Abbreviations
- CADTH
Canadian Agency for Drugs and Technologies in Health
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- IWGDF
International Working Group on the Diabetic Foot
- NICE
National Institute for Health and Care Excellence
- PICO
Population, intervention, comparator, and intervention
- RCT
randomized controlled trial
- SR
systematic review
Context and Policy Issues
Diabetes is characterized by high blood glucose and is associated with large disease burden in Canada.1 In 2015, approximately 9%, or 3.4 million, Canadians had diabetes and in 2018, Diabetes Canada estimated that by 2025 that number will increase to 5 million or 12.1%.1,2 Diabetes is the third highest risk factor for premature mortality after tobacco use and high blood pressure.1 In 2008/2009, one in ten adult deaths in Canada were attributed to diabetes related complications.1,2 Complications of diabetes include acute conditions, such as hyper- or hypoglycemia, diabetic ketoacidosis and hyperglycemic hyperosmolar non-ketotic syndrome, and chronic ones, such as cardiovascular disease, diabetic retinopathy, nephropathy, and extremity complications.3
About 6% of people with diabetes are affected by foot problems, including infection, ulceration, or tissue destruction of the foot, commonly referred to as ‘diabetic foot’.4 Between 0.03% and 1.5% of individuals with diabetic foot need limb amputation at some point in their lives.4 In 2008/2009, the likelihood of hospitalization due to non-traumatic lower limb amputations were about 20 times higher among Canadian adults diagnosed with diabetes, compared to those not diagnosed with diabetes.3
There are two major pathways leading to diabetic foot.4 One is peripheral neuropathy and the other is ischemia due to peripheral arterial disease, both of which can progress rapidly with uncontrolled diabetes.4 Walking without proper protection, lack of awareness, delayed care, and inappropriate care can facilitate the pathological changes and lead to severe consequences, such as foot deformity, fracture, and infection, which may require limb amputation or may directly contribute to patient mortality.4
Several reports by the Canadian Agency for Drugs and Technologies in Health (CADTH) have addressed the importance of diabetic foot care, either through prevention or treatment.5–8 Screening programs for diabetic foot ulcers include assessment of risk (risk stratification), patient education, and referral to specialized care.8 It was found that patient education alone might not be effective for the prevention of foot ulcers and amputations.9 In one CADTH report published in 2014, it was found that diabetic foot ulcer screening, based on risk stratification, was effective in improving clinical outcomes.7 In the same report, eight clinical guidelines all recommended assessing the risk factors of diabetic foot ulcers based on evidence of different levels of strengths.7 In an updated summary published in 2016, one guideline was identified and foot care was recommended for those at high risk for diabetic foot ulcers.8
No evidence identified to support the use of pressure-sensing shoe insoles10 or the direct delivery of podiatry care for the prevention of diabetic foot has been identified in previous CADTH reports.11 In order to have comprehensive understanding of the potential health benefits of preventative foot care, this study aims to review the evidence on the role of preventative foot care on the health outcomes of people with diabetes.
Research Questions
What is the clinical effectiveness of providing preventative foot care for patients with diabetes and asymptomatic feet?
What is the cost-effectiveness of providing preventative foot care for patients with diabetes and asymptomatic feet?
What are the evidence-based guidelines regarding the provision of preventative foot care for patients with diabetes and asymptomatic feet?
Key Findings
One systematic review of critically low quality and three evidence-based guidelines by Diabetes Canada, the National Institute for Health and Care Excellence (NICE) and the International Working Group on the Diabetic Foot (IWGDF) were identified. In the systematic review, a variety of foot care or education program were assessed. Health education program were different in design, setting, approach, outcome measures, and results. The implementation of the health education program was related to an improvement in foot self-care scores and foot problems. Subsequent follow-ups and evaluations were also significantly associated with better outcomes. No relevant cost-effectiveness study was identified. Three guidelines all recommend annual examination of the feet for foot problems among patients with diabetes. Both the guidelines by the NICE and the IWGDF recommend adequate education to improve self-care, risk stratification, and timely referral to specialist care. The NICE guideline further specifies the types of specialists required for foot protection services, procedures to inspect the feet, timing for patient education, and frequencies to assess the risk of developing diabetic foot problems for children or adolescents. The IWGDF guideline recommends that people with diabetes protect their feet by avoiding certain activities, such as walking barefoot and wearing unfit footwear, as well as foot temperature monitoring. There are a variety of guidelines targeting different contexts and settings, all of which recommend preventative foot care for people with diabetes.
Methods
Literature Search Methods
A limited literature search was conducted on key resources including PubMed, The Cochrane Library, University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. No filters were applied to limit retrieval to by publication type. Where possible, retrieval was limited to the human population. The search was also limited to English language documents published between January 1, 2008 and October 17, 2018.
Selection Criteria and Methods
One reviewer screened citations and selected studies. In the first level of screening, titles and abstracts were reviewed and potentially relevant articles were retrieved and assessed for inclusion. The final selection of full-text articles was based on the inclusion criteria presented in .
Exclusion Criteria
Articles were excluded if they did not meet the selection criteria outlined in , they were duplicate publications, or were published prior to 2008. Guidelines with unclear methodology were also excluded. Studies that solely studied patients’ behavioral changes or the levels of self-care were not included.
Critical Appraisal of Individual Studies
The included systematic reviews were critically appraised by one reviewer using AMSTAR 2 tool,12 and guidelines were assessed with the AGREE II instrument.13 Summary scores were not calculated for the included studies; rather, a review of the strengths and limitations of each included study were described narratively.
