Context and Policy Issues
Cervicitis is a clinical syndrome characterized by the presence of a purulent or mucopurulent discharge that is visible in the endocervical canal or that can be detected with an endocervical smear.1–3 Additionally, other clinical signs of inflammation, such as persistent endocervical bleeding (intermenstrual or post-coital vaginal bleeding) which can be induced by the gentle passing of a cotton swab through the endocervix, can indicate cervicitis.1–3 One study reported that up to 40% of women assessed at a sexually transmitted disease clinic showed signs and symptoms of cervicitis, demonstrating the importance of improving treatment strategies for these women.4
Currently, it is common clinical practice to prescribe presumptive antibiotics for Chlamydia trachomatis and Neisseria gonorrhoea to patients with signs of cervicitis.1–3 However, fewer than one third of cervicitis cases are determined to be a result of Chlamydia trachomatis or Neisseria gonorrhoea infection following laboratory analysis.2,4,5 Other potential causes of cervicitis include Chlamydia trachomatis, Bacterial vaginosis, Mycoplasma genitalium, genital herpes, abnormality of vaginal flora, frequent douching, chemical irritants, or contraceptive methods.1,3–5 In addition to presumptive antibiotics being ineffective for treating some of these etiologies, there is growing concern that the overprescription of azithromycin, cephalosporins, and other antimicrobials may be leading to decreased susceptibility and increased resistance in bacterial strains found in Canada and the rest of the world.6,7
The purpose of this report is to summarize and critically appraise the evidence available regarding the treatment and management of cervicitis in non-pregnant women. This will include evidence on the comparative clinical effectiveness of doxycycline versus azithromycin for cervicitis caused by Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitalium and evidence on the clinical effectiveness of using a test-and-wait approach for the management of cervicitis of unknown etiology. As well, this report aims to review evidence-based guidelines regarding the the management and treatment of cervicitis in non-pregnant women.
Research Questions
What is the comparative clinical effectiveness of doxycycline versus azithromycin for the treatment of non-pregnant women with cervicitis caused by Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitalium?
What is the clinical effectiveness of using a test-and-wait approach for the management of non-pregnant women with diagnosed cervicitis?
What are the evidence-based guidelines regarding the management and treatment of cervicitis in non-pregnant women?
Key Findings
Evidence regarding the comparative clinical effectiveness of doxycycline versus azithromycin for the treatment of non-pregnant women with cervicitis caused by Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitalium suggested that azithromycin was more effective at achieving both microbiological and clinical cure.7 It is important to note that this evidence was limited to one non-randomized study.7
Regarding cervicitis treatment management strategies, evidence from one randomized controlled trial5 favoured using a test-and-wait approach over presumptive treatment in non-pregnant women with cervicitis of unknown etiology.
The evidence-based guidelines recommended azithromycin or doxycycline (alone or in combination with cephalosporins) for cervicitis of unknown etiology.1,3 One guideline1 stated that presumptive treatment for Chlamydia trachomatis and Neisseria gonorrhoea should be provided to women at high risk for these sexually transmitted infections. Alternatively, deferring treatment until results of diagnostic tests are available is an option for women at lower risk of sexually transmitted diseases.1
Methods
Literature Search Methods
A limited literature search was conducted on key resources including PubMed, The Cochrane Library, University of York Centre for Reviews and Dissemination (CRD) databases, Canadian and major international health technology agencies, as well as a focused Internet search. Methodological filters were applied to limit the retrieval to health technology assessments, systematic reviews, and meta analyses, randomized controlled trials, non-randomized studies, and guidelines. Where possible, retrieval was limited to the human population. The search was limited to English language documents published between January 1, 2012 and August 29, 2017.
Selection Criteria and Methods
One reviewer screened citations and selected studies. In the first level of screening, titles and abstracts were reviewed and potentially relevant articles were retrieved and assessed for inclusion. The final selection of full-text articles was based on the inclusion criteria presented in .
Exclusion Criteria
Articles were excluded if they did not meet the selection criteria outlined in , they were duplicate publications, or were published prior to 2012. Studies on the treatment and management of sexually transmitted infections (e.g., Neisseria gonorrhoeae, Chlamydia trachomatis, or Mycoplasma genitalium) without specific mention of cervicitis were excluded.
Critical Appraisal of Individual Studies
The included randomized controlled trial (RCT) and non-randomized study (NRS) were critically appraised using the Downs and Black checklist,8 and guidelines were assessed with the AGREE II instrument.9 Summary scores were not calculated for the included studies; rather, a review of the strengths and limitations of each included study were described.
