Attribution Statement: LactMed is a registered trademark of the U.S. Department of Health and Human Services.
NCBI Bookshelf. A service of the National Library of Medicine, National Institutes of Health.
Drugs and Lactation Database (LactMed®) [Internet]. Bethesda (MD): National Institute of Child Health and Human Development; 2006-.
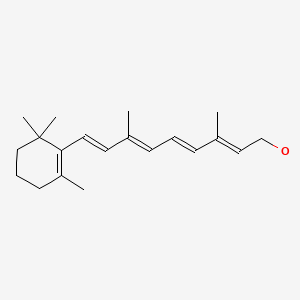
CASRN: 68-26-8
Drug Levels and Effects
Summary of Use during Lactation
Vitamin A (retinol) and provitamin A carotenoids are normal components of human milk.[1] Vitamin A in milk has antioxidant properties.[2] The recommend dietary intake in lactating women is 1300 mcg retinol daily, compared to 770 mcg daily during pregnancy. The recommended daily intake for infants aged 6 months or less is 400 mcg. Vitamin A deficiency is not uncommon, and maternal supplementation may be needed during lactation to achieve the recommended daily vitamin A intake. Maternal single doses up to 120,000 mcg (400,000 IU) or daily doses up to 1500 mcg (5,000 IU) are not expected to harm the breastfed infant. Higher maternal doses have not been studied. Daily maternal doses above 3,000 mcg (10,000 IU) should be avoided.[3]
Drug Levels
Vitamin A (retinol) measurements are expressed in the literature as mcg, IU, or micromoles. One mcg is equal to 3.33 IU (0.3 mcg = 1 IU), and also to 0.0035 micromoles (286 mcg = 1 micromole). Beta-carotene from vitamin supplements is one-half as potent as retinol. One mcg of beta-carotene from vitamin supplements is therefore equal to 0.5 mcg retinol (see the LactMed beta-carotene record). A serum retinol concentration less than 0.7 micromoles/L (<200 mcg/L) indicates biochemical vitamin A deficiency, and 0.7 to 1.05 micromoles/L (200 to 300 mcg/L) indicates marginal deficiency.[2] Milk levels less than 1.05 micromoles/L (<300 mcg/L) indicates low milk vitamin A content.[4]
Most retinol present in milk are retinyl esters (e.g., retinyl acetate), which can be de-esterified in the infant's digestive tract.[5] Mature milk retinol levels correlate with maternal serum retinol levels, and levels of milk retinol and beta-carotene are correlated with one another.[6-10] Milk retinol and carotenoid levels in colostrum are higher than in mature milk. Intra-individual colostrum levels vary widely, but are consistently higher than and not correlated with maternal serum levels, suggesting active colostrum enrichment.[11] Levels decrease over the first 1 to 2 weeks postpartum and then stabilize.[2,12,13] Vitamin A partitions into milk fat and milk retinol levels are positively correlated with milk fat.[9,14] Hindmilk levels are higher than foremilk.[15,16] Milk vitamin A content increases as maternal dietary vitamin A increases.[17] Nutritionally deficient mothers have lower milk retinol and provitamin A carotenoid levels than those of well-nourished mothers.[6,18,19] Premature birth may also be associated with lower milk retinol levels.[20,21]
Maternal Levels. Healthy mothers not taking a supplement have retinol levels averaging 800 to 1400 mcg/L in colostrum and 300 to 800 mcg/L in mature milk.[10,11,13,16,19,22,23] Beta-carotene, lutein and lycopene are among the most abundant carotenoids in milk, totaling 300 to 400 mcg/L in the first week postpartum and 50 to 200 mcg/L in mature milk.[1,10,12,13,19]
Numerous studies targeting lactating women living in regions with endemic vitamin A deficiency have evaluated the effects of a single vitamin A dose of 200,000 to 400,000 IU given in the early postpartum period. Most of these studies demonstrate small increases in milk retinol levels compared to the control or placebo group during the first 3 months postpartum. In a meta-analysis of six such studies, the average increase in milk retinol was 57 mcg/L in the mothers treated with vitamin A compared to placebo.[24] Studies that controlled for milk fat content had similar outcomes. In two of the analyzed studies, the frequencies of low milk levels (<300 mcg/L) were 25% and 50% lower in supplemented mothers compared to control. Based on the average increase in milk retinol reported in this meta-analysis, the single, high-dose vitamin A postpartum maternal supplementation strategy would provide breastfed infants with an extra 3.5 to 13 mcg/kg of retinol daily after the first postpartum week.