Summary of Evidence
Quantity of Research Available
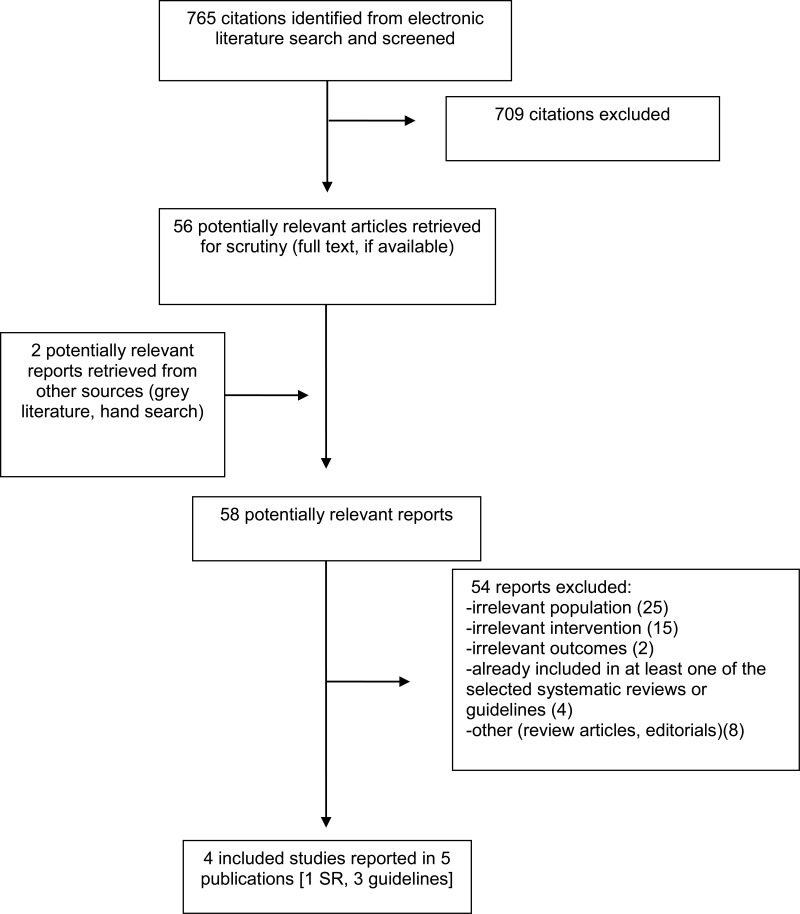
A total of 765 citations were identified in the literature search. Following screening of titles and abstracts, 709 citations were excluded and 56 potentially relevant reports from the electronic search were retrieved for full-text review. Two potentially relevant publications were retrieved from the grey literature search for full text review. Of these potentially relevant articles, 54 publications were excluded for various reasons, and four publications met the inclusion criteria and were included in this report. These comprised one systematic review and three evidence-based guidelines (published in four citations). Appendix 1 presents the PRISMA14 flowchart of the study selection. Additional citations that may be of interest are included in Appendix 5.
Summary of Study Characteristics
Additional details regarding the characteristics of included publications are provided in Appendix 2.
Study Design
One systematic review (SR) published in 2016 was included.15 Multiple databases were searched, a protocol was not published, and due to heterogeneity, meta-analysis was not conducted.15 Three evidence-based guidelines were published in 2015, 2017 and 2018.16–18 Systematic literature searches were conducted for the guidelines, but the search end dates were not mentioned.16–18
Country of Origin
The authors of the SR were based in Malaysia.15 The most recent guideline was published by Diabetes Canada, applicable to Canadian clinicians.18 Another guideline was published by the National Institute for Health and Care Excellence (NICE) in the United Kingdom and applicable to the National Health Service (NHS) settings.16 The other was developed by the International Working Group on the Diabetic Foot (IWGDF) based in the Netherlands and authors stated that the guideline is applicable to all countries.17
Patient Population
Studies that included people 60 years and older with diabetes were eligible for the SR.15 The exact age ranges of the participants in the primary studies were not described.15 Two of the 14 primary studies included people at high risk for foot problems and the patient characteristics on the other primary studies were not described.15
The intended users and target populations of the guideline published by Diabetes Canada, the NICE, and the IWGDF were clinicians and people with diabetes respectively.16–18
Interventions and Comparators
Studies that examined health education programs assisted with multimedia and programs conducted by health professionals were the interventions of interest and eligible for the SR.15 The identified interventions included foot self-care education programs, general measures of diabetes self-care education programs, and theory-based education tools for the prevention of health and foot problems.15 A variety of approaches were observed.15 They were categorized by whether implemented in groups or in health care settings.15 Nine primary studies were group-based, three were one-to-one interventions, and the approaches in two studies were unknown.15 Nine studies were in health care settings, three in home settings, and two in the settings that involved health care or home visits or other communication tools.15 Comparators identified in the primary studies included usual care and written education.15 However, the comparators in nine of the 14 primary studies were not described or were unclear.15
The interventions or practices for diabetes management were evaluated in the Diabetes Canada guideline.18 Interventions for foot care were evaluated as part of the guideline, but the exact search terms were not described.18 The interventions or practices for the prevention and management of diabetic foot problems were eligible for the NICE guideline.16 The IWGDF guideline included interventions for foot ulcer prevention in people at-risk for diabetes-related foot problems to prevent and heal foot ulcers in diabetes, as well as other measures for the management and diagnosis of diabetic foot problems.17
Outcomes
The primary outcome in the SR was diabetes foot self-care, including inspection, hygiene, appropriate socks and shoes (n of primary studies = 10).15 The secondary outcomes were foot problems, including neuropathy (n = 1), ulceration (n = 2), foot disability (n = 1), callus (n = 1), tinea pedis (n = 1), and foot scores (n = 1).15
In the Diabetes Canada guideline, clinically relevant outcomes were searched and evaluated by the guideline authors.18 In the NICE guideline, the outcomes searched in the literature were specific to the research questions.16 Overall, treatment objectives in the prevention, recognition, diagnosis, treatment and management of diabetic foot problems such as rates of ulceration, infection, complications and amputation rates were considered.16 In the IWGFD guideline, the outcomes considered were foot problems in persons with diabetes.17
Summary of Critical Appraisal
In the SR by Ahmad Sharoni et al., the population, intervention, comparator, and outcome components and selection of study design were reported.15 A comprehensive literature search with multiple databases was conducted and the included studies were well-described.15 The risk of bias in the primary studies was assessed with Cochrane Collaboration’s tool for assessing risk of bias.15 The risk of bias due to authors’ subjective selection of the literature might have been minimized. However, the review protocol was not published a priori.15 Study selection and data extraction were not conducted in duplicate.15 There might be some risk due to the inconsistency in study selection at these stages. The list of excluded studies was not provided.15 This limited research reproducibility and prevented the readers from further scrutinizing the reasons of exclusion. The funding sources of the included studies were not provided.15 This might lead to a collection of studies that favored the interventions due to potential publication bias where studies funded commercial interests tend to be more likely to be published.19 There was no meta-analysis conducted for the diversity of interventions and settings.15 There was no enough evidence to pool. Risk of bias in the included studies was not considered when interpreting the results.15 The results from poor-quality studies might have been weighted more than they should be – however this is unclear based on the publication. The heterogeneity between studies was not explained.15 The review authors’ conflict of interest was not declared.15 The existence and the potential impact of the funding agencies were not clear.
