1. Introduction
Removal of hair from the intended site of surgical incision has traditionally been part of the routine preoperative preparation of patients undergoing surgery. Hair removal may be necessary to facilitate adequate exposure to the site and preoperative skin marking. Furthermore, suturing and the application of wound dressings can be complicated by the presence of hair. Apart from these practical issues, hair has been associated with a lack of cleanliness and the potential to cause surgical site infection (SSI). However, there is also the belief that hair removal inversely increases the risk of SSI by causing microscopic trauma of the skin. To minimize the potential of skin trauma, the use of clippers instead of razors has been proposed for preoperative hair removal. Clippers cut the hair close to the skin without actually touching it, whereas razors involve a sharp blade drawn directly over the skin. A third method for hair removal is the application of depilatory creams containing chemicals. The drawbacks are the necessity to leave the cream in place for approximately 15–20 minutes for the hair to be dissolved and the potential for allergic reactions. A Cochrane review, published in 2009 and updated in 2011, concluded that there was no statistically significant effect on SSI rates of hair removal1. However, a significant harm was seen when hair removal with razors was compared with clipping.
2. PICO questions
Does hair removal affect the incidence of SSI?
What method and timing of hair removal is associated with the reduction of SSI?
Population: adult patients undergoing any type of surgical procedure
Intervention: avoidance of hair removal
Comparator: hair removal (different methods and timing)
Outcomes: SSI, SSI-attributable mortality
3. Methods
The following databases were searched: Medline (PubMed); Excerpta Medica Database (EMBASE); Cumulative Index to Nursing and Allied Health Literature (CINAHL); Cochrane Central Register of Controlled Trials (CENTRAL); and WHO regional medical databases.
The time limit for the review was between 1 January 1900 and 17 January 2014. Of note, the usual time limit of 1990 for the systematic reviews conducted for the WHO SSI prevention guidelines was extended to include important relevant literature published prior to this date. Language was restricted to English, French and Spanish. A comprehensive list of search terms was used, including Medical Subject Headings (MeSH) (Appendix 1).
Two independent reviewers screened titles and abstracts of retrieved references for potentially relevant studies. The full text of all potentially eligible articles was obtained. Two authors independently reviewed the full-text articles for eligibility based on inclusion criteria. Duplicate studies were excluded.
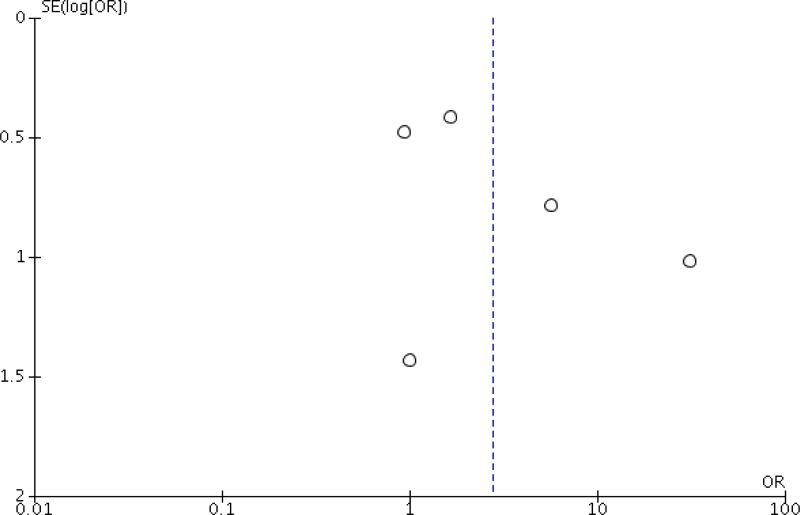
Two authors extracted data in a predefined evidence table (Appendix 2) and critically appraised the retrieved studies using the Cochrane collaboration tool2 for assessing risk of bias (Appendix 3). Any disagreements were resolved through discussion or after consultation with the senior author, when necessary. Publication bias was assessed using a funnel plot3.