Summary of Evidence
Quantity of Research Available
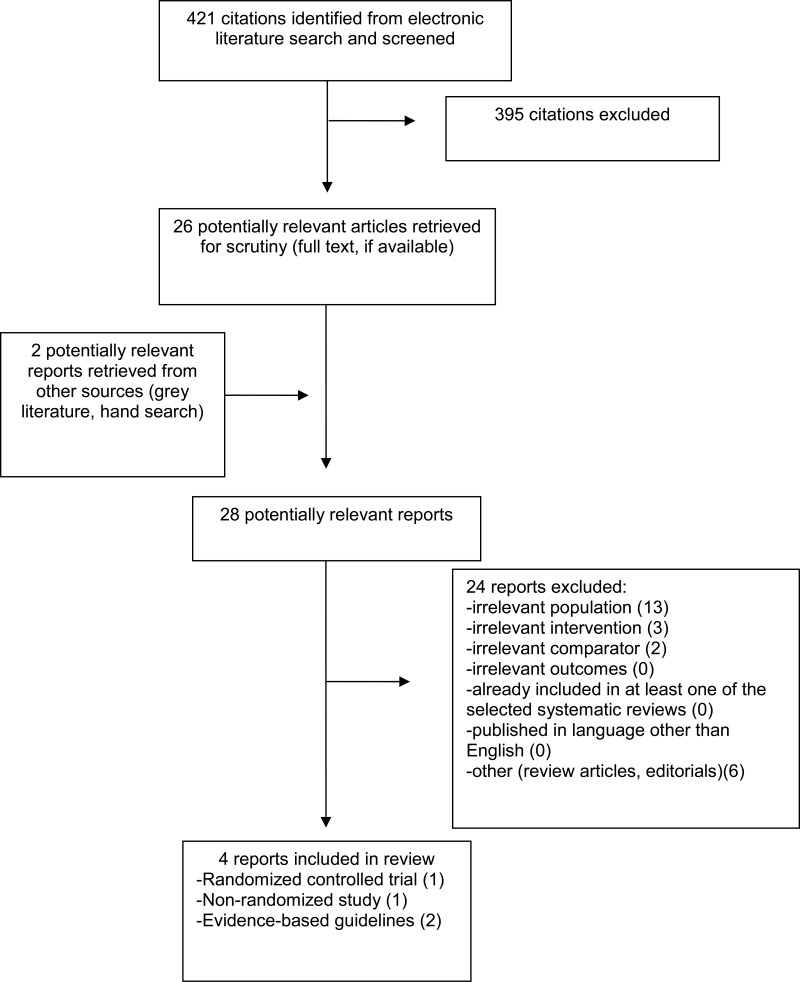
A total of 421 citations were identified in the literature search. Following screening of titles and abstracts, 395 citations were excluded and 26 potentially relevant reports from the electronic search were retrieved for full-text review. Two potentially relevant publications were retrieved from the grey literature search. Of these potentially relevant articles, 24 publications were excluded for various reasons, while four publications met the inclusion criteria and were included in this report. These four publications comprised one RCT,10 one NRS,7 and two evidence-based guidelines.1,11
Appendix 1 describes the PRISMA flowchart of the study selection.
Additional references of potential interest are provided in Appendix 5.
Summary of Study Characteristics
Additional details regarding the characteristics of included publications are provided in Appendix 2.
Study Design
One RCT,10 one NRS,7 and two evidence-based guidelines1,11 were eligible for inclusion in this review.
The included RCT5 appears to have been unblinded, and the NRS was a retrospective case-study.7
Year of Publication and Country of Origin
The RCT5 was published in 2016, and the NRS7 was published in 2013. The guidelines were published in 20173 and 2015.1
The RCT and the NRS were conducted in India and Sweden, respectively.5,7 The two guidelines were published in Canada3 and United States.1
Patient Population
The identified RCT5 included 200 women who presented with abnormal vaginal discharge caused by vaginitis or cervicitis. The patient age ranged between 18 years and 45 years.5
The NRS by Anagrius et al.7 included 407 patients (195 women) who tested positive for Mycoplasma genitalium infection detected with polymerase chain reaction. Cervicitis or urethritis was microbiologically confirmed in 98% of women treated with doxycycline, 91% of women treated with azithromycin 1 g, and 100% of the of women treated with azithromycin 1.5 g.7
The Centers for Disease Control and Prevention (CDC) guidelines1 and the National Institute for Excellence in Health and Social Services (INESSS) guidelines3 were published to inform the treatment of patients diagnosed with or who are at risk for sexually transmitted infections or diseases. These guidelines both included recommendations for patients with cervicitis of various etiologies.