In the Diabetes Canada, NICE and IWGDF guidelines, the overall objectives, health questions, and applicable populations were specifically described.16–18 Relevant professional groups were included in the guideline development groups and the target users were clearly defined.16–18 The strengths and limitations of the body of evidence were described and the evidence to support the recommendations were identified.16–18 The recommendations in the three guidelines were specific and unambiguous and the key recommendation were easily identifiable.16–18
The NICE and IWGDF guidelines provided different options for prevention and resource implications were provided.16,17 The facilitators and barriers to the application and the potential resource implications were described.16,17 The options for prevention and the facilitators and barriers to the application were not described in the Diabetes Canada guideline.18
In the Diabetes Canada and NICE guideline, patients’ views and preferences were considered in the guideline development.16,18 The criteria for selecting the evidence, the methods for formulating the recommendations, and the advices to implement the recommendations were described.16,18 The critical appraisal tools were specified in the guidelines.
In contrast, Schaper et al. did not describe the views and preferences of the patients, the criteria for selecting the evidence, the methods for formulating the recommendations in the IWGDF guideline.17 Patients’ perspectives and views would have been potentially beneficial to improve guideline feasibility. It was unclear whether certain studies might be preferred by guideline authors to form recommendations. The health benefits, side effects, and risks of the interventions were not explicitly considered.17
The role of the funding bodies and competing interests of the guideline authors were declared in the Diabetes Canada guideline,18 while the other two did not.16,17 The critical appraisal tool used by the IWGDF was the Grading of Recommendations Assessment, Development and Evaluation (GRADE).17
External review, update procedures, and monitoring or auditing criteria were not mentioned in the three guidelines.16–18
Additional details regarding the strengths and limitations of included publications are provided in Appendix 3.
Summary of Findings
Appendix 4 presents a table of the main study findings and authors’ conclusions.
Clinical Effectiveness of Preventive Diabetic Foot Care for Patients with Diabetes
One SR of critically low quality by Ahmad Sharoni et al. was identified.15 A variety of foot care or education programs were examined, including diabetes foot self-care education, general measures of diabetes self-care programs, and theory-based education tools for the prevention of foot.15 Health education programs were different in the design of education tools, setting, approach, outcome measures and results.15 It was concluded that foot assessment, verbal and written instructions, and discussion were associated with improvement in foot self-care and foot problems.15
Two of the primary studies included in the SR found that health education programs were related to improvement in both foot self-care scores and incidence of neuropathy and ulcers.15 Nine primary studies identified improvement in foot self-care scores and did not find significant impact on the incidence of foot problems.15 Additionally, the authors of the SR reported that foot care or education programs that occurred either in groups or individually would be useful to reduce the incidence of foot problems.15
Follow-up sessions and evaluations by professionals were significantly associated with better outcomes after one month to three years of follow-up.15 The implementation of the health education program was related to an improvement in foot self-care scores and foot problems (such as neuropathy, foot disability, lesion, ulcer, tinea pedis and callus grade).15
Cost-Effectiveness of Preventive Diabetic Foot Care for Patients with Diabetes
No relevant cost-effectiveness studies regarding preventive diabetic foot care for patients with diabetes were identified; therefore, no summary can be provided.