A study involving 102 mothers from Hyderabad, India given 200,000 IU of vitamin A within 24 hours of birth reported higher average milk retinol levels in the vitamin A group at postpartum day 10 (1100 mcg/L vs. 800 mcg/L), and day 30 (750 mcg/L vs 600 mcg/L), but not on or after day 45. The increase in milk retinol intake from maternal supplementation during the first month after birth for a breastfed infant based on these results would be about 30 mcg/kg daily.[23] In a similar study conducted in northeastern Brazil, average milk retinol was higher in the colostrum of the supplemented group 24 hours after the dose (2360 mcg/L vs 1010 mcg/L), but was not significantly different at 30 days (525 mcg/L vs. 478 mcg/L).[25]
A large study conducted in Ghana, Peru, and India gave vitamin A 200,000 IU or placebo to 2,990 breastfeeding mothers at 18 to 42 days postpartum. The average milk retinol level at baseline was similar in both groups (52.2 vs 51.6 nmol/gram of fat), but was higher at 2 months postpartum in the vitamin A group (49.8 vs. 42.7 nmol/gram of fat). The percentage of mothers at 2 months with milk retinol of 28 nanomoles/gram of fat or less, indicating low milk vitamin A content, was 49% in the treatment group compared to 79% in the placebo group. At 6 months postpartum, there were no differences between the groups.[26]
Studies comparing a 400,000 IU dose to a 200,000 IU dose of vitamin A have found no differences in milk vitamin A levels between the two dosage groups.[27-31]
One hundred forty healthy, low-income mothers in Rabat, Morocco were given 200,000 IU of vitamin A as a one-time dose beginning at 2 to 3 weeks after birth. In addition, the mothers were randomized to receive vegetable oil fortified with retinyl palmitate 30 IU per gram of oil, or non-fortified oil. The oil was to be used in the home during routine food preparation, not as a daily required study dose. Both groups had milk retinol levels near 515 mcg/L at baseline. After three months, average milk levels were 386 mcg/L in the nonfortified group and 592 mcg/L in the fortified group; 20% of mothers in the nonfortified group had low milk levels (<300 mcg/L) compared to none in the fortified group. After 6 months, the differences were 172 mcg/L vs. 398 mcg/L, and 100% vs. 2.7%, respectively.[32] Based on the average milk levels reported, exclusively breastfed infants would receive approximately an extra 30 mcg/kg retinol daily from the regimen used in this study.
Daily supplementation of 2165 IU vitamin A was compared to no supplementation in 119 Gambian pregnant and postpartum women. Milk retinol levels collected once weekly between postpartum weeks 3 and 15 were higher in the supplemented mothers, ranging from 800 to 1000 mcg/L, compared to 500 to 700 mcg/L in the non-supplemented mothers. Adjusting for milk fat content did not change the results.[33] Based on the milk levels reported, breastfed infants would receive an extra 45 mcg/kg retinol daily as a result of this long-term, pregnancy through postpartum extended supplementation approach.
Two hundred forty-five healthy, exclusively breastfeeding mothers in Nanjing, China were randomized to receive a daily vitamin A supplement of 1800 IU or placebo for 2 months beginning at 1 to 2 months postpartum. Both groups had similar average milk retinol levels of approximately 450 mcg/L at baseline. After two months, average milk level in the supplemented group was 290 mcg/L compared to 240 mcg/L in the control group. The difference amounts to an extra 7.5 mcg/kg retinol daily received by the breastfed infant from the short period of maternal supplementation.[23]
HIV-infected pregnant women with vitamin A deficiency or marginal deficiency in Tanzania were enrolled in a study to receive 1 of 4 supplements during pregnancy and lactation. Groups received either multivitamins (thiamine, riboflavin, vitamin B6, niacin, vitamin B12, vitamin C, vitamin E, and folic acid), multivitamins plus vitamin A 5000 IU and beta-carotene 30 mg, the same doses of vitamin A and beta-carotene alone, or placebo once daily beginning in their second trimester and continuing for two years. Breastmilk samples were collected at delivery and at 3-month intervals thereafter up to 1 year. Breastmilk retinol levels in the vitamin A and beta-carotene supplemented groups were consistently about 2 to 3 micromoles/L (570 to 860 mcg/L) higher during the entire study period than in the groups that received no supplement. The average milk levels were 1400 mcg/L vs 640 mcg/L at 3 months, 1350 mcg/L vs 640 mcg/L at 6 months, and 1300 mcg/L vs 630 mcg/L at 12 months.[34] Based on the maximum average retinol levels reported, an exclusively breastfed infant would receive an extra 114 mcg/kg daily of retinol from the maternal supplementation used in this study.
