Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
CASRN: 7759-35-5
Drug Levels and Effects
Summary of Use during Lactation
Based on the available evidence, expert opinion in the United States holds that postpartum women who are breastfeeding should not use combined hormonal contraceptives during the first 3 weeks after delivery because of concerns about increased risk for venous thromboembolism and generally should not use combined hormonal contraceptives during the fourth week postpartum because of concerns about potential effects on breastfeeding performance. Postpartum breastfeeding women with other risk factors for venous thromboembolism generally should not use combined hormonal contraceptives until 6 weeks after delivery.[1,2] World Health Organization guidelines are more restrictive, stating that combined oral contraceptives should not be used in nursing mothers before 42 days postpartum and the disadvantages of using the method generally outweigh the advantages between 6 weeks and 6 months postpartum.[3] A decrease in milk supply can happen over the first few days of estrogen exposure.[4]
Drug Levels
Maternal Levels. Six postpartum women who were breastfeeding their infants were given subdermal implants containing 20 mg of segesterone acetate. Paired milk and plasma samples were obtained at about 2 weeks after insertion and at 10-day intervals for up to 2 additional times. Among 13 milk samples, the mean segesterone concentration was 37.5 ng/L (range 7 to 73 ng/L).[5]
Sixty-six postpartum women who were fully breastfeeding their infants were given subdermal implants containing 50 mg of segesterone acetate. A breastmilk sample was obtained at 75 days post-insertion from 24 of the women. The average milk level was 138 ng/L (range 73 to 237 ng/L).[6]
One hundred postpartum women who were fully breastfeeding their infants were given subdermal implants containing 80 mg of segesterone acetate at 55 to 60 days postpartum. The implants released about 100 mcg of segesterone acetate daily. Breastmilk samples were obtained from 14 of the women once weekly for the first month after implant insertion, then every 2 weeks until weaning. Milk segesterone levels ranged from 20 to 50 ng/L. The authors estimated that the dose transferred to the infant, assuming a daily intake of 800 mL of milk, was about 50 ng daily in the first month after insertion, decreasing to around 20 ng daily thereafter.[7]
Infant Levels. Sixty-six postpartum women who were fully breastfeeding their infants were given subdermal implants containing 50 mg of segesterone acetate. An infant blood sample was obtained at 75 days post-insertion from 25 of the infants. The average infant serum level was 7 ng/L (range <5 to 20 ng/L).[6]
Effects in Breastfed Infants
Relevant published information on segesterone acetate and ethinyl estradiol vaginal insert was not found as of the revision date. Studies on the use of segesterone acetate implants have found no adverse effects on growth and development.[6,7]
Effects on Lactation and Breastmilk
Relevant published information was not found as of the revision date.
Alternate Drugs to Consider
Etonogestrel, Intrauterine Copper Contraceptive, Oral Levonorgestrel, Intrauterine Levonorgestrel, Levonorgestrel Implant, Medroxyprogesterone Acetate, Norethindrone, Progesterone
References
- 1.
- Curtis KM, Tepper NK, Jatlaoui TC, et al. U.S. Medical Eligibility Criteria for Contraceptive Use, 2016. MMWR Recomm Rep 2016;65:1-103. [PubMed: 27467196]
- 2.
- Summary Chart of U.S. Medical Eligibility Criteria for Contraceptive Use. 2020. https://www
.cdc.gov/reproductivehealth /contraception /pdf/summary-chart-us-medical-eligibility-criteria_508tagged.pdf - 3.
- World Health Organization. Medical Eligibility Criteria For Contraceptive Use: Fifth Ed. 2015. http://www
.who.int/reproductivehealth /publications /family_planning/MEC-5/en/ [PubMed: 26447268] - 4.
- Moses-Kolko EL, Berga SL, Kalro B, et al. Transdermal estradiol for postpartum depression: A promising treatment option. Clin Obstet Gynecol 2009;52:516-29. [PMC free article: PMC2782667] [PubMed: 19661765]
- 5.
- Lähteenmäki PL, Díaz S, Miranda P, et al. Milk and plasma concentrations of the progestin ST-1435 in women treated parenterally with ST-1435. Contraception 1990;42:555-62. [PubMed: 2272183]
- 6.
- Coutinho EM, Athayde C, Dantas C, et al. Use of a single implant of elcometrine (ST-1435), a nonorally active progestin, as a long acting contraceptive for postpartum nursing women. Contraception 1999;59:115-22. [PubMed: 10361626]
- 7.
- Massai MR, Díaz S, Quinteros E, et al. Contraceptive efficacy and clinical performance of Nestorone implants in postpartum women. Contraception 2001;64:369-76. [PubMed: 11834236]
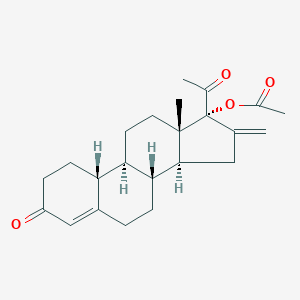
Substance Identification
Substance Name
CAS Registry Number
7759-35-5
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Medroxyprogesterone Acetate.[Drugs and Lactation Database (...]Review Medroxyprogesterone Acetate.. Drugs and Lactation Database (LactMed®). 2006
- Review Etonogestrel.[Drugs and Lactation Database (...]Review Etonogestrel.. Drugs and Lactation Database (LactMed®). 2006
- Review Contraceptives, Oral, Combined.[Drugs and Lactation Database (...]Review Contraceptives, Oral, Combined.. Drugs and Lactation Database (LactMed®). 2006
- Review Norethynodrel.[Drugs and Lactation Database (...]Review Norethynodrel.. Drugs and Lactation Database (LactMed®). 2006
- Review Intrauterine Levonorgestrel.[Drugs and Lactation Database (...]Review Intrauterine Levonorgestrel.. Drugs and Lactation Database (LactMed®). 2006
- Segesterone Acetate - Drugs and Lactation Database (LactMed®)Segesterone Acetate - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