Guidelines
Three evidence-based guidelines that provided recommendations for clinicians who provide diabetes care were identified.16–18 All provided recommendations for the prevention and management of diabetic foot problems.16–18
Diabetes Canada guideline18
The guideline from Diabetes Canada recommends that healthcare providers provide foot examination to identify patients with diabetes who are at risk for ulcers and lower-extremity amputation.18 Foot examination should be conducted at least annually and at more frequent intervals in high-risk patients and the examination should include the assessment for neuropathy, skin changes, peripheral arterial diseases, and structural abnormality.18 According to the Diabetes Canada criteria for the strengths of evidence, the grades of the recommendations were Grade C (Level 3), Grade D (Level 4) and Grade D (Level 4) respectively.18
International Working Group on the Diabetic Foot guideline17
The evidence-based guideline by the IWGDF was summarized by Schaper et al.17 The detailed list of the evidence-based recommendations for the prevention of foot problems in diabetes was published in Bus et al.20
The IWGDF recommends annual examination of the feet for signs or symptoms of peripheral neuropathy and peripheral artery disease individuals with diabetes who are at risk of foot ulceration (GRADE strength of recommendation: strong; quality of evidence: low).20 Further, they recommend screening for a history of foot problems in patients with diabetes and peripheral neuropathy (strong; low).20 They state that pre-ulcerative signs on the foot of patients with diabetes should be treated strong; low).20 To protect feet, the IWGDF guidelines recommend that those at-risk for foot problems avoid walking barefoot, in socks only, or in thin-soled standard slippers and should wear properly fitting footwear (strong; low).20 It is further recommended hat at-risk patients inspect their feet and inside of their shoes daily, wash their feet daily, avoid both chemical agents or plasters to remove calluses or corns, should use emollients to lubricate dry skin, and cut toe nails straight across (weak; low).20 Education activities that aim to improve foot care knowledge and behaviour and to encourage patients to foot care advices are recommended (weak; low).20 Additionally, foot temperature monitoring at home is recommended to identify the early signs of inflammation (weak; moderate).20
National Institute for Health and Care Excellence guideline16
The recommendations regarding the prevention of diabetic foot problems are grouped into two themes: care across all settings and assessing the risk of developing a diabetic foot problem.16
To provide care across all settings, the NICE guideline recommends providing foot protection services led by podiatrists with specialized training in diabetic foot problems and access to a team of specialists for preventing diabetic foot problems in the community (strength of evidence based on NICE criteria: strong).16 Special considerations may need to be made for those with disabilities, who are housebound, or who are living in care settings in order to ensure access to foot care assessment and treatment (not strong).16
To assess the risk of developing a diabetic foot problem, NICE has recommendations regarding the frequency of assessments, methods to assess the risk of developing diabetic foot problems, management of risks, and patient information about risks.16
Regarding frequency of assessment, NICE recommends that, basic foot care advice should be given to children (aged 12 years or younger) with diabetes as well as their family or care givers (strong).16 Further, foot assessment should be provided annually and information on foot care provided for those who are 12 to 17, and young people with diabetes-related foot problems should be referred for further care (strong).16 For adults with diabetes, the NICE guideline recommends assessing the risk of diabetic foot problems when diabetes is diagnosed, at least annually thereafter, when any foot problems occur, on any admission to hospital, and during changes in their status while hospitalized (strong).16
While assessing the risk of developing a diabetic foot problem, the NICE guideline states that it is important to remove shoes and socks, in order to determine risk factors including neuropathy limb ischemia, ulceration, callus, infection, inflammation, deformity, gangrene, or Charcot arthropathy (strong).16 They recommend stratifying the patient’s current risk of developing a diabetic foot problem as low, moderate, or high risk (strong).16
The NICE recommendations state that risks of developing diabetic foot problems should be managed. Annual assessments with an emphasis on foot care and advice regarding the disease progression should be given to individuals at low risks of developing diabetic foot problems, those with moderate or high risk of developing diabetic foot problems should be referred to foot protection services, and foot protection services should be initiated in a timely manner according to the risks (strong).16 Further, they recommend that those at low risk should be reassessed annually and those at moderate risk should be reassessed every three to six months (strong).16
Regarding patient information, NICE recommends that oral or written information should be provided when diabetes is diagnosed, during the assessments of patients’ feet, and if foot problems occur (strong).16 The information should outline basic foot care advice, the importance of foot care, signs of foot emergencies, who to contact in case of emergencies, footwear advice, the patients’ current risks of developing a foot problem, information about diabetes, and the importance of blood glucose control (strong).16
Limitations
There were several limitations to the review. Many related studies were excluded because they focused on patients with active symptoms or at moderate or high risks. There were relatively few studies on the preventive measures among patient with diabetes at low risks of developing ulceration or other foot problems. Due to some lack of clarity in reporting, while the populations in the primary studies included in the SR by Ahmad Sharoni et al. were patients with diabetes, presence or the risk of developing diabetic foot problems was not specified in all primary studies.15 Therefore, some of the included primary studies may have included those with symptomatic feet.
Conclusions and Implications for Decision or Policy Making
One SR of critically low quality by Ahmad Sharoni et al. and three evidence-based guidelines were identified.15–18 No relevant cost-effectiveness studies were identified. In the SR, a variety of foot care or education programs were assessed.15 Health education programs were different in design, setting, approach, outcome measures and results.15 Programs were related to an improvement in foot self-care scores and foot problems (such as neuropathy, foot disability, lesion, ulcer, tinea pedis and callus grade).15 After initial assessment of patients’ feet by professionals, subsequent follow-ups of the feet and evaluations were also significantly associated with better outcomes.15 The insurance status of the patients was not discussed.15
The guidelines by Diabetes Canada, NICE and the IWGDF recommend annual examination of the feet for foot problems among patients with diabetes.16–18 Both the NICE and the IWGDF guidelines recommend adequate education to improve self-care, risk stratification, and timely referral to specialist care.16,17 Moreover, the NICE guideline further specifies the types of specialists required for foot protection services, procedures to inspect the feet, timing for patient education, the frequencies to assess the risk of developing diabetic foot problems for children or adolescents.16 The IWGDF guideline recommends that patients protect their feet by avoiding certain activities, such as walking barefoot and wearing unfit footwear.17 Foot temperature monitoring is also recommended.17
In previous CADTH reports, the effectiveness of diabetic foot ulcer screening based on risk stratification was found to be effective to improve clinical outcomes7 and summary of nine evidence-based guidelines recommended the implementation of screening programs for diabetic foot ulcers that included assessment of risk (risk stratification), patient education, and referral to specialized care.8 There exist several guidelines for the prevention of diabetic foot problems identified in this or previous CADTH reports.5–8 The recommendations in various guidelines are established by different groups of professionals in separate settings. Preventative foot care strategies seem to be fairly widely recommended for people with diabetes.
References
- 1.
Diabetes Canada Clinical Practice Guidelines Expert Committee, Houlden
RL. 2018
Clinical practice guidelines: introduction.