Premature birth may be associated with lower milk retinol levels. A southeastern Brazilian study of non-supplemented mothers reported average levels of 286 mcg/L at around 30 days postpartum in those who delivered preterm babies compared to 534 mcg/L in those delivering at term.[21] Similarly, in a study from Mexico of non-supplemented mothers who experienced high-risk pregnancies (e.g., preeclampsia, anemia, advanced maternal age or gestational diabetes), premature birth increased the odds of low milk retinol levels compared to term birth, and compared to mothers with normal pregnancies.[21]
Infant Levels. One hundred nine Indian mothers were given a single dose of vitamin A 200,000 IU or no vitamin A within 48 hours of delivery. At 3 months postpartum the average infant serum retinol level was higher (1.06 micromoles/L vs 0.77 micromoles/L) and the percentage of infants with serum levels <0.7 micromoles/L was lower (2.6% vs 44.8%) in the vitamin A group. One-half of all infants had umbilical cord retinol levels <0.7 micromoles/L, but differences between the two groups for this baseline measurement were not reported.[35]
One hundred forty Indonesian mothers were given a single oral dose of 300,000 IU vitamin A as retinyl palmitate or placebo between 7 and 21 days postpartum. Baseline infant serum retinol was not measured. At 6 months postpartum, average infant serum retinol levels did not differ between the two groups. However, the proportion of infants with levels <0.52 micromoles/L was lower in the treatment group, 15% vs 36%. Breastfeeding rates and infant diet were the same in both groups.[36]
One hundred forty mothers in Bangladesh were given 200,000 IU vitamin A or placebo between 1 and 3 weeks postpartum. Baseline infant serum retinol was not measured. Infant vitamin A dietary and supplemental intakes during the first 6 months of age were not different between the two groups. Infants were partially breastfed for 6 months, at which time the average infant serum retinol level was higher in the vitamin A group, 0.84 micromoles/L compared to 0.77 micromoles/L in the placebo group. Biochemical indicators of adequate infant vitamin A storage were also better in the vitamin A group.[37]
One hundred ten Gambian women were given 200,000 IU vitamin A shortly after delivery. Breastfeeding rates were not given, but >90% of participants were able to provide milk for study analysis during the 6 months postpartum milk collection period. Average infant serum retinol increased from 0.67 micromoles/L in cord blood to 0.85 micromoles/L at 9 months. The percentage of infants with levels <0.7 micromoles/L decreased from 61% at birth to 31% at 9 months.[27]
To compare a 200,000 IU to a 400,000 IU maternal dose, 173 Brazilian mothers were given 200,000 IU vitamin A once after delivery, or once after delivery and again at 10 days postpartum. Their infants were more than 75% breastfed for 6 months, but not supplemented with vitamin A directly. The average infant serum levels in umbilical cord blood and in blood at 2, 4 and 6 months postpartum were similar in both groups: 1.1, 1.2, 1.5, and 1.55 micromoles/L, respectively. The increase compared to baseline was statistically significant in both groups. This study suggests that a single high maternal dose of vitamin A can improve infant vitamin A status through breastmilk, but a 400,000 IU dose offered no added improvement in status over a 200,000 IU maternal postpartum dose.[38]
One hundred exclusively breastfeeding Indian mothers were given 200,000 IU vitamin A or placebo as a single oral dose within 24 hours after delivery. Average infant serum retinol levels increased from approximately 0.5 micromoles/L in cord blood to 0.8 to 0.9 micromoles/L at 6 weeks to 6 months in both groups.[22]
In Kenya, 564 mothers were given 400,000 IU vitamin A or placebo within 24 hours of birth. About 30% of the mothers were vitamin A deficient at study entry. Their infants were also randomized to receive 100,000 IU vitamin A or placebo at 14 weeks of age. The average serum retinol level was similar in all infants at 14 weeks of age, about 0.9 micromoles/L, and again at 26 weeks among all infants who received placebo, about 1.0 micromoles/L. The lack of a difference did not change when controlling for maternal baseline serum retinol. Breastfeeding rates were not reported.[39]