Meta-analyses of available comparisons related to hair removal or not and the different methods used were performed using Review Manager v5.3 as appropriate4 (Appendix 4). Odds ratios (OR) and mean differences with 95% confidence intervals (CI) were extracted and pooled for each comparison with a random effects model. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) methodology (GRADE Pro software, http://gradepro.org/)5,6 was used to assess the quality of the body of retrieved evidence (Appendix 5).
4. Study selection
Flow chart of the study selection process
5. Summary of the findings
Overall, 15 randomized or quasi-randomized trials7–21 comparing the effect of preoperative hair removal vs. no hair removal or different methods of hair removal (shaving, clipping and depilatory cream) were identified as relevant to the research question. Any kind of surgical procedure was included. As no hair removal and clipping are similar in terms of reduced potential to cause microscopic skin trauma, an additional analysis was performed combining these two comparisons. Based on these considerations, we were able to make the following comparisons:
Hair removal vs. no hair removal
Shaving vs. no hair removal
Clipping vs. no hair removal
Depilatory cream vs. no hair removal
Comparisons of methods of hair removal
Clipping vs. shaving
Shaving vs. depilatory cream
Clipping and no hair removal vs. shaving
Timing of hair removal
Night before vs. day of surgery
The results of the meta-analyses based on these comparisons are as follows (Appendix 4).
Hair removal vs. no hair removal
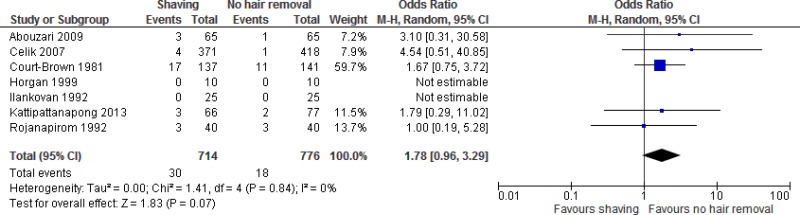
Seven studies
7,11,12,15–17,19 comparing shaving vs. no hair removal were identified. Meta-analysis of these studies showed that shaving had neither benefit nor harm when compared to no hair removal (OR: 1.78; 95% CI: 0.96–3.29).
The quality of evidence for this comparison was low (
Appendix 5).
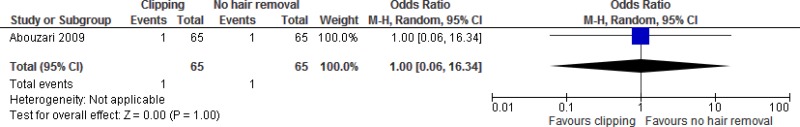
One study
7 comparing clippers vs. no hair removal was identified. This study showed that hair removal with clippers had neither benefit nor harm when compared to no hair removal (OR: 1.00; 95% CI: 0.06–16.34).
The quality of evidence for this comparison was very low (
Appendix 5).
One study
12 comparing depilatory cream vs. no hair removal was identified. This study showed that hair removal with depilatory cream had neither benefit nor harm when compared to no hair removal (OR: 1.02; 95% CI: 0.42–2.49). The quality of evidence for this comparison was very low (
Appendix 5).
Comparisons of methods of hair removal
Four studies
7,9,10,14 comparing clipping vs. shaving were identified. Meta-analysis of these studies showed a significantly lower risk of SSI following hair removal with clippers compared to shaving (OR: 0.51; 95% CI: 0.29–0.91).
The quality of evidence for this comparison was low (
Appendix 5).