Can J Diabetes. 2018;42:S1–S5. [
PubMed: 29650079]
- 2.
- 3.
- 4.
- 5.
- 6.
- 7.
- 8.
- 9.
- 10.
- 11.
- 12.
- 13.
- 14.
Liberati
A, Altman
DG, Tetzlaff
J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration.
J Clin Epidemiol. 2009;62(10):e1–e34. [
PubMed: 19631507]
- 15.
Ahmad Sharoni
SK, Minhat
HS, Mohd Zulkefli
NA, Baharom
A. Health education programmes to improve foot self-care practices and foot problems among older people with diabetes: a systematic review.
Int J Older People Nurs. 2016;11(3):214–239. [
PubMed: 26916809]
- 16.
- 17.
Schaper
NC, Van Netten
JJ, Apelqvist
J, Lipsky
BA, Bakker
K. Prevention and management of foot problems in diabetes: a summary guidance for daily practice 2015, based on the IWGDF guidance documents.
Diabetes Res Clin Pract. 2017;124:84–92. [
PubMed: 28119194]
- 18.
Embil
JM, Albalawi
Z, Bowering
K, Trepman
E. Foot care.
Can J Diabetes. 2018;42
Suppl 1:S222–s227. [
PubMed: 29650101]
- 19.
- 20.
Bus
SA, van Netten
JJ, Lavery
LA, et al. IWGDF guidance on the prevention of foot ulcers in at-risk patients with diabetes.
Diabetes Metab Res Rev. 2016;32
Suppl 1:16–24. [
PubMed: 26334001]
Appendix 1. Selection of Included Studies
Appendix 2. Characteristics of Included Publications
Table 2Characteristics of Included Systematic Reviews and Meta-Analyses
View in own window
| First Author, Publication Year, Country | Study Designs and Numbers of Primary Studies Included | Population Characteristics | Intervention and Comparator(s) | Clinical Outcomes, Length of Follow-Up |
|---|
| Ahmad Sharoni et al. 2016,15 Malaysia | N = 14, 4 RCTs, 3 non-randomized controlled trials, 6 non-randomized case series, 1 non-randomized study (details unspecified)
Publication date range from January 2000 to the recent year | 25 to 436 participants in the primary studies
The risk of diabetic foot not described
High-risk patients identified in 2 primary studies (Lincoln 2008, Calle-Pascual 2002)
Inclusion criteria:
- -
Older people with diabetes - -
Average age of 60 years or more
| Interventions:
- -
diabetes foot self-care education programs (N = 8) - -
general measures of diabetes self-care education programs, such as foot care aspect (N = 6) - -
theory-based tools: self-efficacy theories (N = 2), social cognitive theory (N = 1) and empowerment and discovery learning theories (N = 1)
Group-based (n = 9) or one-to-one approaches (n = 3); unknown (n = 2)
Health care (n = 9) or home (n = 3) or mixed settings (n = 2)
Follow-up: one month to three years
Inclusion criteria for interventions:
- -
“Educational programmes that included teaching, coaching, discussion, demonstration and assessment” - -
“programmes conducted by medical personnel (e.g. diabetic nurse educator, dietician, psychologist, occupational therapist, physician and/or podiatrist)”
Comparators not described in Comparators:
- -
Usual care (N = 4) - -
Written education (N = 1) - -
Not described in the primary study (specified by the review authors) (N = 1) - -
Not described by the review authors (N = 8)
| Primary outcome: “diabetes foot self-care (e.g. inspection, hygiene, appropriate socks and shoe, nail care, professional treatment)” (n = 12)
Secondary outcome: foot problems [e.g. neuropathy (n = 1), lesion, ulcer (n = 2), amputation, foot disability (n = 1), callus (n = 1), tinea pedis (n = 1)] and foot scores (n = 1) (p. 217) |
RCT = randomized controlled trial
Table 3Characteristics of Included Guidelines
View in own window
| Intended Users, Target Population | Intervention and Practice Considered | Major Outcomes Considered | Evidence Collection, Selection, and Synthesis | Evidence Quality Assessment | Recommendations Development and Evaluation | Guideline Validation |
|---|
| Diabetes Canada guideline in Embil et al. 201818 |
|---|
| Healthcare professionals in Canada, people with diabetes | Interventions or practices for the prevention and management of diabetic foot problems | “clinically relevant outcomes” (p. S6 in the Methods section, Chapter 2) | Major literature databases searched: MEDLINE, EMBASE, CINAHL, the Cochrane Central Register of Trials, and PsycINFO | A critical appraisal checklist in in the Methods section, Chapter 2 | “Expert Committee members evaluated the relevant literature, and guidelines were developed and initially reviewed by the Expert Committee. In the absence of new evidence since the publication of the 2013 Clinical Practice Guidelines, recommendations from the 2013 document were not changed” (p. S7 in the Methods section, Chapter 2) | Independent Methodological Review: 9 university-based clinician faculty with advanced training in research methods
External Peer Review: involving stakeholders and experts in relevant fields, including specialists, community primary care providers, academic departments of family medicine across Canada, and specialty and disease support organizations |
| International Group on the Diabetic Foot guideline in Schaper et al. 201717 |
|---|
Clinicians, patients with diabetes
Published by the International Working Group on the Diabetic Foot | Interventions for
- 1)
Prevention of foot ulcers in at-risk patients with diabetes - 2)
Footwear and offloading to prevent and heal foot ulcers in diabetes - 3)
Diagnosis, prognosis and management of peripheral artery disease in patients with foot ulcers in diabetes, - 4)
Diagnosis and management of foot infections in persons with diabetes, and - 5)
Interventions to enhance healing of chronic ulcers of the foot in diabetes
| Foot problems in persons with diabetes |
- -
Almost 80,000 studies detected by literature search - -
Review of the title and abstract - -
Studies fulfilling a minimal set of quality criteria (not described) were selected by the reviewers in the working groups - -
429 articles for complete quality analysis.
