammer C, Kher N, Berry C, Largosa A. Nortriptyline-induced fulminant hepatic failure. J Clin Gastroenterol. 1995;20:54–6. [PubMed: 7884180](82 year old woman developed jaundice 2 months after starting nortriptyline [bilirubin 6.5 mg/dL, AST 1530 U/L, Alk P 276 U/L, protime 13.9 sec], with ascites on ultrasound, progressive jaundice, stupor and death from hepatic failure 7 weeks later).
- Remy AJ, Larrey D, Pageaux GP, Ribstein J, Ramos J, Michel H. Cross hepatotoxicity between tricyclic antidepressants and phenothiazines. Eur J Gastroenterol Hepatol. 1995;7:373–6. [PubMed: 7600146](65 year old woman developed fatigue and serum enzyme elevations [ALT ~1300 U/L; Alk P ~380 U/L] 1 month after starting trimipramine; 3 years later she developed nausea and ALT elevations 10 days after starting desipramine [ALT ~250 U/L], and 2 years later developed abdominal pain and fever and enzyme elevations [ALT ~1100 U/L, Alk P ~ 510 U/L] 8 days after starting cyamemazine; each time with rapid recovery and no jaundice).
- Pedersen AMB, Enevoldsen HK, Kohler H. Nortriptyline-induced hepatic failure. Ther Drug Monit. 1996;18:100–2. [PubMed: 8848811](52 year old woman developed jaundice 3 months after starting nortriptyline [bilirubin 5.0 mg/dL, ALT 9,590 U/L, Alk P 343 U/L, prothrombin activity 18%], testing revealed high nortriptyline levels and no acetaminophen; rapid spontaneous recovery).
- Allison DB, Mentore JL, Heo M, Chandler LP, Cappelleri JC, Infante MC, Weiden PJ. Antipsychotic-induced weight gain: a comprehensive research synthesis. Am J Psychiatry. 1999;156:1686–96. [PubMed: 10553730](Systematic review of 81 articles on weight change with antipsychotics; using change after 10 weeks to compare: clozapine +5.7, olanzapine +4.2, chlorpromazine +4.2, risperidone +1.7, loxapine +0.6, haloperidol +0.5, ziprasidone +0.3, molindone -0.1, and pimozide -2.7 kilograms).
- Grohmann R, Rüther E, Engel RR, Hippius H. Assessment of adverse drug reactions in psychiatric inpatients with the AMSP drug safety program: methods and first results for tricyclic antidepressants and SSRIs. Pharmacopsychiatry. 1999;32:21–8. [PubMed: 10071179](Analysis of reporting of adverse events among inpatients in 29 German hospitals between 1993 to 1997; 896 severe adverse events among 48,564 patients [1.8%], both total and hepatic events were more common with tricyclics than SSRIs).
- Carvajal García-Pando A, García del Pozo J, Sánchez AS, Velasco MA, Rueda de Castro AM, Lucena MI. Hepatotoxicity associated with the new antidepressants. J Clin Psychiatry. 2002;63:135–7. [PubMed: 11874214](Analysis of cases of hepatotoxicity from antidepressants in Spanish Pharmacovigilance System from 1989-1999, identified 99 cases; among SSRIs, 26 due to fluoxetine, 14 paroxetine, 6 fluvoxamine, 5 sertraline, 3 venlafaxine and 2 citalopram; among tricyclics, 16 clomipramine 7 amitriptyline, 6 imipramine; among miscellaneous, 3 nefazodone and 1 trazodone; but all similar in rate ~1-3 per 100,000 patient-years of exposure, except for nefazodone=29/100,000. Nortriptyline not mentioned).
- Lucena MI, Carvajal A, Andrade RJ, Velasco A. Antidepressant-induced hepatotoxicity. Expert Opin Drug Saf. 2003;2:249–62. [PubMed: 12904104](Review of hepatotoxicity of antidepressants; antidepressant use has increased markedly between 1992 and 2002, accounting for 5% of cases of hepatotoxicity; tricyclics less likely to cause injury than MAO inhibitors; predominantly cholestatic patterns with onset in first 2-3 weeks; occasional reports of prolonged cholestasis).