Interventions and Comparators
The interventions of interest in the SR12 were antimicrobial therapies targeting Mycoplasma genitalium. These included doxycycline, azithromycin, tetracycline, erythromycin, metronidazole, levofloxacin, lymecycline, minocycline, spectinomycin, moxifloxacin, ofloxacin, rifalazil, cefoxitin, gatifloxacin, sitafloxacin, clarithromycin, pristinamycin, josamycin, and solithromycin.12 Primary studies compared these antimicrobials to each other or to the same drug at an alternative dosing strategy.12
In the RCT by Meena and Bansal,5 the intervention was laboratory identification of the causative organism (e.g., Neisseria gonorrhoeae, Chlamydia trachomatis, or Mycoplasma genitalium) followed by treatment only as necessary in women presenting with vaginitis or cervicitis. The comparator group was given syndromic management on the same day of examination based on symptoms and risk factors; patients with endocervical discharge or high risk factors were given azithromycin (2 g single dose) plus tinidazole (2 g single dose) plus fluconazole (150 mg single dose). Patients with only vaginal discharge were given tinidazole (2 g single dose) and fluconazole (150 mg).5
The NRS7 evaluated three treatment strategies for patients infected with Mycoplasma genitalium. These strategies utilized doxycycline (1 g) or azithromycin (at 1 g or 1.5 g). Patients who required a second-line treatment were given azithromycin 1.5 g (if doxycycline had failed) or moxifloxacin (if azithromycin had failed).7
The CDC guidelines1 included both pharmacological and nonpharmacological interventions for the prevention and treatment of sexually transmitted diseases. These included antimicrobial therapies, prevention counselling, vaccination, and contraceptive methods.
The INESSS guidelines3 contained pharmacological interventions for the management of clinical symptoms associated with sexually transmissible and blood-borne infections.
Outcomes
The RCT5 used the rate of complete cure of abnormal vaginal discharge at follow-up (two weeks after treatment initiation) as the primary outcome. The NRS6 assessed microbiological cure of Mycoplasma genitalium (confirmed with polymerase chain reaction) and clinical cure (absence of urethritis and/or cervicitis) at test of cure follow-up (four to 52 weeks after treatment initiation).
The outcomes of interest in the guidelines published by the CDC1 were microbiologic eradication, alleviation of signs and symptoms, cost-effectiveness, and prevention sequelae and transmission. The outcomes used in the INESSS guidelines3 were the successful management of symptoms and elimination of infection determined by test of cure.
Summary of Critical Appraisal
A summary of the critical appraisal of the included clinical studies, and evidence based guidelines are briefly described below. Details are available in Appendix 3, and .
Clinical Studies
The RCT5 was generally well-conducted but had some limitations, based on the assessment made using the Downs and Black checklist8. The authors used an appropriate method of randomization, described patient characteristics in sufficient detail, defined the objectives of the study, and all patients had the same time of follow-up and outcome assessment. Important limitations of this publication include a lack of blinding of patients and outcome assessors, the analysis did not address potential confounders, there was no mention of patients lost to follow-up, and there was an absence of explicit inclusion and exclusion criteria.
The included NRS7 was of moderate-to-low quality. The authors described the objective, intervention, main outcomes, and the inclusion and exclusion criteria. Because the study was based on a retrospective chart review, the trial design was likely representative of the patient population and care setting of interest. The nature of this study made it so that the randomization of patients and the blinding of patients and outcome assessors were not done. There was reference to a potential assignment of patients to various treatment groups based on risk factors present at initial assessment. This could have led to biased results that were not corrected for. A final major flaw in this study was the large variety in time of follow-up. This ranged between four weeks and 52 weeks and there does not appear to be any corrections in the data analysis to account for this variation.
Evidence-Based Guidelines
Both the CDC1 and INESSS3 guidelines were explicit in terms of scope and purpose, clarity of presentation, and consulted relevant clinical experts. Both guidelines conducted a systematic review to gather evidence to help formulate recommendations; however, the CDC guideline1 appears to have used only one electronic database (MEDLINE). The strength of the evidence appears to have been considered when drafting the recommendations. Conflicts of interest were declared in both guidelines. Prior to publication, both guidelines were externally reviewed by experts. Neither guideline appeared to include patient views and preference during their development nor made mention to a policy or plans for updating the guideline in future years as additional evidence becomes available. Overall, the identified guidelines were of fairly high quality.
Summary of Findings
The overall findings of the included literature are summarized below. A detailed summary of the main findings and recommendations are available in Appendix 4: and .
1. What is the comparative clinical effectiveness of doxycycline versus azithromycin for the treatment of non-pregnant women with cervicitis caused by Neisseria gonorrhoeae, Chlamydia trachomatis, and Mycoplasma genitalium?
Microbiologic Cure
One NRS7 assessed the outcome and microbiologic cure in non-pregnant women treated with either doxycycline or azithromycin for cervicitis. Included patients were diagnosed with cervicitis known to be a result of Mycoplasma genitalium infection. Microbiological cure rates of 47.5% (38/80), 96.2% (50/52), and 100% (12/12) were reported for women receiving 1.0 g doxycycline, 1.0 g azithromycin, and 1.5 g azithromycin, respectively.7 Based on the results of this study, it appears as if azithromycin was more effective than doxycycline for the eradication of Mycoplasma genitalium in this population.
Adverse Events
The NRS7 made no specific mention of adverse events related to the treatment of cervicitis with doxycycline or azithromycin. Therefore, no further comments can be made regarding the potential adverse effects of these treatment regimens.
2. What is the clinical effectiveness of using a test-and-wait approach for the management of non-pregnant women with diagnosed cervicitis?