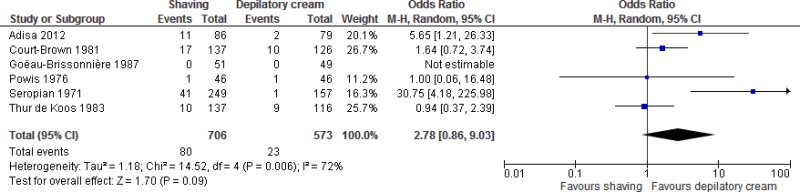
Six studies
8,12,13,18,20,21 comparing shaving vs. depilatory cream were identified. Meta-analysis of these studies showed neither benefit nor harm when shaving was compared to hair removal with depilatory cream (OR: 2.78; 95% CI: 0.86–9.03).
The quality of evidence for this comparison was very low (
Appendix 5).
Ten studies
7,9–12,14–17,19 comparing clipping or no hair removal vs. shaving were identified. Meta-analysis of these studies showed a significantly lower risk of SSI following hair removal with clippers or no hair removal compared to shaving (OR: 0.51; 95% CI: 0.34–0.78).
The quality of evidence for this comparison was moderate (
Appendix 5).
Timing of hair removal
One study
9 comparing hair removal the night before surgery vs. hair removal on the day of surgery by either shaving or clipping was identified. The study showed that hair removal on the night before surgery had neither benefit nor harm when compared to hair removal on the day of surgery (OR: 1.22; 95% CI: 0.44–3.42).
The quality of evidence for this comparison was very low (
Appendix 5).
In conclusion the retrieved evidence can be summarized as follows:
View in own window
| Comparison no. | Subgroup | Summary results |
|---|
| 1. | a | Overall, a low quality of evidence shows that shaving, clipping or the use of depilatory cream has neither benefit nor harm when compared to no hair removal in reducing the risk of SSI. |
| b | Overall, a very low quality of evidence shows that clipping has neither benefit nor harm when compared to no hair removal in reducing the risk of SSI. |
| c | Overall, a very low quality of evidence shows that the use of depilatory cream has neither benefit nor harm when compared to no hair removal in reducing the risk of SSI. |
| 2. | a | Overall, a low quality of evidence shows that clipping has a significant benefit in reducing the risk of SSI when compared to shaving. |
| b | Overall, a very low quality of evidence shows that depilatory cream has neither benefit nor harm when compared to shaving in reducing the risk of SSI. |
| c | Overall, a moderate quality of evidence shows that clipping or no hair removal has a significant benefit in reducing the risk of SSI when compared to shaving. |
| 3. | a | Overall, a very low quality of evidence shows that the timing of hair removal on the night before surgery has neither benefit nor harm when compared to the day of surgery in reducing the risk of SSI. |
6. Other factors considered in the review of studies
The systematic review team identified the following other factors to be considered.
Values and preferences
Ilankovan and colleagues studied patient and surgeon preferences regarding hair removal before maxillofacial surgery. They showed that patients prefer no hair removal over shaving, while the surgeon’s assessment of the difficulty of wound closure did not differ between the two methods16.
7. Key uncertainties and future research priorities
Available evidence is mostly underpowered and limited by flawed methodological design. Certain comparisons (depilatory cream vs. clipping) have not been made yet. Furthermore, the timing of hair removal and the location (ward or operating room [OR]) have not been sufficiently studied. Future well-designed and adequately-powered studies are needed to draw more firm conclusions.
Appendices
Appendix 1. Search terms
Medline
- 1.
surgical wound infection/ or (surgical site infection* or SSI or SSIs or surgical wound infection* or surgical infection* or post-operative wound infection* or postoperative wound infection*).ti,ab,kw.
- 2.
wound infection.mp. or exp wound infection/
- 3.
hair removal/ or (hair remov* or shaving or shave).ti,ab,kw.
- 4.
1 or 2
- 5.