In Brazil, 61 breastfeeding mothers received 200,000 IU vitamin A or placebo between 20 and 30 days postpartum. At 3 months postpartum the average infant serum retinol levels were similar: 0.69 micromoles/L in the vitamin A group and 0.64 micromoles/L in the placebo group. Seventy-five percent of infants were exclusively breastfed throughout the study period.[8]
Effects in Breastfed Infants
Maternal vitamin A supplementation during pregnancy and lactation has not reduced mortality or the risk of anemia in breastfed infants living in developing regions, but there may be health benefits related to improved antioxidant capacity and immune function.[24,40,41]
One hundred exclusively breastfeeding mothers in India were given 200,000 IU vitamin A or placebo as a single oral dose within 24 hours after delivery. There were no differences in weight gain of their infants during postpartum hospitalization between the groups, and no infants in the vitamin A group had symptoms of hypervitaminosis A, such as excessive crying, raised fontanelle and vomiting. All the infants received a dose of oral polio vaccine (OPV) between 48 and 72 hours after birth. There were no differences between the two groups in OPV seroconversion rates or antibody titers at 6 weeks.[42] Similarly, 1,085 exclusively breastfeeding mothers in Ghana were given 200,000 IU vitamin A or placebo at 3 to 4 weeks postpartum. There were no differences in infant immune response to polio or tetanus vaccination at 6 weeks and 6 months of age.[43]
The infants of 197 mothers in Gambia given either 200,000 or 400,000 IU vitamin A in the first week after delivery showed no signs of adverse reactions to vitamin A during the 12-month follow-up period.[27]
Two hundred forty-five healthy, exclusively breastfeeding mothers in Nanjing, China were randomized to receive a daily vitamin A 1800 IU supplement or placebo for 2 months beginning at 1 to 2 months postpartum. By the end of the 2 month study, infants in both groups had similar rates of febrile illnesses, respiratory tract infections, diarrhea, and eczema, although it was not stated how these data were collected.[23]
Effects on Lactation and Breastmilk
HIV-infected mothers in Tanzania had a higher rate of severe subclinical mastitis (36%), determined by measuring serial milk electrolyte concentrations, when taking a daily vitamin A supplement during pregnancy and postpartum compared to placebo (23%). Mothers taking a multivitamin without vitamin A also had a higher rate (38%) than placebo, suggesting a vitamin A-independent effect. Given the many other benefits of multivitamin supplementation in this specific patient population, the authors did not recommend avoiding supplementation due to a potential risk of mastitis.[44]
In a Brazilian study, 57 mothers received either 200,000 IU vitamin A or no vitamin A within 2 days after birth. At 24 hours after administration, the average level of alpha-tocopherol (vitamin E) was 16.4% lower in the colostrum of mothers who received in the vitamin A (28 micromoles/L compared to 24.5 micromoles/L), but it was not significantly different at 30 days after administration, at about 6 micromoles/L.[25] The reported vitamin E colostrum levels in this study are within normal limits, thus the small reduction in the vitamin A-supplemented mothers may not be clinically important. A different Brazilian research group conducting the same experiment using a vitamin A supplement with low-dose vitamin E 110 IU added as a preservative found no effect of vitamin A on colostrum alpha-tocopherol.[45]
Alternate Drugs to Consider
References
- 1.
- Khachik F, Spangler CJ, Smith JC, Jr, et al. Identification, quantification, and relative concentrations of carotenoids and their metabolites in human milk and serum. Anal Chem 1997;69:1873-81. [PubMed: 9164160]
- 2.
- Szlagatys-Sidorkiewicz A, Zagierski M, Jankowska A, et al. Longitudinal study of vitamins A, E and lipid oxidative damage in human milk throughout lactation. Early Hum Dev 2012;88:421-4. [PubMed: 22085741]
- 3.
- National Institutes of Health Office of Dietary Supplements. Vitamin A fact sheet for health professionals. 2022. [ Accessed Dec 13, 2023] https://ods
.od.nih.gov /factsheets/VitaminA-HealthProfessional/ - 4.