| Grading of Recommendations Assessment, Development and Evaluation (GRADE) | Not described | Not described |
| National Institute for Health and Care Excellence 201516 |
|---|
| Healthcare professionals, people with diabetes | Interventions or practices for the prevention and management of diabetic foot problems | “treatment objectives in the prevention, recognition, diagnosis, treatment and management of diabetic foot problems such as rates of ulceration, infection, complications and amputation rates” (p. 33) | Specific to the research questions, including clinical and economic studies
Major literature databases were searched. |
- -
Grading of Recommendations Assessment, Development and Evaluation (GRADE) for pairwise meta-analyses for interventional evidence - -
Modified GRADE for prognostic evidence - -
Modified GRADE for diagnostic evidence
| Not described | Not described |
GRADE = Grading of Recommendations Assessment, Development and Evaluation, UK = United Kingdom
Appendix 3. Critical Appraisal of Included Publications
Table 4Strengths and Limitations of Systematic Reviews and Meta-Analyses using AMSTAR 212
View in own window
| Strengths | Limitations |
|---|
| Ahmad Sharoni et al. 201615 |
|---|
- -
PICO criteria mentioned - -
Selection of study design explained - -
Comprehensive literature search with multiple databases - -
Included studies described in details - -
Risk of bias assessed with published tools
|
- -
PICO components unclear in some primary studies - -
Review protocol not published a priori - -
Study selection not in duplicate - -
Data extraction not in duplicate - -
List of excluded studies not provided - -
Funding sources of included studies not provided - -
No meta-analysis - -
Risk of bias not considered when interpreting the results - -
Heterogeneity not explained - -
Authors’ conflict of interest not declared
|
PICO = population, intervention, comparator, outcome
Table 5Strengths and Limitations of Guidelines using AGREE II13
View in own window
| Item | Guideline |
|---|
| Diabetes Canada guideline in Embil et al. 201818 | International Working Group on the Diabetic Foot guideline in Schaper et al. 201717 | National Institute for Health and Care Excellence 201516 |
|---|
| Domain 1: Scope and Purpose |
|---|
| 1. The overall objective(s) of the guideline is (are) specifically described. | Strongly agreed | Strongly agreed | Strongly agreed |
| 2. The health question(s) covered by the guideline is (are) specifically described. | Strongly agreed | Strongly agreed | Strongly agreed |
| 3. The population (patients, public, etc.) to whom the guideline is meant to apply is specifically described. | Strongly agreed | Strongly agreed | Strongly agreed |
| Domain 2: Stakeholder Involvement |
|---|
| 4. The guideline development group includes individuals from all relevant professional groups. | Strongly agreed | Strongly agreed | Strongly agreed |
| 5. The views and preferences of the target population (patients, public, etc.) have been sought. | Strongly agreed | Strongly disagreed | Strongly agreed |
| 6. The target users of the guideline are clearly defined. | Strongly agreed | Strongly agreed | Strongly agreed |
| Domain 3: Rigour of Development |
|---|
| 7. Systematic methods were used to search for evidence. | Strongly agreed | Partly agreed | Strongly agreed |
| 8. The criteria for selecting the evidence are clearly described. | Strongly disagreed | Strongly disagreed | Strongly agreed |
| 9. The strengths and limitations of the body of evidence are clearly described. | Agreed | Partly agreed | Strongly agreed |
| 10. The methods for formulating the recommendations are clearly described. | Strongly agreed | Disagreed | Strongly agreed |
| 11. The health benefits, side effects, and risks have been considered in formulating the recommendations. | Agreed | Strongly disagreed | Strongly agreed |
| 12. There is an explicit link between the recommendations and the supporting evidence. | Strongly agreed | Strongly agreed | Strongly agreed |
| 13. The guideline has been externally reviewed by experts prior to its publication. | Strongly agreed | Strongly disagreed | Strongly disagreed |
| 14. A procedure for updating the guideline is provided. | Strongly disagreed | Strongly disagreed | Strongly disagreed |
| Domain 4: Clarity of Presentation |
|---|
| 15. The recommendations are specific and unambiguous. | Strongly agreed | Strongly agreed | Strongly agreed |
| 16. The different options for management of the condition or health issue are clearly presented. | Strongly disagreed | Strongly agreed | Strongly agreed |
| 17. Key recommendations are easily identifiable. | Strongly agreed | Strongly agreed | Strongly agreed |
| Domain 5: Applicability |
|---|
| 18. The guideline describes facilitators and barriers to its application. | Strongly disagreed | Agreed | Strongly agreed |
| 19. The guideline provides advice and/or tools on how the recommendations can be put into practice. | Strongly disagreed | Partly agreed | Strongly agreed |
| 20. The potential resource implications of applying the recommendations have been considered. | Strongly disagreed | Strongly agreed | Strongly agreed |
| 21. The guideline presents monitoring and/or auditing criteria. | Strongly disagreed | Strongly disagreed | Strongly disagreed |
| Domain 6: Editorial Independence |
|---|
| 22. The views of the funding body have not influenced the content of the guideline. | Strongly agreed | Strongly disagreed | Strongly disagreed |
| 23. Competing interests of guideline development group members have been recorded and addressed. | Strongly agreed | Strongly disagreed | Strongly disagreed |
Appendix 4. Main Study Findings and Authors’ Conclusions
Table 6Summary of Findings Included Systematic Reviews and Meta-Analyses
View in own window
| Main Study Findings | Authors’ Conclusion |
|---|
| Ahmad Sharoni et al. 201615 |
|---|
- -
Neuropathy and ulcers: improvement in both foot self-care scores and reduced incidence (Chen et al., 2011; Calle-Pascual et al., 2002) - -
Foot self-care score: improvement identified in 9 studies, but no major impact on other outcomes (Dettori et al., 2005; Deakin et al., 2006; Borges & Ostwald, 2008; Lincoln et al., 2008; Ko et al., 2011; Saleh et al., 2012; Tang et al., 2012; Williams et al., 2014; Aikens et al., 2015) - -