- Degner D, Grohmann R, Kropp S, Rüther E, Bender S, Engel RR, Schmidt LG. Severe adverse drug reactions of antidepressants: results of the German multicenter drug surveillance program AMSP. Pharmacopsychiatry. 2004;37 Suppl 1:S39–45. [PubMed: 15052513](53,042 patients treated with antidepressants in 35 psychiatric hospitals in Germany from 1993-2000 were monitored for adverse drug reactions; increased liver enzymes reported in 16% on tricyclics, 5.5% on SSRIs and 12% of monoamine oxidase inhibitors).
- Sabaté M, Ibáñez L, Pérez E, Vidal X, Buti M, Xiol X, Mas A, et al. Risk of acute liver injury associated with the use of drugs: a multicentre population survey. Aliment Pharmacol Ther. 2007;25:1401–9. [PubMed: 17539979](Among 126 cases of drug induced liver injury seen in Spain between 1993-2000, 3 were due to amitriptyline with a relative risk of 14.2: estimated frequency of 6 per 100,000 person-year exposures).
- DeSanty KP, Amabile CM. Antidepressant-induced liver injury. Ann Pharmacother. 2007;41:1201–11. [PubMed: 17609231](Review of drug induced liver injury and summary analysis of reports of injury from MAO inhibitors, SSRIs, tricyclics and atypical agents).
- Chalasani N, Fontana RJ, Bonkovsky HL, Watkins PB, Davern T, Serrano J, Yang H, Rochon J., Drug Induced Liver Injury Network (DILIN). Causes, clinical features, and outcomes from a prospective study of drug-induced liver injury in the United States. Gastroenterology. 2008;135:1924–34. [PMC free article: PMC3654244] [PubMed: 18955056](Among 300 cases of drug induced liver disease in the US collected from 2004 to 2008, only 1 case was attributed to amitriptyline, no other tricyclic mentioned).
- Reuben A, Koch DG, Lee WM., Acute Liver Failure Study Group. Drug-induced acute liver failure: results of a U.S. multicenter, prospective study. Hepatology. 2010;52:2065–76. [PMC free article: PMC3992250] [PubMed: 20949552](Among 1198 patients with acute liver failure enrolled in a US prospective study between 1998 and 2007, 133 were attributed to drug induced liver injury, but none were linked to tricyclic antidepressants).
- Molleston JP, Fontana RJ, Lopez MJ, Kleiner DE, Gu J, Chalasani N., Drug-induced Liver Injury Network. Characteristics of idiosyncratic drug-induced liver injury in children: results from the DILIN prospective study. J Pediatr Gastroenterol Nutr. 2011;53:182–9. [PMC free article: PMC3634369] [PubMed: 21788760](Among 30 children with suspected drug induced liver injury, half [n=15] were due to antimicrobials [minocycline 4, INH 3, azithromycin 3] and the rest largely due to CNS agents and anticonvulsants; one case was attributed to amitriptyline, but no other tricyclic antidepressant was listed).
- Park SH, Ishino R. Liver injury associated with antidepressants. Curr Drug Saf. 2013;8:207–23. [PubMed: 23914755](Review of drug induced liver injury due to antidepressants; nortriptyline is not mentioned).
- Björnsson ES, Bergmann OM, Björnsson HK, Kvaran RB, Olafsson S. Incidence, presentation and outcomes in patients with drug-induced liver injury in the general population of Iceland. Gastroenterology. 2013;144:1419–25. [PubMed: 23419359](In a population based study of drug induced liver injury from Iceland, 96 cases were identified over a 2 year period, none of which were attributed to amitriptyline or other tricyclic antidepressant).