Cure of Cervicitis and Vaginitis Symptoms
One RCT5 evaluated the cure of symptoms (cervicitis and vaginitis) outcome in non-pregnant women with cervicitis alone or cervicitis and vaginitis treated with either targeted management (i.e., diagnostic testing followed by treatment only as necessary) or syndromic management (i.e., empirical treatment). The study reported that targeted management was more effective in achieving symptom cure in both women with cervicitis and women with cervicitis and vaginitis.5 Although the data from this study would suggest that targeted management is superior for the treatment of women with cervicitis of unknown etiology, the results must be taken with caution due to the sample size (N=48).
Adverse Events
The identified RCT5 made no specific mention of adverse events related to treatment of cervicitis with targeted management or syndromic management. Therefore, no further comments can be made regarding the potential adverse effects of these treatment strategies.
3. What are the evidence-based guidelines regarding the management and treatment of cervicitis in non-pregnant women
Two evidence-based guidelines that qualify under the inclusion criteria for this research question were identified. The CDC guidelines1 included recommendations regarding the management and treatment of a large variety of STDs. The following recommendation was made specifically regarding cervicitis:
“Several factors should affect the decision to provide presumptive therapy for cervicitis. Presumptive treatment with antimicrobials for C. trachomatis and N. gonorrhoeae should be provided for women at increased risk (e.g., those aged <25 years and those with a new sex partner, a sex partner with concurrent partners, or a sex partner who has a sexually transmitted infection), especially if follow-up cannot be ensured or if testing with NAAT is not possible. Trichomoniasis and BV should also be treated if detected (see Bacterial Vaginosis and Trichomoniasis). For women at lower risk of STDs, deferring treatment until results of diagnostic tests are available is an option. If treatment is deferred and NAATs for C. trachomatis and N. gonorrhoeae are negative, a follow-up visit to see if the cervicitis has resolved can be considered.”1(p.54)
The guidelines published by INESSS3 included recommendations regarding the syndromic approach to treating various STBBIs. These guidelines recommended the following treatment regimens for patients (aged 14 or older) presenting with cervicitis:
1st choice: azithromycin 1 g p.o. in a single dose and either cefixime 800 mg p.o. in a single dose or ceftriaxone 250 mg IM in a single dose
2nd choice: doxycycline 100 mg p.o. b.i.d. for 7 days and either cefixime 800 mg p.o. in a single dose or ceftriaxone 250 mg IM in a single dose
For patients with a history of allergic reaction to cephalosporins or history of severe or very severe delayed or immediate reaction to penicillins: Azithromycin 2 g p.o. in a single dose
Limitations
A number of limitations were identified in the critical appraisals (Appendix 3), however, additional limitations exist. Overall, there was a limited amount of evidence which provided answers to our research questions. In addition, the studies which were identified were often of moderate quality and utilized sample sizes that ranged from 200 to 407 patients.
Of the primary studies included in the SR,12 one was relevant to this report. It, however, was difficult to examine as the authors’ analysis did not focus on non-pregnant women with cervicitis, receiving either doxycycline or azithromycinin.
Adverse events were not reported in the SR12, the RCT5, or the NRS.7 It is unclear if this is a result of a low occurrence of adverse events or if it is due to a lack of reporting.
Neither the SR nor any of the included clinical studies were conducted in Canada, hence may not be generalizable for the Canadian setting. This is especially problematic for antibiotic effectiveness questions due to the potential for regional differences in the prevalence of antimicrobial resistance.6
Conclusions and Implications for Decision or Policy Making
A total of five relevant publications, including one SR,12 one RCT,5 one NRS,7 and two evidence-based guidelines1,3 were identified.
Azithromycin was generally favoured over doxycycline as a treatment for non-pregnant women with cervicitis caused by Neisseria gonorrhoeae, Chlamydia trachomatis, or Mycoplasma genitalium. An exception to this was the CDC guidelines,1 where both azithromycin and doxycycline were presented as treatment options, with no preference given to one over the other. Policy-makers should be aware that neither of the primary studies cited supporting this statement were conducted in Canada,7,12 and regional differences in resistance to antimicrobial agents may vary.6
The use of a test-and-wait (followed by treatment as necessary) approach for the management of non-pregnant women with cervicitis of unknown etiology was favoured in the identified RCT.5 Patients with cervicitis who received targeted management had higher rates of both clinical and microbiological cure.5 This conclusion was echoed in the CDC guidelines,1 where a test-and-wait approach is suggested as an option for women at lower risk of STDs. The INESSS guidelines3 made no mention of using a test-and-wait approach, but recommended that appropriate laboratory analyses must be completed for patients with cervicitis, and that the choice of treatment can be reassessed when the results are available.
References
- 1.
- 2.
- 3.
- 4.
Taylor
SN. Cervicitis of unknown etiology. Curr Infect Dis Rep. 2014
Jun;16(7):409. [
PubMed: 24859465]
- 5.
Meena
V, Bansal
CL. Study to evaluate targeted management and syndromic management in women presenting with abnormal vaginal discharge. J Obstet Gynaecol India. 2016
Oct;66(Suppl 1):534–40. [
PMC free article: PMC5016465] [
PubMed: 27651658]
- 6.