- Brown E, Akre J. Indicators for assessing vitamin A deficiency and their application in monitoring and evaluating intervention programmes. Geneva: World Health Organization 1996;WHO/NUT/96.10.
- 5.
- Lammi-Keefe CJ, Jensen RG. Fat-soluble vitamins in human milk. Nutr Rev 1984;42:365-71. [PubMed: 6396543]
- 6.
- Butte NF, Calloway DH. Evaluation of lactational performance of Navajo women. Am J Clin Nutr 1981;34:2210-5. [PubMed: 7293949]
- 7.
- Mello-Neto J, Rondo PH, Oshiiwa M, et al. The influence of maternal factors on the concentration of vitamin A in mature breast milk. Clin Nutr 2009;28:178-81. [PubMed: 19249141]
- 8.
- Martins TM, Ferraz IS, Daneluzzi JC, et al. Impact of maternal vitamin A supplementation on the mother-infant pair in Brazil. Eur J Clin Nutr 2010;64:1302-7. [PubMed: 20842169]
- 9.
- Dror DK, Allen LH. Retinol-to-fat ratio and retinol concentration in human milk show similar time trends and associations with maternal factors at the population level: A systematic review and meta-analysis. Adv Nutr 2018;9 (Suppl 1):332S-346S. [PMC free article: PMC6008956] [PubMed: 29846525]
- 10.
- Gebre-Medhin M, Vahlquist A, Hofvander Y, et al. Breast milk composition in Ethiopian and Swedish mothers. I. Vitamin A and beta-carotene. Am J Clin Nutr 1976;29:441-51. [PubMed: 944526]
- 11.
- de Vries JY, Pundir S, Mckenzie E, et al. Maternal circulating vitamin status and colostrum vitamin composition in healthy lactating women-a systematic approach. Nutrients 2018;10:E687. [PMC free article: PMC6024806] [PubMed: 29843443]
- 12.
- Gossage CP, Deyhim M, Yamini S, et al. Carotenoid composition of human milk during the first month postpartum and the response to beta-carotene supplementation. Am J Clin Nutr 2002;76:193-7. [PubMed: 12081834]
- 13.
- Sakurai T, Furukawa M, Asoh M, et al. Fat-soluble and water-soluble vitamin contents of breast milk from Japanese women. J Nutr Sci Vitaminol (Tokyo) 2005;51:239-47. [PubMed: 16261995]
- 14.
- Stoltzfus RJ, Underwood BA. Breast-milk vitamin A as an indicator of the vitamin A status of women and infants. Bull World Health Organ 1995;73:703-11. [PMC free article: PMC2486808] [PubMed: 8846497]
- 15.
- Hampel D, Shahab-Ferdows S, Islam MM, et al. Vitamin concentrations in human milk vary with time within feed, circadian rhythm, and single-dose supplementation. J Nutr 2017;147:603-11. [PMC free article: PMC5368580] [PubMed: 28202638]
- 16.
- Nimmannun K, Davis CR, Srisakda P, et al. Breast milk retinol concentrations reflect total liver vitamin a reserves and dietary exposure in thai lactating women from urban and rural areas. J Nutr 2023;152:2689-98. [PubMed: 36170963]
- 17.
- Kodentsova VM, Vrzhesinskaya OA. Evaluation of the vitamin status in nursing women by vitamin content in breast milk. Bull Exp Biol Med 2006;141:323-7. [PubMed: 17073150]
- 18.
- Bates CJ, Prentice A. Breast milk as a source of vitamins, essential minerals and trace elements. Pharmacol Ther 1994;62:193-220. [PubMed: 7991643]
- 19.
- Lu Z, Chan YT, Lo KK, et al. Carotenoids and vitamin A in breastmilk of Hong Kong lactating mothers and their relationships with maternal diet. Nutrients 2022;14:2031. [PMC free article: PMC9148123] [PubMed: 35631170]
- 20.
- Souza G, Dolinsky M, Matos A, et al. Vitamin A concentration in human milk and its relationship with liver reserve formation and compliance with the recommended daily intake of vitamin A in pre-term and term infants in exclusive breastfeeding. Arch Gynecol Obstet 2015;291:319-25. [PubMed: 25118833]
- 21.