Incidence of foot problems: “lower foot score (Baba et al., 2015), lower foot disability score, treatment session and lesion (Waxman et al., 2003) and reduction in the severity of tinea pedis and callus (Fujiwara et al., 2011)” (p. 235) - -
Summary: ‘all education programmes implemented by the previous researchers showed improvements in foot self-care and foot problems among the older people with diabetes” (p. 235)
|
- -
“Health education programmes varied according to their design, setting, approach, outcome measured and results.” - -
“Foot assessment, verbal and written instructions and discussion were proved to improve the foot self-care and foot problems” - -
“Subsequent follow-ups and evaluations had a significant effect - -
“An improvement was observed in foot self-care scores and foot problems (such as neuropathy, foot disability, lesion, ulcer, tinea pedis and callus grade) after implementation of the health education programme.” (p. 214)
|
Table 7Summary of Recommendations in Included Guidelines
View in own window
| Recommendations | Strength of Evidence and Recommendations |
|---|
| Diabetes Canada guideline in Embil et al. 201818 |
|---|
| Only recommendations about the prevention of diabetic foot problems listed here | |
- -
“Health-care providers should perform foot examinations to identify people with diabetes at risk for ulcers and lower-extremity amputation”
|
- -
Grade C, Level 3 according to classification rules in in the Methods section, Chapter 2
|
- -
Foot examination at least annually and at more frequent intervals in high-risk people
|
- -
Grade D, Level 4
|
- -
Foot examination “should include assessment for neuropathy, skin changes (e.g. calluses, ulcers, infection), peripheral arterial disease (e.g. pedal pulses and skin temperature) and structural abnormalities (e.g. range of motion of ankles and toe joints, bony deformities)” (p. S2250)
| - -
Grade D, Level 4
|
| International Working Group on the Diabetic Foot guideline in Schaper et al. 201717 |
|---|
| This is a summary of the evidence-based guideline published by the International Working Group on the Diabetic Foot (IWGDF). See the list of recommendations for the prevention of foot ulcers in at-risk patients with diabetes in Bus et al.20 | |
- -
“To identify a person with diabetes at risk for foot ulceration, examine the feet annually to seek evidence for signs or symptoms of peripheral neuropathy and peripheral artery disease”
| - -
GRADE strength of recommendation: strong; Quality of evidence: low
|
- -
“In a person with diabetes who has peripheral neuropathy, screen for a history of foot ulceration or lower-extremity amputation, peripheral artery disease, foot deformity, pre-ulcerative signs on the foot, poor foot hygiene and ill-fitting or inadequate footwear”
| - -
Strong; Low
|
- -
“Treat any pre-ulcerative sign on the foot of a patient with diabetes. This includes removing callus, protecting blisters and draining when necessary, treating ingrown or thickened toe nails, treating haemorrhage when necessary and prescribing antifungal treatment for fungal infections”
| - -
Strong; Low
|
- -
“To protect their feet, instruct an at-risk patient with diabetes not to walk barefoot, in socks only, or in thin-soled standard slippers, whether at home or when outside”
| - -
Strong; Low
|
- -
“Instruct an at-risk patient with diabetes to daily inspect their feet and the inside of their shoes, daily wash their feet (with careful drying particularly between the toes), avoid using chemical agents or plasters to remove callus or corns, use emollients to lubricate dry skin and cut toe nails straight across”
| - -
Weak; Low
|
- -
“To prevent a recurrent plantar foot ulcer in an at-risk patient with diabetes, prescribe therapeutic footwear that has a demonstrated plantar pressure-relieving effect during walking (i.e. 30% relief compared with plantar pressure in standard of care therapeutic footwear) and encourage the patient to wear this footwear”
| - -
Strong; Moderate
|
- -
“To prevent a first foot ulcer in an at-risk patient with diabetes, provide education aimed at improving foot care knowledge and behaviour, as well as encouraging the patient to adhere to this foot care advice”
| - -
Weak; Low
|
- -
“Instruct a high-risk patient with diabetes to monitor foot skin temperature at home to prevent a first or recurrent plantar foot ulcer. This aims at identifying the early signs of inflammation, followed by action taken by the patient and care provider to resolve the cause of inflammation”
| - -
Weak; Moderate
|
- -
“Do not use a nerve decompression procedure in an effort to prevent a foot ulcer in an at-risk patient with diabetes, in preference to accepted standards of quality care” (p. 16 to 17 in Bus et al.20)
| - -
Weak; Low
|
| National Institute for Health and Care Excellence 201516 |
|---|
| Only recommendations about the prevention of diabetic foot problems listed here | |
Care across all settings
- -
“A foot protection service for preventing diabetic foot problems, and for treating and managing diabetic foot problems in the community” (recommendation 8)
|
- -
Recommendation 8: strong, based on the wording according to the wording guidance on page 12
|
- -
“The foot protection service should be led by a podiatrist with specialist training in diabetic foot problems, and should have access to healthcare professionals with skills in the following areas:” diabetology, biomechanics and orthoses, and wound care. (recommendation 5)”
| - -
Recommendation 5: strong
|
- -
“Healthcare professionals may need to discuss, agree and make special arrangements for disabled people and people who are housebound or living in care settings, to ensure equality of access to foot care assessments and treatments for people with diabetes. (recommendation 11)”
| - -
Recommendation 11: not strong
|
Assessing the risk of developing a diabetic foot problem
Frequency of assessments | |
- -
Children with diabetes who are under 12 years: “give them, and their family members or carers (as appropriate), basic foot care advice. (recommendation 17)”
| - -
Recommendation 17: strong
|
- -
Young people with diabetes aged 12 to 17 years: “the paediatric care team or the transitional care team should assess the young person’s feet as part of their annual assessment, and provide information about foot care. If a diabetic foot problem is found or suspected, the paediatric care team or the transitional care team should refer the young person to an appropriate specialist. (recommendation 18)”
| - -