- 7.
- 8.
- 9.
- 10.
Lusk
MJ, Garden
FL, Cumming
RG, Rawlinson
WD, Naing
ZW, Konecny
P. Cervicitis: a prospective observational study of empiric azithromycin treatment in women with cervicitis and non-specific cervicitis. Int J STD AIDS. 2017
Feb;28(2):120–6. [
PubMed: 26792283]
- 11.
Burnett
AM, Anderson
CP, Zwank
MD. Laboratory-confirmed gonorrhea and/or chlamydia rates in clinically diagnosed pelvic inflammatory disease and cervicitis. Am J Emerg Med. 2012
Sep;30(7):1114–7. [
PubMed: 22030186]
- 12.
Abbreviations
- b.i.d.
twice daily (from the Latin “bis in die”)
- CDC
Centers for Disease Control and Prevention
- DNA
deoxyribonucleic acid
- GRADE
Grading of Recommendations Assessment, Development and Evaluation
- IM
intramuscular
- INESSS
Institut national d’excellence en santé et en services
- NAAT
Nucleic Acid Amplification Test
- NR
not reported
- NRS
non-randomized study
- PCR
polymerase chain reaction
- p.o
orally, by mouth (from the Latin “per os”)
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- RCT
randomized controlled trial
- RNA
ribonucleic acid
- STBBI
sexually transmitted and blood-borne infection
- STD
sexually transmitted disease
Appendix 1. Selection of Included Studies
Appendix 2. Characteristics of Included Publications
Table A1Characteristics of Included Clinical Studies
View in own window
| First Author, Publication Year, Country | Study Design | Patient Characteristics | Intervention(s) | Comparator(s) | Clinical Outcomes, Length of Follow-up |
|---|
Meena and Bansal, 20165
India | RCT | Women (between 18 years and 45 years) who presented with abnormal vaginal discharge (vaginitis or mucopurulent cervicitis).
N = 200 | Laboratory identification of the causative organism followed by treatment only as necessary. Tinidazole (2 g single dose) was given for bacterial vaginosis and trichomoniasis, fluconazole (150 mg single dose) was given for candidiasis, and azithromycin (2 g single dose) was given for gonorrhoea and chlamydia. | Syndromic management on the same day of examination based on symptoms and risk factors. Patients with endocervical discharge or high risk factors were given azithromycin (2 g single dose) plus tinidazole (2 g single dose) plus fluconazole (150 mg single dose). Patients with only vaginal discharge were given tinidazole (2 g single dose) and fluconazole (150 mg). | Complete cure of abnormal vaginal discharge at follow-up (2 weeks). |
Anagrius et al., 20137
Sweden | Retrospective case-study | Men and women with a diagnosis of M. genitalium infection confirmed by PCR
N = 407 patients (195 women) | Doxycycline (1 g) | Azithromycin (1 g or 1.5 g) | Microbiological and clinical cure at test of cure follow-up (4 to 52 weeks after treatment initiation). |
PCR = polymerase chain reaction; RCT = randomized controlled trial
Table A2Characteristics of Included Guidelines
View in own window
| Objectives | Methodology |
|---|
| Target Population, Intended Users | Intervention and Practice Consideration | Major Outcomes Considered | Evidence Collection, Selection and Synthesis | Evidence Quality Assessment | Recommendations Development and Evaluation |
|---|
| CDC 20151 |
|---|
Target population:
Patients who have or who are at risk for sexually transmitted infections or diseases
Intended users:
Physicians and other health-care providers | Pharmacological and nonpharmacological interventions for the prevention and treatment sexually transmitted diseases | “These reviews also focused on four principal outcomes of STD therapy for each individual disease or infection: 1) treatment of infection based on microbiologic eradication; 2) alleviation of signs and symptoms; 3) prevention of sequelae; 4) prevention of transmission, including advantages such as cost-effectiveness and other advantages (e.g., single-dose formulations and directly observed therapy) and disadvantages (e.g., side effects) of specific regimens.”1 | “...a systematic literature review using an extensive MEDLINE database evidence-based approach (e.g., using published abstracts and peer-reviewed journal articles).”1 | Quality of retrieved articles was assessed; however, the methods used were not stated. | “The workgroup evaluated the quality of evidence, provided answers to the key questions, and rated the recommendations based on the United Services Preventive Services Task Forces (USPSTF) modified rating system.”1 |
| INESSS 20173 |
|---|
Target population:
Individuals aged 14 and over with signs or symptoms of STIBBIs
Intended users:
Physicians and other health-care providers | Pharmacological interventions for the management of clinical symptoms potentially associated with STBBIs | Management of symptoms and elimination of infection (determined by test of cure). | Evidence was collected from a systematic search in the MEDLINE and Embase databases, a grey literature search, and official antibiotic monographs (approved by Health Canada). | SRs were evaluated using the R-AMSTAR tool.