- Sámano R, Martínez-Rojano H, Hernández RM, et al. Retinol and alpha-tocopherol in the breast milk of women after a high-risk pregnancy. Nutrients 2017;9:E14. [PMC free article: PMC5295058] [PubMed: 28045436]
- 22.
- Bhaskaram P, Balakrishna N, Nair M, Sivakumar, B. Vitamin A deficiency in infants: Effects of postnatal maternal vitamin A supplementation on the growth and vitamin A status. Nutr Res 2000;20:769–78. doi:10.1016/S0271-5317(00)00176-7 [CrossRef]
- 23.
- Ding Y, Hu P, Yang Y, et al. Impact of maternal daily oral low-dose vitamin a supplementation on the mother–infant pair: A randomised placebo-controlled trial in China. Nutrients 2021;13:2370. [PMC free article: PMC8308679] [PubMed: 34371880]
- 24.
- Oliveira JM, Allert R, East CE. Vitamin A supplementation for postpartum women. Cochrane Database Syst Rev 2016;3:CD005944. [PMC free article: PMC8407451] [PubMed: 27012320]
- 25.
- Grilo EC, Medeiros WF, Silva AG, et al. Maternal supplementation with a megadose of vitamin A reduces colostrum level of alpha-tocopherol: A randomised controlled trial. J Hum Nutr Diet 2016;29:652-61. [PubMed: 27231056]
- 26.
- Bahl R, Bhandari N, Wahed MA, et al. Vitamin A supplementation of women postpartum and of their infants at immunization alters breast milk retinol and infant vitamin A status. J Nutr 2002;132:3243-8. [PubMed: 12421835]
- 27.
- Darboe MK, Thurnham DI, Morgan G, et al. Effectiveness of an early supplementation scheme of high-dose vitamin A versus standard WHO protocol in Gambian mothers and infants: a randomised controlled trial. Lancet 2007;369:2088-96. [PubMed: 17586304]
- 28.
- Idindili B, Masanja H, Urassa H, et al. Randomized controlled safety and efficacy trial of 2 vitamin A supplementation schedules in Tanzanian infants. Am J Clin Nutr 2007;85:1312-9. [PubMed: 17490968]
- 29.
- Bezerra DS, de Araujo KF, Azevedo GM, Dimenstein R. A randomized trial evaluating the effect of 2 regimens of maternal vitamin A supplementation on breast milk retinol levels. J Hum Lact 2010;26:148-56. [PubMed: 20110563]
- 30.
- Tomiya MTO, de Arruda IKG, da Silva Diniz A, et al. The effect of vitamin A supplementation with 400 000 IU vs 200 000 IU on retinol concentrations in the breast milk: A randomized clinical trial. Clin Nutr 2017;36:100-6. [PubMed: 26725194]
- 31.
- Bezerra DS, de Melo ATA, de Oliveira Kcan, et al. Breast milk retinol levels after vitamin A supplementation at different postpartum amounts and intervals. Nutrients 2022;14:3570. [PMC free article: PMC9460635] [PubMed: 36079825]
- 32.
- Atalhi N, El Hamdouchi A, Barkat A, et al. Combined consumption of a single high-dose vitamin A supplement with provision of vitamin A fortified oil to households maintains adequate milk retinol concentrations for 6 months in lactating Moroccan women. Appl Physiol Nutr Metab 2020;45:275-82. [PubMed: 31365834]
- 33.
- Villard L, Bates CJ. Effect of vitamin A supplementation on plasma and breast milk vitamin A levels in poorly nourished Gambian women. Hum Nutr Clin Nutr 1987;41:47-58. [PubMed: 3570862]
- 34.
- Webb AL, Aboud S, Furtado J, et al. Effect of vitamin supplementation on breast milk concentrations of retinol, carotenoids and tocopherols in HIV-infected Tanzanian women. Eur J Clin Nutr 2009;63:332-9. [PMC free article: PMC3095494] [PubMed: 17940544]
- 35.
- Vinutha B, Mehta MN, Shanbag P. Vitamin A status of pregnant women and effect of post partum vitamin A supplementation. Indian Pediatr 2000;37:1188-93. [PubMed: 11086300]
- 36.
- Stoltzfus RJ, Hakimi M, Miller KW, et al. High dose vitamin A supplementation of breast-feeding Indonesian mothers: Effects on the vitamin A status of mother and infant. J Nutr 1993;123:666-75. [PubMed: 8463867]
- 37.