3 and 4
- 8.
limit 5 to yr=“1900 -current”
EMBASE
esthetic surgery/ or (hair remov* or shaving or shave).ti,ab,kw.
surgical infection/ or (surgical site infection* or SSI or SSIs or surgical wound infection* or surgical infection* or post-operative wound infection* or postoperative wound infection*).ti,ab,kw.
exp wound infection/
2 or 3
1 and 4
limit 5 to yr=“1990 -current”
CINAHL
(MH “wound infection+”)
(MH “surgical wound infection”)
(“wound infection”)
(MH “hair removal”)
(“hair removal”)
1 or 2 or 3
4 or 5
6 and 7
Cochrane CENTRAL
wound infection:ti,ab,kw
surgical wound infection:ti,ab,kw
hair removal:ti,ab,kw
shaving:ti,ab,kw
1 or 2
3 or 4
5 and 6
WHO regional medical databases
(ssi)
(surgical site infection)
(surgical site infections)
(wound infection)
(wound infections)
(postoperative wound infection)
(hair removal)
(shaving)
African Index Medicus
infection [Key Word]
surgical [Key Word]
surgery [Key Word]
2 or 3
1 and 4
- ti:
title;
- ab:
abstract;
- kw:
key word.
Appendix 3. Risk of bias assessment of the included studies
View in own window
| Author, year | Sequence generation | Allocation concealment | Participants blinded | Care providers blinded | Outcome assessors blinded | Incomplete outcome data | Selective outcome reporting | Other sources of bias |
|---|
| Abouzari, 2009 7 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | Low risk | - |
| Adisa, 2011 8 | Low risk | Low risk | High risk | Low risk | Low risk | Low risk | Low risk | - |
| Alexander, 19839 | Low risk | Unclear | High risk | Unclear | Unclear | Low risk | Low risk | - |
| Balthazar, 1982 10 | Low risk | Unclear | High risk | Unclear | Unclear | Low risk | Low risk | - |
| Celik, 2007 11 | Low risk | Unclear | High risk | High risk | Unclear | High risk | Low risk | - |
| Court-Brown, 1981 12 | Unclear | Unclear | High risk | High risk | Unclear | Unclear | High risk | - |
| Goëau-Brissonnière, 1987 13 | Low risk | Unclear | High risk | High risk | Unclear | Unclear | Unclear | - |
| Grober, 2013 14 | Unclear | Unclear | Low risk | High risk | Unclear | Unclear | Low risk | - |
| Horgan, 1999 15 | Unclear | High risk | High risk | High risk | Unclear | Low risk | Low risk | - |
| Ilankovan, 1992 16 | Low risk | Unclear | Low risk | High risk | Unclear | Low risk | High risk | - |
| Kattipattanapong, 2012 17 | Low risk | Low risk | High risk | High risk | Unclear | Low risk | Low risk | - |
| Powis, 1976 18 | High risk | Unclear | High risk | Unclear | Low risk | Low risk | Low risk | - |
| Rojanapirom, 1992 19 | Unclear | Unclear | High risk | High risk | Unclear | Low risk | Low risk | - |
| Seropian, 1971 20 | High risk | Unclear | High risk | Unclear | Unclear | Low risk | High risk | - |
| Thur de Koos, 1983 21 | High risk | Unclear | High risk | Unclear | Unclear | Low risk | Unclear | - |
Appendix 4. Comparisons
Comparison 1. Hair removal vs. no hair removal
Comparison 2. Comparisons of methods of hair removal
Comparison 3. Timing of hair removal (hair removal the night before vs. day of surgery)
References
- 1.
Tanner
J, Norrie
P, Melen
K. Preoperative hair removal to reduce surgical site infection. Cochrane Database Systematic Rev. 2011:CD004122. [
PubMed: 22071812]
- 2.
Higgins
JP, Altman
DG, Gotzsche
PC, Jüni
P, Moher
D, Oxman
AD, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. [
PMC free article: PMC3196245] [
PubMed: 22008217]
- 3.
- 4.
The Nordic Cochrane Centre TCC. Review Manager (RevMan). Version 5.3. Copenhagen: The Cochrane Collaboration; 2014.
- 5.