CPGs were evaluated using the AGREE II assessment tool | Expert consensus based on evidence from systematic reviews Stakeholders and public consultation; unclear if stakeholders were internal or external |
AGREE= Appraisal of Guidelines for Research and Evaluation; CDC = Centers for Disease Control and Prevention; CPG = clinical practice guideline; INESSS = Institut national d’excellence en santé et en services sociaux; R-AMSTAR = Revised Measurement Tool to Assess Systematic Reviews; SR = systematic review; STD = sexually transmitted disease; STIBBI = sexually transmitted and blood-borne infection; STI = sexually transmitted infection
Appendix 3. Critical Appraisal of Included Publications
Table A3Strengths and Limitations of Clinical Studies using Downs and Black Checklist
View in own window
| Strengths | Limitations |
|---|
| Meena and Bansal 20165 |
|---|
The objective of the study was stated and explained in detail Patients were allocated to treatment groups through computer-generated randomization Interventions of interest were clearly described Patient characteristics were described P-values were reported The authors mentioned that there were no conflicts of interest Study participants and care setting appear to be representative of the population and care setting of interest Time of follow-up was the same for all patients
|
The outcomes of interest were not stated until they were presented as results Inclusion and exclusion criteria were not explicitly stated Open-label, unblinded trial Confounders were not mentioned or adjusted for Unclear if sample size calculations were undertaken Unclear if there were any withdrawals or patients lost to follow-up Unclear if there were any adverse events resulting from the intervention
|
| Anagrius et al. 20137 |
|---|
The objectives and outcomes of the study were stated and explained in detail Inclusion and exclusion criteria were described in the methods section Interventions were defined and specific dosages were provided Due to the nature of the study (retrospective case-study), the patient population, staff, and care setting are likely relevant to those of interest The findings of the study are described The outcome measures appear to be valid and reliable
|
Time of follow-up (and test of cure assessment) was not standardized and varied between patients (ranged from 4 weeks to 52 weeks). Additionally, there was no mention of adjustment to correct for this variation Confounders were not mentioned or adjusted for Unclear if there were any adverse events resulting from the intervention The characteristics of patients lost to follow-up were not mentioned Because this is a retrospective case-study, there was no attempt at blinding patients or healthcare staff to the treatment given There was no randomization to intervention groups Patients were likely recruited into intervention groups during alternate time periods (doxycycline from 1998 to 2003 and azithromycin from 2003 to 2005) Patient recruitment into different intervention groups appears to have been risk factor based
|
Table A4Strengths and Limitations of Guidelines using AGREE II
View in own window
| Strengths | Limitations |
|---|
| Centers for Disease Control and Prevention 20151 |
|---|
Scope, purpose, and target population were stated Developed by CDC staff and an independent workgroup selected on the basis of their expertise in the clinical management of STDs All workgroup members disclosed potential conflicts of interest A systematic review was conducted using MEDLINE Recommendations were rated based on the United Services Preventive Services Task Forces modified rating system Strengths and limitations of the cited evidence were considered when drafting the recommendations The guideline was externally reviewed by a second independent panel of public health and clinical experts Recommendations were specific and easily identifiable
|
|
| National Institute for Excellence in Health and Social Services (INESSS) 20173 |
|---|
Scope, purpose, and target population were stated A systematic search was conducted using multiple databases (MEDLINE and Embase) as well as a grey literature search The experiential knowledge of Quebec experts and clinicians who collaborated in the project was consulted when writing recommendations The target users of the guideline were stated The methodology for selecting evidence, including inclusion and exclusion criteria, is well-defined Strengths and limitations of the cited evidence were considered when drafting the recommendations Recommendations were specific and easily identifiable The guideline was externally reviewed by experts prior to its publication Potential conflicts of interest of the authors were declared
|
|
Appendix 4. Main Study Findings and Author’s Conclusions
Table A5Summary of Findings of Included Primary Studies
View in own window
| Main Study Findings | Author’s Conclusion |
|---|
| Meena and Bansal 20165 |
|---|
This randomized controlled trial included a total of 200 women with vaginitis (n=145), cervicitis (n=37), or both (n=18). However, only the results relevant under the inclusion criteria of this report will be presented (women with cervicitis).
Comparison of targeted management (diagnostic testing followed by treatment only as necessary) vs. syndromic management (empirical treatment) for women with cervicitis
55 women with cervicitis or cervicitis and vaginitis were treated with either targeted management or syndromic management Of those that received targeted management (and had their cervicitis and vaginitis laboratory confirmed), 5/7(71.4%) of those with cervicitis and 10/14 (71.4%) of those with cervicitis and vaginitis were cured of their symptoms (p value <0.001) Of those that received syndromic management, 14/26 (54%) of those with cervicitis and 0/1 (0%) of those with cervicitis and vaginitis were cured of their symptoms (p value <0.001)
| “Response to treatment for vaginitis was 76.3 % in targeted management group, whereas it was 41 % in syndromic management group. With cervicitis, 71.4 % women responded to treatment in targeted group as compared to 54 % in syndromic management group. This difference was statistically significant. Low response to treatment in syndromic management group is due to low sensitivity of clinical examination in diagnosing the nature of vaginal discharge. Thus, in clinics where laboratory facilities are available, they should be used to confirm the diagnosis for targeted management.”5(p539) |
| Anagrius et al. 20137 |
|---|
This retrospective case-study included both men (n=212) and women (n=195) with a diagnosis of M. genitalium infection confirmed by PCR. However, only the results relevant under the inclusion criteria of this report will be presented (women with cervicitis).