- Voican CS, Corruble E, Naveau S, Perlemuter G. Antidepressant-induced liver injury: a review for clinicians. Am J Psychiatry. 2014;171:404–15. [PubMed: 24362450](Review of the frequency and clinical features of drug induced liver injury due to antidepressants; imipramine, desipramine, amitriptyline and clomipramine are discussed, but not nortriptyline).
- Hernández N, Bessone F, Sánchez A, di Pace M, Brahm J, Zapata R, A, Chirino R, et al. Profile of idiosyncratic drug induced liver injury in Latin America. An analysis of published reports. Ann Hepatol. 2014;13:231–9. [PubMed: 24552865](Systematic review of literature of drug induced liver injury in Latin American countries published from 1996 to 2012 identified 176 cases, only one of which was attributed to an antidepressant [amitriptyline] and none to a MAO inhibitor, SSRI or SNRI).
- Chalasani N, Bonkovsky HL, Fontana R, Lee W, Stolz A, Talwalkar J, Reddy KR, et al. United States Drug Induced Liver Injury Network. Features and outcomes of 899 patients with drug-induced liver injury: The DILIN Prospective Study. Gastroenterology. 2015;148:1340–52.e7. [PMC free article: PMC4446235] [PubMed: 25754159](Among 899 cases of drug induced liver injury enrolled in a US prospective study between 2004 and 2013, 20 cases [2%] were attributed to antidepressants including 9 due to SNRIs [7 to duloxetine, 1 each to nefazodone and trazodone], 5 to bupropion, 5 to SSRIs [3 to escitalopram, and 1 each to fluoxetine and sertraline], and only 1 to tricyclics [imipramine], but none to nortriptyline).
- Woo HJ, Kim HY, Choi ES, Cho YH, Kim Y, Lee JH, Jang E. Drug-induced liver injury: A 2-year retrospective study of 1169 hospitalized patients in a single medical center. Phytomedicine. 2015;22:1201–5. [PubMed: 26598920](Among 1169 inpatients seen at a single Korean referral medical center over a 2 year period, 11 developed suspected drug induced liver injury, 6 attributed to dietary supplements and 5 to conventional drugs including 2 antidepressants [minocycline, donepezil, warfarin, gabapentin/milnacipran, and antihistamines]).
- Voican CS, Martin S, Verstuyft C, Corruble E, Perlemuter G, Colle R. Liver function test abnormalities in depressed patients treated with antidepressants: a real-world systematic observational study in psychiatric settings. PLoS One. 2016;11:e0155234. [PMC free article: PMC4865191] [PubMed: 27171561](Among 321 psychiatric inpatients, only 116 [36%] had liver tests performed and only 18 during therapy with an antidepressant, 3 of which were suspected to have drug induced liver injury, 1 each with escitalopram, venlafaxine and amitriptyline, all without jaundice and 2 without symptoms, all 3 resolving).
- Friedrich ME, Akimova E, Huf W, Konstantinidis A, Papageorgiou K, Winkler D, Toto S, et al. Drug-induced liver injury during antidepressant treatment: results of AMSP, a drug surveillance program. Int J Neuropsychopharmacol. 2016;19(4):pyv126. pii. [PMC free article: PMC4851269] [PubMed: 26721950](Among 184,234 psychiatric inpatients from 80 hospitals, 149 cases [0.08%] of drug induced liver injury were reported including 71 of 50,201 patients treated with tricyclics, 18 of 11,876 receiving trimipramine and 2 of 2,016 receiving nortriptyline).
- Gahr M, Zeiss R, Lang D, Connemann BJ, Hiemke C, Schönfeldt-Lecuona C. Drug-Induced liver injury associated with antidepressive psychopharmacotherapy: an explorative assessment based on quantitative signal detection using different MedDRA terms. J Clin Pharmacol. 2016;56:769–78. [PubMed: 26470856](Using data on adverse drug reaction reports from the Uppsala Monitoring Center of WHO, there were higher relative hepatotoxicity reports for nefazodone, agomelatine, many tricyclics and mirtazapine).