GRADEpro guideline development tool. Summary of findings tables, health technology assessment and guidelines. GRADE Working Group, Ontario: McMaster University and Evidence Prime Inc.; 2015 (
http://www.gradepro.org, accessed 5 May 2016).
- 6.
Guyatt
G, Oxman
AD, Akl
EA, Kunz
R, Vist
G, Brozek
J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–94. [
PubMed: 21195583]
- 7.
Abouzari
M, Sodagari
N, Hasibi
M, Behzadi
M, Rashidi
A. Re: Nonshaved cranial surgery in black Africans: a short-term prospective preliminary study (Adeleye and Olowookere, Surg Neurol 2008;69–72) Effect of hair on surgical wound infection after cranial surgery: a 3-armed randomized clinical trial. Surg Neurol. 2009;71:261–2. [
PubMed: 18440617]
- 8.
Adisa
AO, Lawal
OO, Adejuyigbe
O. Evaluation of two methods of preoperative hair removal and their relationship to postoperative wound infection. J Infect Dev Ctries. 2011;5:717–22. [
PubMed: 21997940]
- 9.
Alexander
JW, Fischer
JE, Boyajian
M, Palmquist
J, Morris
MJ. The influence of hair-removal methods on wound infections. Arch Surg. 1983;118:347–52. [
PubMed: 6824435]
- 10.
Balthazar
ER, Colt
JD, Nichols
RL. Preoperative hair removal: a random prospective study of shaving versus clipping. South Med J
1982;75:799–801. [
PubMed: 7089645]
- 11.
Celik
SE, Kara
A. Does shaving the incision site increase the infection rate after spinal surgery?
Spine. 2007;32:1575–7. [
PubMed: 17621202]
- 12.
Court-Brown
C. Preoperative skin depilation and its effect on postoperative wound infections. J R Coll Surg Edinb. 1981;26:238–41. [
PubMed: 7021812]
- 13.
Goëau-Brissonnière
O, Coignard
S, Merao
AP, Haicault
G, Sasako
M, Patel
JC. [Preoperative skin preparation. A prospective study comparing a depilatory agent in shaving.] [Article in French] Presse Med. 1987;16:1517–9. [
PubMed: 2958817]
- 14.
Grober
ED, Domes
T, Fanipour
M, Copp
JE. Preoperative hair removal on the male genitalia: clippers vs. razors. J Sex Med. 2013;10:589–94. [
PubMed: 22908852]
- 15.
Horgan
MA, Kernan
JC, Schwartz
MS, Kellogg
JX, McMenomey
SO, Delashaw
JB. Shaveless brain surgery: safe, well tolerated, and cost effective. Skull Base Surg. 1999;9:253–8. [
PMC free article: PMC1656773] [
PubMed: 17171113]
- 16.
Ilankovan
V, Starr
DG. Preoperative shaving: patient and surgeon preferences and complications for the Gillies incision. J R Coll Surg Edinb. 1992;37:399–401. [
PubMed: 1283411]
- 17.
Kattipattanapong
W, Isaradisaikul
S, Hanprasertpong
C. Surgical site infections in ear surgery: hair removal effect; a preliminary, randomized trial study. Otolaryngol Head Neck Surg. 2013;148:469–74. [
PubMed: 23283828]
- 18.
- 19.
Rojanapirom
S, Danchaivijitr
S. Pre-operative shaving and wound infection in appendectomy. J Med Assoc Thai. 1992;75 (Suppl.2):20–3. [
PubMed: 1402495]
- 20.
Seropian
R, Reynolds
BM. Wound infections after preoperative depilatory versus razor preparation. Am. J Surg. 1971;121:251–4. [
PubMed: 5546329]
- 21.
Thur de Koos
P, McComas
B. Shaving versus skin depilatory cream for preoperative skin preparation. A prospective study of wound infection rates. Am J. Surg. 1983;145:377–8. [
PubMed: 6837864]