Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 843663-66-1
Drug Levels and Effects
Summary of Use during Lactation
Data from two women taking bedaquiline and one of their breastfed infants indicate that exposure of the infant to the drug via breastmilk is substantial, with one infant having a therapeutic serum level. The clinical consequences of this exposure are unknown. The drug could protect the infant from multidrug-resistant tuberculosis, or could result in adverse effects. If bedaquiline is required by the mother, it is not a reason to discontinue breastfeeding. Monitor breastfed infants for adverse reactions, such as inadequate weight gain, liver toxicity, nausea, arthralgia, headache, hemoptysis, and chest pain.[1]
Drug Levels
Bedaquiline is metabolized to an N-monodesmethyl metabolite (M2). M2 has 4-fold to 6-fold lower antimycobacterial potency compared to bedaquiline. After reaching peak equilibrium levels with repeat administration, the mean terminal elimination half-lives of bedaquiline and M2 are approximately 5.5 months.
Maternal Levels. Two mothers taking bedaquiline 200 mg three times weekly provided milk samples after a dose of the drug. Both were also taking linezolid, high-dose isoniazid, levofloxacin, clofazimine, pyrazinamide and ethambutol for tuberculosis, as well as tenofovir, emtricitabine and nevirapine for HIV. One mother’s milk bedaquiline levels between 26.5 and 30.8 hours after a dose were between 5.75 and 8.11 mg/L and M2 levels were between 0.57 and 0.81 mg/L. The second woman had a bedaquiline milk level of 6 mg/L at 6 hours after a dose. Other levels taken at 2, 4 and 48 hours after a dose ranged between 2.6 and 3.2 mg/L. M2 levels at the same times ranged between 2.7 and 3.6 mg/L. A pharmacokinetic model was developed and using the average maternal bedaquiline serum concentrations, the infant bedaquiline dose would be 0.816 mg/kg daily and the infant M2 dose would be 0.07 mg/kg daily. Based on the average maternal dose of 1.22 mg/kg daily, the estimated relative infant dosage would be about 73% of the maternal dosage.[2]
Infant Levels. One infant was breastfed by a mother who was taking bedaquiline. A single random plasma concentration was similar to the maternal plasma concentration. In 3 other non-breastfed infants, plasma concentrations were detectable but lower than maternal plasma concentrations.
Effects in Breastfed Infants
A woman who was co-infected with HIV and rifampin-resistant tuberculosis took bedaquiline (dosage not stated) as part of her antituberculosis regimen, which consisted of pyrazinamide and other unnamed drugs. At the 1-month follow-up, the infant was small and not gaining weight well, but the mother was nauseated from her medication regimen and had also lost weight. Six months later after completion of the mother’s therapy, her infant’s weight was increasing, following the normal trajectory of the growth chart, and reaching her developmental milestones.[1]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
References
- 1.
- Loveday M, Hlangu S, Furin J. Breastfeeding in women living with tuberculosis. Int J Tuberc Lung Dis. 2020;24:880–91. [PubMed: 33156754]
- 2.
- Court R, Gausi K, Mkhize B, et al. Bedaquiline exposure in pregnancy and breastfeeding in women with rifampicin-resistant tuberculosis. Br J Clin Pharmacol. 2022;88:3548–58. [PMC free article: PMC9296589] [PubMed: 35526837]
Substance Identification
Substance Name
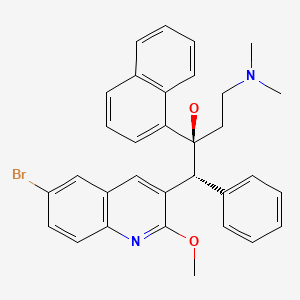
Bedaquiline
CAS Registry Number
843663-66-1
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Bedaquiline: Fallible Hope Against Drug Resistant Tuberculosis.[Indian J Microbiol. 2017]Review Bedaquiline: Fallible Hope Against Drug Resistant Tuberculosis.Singh P, Kumari R, Lal R. Indian J Microbiol. 2017 Dec; 57(4):371-377. Epub 2017 Oct 24.
- Review Levetiracetam.[Drugs and Lactation Database (...]Review Levetiracetam.. Drugs and Lactation Database (LactMed®). 2006
- Review Solriamfetol.[Drugs and Lactation Database (...]Review Solriamfetol.. Drugs and Lactation Database (LactMed®). 2006
- Review Cinacalcet.[Drugs and Lactation Database (...]Review Cinacalcet.. Drugs and Lactation Database (LactMed®). 2006
- Review Brivaracetam.[Drugs and Lactation Database (...]Review Brivaracetam.. Drugs and Lactation Database (LactMed®). 2006
- Bedaquiline - Drugs and Lactation Database (LactMed®)Bedaquiline - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