Recommendation 18: strong
|
- -
Adults with diabetes: “assess their risk of developing a diabetic foot problem at the following times: When diabetes is diagnosed, and at least annually thereafter (see recommendation 20). If any foot problems arise. On any admission to hospital, and if there is any change in their status while they are in hospital. (recommendation 19)”
| - -
Recommendation 20: strong - -
Recommendation 19: strong
|
Assessing the risk of developing a diabetic foot problem
- -
“When examining the feet of a person with diabetes, remove their shoes, socks, bandages and dressings, and examine both feet for evidence of the following risk factors:” neuropathy, limb ischaemia, ulceration, callus, infection and/or inflammation, deformity, gangrene and Charcot arthropathy. (recommendation 13)”
|
- -
Recommendation 13: strong
|
- -
Risk stratification into low, moderate and high risks: “Assess the person’s current risk of developing a diabetic foot problem or needing an amputation” (recommendation 15)
| - -
Recommendation 15: strong
|
Managing the risk of developing a diabetic foot problem
- -
People at low risk of developing a diabetic foot problem: “continue to carry out annual foot assessments, emphasise the importance of foot care, and advise them that they could progress to moderate or high risk. (recommendation 16)”
|
- -
Recommendation 16: strong
|
- -
People who are at moderate or high risk of developing a diabetic foot problem: refer to the foot protection service (recommendation 9)
| - -
Recommendation 9: strong
|
- -
Initial assessment by foot protection service: within 2 to 4 weeks for people who are at high risk of developing a diabetic foot problem, within 6 to 8 weeks for people who are at moderate risk (recommendation 10)
| - -
Recommendation 10: strong
|
- -
Reassessment intervals: annually for people who are at low risk, frequently (for example, every 3 to 6 months) for people who are at moderate risk, more frequently (for example, every 1 to 2 months) for people who are at high risk, if there is no immediate concern, very frequently (for example, every 1 to 2 weeks) for people who are at high risk, if there is immediate concern. “Consider more frequent reassessments for people who are at moderate or high risk, and for people who are unable to check their own feet.” (recommendation 20)”
| - -
Recommendation 20: not strong
|
Patient information about the risk of developing a diabetic foot problem
- -
“Provide information and clear explanations to people with diabetes and/or their family members or carers (as appropriate) when diabetes is diagnosed, during assessments, and if problems arise. Information should be oral and written” including: basic foot care advice and the importance of foot care, foot emergencies and who to contact, footwear advice, the person’s current individual risk of developing a foot problem, information about diabetes and the importance of blood glucose control (see recommendation 23). (recommendation 22)
|
- -
Recommendation 22: strong
|
- -
Guidance on education programmes and information about diabetes: “see the education and information section in ‘Type 1 diabetes in adults: diagnosis and management’ (NICE guideline NG17), the patient education section in ‘Type 2 diabetes in adults: management and the sections education and information for children and young people with type 1 diabetes and education and information for children and young people with type 2 diabetes in ‘Diabetes (type 1 and type 2) in children and young people: diagnosis and management’ (NICE guideline NG18)” (recommendation 23) (p. 20 to 27)
| - -
Recommendation 23: not strong
|
IWGDF = the International Working Group on the Diabetic Foot, NICE = National Institute for Health and Care Excellence
Appendix 5. Additional References of Potential Interest
Reviews of economic studies
Chow
I, Lemos
EV, Einarson
TR. Management and prevention of diabetic foot ulcers and infections: a health economic review.
PharmacoEconomics. 2008;26(12):1019–1035. [
PubMed: 19014203]
Narrative reviews
Morey-Vargas
OL, Smith
SA. BE SMART: strategies for foot care and prevention of foot complications in patients with diabetes.
Prosthet Orthotics Int. 2015;39(1):48–60. [
PubMed: 25614501]
About the Series
CADTH Rapid Response Report: Summary with Critical Appraisal
Funding: CADTH receives funding from Canada’s federal, provincial, and territorial governments, with the exception of Quebec.
Suggested citation:
Preventative foot care for patients with diabetes: a review of clinical effectiveness, cost-effectiveness, and guidelines. Ottawa: CADTH; 2018 Nov. (CADTH rapid response report: summary with critical appraisal).
Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services.
While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. The views and opinions of third parties published in this document do not necessarily state or reflect those of CADTH.
CADTH is not responsible for any errors, omissions, injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the contents of this document or any of the source materials.
This document may contain links to third-party websites. CADTH does not have control over the content of such sites. Use of third-party sites is governed by the third-party website owners’ own terms and conditions set out for such sites. CADTH does not make any guarantee with respect to any information contained on such third-party sites and CADTH is not responsible for any injury, loss, or damage suffered as a result of using such third-party sites. CADTH has no responsibility for the collection, use, and disclosure of personal information by third-party sites.
Subject to the aforementioned limitations, the views expressed herein are those of CADTH and do not necessarily represent the views of Canada’s federal, provincial, or territorial governments or any third party supplier of information.
This document is prepared and intended for use in the context of the Canadian health care system. The use of this document outside of Canada is done so at the user’s own risk.
This disclaimer and any questions or matters of any nature arising from or relating to the content or use (or misuse) of this document will be governed by and interpreted in accordance with the laws of the Province of Ontario and the laws of Canada applicable therein, and all proceedings shall be subject to the exclusive jurisdiction of the courts of the Province of Ontario, Canada.