Comparison of doxycycline vs. azithromycinin in women with cervicitis
180 women with a diagnosis of M. genitalium infection were treated with 1.0 g doxycline (n=102), 1.0 g azithromycin (n=62), or 1.5 g azithromycin (n=16). Microscopic signs of urethritis and/or cervicitis were observed in 98%, 91%, and 100% of these women at inclusion, respectively. These rates of urethritis and/or cervicitis decreased to 53%, 50%, and 30% for those microbiologically cured at follow-up Of those that received 1.0 g doxycycline, 38/80 (47.5%) had microbiologic cure at follow-up (22 patients were excluded) Of those that received 1.0 g azithromycin, 50/52 (96.2%) had microbiologic cure at follow-up (10 patients were excluded) Of those that received 1.5 g azithromycin, 12/12 (100%) had microbiologic cure at follow-up (4 patients were excluded)
| “Azithromycin 1 g single dose and 1.5 g extended dosage had a significantly higher microbiological cure-rates then doxycycline when all patients were compared (p,0.0001 for both). For men and women separately, all comparisons between doxycycline and azithromycin were also significantly in favour of azithromycin (p,0.0005). No statistically significant difference in the cure rates between the two azithromycin dosages when given as primary treatment could be found, to some extent due to the small number of patients given 1.5 g as the primary treatment.”7(pe61481)
“These findings confirm the results from other studies showing that doxycycline is inefficient in eradicating M. genitalium. Although azithromycin 1 g was not significantly less efficient than extended dosage, it was associated with selection of macrolide resistant M. genitalium strains and should not be used as first line therapy for M. genitalium. Monitoring of M. genitalium macrolide resistance should be encouraged.”7(pe61481) |
PCR = polymerase chain reaction
Table A6Summary Included Evidence-Based Guidelines
View in own window
| Guideline | Selected Recommendations |
|---|
| CDC 20151 - Sexually Transmitted Diseases Treatment Guidelines | “Several factors should affect the decision to provide presumptive therapy for cervicitis. Presumptive treatment with antimicrobials for C. trachomatis and N. gonorrhoeae should be provided for women at increased risk (e.g., those aged <25 years and those with a new sex partner, a sex partner with concurrent partners, or a sex partner who has a sexually transmitted infection), especially if follow-up cannot be ensured or if testing with NAAT is not possible. Trichomoniasis and BV should also be treated if detected (see Bacterial Vaginosis and Trichomoniasis). For women at lower risk of STDs, deferring treatment until results of diagnostic tests are available is an option. If treatment is deferred and NAATs for C. trachomatis and N. gonorrhoeae are negative, a follow-up visit to see if the cervicitis has resolved can be considered.”(p54) |
| INESSS 20173 - STBBI-Syndromic Approach | These guidelines recommend the following treatment regimens for patients (aged 14 or older) presenting with cervicitis:
1st choice: azithromycin 1 g p.o. in a single dose and either cefixime 800 mg p.o. in a single dose or ceftriaxone 250 mg IM in a single dose 2nd choice: doxycycline 100 mg p.o. b.i.d. for 7 days and either cefixime 800 mg p.o. in a single dose or ceftriaxone 250 mg IM in a single dose For patients with a history of allergic reaction to cephalosporins or history of severe or very severe delayed or immediate reaction to penicillins: Azithromycin 2 g p.o. in a single dose
|
b.i.d = twice daily (from the Latin “bis in die”); CDC = Centers for Disease Control and Prevention; CPG = clinical practice guideline; IM = intramuscular; INESSS = Institut national d’excellence en sante et en services sociaux; NAAT = Nucleic Acid Amplification Test; p.o. = orally, by mouth (from the Latin “per os”); STD = sexually transmitted disease
Appendix 5. Additional References of Potential Interest
Systematic Reviews and Meta-Analyses
Alternative Population
Horner
P, Ingle
SM, Garrett
F, Blee
K, Kong
F, Muir
P, et al. Which azithromycin regimen should be used for treating Mycoplasma genitalium? A meta-analysis. Sex Transm Infect. 2017
Jul
17.
PubMed: PM28717050 [
PubMed: 28717050]
Manhart
LE, Jensen
JS, Bradshaw
CS, Golden
MR, Martin
DH. Efficacy of antimicrobial therapy for Mycoplasma genitalium infections. Clin Infect Dis. 2015
Dec
15;61
Suppl 8:S802–S817.