- Rice AL, Stoltzfus RJ, de Francisco A, et al. Maternal vitamin A or beta-carotene supplementation in lactating Bangladeshi women benefits mothers and infants but does not prevent subclinical deficiency. J Nutr 1999;129:356-65. [PubMed: 10024613]
- 38.
- Dos Santos CS, Kruze I, Fernándes T, et al. The effect of a maternal double megadose of vitamin A supplement on serum levels of retinol in children aged under six months. J Nutr Metab 2013;2013:876308. [PMC free article: PMC3886490] [PubMed: 24455219]
- 39.
- Ayah RA, Mwaniki DL, Magnussen P, et al. The effects of maternal and infant vitamin A supplementation on vitamin A status: a randomised trial in Kenya. Br J Nutr 2007;98:422-30. [PubMed: 17391562]
- 40.
- Miller MF, Stoltzfus RJ, Iliff PJ, et al. Effect of maternal and neonatal vitamin A supplementation and other postnatal factors on anemia in Zimbabwean infants: a prospective, randomized study. Am J Clin Nutr 2006;84:212-22. [PubMed: 16825698]
- 41.
- Cox SE, Arthur P, Kirkwood BR, et al. Vitamin A supplementation increases ratios of proinflammatory to anti-inflammatory cytokine responses in pregnancy and lactation. Clin Exp Immunol 2006;144:392-400. [PMC free article: PMC1941972] [PubMed: 16734607]
- 42.
- Bhaskaram P, Balakrishna N. Effect of administration of 200,000 IU of vitamin A to women within 24 hrs after delivery on response to PPV administered to the newborn. Indian Pediatr 1998;35:217-22. [PubMed: 9707874]
- 43.
- Newton S, Cousens S, Owusu-Agyei S, et al. Vitamin A supplementation does not affect infants' immune responses to polio and tetanus vaccines. J Nutr 2005;135:2669-73. [PubMed: 16251628]
- 44.
- Arsenault JE, Aboud S, Manji KP, et al. Vitamin supplementation increases risk of subclinical mastitis in HIV-infected women. J Nutr 2010;140:1788-92. [PMC free article: PMC2937574] [PubMed: 20739447]
- 45.
- García L, Ribeiro K, Araujo K, et al. Alpha-tocopherol concentration in the colostrum of nursing women supplemented with retinyl palmitate and alpha-tocopherol. J Hum Nutr Diet 2010;23:529-34. [PubMed: 20831709]
Substance Identification
Substance Name
Vitamin A
CAS Registry Number
68-26-8 79-81-2
Disclaimer: Information presented in this database is not meant as a substitute for professional judgment. You should consult your healthcare provider for breastfeeding advice related to your particular situation. The U.S. government does not warrant or assume any liability or responsibility for the accuracy or completeness of the information on this Site.
- User and Medical Advice Disclaimer
- Drugs and Lactation Database (LactMed) - Record Format
- LactMed - Database Creation and Peer Review Process
- Fact Sheet. Drugs and Lactation Database (LactMed)
- Drugs and Lactation Database (LactMed) - Glossary
- LactMed Selected References
- Drugs and Lactation Database (LactMed) - About Dietary Supplements
- Breastfeeding Links
- PMCPubMed Central citations
- PubChem SubstanceRelated PubChem Substances
- PubMedLinks to PubMed
- Review Vitamin D.[Drugs and Lactation Database (...]Review Vitamin D.. Drugs and Lactation Database (LactMed®). 2006
- Review Vitamin B(12).[Drugs and Lactation Database (...]Review Vitamin B(12).. Drugs and Lactation Database (LactMed®). 2006
- Review Tretinoin.[Drugs and Lactation Database (...]Review Tretinoin.. Drugs and Lactation Database (LactMed®). 2006
- Review Isotretinoin.[Drugs and Lactation Database (...]Review Isotretinoin.. Drugs and Lactation Database (LactMed®). 2006
- Review Vitamin E.[Drugs and Lactation Database (...]Review Vitamin E.. Drugs and Lactation Database (LactMed®). 2006
- Vitamin A - Drugs and Lactation Database (LactMed®)Vitamin A - Drugs and Lactation Database (LactMed®)
Your browsing activity is empty.
Activity recording is turned off.
See more...