- Chen VC, Lin CF, Hsieh YH, Liang HY, Huang KY, Chiu WC, Lee Y, McIntyre RS, et al. Hepatocellular carcinoma and antidepressants: a nationwide population-based study. Oncotarget. 2017;8:30464–70. [PMC free article: PMC5444756] [PubMed: 27783998](Among almost 50,000 cases of hepatocellular carcinoma registered in the Taiwan National Health Insurance Research Database, the rate of antidepressant use was lower than in approximately 250,000 matched controls from the database).
- Ferrajolo C, Scavone C, Donati M, Bortolami O, Stoppa G, Motola D, Vannacci A, et al. DILI-IT Study Group. Antidepressant-Induced Acute liver injury: a case-control study in an Italian inpatient population. Drug Saf. 2018;41:95–102. [PubMed: 28770534](Among 179 cases of hospitalizations for unexplained acute liver injury enrolled in an Italian prospective study between 2010 and 2014, 17 had been exposed to antidepressants including citalopram [n=4], sertraline [n=3], amitriptyline [n=3] and paroxetine [n=2], clomipramine [n=1] and amitriptyline [n=1]).
- Billioti de Gage S, Collin C, Le-Tri T, Pariente A, Bégaud B, Verdoux H, Dray-Spira R, et al. Antidepressants and hepatotoxicity: a cohort study among 5 million individuals registered in the French National Health Insurance Database. CNS Drugs. 2018;32:673–84. [PMC free article: PMC6061298] [PubMed: 29959758](Among 5 million persons identified in a national French health insurance database who started an antidepressant between 2010 and 2015, 382 developed serious liver injury resulting in hospitalization, rates per 100,0000 persons-years being 19 for SSRIs, 22 venlafaxine, 13 duloxetine, and 33 mirtazapine; conventional tricyclics and MAO inhibitors not discussed).
- Pladevall-Vila M, Pottegård A, Schink T, Reutfors J, Morros R, Poblador-Plou B, Timmer A, et al. Risk of acute liver injury in agomelatine and other antidepressant users in four European countries: a cohort and nested case-control study using automated health data sources. CNS Drugs. 2019;33:383–95. [PMC free article: PMC6441103] [PubMed: 30830574](Analysis of data sources from 4 European countries identified 3.2 million persons initiating antidepressant therapy among whom there was no increased risk for acute liver injury for agomelatine compared to citalopram, an SSRI with a low rate of hepatotoxicity).
- Drugs for depression. Med Lett Drugs Ther. 2020;62(1592):25–32. [PubMed: 32320387](Concise review of the mechanism of action, clinical efficacy, safety and costs of drugs for depression, mentions that tricyclics and MAO inhibitors remain valuable alternatives for treatment of moderate-to-severe depression, despite concerns about their safety; hepatotoxicity is mentioned only for nefazodone [now rarely used because of severe hepatotoxicity] and duloxetine [in heavy drinkers]).
- Ueberberg B, Frommberger U, Messer T, Zwanzger P, Kuhn J, Anghelescu I, Ackermann K, et al. Drug-induced liver injury (DILI) in patients with depression treated with antidepressants: a retrospective multicenter study. Pharmacopsychiatry. 2020;53:60–4. [PubMed: 31958850](Among 329 psychiatric inpatients with depression seen at 6 psychiatric centers in Germany, 17 [5%] had serum aminotransferase elevations but none had clinically apparent liver injury, most commonly implicated drugs included mirtazapine, agomelatine, citalopram and venlafaxine).
Publication Details
Publication History
Last Update: April 5, 2020.
Copyright
Publisher
National Institute of Diabetes and Digestive and Kidney Diseases, Bethesda (MD)
NLM Citation
LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012-. Nortriptyline. [Updated 2020 Apr 5].