PubMed: PM26602619 [
PubMed: 26602619]
Lau
A, Bradshaw
CS, Lewis
D, Fairley
CK, Chen
MY, Kong
FY, et al. The Efficacy of azithromycin for the treatment of genital Mycoplasma genitalium: a systematic review and meta-analysis. Clin Infect Dis. 2015
Nov
1;61(9):1389–99.
PubMed: PM26240201 [
PubMed: 26240201]
Kong
FY, et al. Azithromycin versus doxycycline for the treatment of genital chlamydia infection: a meta-analysis of randomised controlled trials. Clin Infect Dis; 2014
Jul
15;59(2):193–205.
PubMed: PM24729507 [
PubMed: 24729507]
Randomized Controlled Trials
Alternative Comparator
McCormick
DF, Rahman
M, Zadrozny
S, Alam
A, Ashraf
L, Neilsen
GA, et al. Prevention and control of sexually transmissible infections among hotel-based female sex workers in Dhaka, Bangladesh. Sex Health. 2013
Dec;10(6):478–86.
PubMed: PM24262217 [
PubMed: 24262217]
Alternative Population
Falk
L, Enger
M, Jensen
JS. Time to eradication of Mycoplasma genitalium after antibiotic treatment in men and women. J Antimicrob Chemother. 2015
Nov;70(11):3134–40.
PubMed: PM26283670 [
PubMed: 26283670]
Non-Randomized Studies
Alternative Comparator
Terada
M, Izumi
K, Ohki
E, Yamagishi
Y, Mikamo
H. Antimicrobial efficacies of several antibiotics against uterine cervicitis caused by Mycoplasma genitalium. J Infect Chemother. 2012
Jun;18(3):313–7.
PubMed: PM22020630 [
PubMed: 22020630]
Alternative Population
Schumacher
CM, Ghanem
KG. Retreatment rates for uncomplicated gonorrhea infection: comparing ceftriaxone and azithromycin versus ceftriaxone and doxycycline. Sex Transm Dis. 2013
Jul;40(7):539–45.
PubMed: PM23965767 [
PubMed: 23965767]
No Comparator
Lusk
MJ, Garden
FL, Cumming
RG, Rawlinson
WD, Naing
ZW, Konecny
P. Cervicitis: a prospective observational study of empiric azithromycin treatment in women with cervicitis and non-specific cervicitis. Int J STD AIDS. 2017
Feb;28(2):120–6.
PubMed: PM 26792283 [
PubMed: 26792283]
Review Articles
Jensen
JS, Cusini
M, Gomberg
M, Moi
H. Background review for the 2016 European guideline on Mycoplasma genitalium infections. J Eur Acad Dermatol Venereol. 2016
Oct;30(10):1686–93.
PubMed: PM 27605499 [
PubMed: 27605499]
Manhart
LE, Jensen
JS, Bradshaw
CS, Golden
MR, Martin
DH. Efficacy of antimicrobial therapy for Mycoplasma genitalium infections. Clin Infect Dis. 2015
Dec
15;61
Suppl 8:S802–S817.
PubMed: PM 26602619 [
PubMed: 26602619]
About the Series
CADTH Rapid Response Report: Summary with Critical Appraisal
Suggested citation:
Management and treatment of cervicitis: a review of clinical effectiveness and guidelines. Ottawa: CADTH; 2017 Sep. (CADTH rapid response report: summary with critical appraisal).
Disclaimer: The information in this document is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. While patients and others may access this document, the document is made available for informational purposes only and no representations or warranties are made with respect to its fitness for any particular purpose. The information in this document should not be used as a substitute for professional medical advice or as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process. The Canadian Agency for Drugs and Technologies in Health (CADTH) does not endorse any information, drugs, therapies, treatments, products, processes, or services.
While care has been taken to ensure that the information prepared by CADTH in this document is accurate, complete, and up-to-date as at the applicable date the material was first published by CADTH, CADTH does not make any guarantees to that effect. CADTH does not guarantee and is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in any third-party materials used in preparing this document. The views and opinions of third parties published in this document do not necessarily state or reflect those of CADTH.
CADTH is not responsible for any errors, omissions, injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the contents of this document or any of the source materials.
This document may contain links to third-party websites. CADTH does not have control over the content of such sites. Use of third-party sites is governed by the third-party website owners’ own terms and conditions set out for such sites. CADTH does not make any guarantee with respect to any information contained on such third-party sites and CADTH is not responsible for any injury, loss, or damage suffered as a result of using such third-party sites. CADTH has no responsibility for the collection, use, and disclosure of personal information by third-party sites.
Subject to the aforementioned limitations, the views expressed herein are those of CADTH and do not necessarily represent the views of Canada’s federal, provincial, or territorial governments or any third party supplier of information.
This document is prepared and intended for use in the context of the Canadian health care system. The use of this document outside of Canada is done so at the user’s own risk.
This disclaimer and any questions or matters of any nature arising from or relating to the content or use (or misuse) of this document will be governed by and interpreted in accordance with the laws of the Province of Ontario and the laws of Canada applicable therein, and all proceedings shall be subject to the exclusive jurisdiction of the courts of the Province of Ontario, Canada.